Molecular Identification and Antifungal Susceptibility Patterns of Clinical Dermatophytes Following CLSI and EUCAST Guidelines
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Processing
2.2. Identification of Isolates
2.3. ITS DNA Sequencing
2.4. Antifungal Susceptibility Testing
2.5. Statistical Analysis
3. Results
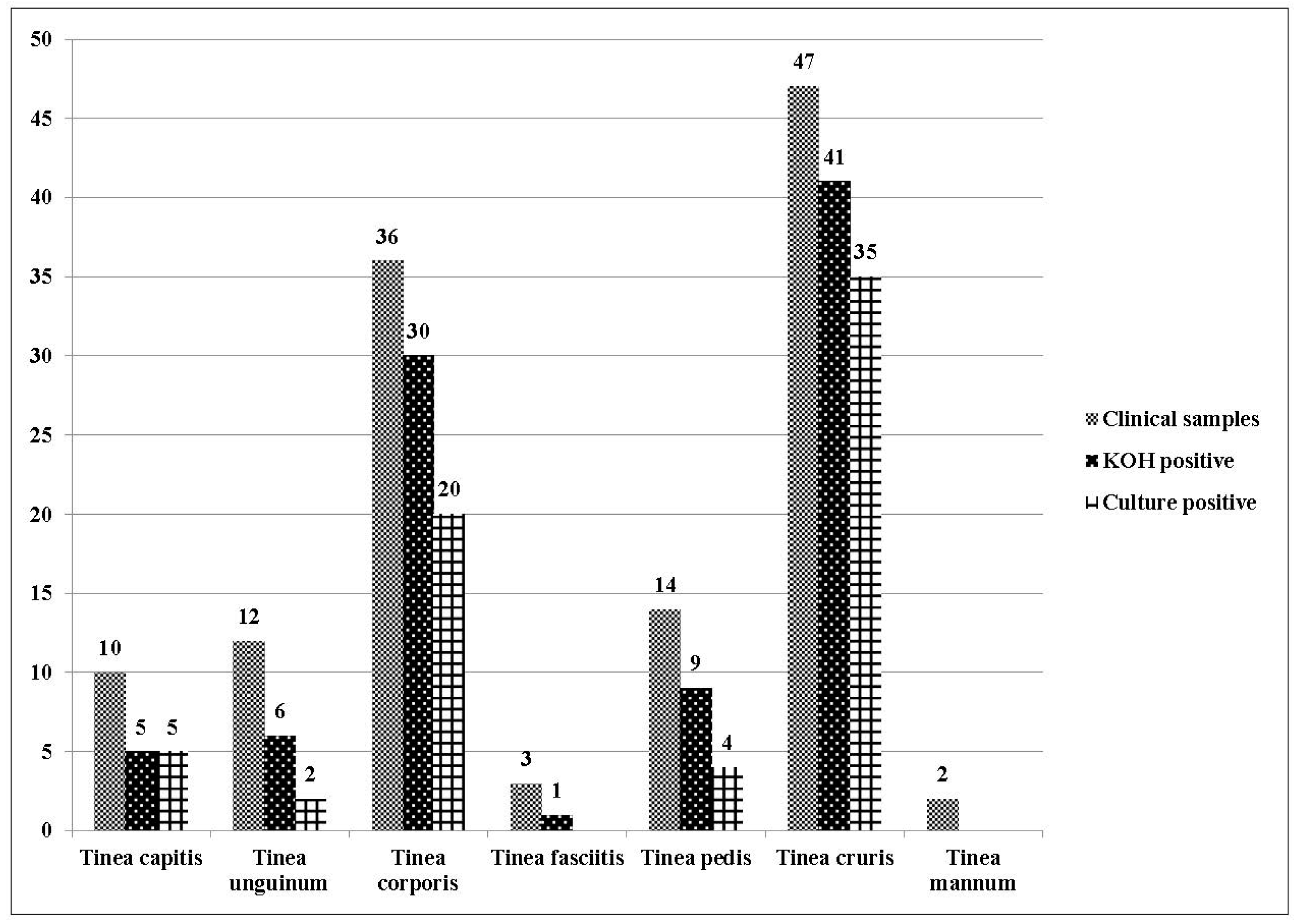
3.1. Identification of Dermatophytes
3.2. Antifungal Susceptibility Testing
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Weitzman, I.; Summerbell, R.C. The Dermatophytes. Clin. Microbiol. Rev. 1995, 8, 240–259. [Google Scholar] [CrossRef]
- Chander, J. Test Book of Medical Mycology, 3rd ed.; Mehta Publishers: Maharashtra, India, 2009; pp. 122–146. [Google Scholar]
- Sharma, V.; Kumawat, T.K.; Sharma, A.; Seth, R.; Chandra, S. Dermatophytes: Diagnosis of dermatophytosis and its treatment. Afr. J. Microbiol. Res. 2015, 9, 1286–1293. [Google Scholar]
- Bhatia, V.K.; Sharma, P.C. Determination of minimum inhibitory concentrations of itraconazole, terbinafine and ketoconazole against dermatophyte species by broth microdilution method. Indian J. Med. Microbiol. 2015, 33, 533–537. [Google Scholar] [PubMed]
- Bhatia, V.K.; Sharma, P.C. Epidemiological studies on dermatophytosis in human patients in Himachal Pradesh, India. Springerplus 2014, 3, 134. [Google Scholar] [CrossRef] [PubMed]
- Elewski, B.E. Onychomycosis: Pathogenesis, diagnosis, and management. Clin. Microbiol. Rev. 1998, 11, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Sugiura, K.; Hashimoto, T.; Ueda, A.; Konno, Y.; Tatsumi, Y. Efficacy coefficients determined using nail permeability and antifungal activity in keratin-containing media are useful for predicting clinical efficacies of topical drugs for onychomycosis. PLoS ONE 2016, 11, e0159661. [Google Scholar] [CrossRef] [PubMed]
- Piraccini, B.M.; Alessandrini, A. Onychomycosis: A Review. J. Fun. 2015, 1, 30–43. [Google Scholar] [CrossRef]
- Vandeputte, P.; Ferrari, S.; Coste, A.T. Antifungal resistance and new strategies to control fungal infections. Int. J. Microbiol. 2012, 2012, 713687. [Google Scholar] [CrossRef] [PubMed]
- Karakousis, A.; Tan, L.; Ellis, D.; Alexiou, H.; Wormald, P.J. An assessment of the efficiency of fungal DNA extraction methods for maximizing the detection of medically important fungi using PCR. J. Microbiol. Methods 2006, 65, 38–48. [Google Scholar] [CrossRef] [PubMed]
- White, T.J.; Bruns, T.; Lee, S.; Taylor, J.W. Amplification and Direct Sequencing of Fungal Ribosomal RNA Genes for Phylogenetics. In PCR Protocols: A Guide to Methods and Applications; Innis, M.A., Gelfand, D.H., Sninsky, J.J., White, T.J., Eds.; Academic Press, Inc.: New York, NY, USA, 1990; pp. 315–322. [Google Scholar]
- Clinical Laboratory Standards Institute. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi; Approved Standard, 2nd ed.; CLSI document M38-A2; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2008. [Google Scholar]
- Arendrup, M.C.; Hope, W.; Howard, S.J. EUCAST Definitive Document E.Def 9.2 Method for the Determination of Broth Dilution Minimum Inhibitory Concentrations of Antifungal Agents for Conidia Forming Moulds; EUCAST: Basel, Switzerland, 2014. [Google Scholar]
- Cuenca-Estrella, M.; Gómez-López, A.; Alastruey-Izquierdo, A.; Bernal-Martinez, L.; Cuesta, I.; Buitrago, M.J.; Rodriguez-Tudela, J.L. Comparison of the Vitek 2 antifungal susceptibility system with the Clinical and Laboratory Standards Institute (CLSI) and European Committee on Antimicrobial Susceptibility Testing (EUCAST) broth microdilution reference methods and with the Sensititre YeastOne and Etest techniques for in vitro detection of antifungal resistance in yeast isolates. J. Clin. Microbiol. 2010, 48, 1782–1786. [Google Scholar] [PubMed]
- Deshmukh, S.K.; Verekar, S.V.; Shrivastav, A. The occurrence of keratinophilic fungi in selected soils of Ladakh (India). Nature 2010, 2, 1247–1252. [Google Scholar] [CrossRef]
- Singh, S.; Beena, P.M. Profile of dermatophyte infections in Baroda. Indian J. Dermatol. Venereol. Leprol. 2003, 69, 281–283. [Google Scholar] [PubMed]
- Singh, S.; Beena, P.M. Comparative study of different microscopic techniques and culture media for the isolation of dermatophytes. Indian J. Med. Microbiol. 2003, 21, 21–24. [Google Scholar] [PubMed]
- Sarma, S.; Borthakur, A.K.A. Clinico—Epidermatological study of dermatophytoses in Northest India. Indian J. Dermatol. Venereol. Leprol. 2007, 73, 427–428. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Mulla, S.; Patel, D.; Shrimali, G. A study of superficial mycosis in south Gujarat region. Natl. J. Commun. Med. 2010, 1, 85–88. [Google Scholar]
- Venkatesan, G.; Singh, A.J.A.; Murugesan, A.G.; Janaki, C.; Shankar, S.G. Trichophyton rubrum—The predominant aetiological agent in human dermatophytosis in Chennai, India. Afr. J. Microbiol. Res. 2007, 1, 9–12. [Google Scholar]
- Ranganathan, S.; Menon, T.; Sentamil, G.S. Effect of socioeconomical status on the prevalence of dermatophytosis in Madras. Indian J. Dermatol. Venereol. Leprol. 1995, 61, 16–18. [Google Scholar] [PubMed]
- Dhib, I.; Khammari, I.; Yaacoub, A.; Hadj Slama, F.; Ben Said, M.; Zemni, R.; Fathallah, A. Relationship between phenotypic and genotypic characteristics of Trichophyton mentagrophytes strains isolated from patients with dermatophytosis. Mycopathologia 2017. [Google Scholar] [CrossRef] [PubMed]
- Li, H.C.; Bouchara, J.P.; Hsu, M.M.L.; Barton, R.; Su, S.; Chang, T.C. Identification of dermatophytes by sequence analysis of the rRNA gene internal transcribed spacer regions. J. Med. Microbiol. 2008, 57, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Balakumar, S.; Rajan, S.; Thirunalasundari, T.; Jeeva, S. Epidemiology of dermatophytosis in and around Tiruchirapalli, Tamilnadu, India. Asian Pac. J. Trop. Dis. 2012, 2, 286–289. [Google Scholar] [CrossRef]
- Pandey, A.; Pandey, M. Isolation and characterization of dermatophytes with tinea infection at Gwalior (M.P.), India. Int. J. Pharm. Sci. Investig. 2013, 2, 5–8. [Google Scholar]
- Kaur, R.; Kashyap, B.; Bhalla, P. A five-year survey of onychomycosis in New Delhi, India: Epidemiological and laboratory aspects. Indian J. Dermatol. 2007, 52, 39–42. [Google Scholar]
- Adhikari, L.; Gupta, A.D.; Pal, R.; Singh, T. Clinico-etiologic correlates of onychomycosis in Sikkim. Indian J. Pathol. Microbiol. 2009, 52, 194–197. [Google Scholar] [PubMed]
- Yadav, P.; Singal, A.; Pandhi, D.; Das, S. Clinicomycological study of dermatophyte toenail onychomycosis in New Delhi, India. Indian J. Dermatol. 2015, 60, 153–158. [Google Scholar] [PubMed]
- Agarwalla, A.; Agrawal, S.; Khanal, B. Onychomycosis in eastern Nepal. Nepal Med. Coll. J. 2006, 8, 215–219. [Google Scholar] [PubMed]
- Hashemi, S.J.; Gerami, M.; Zibafar, E.; Daei, M.; Moazeni, M.; Nasrollahi, A. Onychomycosis in Tehran: Mycological study of 504 patients. Mycoses 2010, 53, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Chadeganipour, M.; Nilipour, S.; Ahmadi, G. Study of onychomycosis in Isfahan, Iran. Mycoses 2010, 53, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Jessup, C.J.; Warner, J.; Isham, N.; Hasan, I.; Ghannoum, M.A. Antifungal susceptibility testing of dermatophytes: Establishing a medium for inducing conidial growth and evaluation of susceptibility of clinical isolates. J. Clin. Microbiol. 2000, 38, 341–344. [Google Scholar] [PubMed]
- Indira, G. In vitro antifungal susceptibility testing of 5 antifungal agents against dermatophytic species by CLSI (M38-A) micro dilution method. Clin. Microbial. 2014, 3, 145. [Google Scholar] [CrossRef]
- Araújo, C.R.; Miranda, K.C.; Fernandes, O.F.L.; Soares, A.J.; Silva, M.R.R. In vitro susceptibility testing of dermatophytes isolated in Goiania, Brazil, against five antifungal agents by broth microdilution method. Rev. Inst. Med. Trop. 2009, 51, 9–12. [Google Scholar] [CrossRef]
- Ghannoum, M.A.; Hajjeh, R.A.; Scher, R.; Konnikov, N.; Gupta, A.K.; Summerbell, R.; Sullivan, S.; Daniel, R.; Krusinski, P.; Fleckman, P.; et al. A large-scale North American study of fungal isolates from nails: The frequency of onychomycosis, fungal distribution and antifungal susceptibility patterns. J. Am. Acad. Dermatol. 2000, 43, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Barros, M.E.; de Assis, S.D.; Hamdan, J.S. Evaluation of susceptibility of Trichophyton mentagrophytes and Trichophyton rubrum clinical isolates to antifungal drugs using a modified CLSI microdilution method (M38-A). J. Med. Microbiol. 2007, 56, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Kohli, Y. In vitro susceptibility testing of ciclopirox, terbinafine, ketoconazole and itraconazole against dermatophytes and nondermatophytes, and in vitro evaluation of combination antifungal activity. Br. J. Dermatol. 2003, 149, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Afshari, M.A.; Shams-Ghahfarokhi, M.; Razzaghi-Abyaneh, M. Antifungal susceptibility and virulence factors of clinically isolated dermatophytes in Tehran, Iran. Iran J. Microbiol. 2016, 8, 36–46. [Google Scholar] [PubMed]
- Tamura, T.; Asahara, M.; Yamamoto, M.; Yamaura, M.; Matsumura, M.; Goto, K.; Rezaei-Matehkolaei, A.; Mirhendi, H.; Makimura, M.; Makimura, K. In Vitro susceptibility of dermatomycoses agents to six antifungal drugs and evaluation by fractional inhibitory concentration index of combined effects of amorolfine and itraconazole in dermatophytes. Microbiol. Immunol. 2014, 58, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, S.; Ahmad, A.; Ali, S.M.; Paithankar, M.; Raval, R.C.; Shah, K.; Bhavsar, B.A.; KR, R.; AM, J.; et al. Topical delivery of lipid based amphotericin B gel in the treatment of fungal infection: A clinical efficacy, safety and tolerability study in patients. J. Clin. Exp. Dermatol. Res. 2014, 5, 248. [Google Scholar]
- Lurati, M.; Baudraz-Rosselet, F.; Vernez, M.; Spring, P.; Bontems, O.; Fratti, M.; Monod, M. Efficacious treatment of non-dermatophyte mould onychomycosis with topical amphotericin B. Dermatology 2011, 223, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Risslegger, B.; Lass-Flörl, C.; Blum, G.; Lackner, M. Evaluation of a modified EUCAST fragmented-mycelium inoculum method for in vitro susceptibility testing of dermatophytes and the activity of novel antifungal agents. Antimicrob. Agents Chemother. 2015, 59, 3675–3682. [Google Scholar] [CrossRef] [PubMed]

| Antifungals, Dermatophyte Species, and the Methodologies Followed | MIC Distribution (μg/mL) (No. of Isolates) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.03 | 0.06 | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | +GM | MIC50 | MIC90 | |
| Itraconazole | |||||||||||||
| T. interdigitale (n = 37) | |||||||||||||
| CLSI | 21 | 13 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.042 | 0.03 | 0.06 |
| EUCAST | 7 | 6 | 11 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0.077 | 0.06 | 0.125 |
| T. tonsurans (n = 17) | |||||||||||||
| CLSI | 15 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.033 | 0.03 | 0.06 |
| EUCAST | 0 | 15 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0.07 | 0.06 | 0.125 |
| T. rubrum (n = 5) | |||||||||||||
| CLSI | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.039 | 0.03 | 0.06 |
| EUCAST | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.07 | 0.06 | 0.125 |
| T. violaceum (n = 3) | |||||||||||||
| CLSI | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| EUCAST | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| M. gypseum (n = 3) | |||||||||||||
| CLSI | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| EUCAST | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| T. verrucosum (n = 1) | |||||||||||||
| CLSI | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | *NA | *NA | *NA |
| EUCAST | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | *NA | *NA | *NA |
| Terbinafine | |||||||||||||
| T. interdigitale (n = 37) | |||||||||||||
| CLSI | 3 | 2 | 5 | 5 | 14 | 5 | 0 | 0 | 2 | 1 | 0.375 | 0.5 | 1 |
| EUCAST | 0 | 5 | 0 | 4 | 6 | 15 | 4 | 0 | 2 | 1 | 0.683 | 1 | 2 |
| T. tonsurans (n = 17) | |||||||||||||
| CLSI | 3 | 0 | 0 | 2 | 2 | 1 | 4 | 2 | 2 | 1 | 0.878 | 2 | 8 |
| EUCAST | 0 | 2 | 1 | 0 | 2 | 2 | 4 | 2 | 3 | 1 | 1.379 | 2 | 8 |
| T. rubrum (n = 5) | |||||||||||||
| CLSI | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0.863 | 0.5 | 8 |
| EUCAST | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0.991 | 0.5 | 8 |
| T. violaceum (n = 3) | |||||||||||||
| CLSI | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.048 | 0.03 | 0.125 |
| EUCAST | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.076 | 0.06 | 0.125 |
| M. gypseum (n = 3) | |||||||||||||
| CLSI | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.048 | 0.03 | 0.125 |
| EUCAST | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.076 | 0.06 | 0.125 |
| T. verrucosum (n = 1) | |||||||||||||
| CLSI | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | *NA | *NA | *NA |
| EUCAST | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | *NA | *NA | *NA |
| Griseofulvin | |||||||||||||
| T. interdigitale (n = 37) | |||||||||||||
| CLSI | 3 | 2 | 5 | 5 | 14 | 5 | 0 | 0 | 2 | 1 | 0.375 | 0.5 | 1 |
| EUCAST | 0 | 5 | 0 | 5 | 11 | 13 | 0 | 0 | 0 | 3 | 0.577 | 0.5 | 1 |
| T. tonsurans (n = 17) | |||||||||||||
| CLSI | 1 | 2 | 0 | 0 | 4 | 3 | 5 | 1 | 0 | 1 | 0.777 | 1 | 4 |
| EUCAST | 0 | 1 | 1 | 1 | 0 | 2 | 4 | 3 | 4 | 1 | 1.995 | 2 | 8 |
| T. rubrum (n = 5) | |||||||||||||
| CLSI | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 1 | 0 | 3.031 | 4 | 8 |
| EUCAST | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 | 0 | 5.278 | 8 | 8 |
| T. violaceum (n = 3) | |||||||||||||
| CLSI | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| EUCAST | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.037 | 0.03 | 0.06 |
| M. gypseum (n = 3) | |||||||||||||
| CLSI | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.076 | 0.06 | 0.125 |
| EUCAST | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.076 | 0.06 | 0.125 |
| T. verrucosum (n = 1) | |||||||||||||
| CLSI | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | *NA | *NA | *NA |
| EUCAST | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | *NA | *NA | *NA |
| Amphotericin B | |||||||||||||
| T. interdigitale (n = 37) | |||||||||||||
| CLSI | 13 | 4 | 18 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0.072 | 0.125 | 0.125 |
| EUCAST | 13 | 4 | 18 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0.072 | 0.125 | 0.125 |
| T. tonsurans (n = 17) | |||||||||||||
| CLSI | 4 | 3 | 5 | 0 | 3 | 1 | 1 | 0 | 0 | 0 | 0.133 | 0.125 | 1 |
| EUCAST | 0 | 7 | 5 | 0 | 0 | 4 | 1 | 0 | 0 | 0 | 0.177 | 0.125 | 1 |
| T. rubrum (n = 5) | |||||||||||||
| CLSI | 1 | 1 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0.162 | 0.25 | 1 |
| EUCAST | 0 | 2 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0.245 | 0.25 | 2 |
| T. violaceum (n = 3) | |||||||||||||
| CLSI | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.125 | 0.125 | 0.125 |
| EUCAST | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0.157 | 0.125 | 0.25 |
| M. gypseum (n = 3) | |||||||||||||
| CLSI | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0.25 | 0.25 | 0.25 |
| EUCAST | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0.25 | 0.25 | 0.25 |
| T. verrucosum (n = 1) | |||||||||||||
| CLSI | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | *NA | *NA | *NA |
| EUCAST | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | *NA | *NA | *NA |
| Antifungal Agents | CLSI (%) (n = 66) | EUCAST (%) (n = 66) | Concordance | ICC (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| <0.5 µg/mL | 0.5–1 µg/mL | ≥2 µg/mL | <0.5 µg/mL | 0.5–1 µg/mL | ≥2 µg/mL | |||
| Itraconazole | 100 | 0 | 0 | 93.9 | 6 | 0 | 83.6 | 0.734 (0.038–0.895) |
| Terbinafine | 40.9 | 36.3 | 22.7 | 28.8 | 40.9 | 30.3 | 98.3 | 0.968 (0.396–0.991) |
| Griseofulvin | 36.3 | 42.4 | 21.2 | 28.8 | 39.4 | 31.8 | 96.7 | 0.957 (0.501–0.987) |
| Amphotericin B | 89.4 | 7.6 | 3 | 87.9 | 7.6 | 4.5 | 97.2 | 0.982 (0.965–0.99) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dabas, Y.; Xess, I.; Singh, G.; Pandey, M.; Meena, S. Molecular Identification and Antifungal Susceptibility Patterns of Clinical Dermatophytes Following CLSI and EUCAST Guidelines. J. Fungi 2017, 3, 17. https://doi.org/10.3390/jof3020017
Dabas Y, Xess I, Singh G, Pandey M, Meena S. Molecular Identification and Antifungal Susceptibility Patterns of Clinical Dermatophytes Following CLSI and EUCAST Guidelines. Journal of Fungi. 2017; 3(2):17. https://doi.org/10.3390/jof3020017
Chicago/Turabian StyleDabas, Yubhisha, Immaculata Xess, Gagandeep Singh, Mragnayani Pandey, and Suneeta Meena. 2017. "Molecular Identification and Antifungal Susceptibility Patterns of Clinical Dermatophytes Following CLSI and EUCAST Guidelines" Journal of Fungi 3, no. 2: 17. https://doi.org/10.3390/jof3020017





