Sex Differences in Acute Coronary Syndromes: A Global Perspective
Abstract
:1. Introduction: Global Burden of ACS and Disparities
2. Sex Differences in Presentation of ACS
3. Pathophysiology of Acute Coronary Syndromes in Women
3.1. Traditional Risk Factors
3.2. Non-Traditional Risk Factors
3.3. Female Specific Risk Enhancers
4. Female Coronary Anatomy and Physiology
5. Myocardial Infarction with Non-Obstructive Coronary Artery (MINOCA) Presentations
6. Bias in the Care of Women with STEMI
7. Sex Disparities in ACS: Global Trends
8. African Region (AFR)
9. Eastern Mediterranean Region (EMR)
10. South-East Asian Region (SEAR)
11. Western Pacific Region (WPR)
12. Region of the Americas (AMR)
13. European Region (EUR)
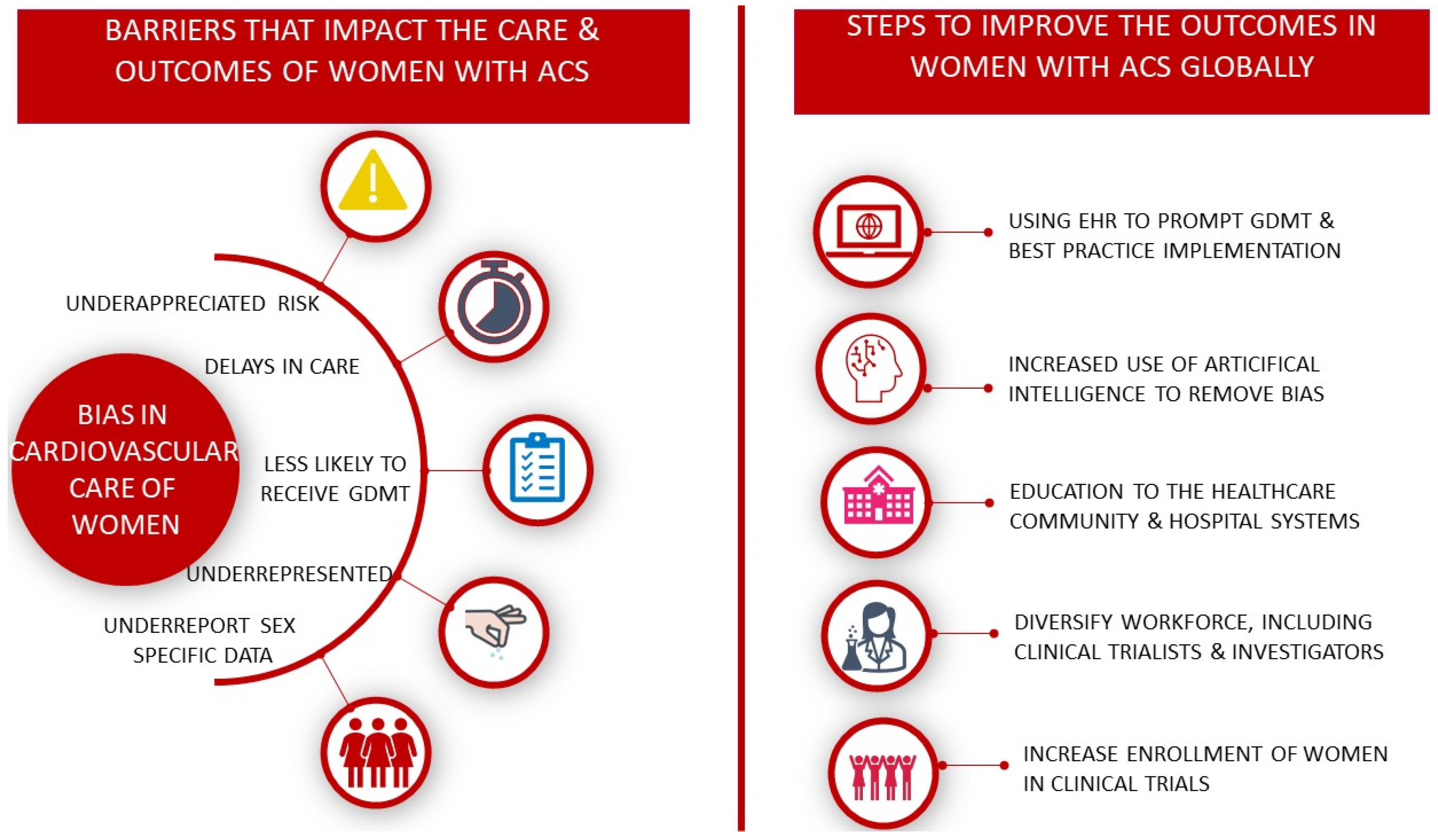
14. Closing the Gaps
15. Underrepresentation of Women in Clinical Trials
16. Targeted Action Plans
17. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. List of World Health Organization (WHO) Regions and Countries Belong to Each Region
References
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [PubMed]
- Jneid, H.; Fonarow, G.C.; Cannon, C.P.; Hernandez, A.F.; Palacios, I.F.; Maree, A.O.; Maree, A.O.; Wells, Q.; Bozkurt, B.; Labresh, K.A.; et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation 2008, 118, 2803–2810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matetic, A.; Shamkhani, W.; Rashid, M.; Volgman, A.S.; Van Spall, H.G.C.; Coutinho, T.; Mehta, L.S.; Sharma, G.; Parwani, P.; Mohamed, M.O.; et al. Trends of Sex Differences in Clinical Outcomes After Myocardial Infarction in the United States. CJC Open 2021, 3, S19–S27. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Curzen, N.; Kinnaird, T.; Lawson, C.A.; Myint, P.K.; Kontopantelis, E.; Mohamed, M.O.; Shoaib, A.; Gale, C.P.; Timmis, A.; et al. Baseline risk, timing of invasive strategy and guideline compliance in NSTEMI: Nationwide analysis from MINAP. Int. J. Cardiol. 2020, 301, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Worrall-Carter, L.; McEvedy, S.; Wilson, A.; Rahman, M.A. Gender Differences in Presentation, Coronary Intervention, and Outcomes of 28,985 Acute Coronary Syndrome Patients in Victoria, Australia. Women’s Health Issues 2016, 26, 14–20. [Google Scholar] [CrossRef] [Green Version]
- ten Haaf, M.E.; Bax, M.; ten Berg, J.M.; Brouwer, J.; van’t Hof, A.W.; van der Schaaf, R.J.; Stella, P.R.; Tjon Joe Gin, R.M.; Tonino, P.A.; de Vries, A.G.; et al. Sex differences in characteristics and outcome in acute coronary syndrome patients in the Netherlands. Neth. Heart J. 2019, 27, 263–271. [Google Scholar] [CrossRef] [Green Version]
- Cenko, E.; Yoon, J.; Kedev, S.; Stankovic, G.; Vasiljevic, Z.; Krljanac, G.; Kalpak, O.; Ricci, B.; Milicic, D.; Manfrini, O.; et al. Sex Differences in Outcomes After STEMI: Effect Modification by Treatment Strategy and Age. JAMA Intern. Med. 2018, 178, 632–639. [Google Scholar] [CrossRef]
- Poon, S.; Goodman, S.G.; Yan, R.T.; Bugiardini, R.; Bierman, A.S.; Eagle, K.A.; Johnston, N.; Huynh, T.; Grondin, F.R.; Schenck-Gustafsson, K.; et al. Bridging the gender gap: Insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am. Heart J. 2012, 163, 66–73. [Google Scholar] [CrossRef]
- Yao, H.; Ekou, A.; Niamkey, T.; Gan, S.H.; Kouamé, I.; Afassinou, Y.; Ehouman, E.; Touré, C.; Zeller, M.; Cottin, Y.; et al. Acute Coronary Syndromes in Sub-Saharan Africa: A 10-Year Systematic Review. J. Am. Heart Assoc. 2022, 11, e021107. [Google Scholar] [CrossRef]
- Yuyun, M.F.; Sliwa, K.; Kengne, A.P.; Mocumbi, A.O.; Bukhman, G. Cardiovascular Diseases in Sub-Saharan Africa Compared to High-Income Countries: An Epidemiological Perspective. Glob. Heart 2020, 15, 15. [Google Scholar] [CrossRef] [Green Version]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics—2022 Update: A Report from the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef]
- Pagidipati, N.J.; Huffman, M.D.; Jeemon, P.; Gupta, R.; Negi, P.; Jaison, T.M.; Sharma, S.; Sinha, N.; Mohanan, P.; Muralidhara, B.G.; et al. Association between Gender, Process of Care Measures, and Outcomes in ACS in India: Results from the Detection and Management of Coronary Heart Disease (DEMAT) Registry. PLoS ONE 2013, 8, e62061. [Google Scholar] [CrossRef]
- Khraishah, H.; Alahmad, B.; Alfaddagh, A.; Jeong, S.Y.; Mathenge, N.; Kassab, M.B.; Kolte, D.; Michos, E.D.; Albaghdadi, M. Sex disparities in the presentation, management and outcomes of patients with acute coronary syndrome: Insights from the ACS QUIK trial. Open Heart 2021, 8, e001470. [Google Scholar] [CrossRef]
- Leurent, G.; Garlantézec, R.; Auffret, V.; Hacot, J.P.; Coudert, I.; Filippi, E.; Rialan, A.; Moquet, B.; Rouault, G.; Gilard, M.; et al. Gender differences in presentation, management and inhospital outcome in patients with ST-segment elevation myocardial infarction: Data from 5000 patients included in the ORBI prospective French regional registry. Arch. Cardiovasc. Dis. 2014, 107, 291–298. [Google Scholar] [CrossRef]
- Lu, H.T.; Nordin, R.; Ahmad, W.A.W.; Lee, C.Y.; Zambahari, R.; Ismail, O.; Liew, H.B.; Sim, K.H. NCVD Investigators Sex differences in acute coronary syndrome in a multiethnic asian population: Results of the malaysian national cardiovascular disease database-acute coronary syndrome (NCVD-ACS) registry. Glob. Heart 2014, 9, 381–390. [Google Scholar] [CrossRef]
- Bugiardini, R.; Badimon, L.; ISACS-TC Investigators and Coordinators. The International Survey of Acute Coronary Syndromes in Transitional Countries (ISACS-TC): 2010–2015. Int. J. Cardiol. 2016, 217, S1–S6. [Google Scholar] [CrossRef]
- Shehab, A.; Al-Dabbagh, B.; AlHabib, K.F.; Alsheikh-Ali, A.A.; Almahmeed, W.; Sulaiman, K.; Al-Motarreb, A.; Nagelkerke, N.; Al Suwaidi, J.; Hersi, A.; et al. Gender Disparities in the Presentation, Management and Outcomes of Acute Coronary Syndrome Patients: Data from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2). PLoS ONE 2013, 8, e55508. [Google Scholar] [CrossRef] [Green Version]
- Kinsara, A.J.; Ismail, Y.M. Gender differences in patients presenting with non-ST segment elevation myocardial infarction in the STAR registry. Egypt. Heart J. Off. Bull. Egypt. Soc. Cardiol. 2021, 73, 54. [Google Scholar] [CrossRef]
- Cader, F.A.; Haq, M.M.; Nasrin, S.; Kabir, C.S. Presentation, Management Practices and In-hospital Outcomes of Patients with Acute Coronary Syndrome in a Tertiary Cardiac Centre in Bangladesh. Bangladesh Heart J. 2017, 32, 106–113. [Google Scholar] [CrossRef] [Green Version]
- Hersi, A.; Al-Habib, K.; Al-Faleh, H.; Al-Nemer, K.; AlSaif, S.; Taraben, A.; Kashour, T.; Abuosa, A.M.; Al-Murayeh, M.A. Gender inequality in the clinical outcomes of equally treated acute coronary syndrome patients in Saudi Arabia. Ann. Saudi Med. 2013, 33, 339–346. [Google Scholar] [CrossRef] [Green Version]
- Chandrasekhar, J.; Mehran, R. Sex-Based Differences in Acute Coronary Syndromes: Insights from Invasive and Noninvasive Coronary Technologies. JACC Cardiovasc. Imaging 2016, 9, 451–464. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Oertelt-Prigione, S.; Prescott, E.; Franconi, F.; Gerdts, E.; Foryst-Ludwig, A.; Maas, A.H.; Kautzky-Willer, A.; Knappe-Wegner, D.; Kintscher, U.; et al. Gender in cardiovascular diseases: Impact on clinical manifestations, management, and outcomes. Eur. Heart J. 2016, 37, 24–34. [Google Scholar] [PubMed] [Green Version]
- Stähli, B.E.; Gebhard, C.; Yonekawa, K.; Gebhard, C.E.; Altwegg, L.A.; Von Eckardstein, A.; Hersberger, M.; Novopashenny, I.; Wolters, R.; Wischnewsky, M.B.; et al. Gender-Related Differences in Patients Presenting with Suspected Acute Coronary Syndromes: Clinical Presentation, Biomarkers and Diagnosis. Cardiology 2015, 132, 189–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansson, I.; Strömberg, A.; Swahn, E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung 2004, 33, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Diercks, D.B.; Owen, K.P.; Kontos, M.C.; Blomkalns, A.; Chen, A.Y.; Miller, C.; Wibiott, S.; Peterson, E.D. Gender differences in time to presentation for myocardial infarction before and after a national women’s cardiovascular awareness campaign: A temporal analysis from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress ADverse Outcomes with Early Implementation (CRUSADE) and the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network-Get with the Guidelines (NCDR ACTION Registry-GWTG). Am. Heart J. 2010, 160, e014733. [Google Scholar] [CrossRef]
- Thuresson, M.; Jarlöv, M.B.; Lindahl, B.; Svensson, L.; Zedigh, C.; Herlitz, J. Symptoms and type of symptom onset in acute coronary syndrome in relation to ST elevation, sex, age, and a history of diabetes. Am. Heart J. 2005, 150, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Canto, J.G.; Goldberg, R.J.; Hand, M.M.; Bonow, R.O.; Sopko, G.; Pepine, C.J.; Long, T. Symptom presentation of women with acute coronary syndromes: Myth vs reality. Arch. Intern. Med. 2007, 167, 2405–2413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McSweeney, J.C.; Cleves, M.A.; Fischer, E.P.; Rojo, M.O.; Armbya, N.; Moser, D.K. Reliability of the McSweeney Acute and Prodromal Myocardial Infarction Symptom Survey among black and white women. Eur. J. Cardiovasc. Nurs. 2013, 12, 360–367. [Google Scholar] [CrossRef]
- Wouters, L.T.C.M.; Zwart, D.L.M.; Erkelens, D.C.A.; De Groot, E.; Van Smeden, M.; Hoes, A.W.; Damoiseaux, R.A.M.J.; Rutten, F.H. Gender-stratified analyses of symptoms associated with acute coronary syndrome in telephone triage: A cross-sectional study. BMJ Open 2021, 11, e042406. [Google Scholar] [CrossRef]
- Khan, N.A.; Daskalopoulou, S.S.; Karp, I.; Eisenberg, M.J.; Pelletier, R.; Tsadok, M.A.; Dasgupta, K.; Norris, C.M.; Pilote, L.; GENESIS PRAXY Team. Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern. Med. 2013, 173, 1863–1871. [Google Scholar] [CrossRef]
- Ferry, A.V.; Anand, A.; Strachan, F.E.; Mooney, L.; Stewart, S.D.; Marshall, L.; Chapman, A.R.; Lee, K.K.; Jones, S.; Orme, K.; et al. Presenting Symptoms in Men and Women Diagnosed with Myocardial Infarction Using Sex-Specific Criteria. J. Am. Heart Assoc. 2019, 8, e012307. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Leifheit, E.C.; Safdar, B.; Bao, H.; Krumholz, H.M.; Lorenze, N.P.; Daneshvar, M.; Spertus, J.A.; D’Onofrio, G. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction. Circulation 2018, 137, 781–790. [Google Scholar] [CrossRef]
- Writing Committee Members; Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 78, 2218–2261. [Google Scholar]
- Elder, P.; Sharma, G.; Gulati, M.; Michos, E.D. Identification of female-specific risk enhancers throughout the lifespan of women to improve cardiovascular disease prevention. Am. J. Prev. Cardiol. 2020, 2, 100028. [Google Scholar] [CrossRef]
- The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators. A Clinical Trial Comparing Primary Coronary Angioplasty with Tissue Plasminogen Activator for Acute Myocardial Infarction. N. Engl. J. Med. 1997, 336, 1621–1628. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, A.; Doshi, S. The role of oxidative stress in menopause. J. Midlife Health 2013, 4, 140. [Google Scholar] [CrossRef]
- Worrall-Carter, L.; McEvedy, S.; Wilson, A.; Rahman, M.A. Impact of comorbidities and gender on the use of coronary interventions in patients with high-risk non-ST-segment elevation acute coronary syndrome. Catheter. Cardiovasc. Interv. 2016, 87, E128–E136. [Google Scholar] [CrossRef]
- Dreyer, R.P.; Smolderen, K.G.; Strait, K.M.; Beltrame, J.F.; Lichtman, J.H.; Lorenze, N.P.; D’Onofrio, G.; Bueno, H.; Krumholz, H.M.; Spertus, J.A. Gender differences in pre-event health status of young patients with acute myocardial infarction: A VIRGO study analysis. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 43–54. [Google Scholar] [CrossRef] [Green Version]
- Yusuf, P.S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the Interheart study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Njølstad, I.; Arnesen, E.; Lund-Larsen, P.G. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction: A 12-year follow-up of the Finnmark Study. Circulation 1996, 93, 450–456. [Google Scholar] [CrossRef]
- Banerjee, A.; Silver, L.E.; Heneghan, C.; Welch, S.J.V.; Bull, L.M.; Mehta, Z.; Banning, A.P.; Rothwell, P.M. Sex-specific familial clustering of myocardial infarction in patients with acute coronary syndromes. Circ. Cardiovasc. Genet. 2009, 2, 98–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bucholz, E.M.; Strait, K.M.; Dreyer, R.P.; Lindau, S.T.; D’Onofrio, G.; Geda, M.; Spatz, E.S.; Beltrame, J.F.; Lichtman, J.H.; Lorenze, N.P.; et al. Sex Differences in Young Patients with Acute Myocardial Infarction: A VIRGO Study Analysis. Eur. Heart J. Acute Cardiovasc. Care 2017, 6, 610–622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Backholer, K.; Peters, S.A.E.; Bots, S.H.; Peeters, A.; Huxley, R.R.; Woodward, M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: A systematic review and meta-analysis. J. Epidemiol. Community Health 2017, 71, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Forrester, S.; Jacobs, D.; Zmora, R.; Schreiner, P.; Roger, V.; Kiefe, C.I. Racial differences in weathering and its associations with psychosocial stress: The CARDIA study. SSM Popul. Health 2019, 7, 100319. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, E1082–E1143. [Google Scholar]
- Wu, P.; Park, K.; Gulati, M. The fourth trimester: Pregnancy as a predictor of cardiovascular disease. Eur. Cardiol. Rev. 2021, 16, e31. [Google Scholar] [CrossRef]
- Grandi, S.M.; Filion, K.B.; Yoon, S.; Ayele, H.T.; Doyle, C.M.; Hutcheon, J.A.; Smith, G.N.; Gore, G.C.; Ray, J.G.; Nerenberg, K.; et al. Cardiovascular Disease-Related Morbidity and Mortality in Women with a History of Pregnancy Complications. Circulation 2019, 139, 1069–1079. [Google Scholar] [CrossRef]
- Tanz, L.J.; Stuart, J.J.; Williams, P.L.; Rimm, E.B.; Missmer, S.A.; Rexrode, K.M.; Mukamal, K.J.; Rich-Edwards, J.W. Preterm Delivery and Maternal Cardiovascular Disease in Young and Middle-Aged Adult Women. Circulation 2017, 135, 578–589. [Google Scholar] [CrossRef] [Green Version]
- Kramer, C.K.; Campbell, S.; Retnakaran, R. Gestational diabetes and the risk of cardiovascular disease in women: A systematic review and meta-analysis. Diabetologia 2019, 62, 905–914. [Google Scholar] [CrossRef] [Green Version]
- McKenzie-Sampson, S.; Paradis, G.; Healy-Profitós, J.; St-Pierre, F.; Auger, N. Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: A retrospective cohort study. Acta Diabetol. 2018, 55, 315–322. [Google Scholar] [CrossRef]
- Markovitz, A.R.; Stuart, J.J.; Horn, J.; Williams, P.L.; Rimm, E.B.; Missmer, S.A.; Tanz, L.J.; Haug, E.B.; Fraser, A.; Timpka, S.; et al. Does pregnancy complication history improve cardiovascular disease risk prediction? Findings from the HUNT study in Norway. Eur. Heart J. 2019, 40, 1113–1120. [Google Scholar] [CrossRef]
- Honigberg, M.C.; Zekavat, S.M.; Niroula, A.; Griffin, G.K.; Bick, A.G.; Pirruccello, J.P.; Nakao, T.; Whitsel, E.A.; Farland, L.V.; Laurie, C.; et al. Premature Menopause, Clonal Hematopoiesis, and Coronary Artery Disease in Postmenopausal Women. Circulation 2021, 143, 410–423. [Google Scholar] [CrossRef]
- Osibogun, O.; Ogunmoroti, O.; Michos, E.D. Polycystic ovary syndrome and cardiometabolic risk: Opportunities for cardiovascular disease prevention. Trends Cardiovasc. Med. 2020, 30, 399–404. [Google Scholar] [CrossRef]
- Zhao, L.; Zhu, Z.; Lou, H.; Zhu, G.; Huang, W.; Zhang, S.; Liu, F. Polycystic ovary syndrome (PCOS) and the risk of coronary heart disease (CHD): A meta-analysis. Oncotarget 2016, 7, 33715–33721. [Google Scholar] [CrossRef] [Green Version]
- Hiteshi, A.K.; Li, D.; Gao, Y.; Chen, A.; Flores, F.; Mao, S.S.; Budoff, M.J. Gender differences in coronary artery diameter are not related to body habitus or left ventricular mass. Clin. Cardiol. 2014, 37, 605–609. [Google Scholar] [CrossRef]
- Murthy, V.L.; Naya, M.; Taqueti, V.R.; Foster, C.R.; Gaber, M.; Hainer, J.; Dorbala, S.; Blankstein, R.; Rimoldi, O.; Camici, P.G.; et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 2014, 129, 2518–2527. [Google Scholar] [CrossRef] [Green Version]
- Patel, M.B.; Bui, L.P.; Kirkeeide, R.L.; Gould, K.L. Imaging Microvascular Dysfunction and Mechanisms for Female-Male Differences in CAD. JACC Cardiovasc. Imaging 2016, 9, 465–482. [Google Scholar] [CrossRef]
- Ong, P.; Camici, P.G.; Beltrame, J.F.; Crea, F.; Shimokawa, H.; Sechtem, U.; Kaski, J.C.; Bairey Merz, C.N.; Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for microvascular angina. Int. J. Cardiol. 2018, 250, 16–20. [Google Scholar] [CrossRef]
- Scalone, G.; Niccoli, G.; Crea, F. Editor’s Choice- Pathophysiology, diagnosis and management of MINOCA: An update. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 54–62. [Google Scholar] [CrossRef]
- Pelliccia, F.; Pepine, C.J.; Berry, C.; Camici, P.G. The role of a comprehensive two-step diagnostic evaluation to unravel the pathophysiology of MINOCA: A review. Int. J. Cardiol. 2021, 336, 1–7. [Google Scholar] [CrossRef]
- Ouldzein, H.; Elbaz, M.; Roncalli, J.; Cagnac, R.; Carrié, D.; Puel, J.; Alibelli-Chemarin, M.J. Plaque rupture and morphological characteristics of the culprit lesion in acute coronary syndromes without significant angiographic lesion: Analysis by intravascular ultrasound. Ann. Cardiol. Angeiol. 2012, 61, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.R.; Srichai, M.B.; Iqbal, S.N.; Slater, J.N.; Mancini, G.B.J.; Feit, F.; Pena-Sing, I.; Axel, L.; Attubato, M.J.; Yatskar, L.; et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation 2011, 124, 1414–1425. [Google Scholar] [CrossRef] [PubMed]
- White, S.J.; Newby, A.C.; Johnson, T.W. Endothelial erosion of plaques as a substrate for coronary thrombosis. Thromb. Haemost. 2016, 115, 509–519. [Google Scholar] [PubMed]
- Perera, D.; Berry, C.; Hoole, S.P.; Sinha, A.; Rahman, H.; Morris, P.D.; Kharbanda, R.K.; Petraco, R.; Channon, K. Invasive coronary physiology in patients with angina and non-obstructive coronary artery disease: A consensus document from the coronary microvascular dysfunction workstream of the British Heart Foundation/National Institute for Health Research Partnership. Heart 2022. [Google Scholar] [CrossRef]
- Nishiguchi, T.; Tanaka, A.; Ozaki, Y.; Taruya, A.; Fukuda, S.; Taguchi, H.; Iwaguro, T.; Ueno, S.; Okumoto, Y.; Akasaka, T. Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 263–270. [Google Scholar] [CrossRef]
- Saw, J.; Aymong, E.; Sedlak, T.; Buller, C.E.; Starovoytov, A.; Ricci, D.; Robinson, S.; Vuurmans, T.; Gao, M.; Humphries, K.; et al. Spontaneous coronary artery dissection: Association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ. Cardiovasc. Interv. 2014, 7, 645–655. [Google Scholar] [CrossRef] [Green Version]
- Tweet, M.S.; Hayes, S.N.; Pitta, S.R.; Simari, R.D.; Lerman, A.; Lennon, R.J.; Gersh, B.J.; Khambatta, S.; Best, P.J.; Rihal, C.S.; et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012, 126, 579–588. [Google Scholar] [CrossRef] [Green Version]
- Pasupathy, S.; Air, T.; Dreyer, R.P.; Tavella, R.; Beltrame, J.F. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation 2015, 131, 861–870. [Google Scholar] [CrossRef] [Green Version]
- Crump, R.; Shandling, A.H.; Van Natta, B.; Ellestad, M. Prevalence of patent foramen ovale in patients with acute myocardial infarction and angiographically normal coronary arteries. Am. J. Cardiol. 2000, 85, 1368–1370. [Google Scholar] [CrossRef]
- Sastry, S.; Riding, G.; Morris, J.; Taberner, D.; Cherry, N.; Heagerty, A.; McCollum, C. Young Adult Myocardial Infarction and Ischemic Stroke: The role of paradoxical embolism and thrombophilia (The YAMIS Study). J. Am. Coll. Cardiol. 2006, 48, 686–691. [Google Scholar] [CrossRef] [Green Version]
- Sykes, R.; Doherty, D.; Mangion, K.; Morrow, A.; Berry, C. What an interventionalist needs to know about MI with non-obstructive coronary arteries. Interv. Cardiol. Rev. 2021, 16, e10. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar]
- Tamis-Holland, J.E.; Jneid, H.; Reynolds, H.R.; Agewall, S.; Brilakis, E.S.; Brown, T.M.; Lerman, A.; Cushman, M.; Kumbhani, D.J.; Arslanian-Engoren, C.; et al. Contemporary Diagnosis and Management of Patients with Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement from the American Heart Association. Circulation 2019, 139, E891–E908. [Google Scholar] [CrossRef]
- Ghadri, J.R.; Wittstein, I.S.; Prasad, A.; Sharkey, S.; Dote, K.; Akashi, Y.J.; Cammann, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018, 39, 2032–2046. [Google Scholar] [CrossRef] [Green Version]
- Galiuto, L.; De Caterina, A.R.; Porfidia, A.; Paraggio, L.; Barchetta, S.; Locorotondo, G.; Rebuzzi, A.G.; Crea, F. Reversible coronary microvascular dysfunction: A common pathogenetic mechanism in Apical Ballooning or Tako-Tsubo Syndrome. Eur. Heart J. 2010, 31, 1319–1327. [Google Scholar] [CrossRef] [Green Version]
- Gulati, M. Yentl’s Bikini: Sex Differences in STEMI. J. Am. Heart Assoc. 2019, 8, e012873. [Google Scholar] [CrossRef]
- Sulaiman, S.; Kawsara, A.; Mohamed, M.O.; Van Spall, H.G.C.; Sutton, N.; Holmes, D.R.; Mamas, M.A.; Alkhouli, M. Treatment Effect of Percutaneous Coronary Intervention in Men Versus Women With ST-Segment-Elevation Myocardial Infarction. J. Am. Heart Assoc. 2021, 10, e021638. [Google Scholar] [CrossRef]
- Lee, C.Y.; Ting, K.L.; Lu, H.T.; Ali, R.M.; Fong, A.Y.Y.; Wan Ahmad, W.A. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry. PLoS ONE 2021, 16, e0246474. [Google Scholar] [CrossRef]
- Hao, Y.; Liu, J.; Liu, J.; Yang, N.; Smith, S.C.; Huo, Y.; Fonarow, G.C.; Ge, J.; Taubert, K.A.; Morgan, L.; et al. Sex Differences in In-Hospital Management and Outcomes of Patients with Acute Coronary Syndrome. Circulation 2019, 139, 1776–1785. [Google Scholar] [CrossRef]
- Edmund Anstey, D.; Li, S.; Thomas, L.; Wang, T.Y.; Wiviott, S.D. Race and Sex Differences in Management and Outcomes of Patients After ST-Elevation and Non-ST-Elevation Myocardial Infarct: Results From the NCDR. Clin. Cardiol. 2016, 39, 585–595. [Google Scholar] [CrossRef] [Green Version]
- Udell, J.A.; Fonarow, G.C.; Maddox, T.M.; Cannon, C.P.; Frank Peacock, W.; Laskey, W.K.; Grau-Sepulveda, M.V.; Smith, E.E.; Hernandez, A.F.; Peterson, E.D.; et al. Sustained sex-based treatment differences in acute coronary syndrome care: Insights from the American Heart Association Get with The Guidelines Coronary Artery Disease Registry. Clin. Cardiol. 2018, 41, 758–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, S.A.E.; Colantonio, L.D.; Zhao, H.; Bittner, V.; Dai, Y.; Farkouh, M.E.; Monda, K.L.; Safford, M.M.; Muntner, P.; Woodward, M. Sex Differences in High-Intensity Statin Use Following Myocardial Infarction in the United States. J. Am. Coll. Cardiol. 2018, 71, 1729–1737. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, G.; Safdar, B.; Lichtman, J.H.; Strait, K.M.; Dreyer, R.P.; Geda, M.; Spertus, J.A.; Krumholz, H.M. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: Results from the VIRGO study. Circulation 2015, 131, 1324–1332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, S.; Stouffer, G.A.; Kucharska-Newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Porterfield, D.; Blankstein, R.; Rosamond, W.D.; Bhatt, D.L.; et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation 2019, 139, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Huded, C.P.; Kumar, A.; Johnson, M.; Abdallah, M.; Ballout, J.A.; Kravitz, K.; Menon, V.; Gullett, T.C.; Hantz, S.; Ellis, S.G.; et al. Incremental prognostic value of guideline-directed medical therapy, transradial access, and door-to-balloon time on outcomes in ST-segment-elevation myocardial infarction. Circ. Cardiovasc. Interv. 2019, 12, e007101. [Google Scholar] [CrossRef] [PubMed]
- Shah, T.; Haimi, I.; Yang, Y.; Gaston, S.; Taoutel, R.; Mehta, S.; Lee, H.J.; Zambahari, R.; Baumbach, A.; Henry, T.D.; et al. Meta-Analysis of Gender Disparities in In-hospital Care and Outcomes in Patients with ST-Segment Elevation Myocardial Infarction. Am. J. Cardiol. 2021, 147, 23–32. [Google Scholar] [CrossRef]
- Stehli, J.; Martin, C.; Brennan, A.; Dinh, D.T.; Lefkovits, J.; Zaman, S. Sex Differences Persist in Time to Presentation, Revascularization, and Mortality in Myocardial Infarction Treated with Percutaneous Coronary Intervention. J. Am. Heart Assoc. 2019, 8, e012161. [Google Scholar] [CrossRef] [Green Version]
- WHO. Alphabetical List of WHO Member States. Available online: https://www.who.int/countries (accessed on 15 June 2022).
- Isezuo, S.; Sani, M.U.; Talle, A.; Johnson, A.; Adeoye, A.M.; Ulgen, M.S.; Mbakwem, A.; Ogah, O.; Edafe, E.; Kolo, P.; et al. Registry for Acute Coronary Events in Nigeria (RACE-Nigeria): Clinical Characterization, Management, and Outcome. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2022, 11, 20244. [Google Scholar] [CrossRef]
- Maurin, O.; Massoure, P.L.; De, R.S.; Topin, F.; Sbardella, F.; Lamblin, G.; Kaiser, E. Acute myocardial infarction in Djibouti: 2-year prospective study. Med. Sante Trop. 2012, 22, 297–301. [Google Scholar] [CrossRef]
- Mboup, M.C.; Mingou, J.; Ba, D.M.; Dia, K.; Fall, P.D. Characteristics of acute coronary syndromes in Sub-Saharan African women. Ann. Cardiol. Angeiol. 2019, 68, 115–119. [Google Scholar] [CrossRef]
- Marie, D.; Mingou, J.S.; Dia, K.; Gbadamassi, S.E.O.K.; Fall, P.D.; Diao, M.; Mboup, M.C. Clinical Presentation, Risk Factor, and Outcomes of Acute Coronary Syndrome in Women at an Urban Referral Center in Dakar, Senegal. Glob. Heart 2019, 14, 35–39. [Google Scholar] [CrossRef]
- Mirghani, H.O.; Elnour, M.A.; Taha, A.M.; Elbadawi, A.S. Gender inequality in acute coronary syndrome patients at Omdurman Teaching Hospital, Sudan. J. Family Community Med. 2016, 23, 100–104. [Google Scholar]
- Yao, H.; Ekou, A.; Hadéou, A.; N’Djessan, J.J.; Kouamé, I.; N’Guetta, R. Medium and long-term follow-up after ST-segment elevation myocardial infarction in a sub-Saharan Africa population: A prospective cohort study. BMC Cardiovasc. Disord. 2019, 19, 65. [Google Scholar] [CrossRef] [Green Version]
- Bazzino, O.; Monaco, R.; Mario, B.; Sergio, C.; Valeria, C.M.; Sergio, E.; Ricardo, E.; Juan, G.; Ernesto, J.; Carlos, K.; et al. Management of acute coronary syndromes in developing countries: Acute coronary events-a multinational survey of current management strategies. Am. Heart J. 2011, 162, 852–859.e22. [Google Scholar]
- Shehab, A.; Bhagavathula, A.S.; Alhabib, K.F.; Ullah, A.; Suwaidi, J.A.; Almahmeed, W.; AlFaleh, H.; Zubaid, M. Age-Related Sex Differences in Clinical Presentation, Management, and Outcomes in ST-Segment–Elevation Myocardial Infarction: Pooled Analysis of 15 532 Patients From 7 Arabian Gulf Registries. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2020, 9, e013880. [Google Scholar] [CrossRef]
- El-Menyar, A.; Zubaid, M.; Sulaiman, K.; AlMahmeed, W.; Singh, R.; Alsheikh-Ali, A.A.; Al Suwaidi, J.; Gulf Registry of Acute Coronary Events (Gulf RACE) Investigators. Atypical presentation of acute coronary syndrome: A significant independent predictor of in-hospital mortality. J. Cardiol. 2011, 57, 165–171. [Google Scholar] [CrossRef] [Green Version]
- Reda, A.; Ashraf, M.; Soliman, M.; Ragy, H.; Elkersh, A.; Abdou, W.; Mostafa, T.; Hassan, M.; Farag, E.; Khamis, H.; et al. Gender-related Differences in Risk factors and Treatment Strategies in Patients with Acute Coronary Syndrome across Egypt: Part of the Cardio- Risk Project. Atheroscler. Suppl. 2018, 33, e2. [Google Scholar] [CrossRef]
- Altaf, A.; Shah, H.; Salahuddin, M. Gender based differences in clinical and Angiographic characteristics and outcomes of Acute Coronary Syndrome (ACS) in Asian population. Pakistan J. Med. Sci. 2019, 35, 1349–1354. [Google Scholar] [CrossRef] [Green Version]
- Reda, A.; Soliman, M.; El Kersh, A.; Abdou, W.; Mostafa, M.; Beshay, M.; Gamal, A.; Farag, E.; Mostafa, T.; El-Ghany, M.A.; et al. The pattern of risk-factor profile in Egyptian patients with acute coronary syndrome: Phase II of the Egyptian cross-sectional CardioRisk project. Cardiovasc. J. Afr. 2019, 30, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Sriha Belguith, A.; Beltaief, K.; Msolli, M.A.; Bouida, W.; Abroug, H.; Ben Fredj, M.; Zemni, I.; Grissa, M.H.; Boubaker, H.; Hsairi, M.; et al. Management of acute coronary syndrome in emergency departments: A cross sectional multicenter study (Tunisia) 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Emerg. Med. 2018, 18, 50. [Google Scholar] [CrossRef] [Green Version]
- Abbasi, S.H.; Ponce de Leon, A.; Kassaian, S.E.; Karimi, A.A.; Sundin, Ö.; Soares, J.; Macassa, G. Gender Differences in the Risk of Coronary Artery Disease in Iran. Iran. J. Public Health 2012, 41, 36. [Google Scholar] [PubMed]
- Joshi, P.; Islam, S.; Pais, P.; Reddy, S.; Dorairaj, P.; Kazmi, K.; Pandey, M.R.; Haque, S.; Mendis, S.; Rangarajan, S.; et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. J. Am. Med. Assoc. 2007, 297, 286–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allana, S.; Khowaja, K.; Ali, T.S.; Moser, D.K.; Khan, A.H. Gender Differences in Factors Associated with Prehospital Delay Among Acute Coronary Syndrome Patients in Pakistan. J. Transcult. Nurs. 2015, 26, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Gender Differences in Presentation, Management and Outcomes among Patients with Acute Coronary Syndrome in Dhaka, Bangladesh. Available online: tctmd.com (accessed on 15 June 2022).
- Xavier, D.; Pais, P.; Devereaux, P.; Xie, C.; Prabhakaran, D.; Reddy, K.S.; Gupta, R.; Joshi, P.; Kerkar, P.; Thanikachalam, S.; et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet 2008, 371, 1435–1442. [Google Scholar] [CrossRef]
- Sigamani, A.; Kamath, D.; Xavier, D.; Pais, P. New evidence for gender disparities in cardiac interventions: CREATE-ing some clarity [Internet]. Interv. Cardiol. 2013, 5, 1–4. [Google Scholar] [CrossRef]
- Patel, A.; Vishwanathan, S.; Nair, T.; Bahuleyan, C.G.; Jayaprakash, V.L.; Baldridge, A.; Huffman, M.D.; Prabhakaran, D.; Mohanan, P.P. Sex Differences in the Presentation, Diagnosis, and Management of Acute Coronary Syndromes: Findings from the Kerala-India ACS Registry. Glob. Heart 2015, 10, 273–280. [Google Scholar] [CrossRef] [Green Version]
- Cader, F.A.; Rahman, A.; Ullah, M.; Rahman, M.A.; Alam, M.S.; Nasrin, S.; Momen, A.; Kundu, S.K.; Chakraborty, S.; Bala, P. Gender Differences in Clinical, Angiographic and Procedural Profiles between Young Patients with Acute Coronary Syndrome undergoing Percutaneous Coronary Intervention. Cardiovasc. J. 2018, 10, 113–120. [Google Scholar] [CrossRef]
- Cader, F.A.; Rahman, A.; Rahman, M.A.; Zaman, S.; Arefin, M.; Reza, A.; Matin, M.A.; Afroz, F.; Hasnat, A.; Jafor, M.; et al. Comparison of Short-term Outcomes of Percutaneous Coronary Intervention between Young Male and Female Patients with Acute Coronary Syndrome. Bangladesh Heart J. 2018, 33, 1–9. [Google Scholar] [CrossRef]
- Galappatthy, P.; Bataduwaarachchi, V.; Ranasinghe, P.; Galappatthy, G.; Senerath, U.; Wijeyaratne, C.; Ekanayake, R. Sex Difference in Risk Factors, GRACE Scores, and Management among Post-Acute Coronary Syndrome Patients in Sri Lanka. Cardiol. Res. Pract. 2020, 2020, 4560218. [Google Scholar] [CrossRef]
- Srichaiveth, B.; Ruengsakulrach, P.; Visudharom, K.; Sanguanwong, S.; Tangsubutr, W.; Insamian, P. Impact of gender on treatment and clinical outcomes in acute ST elevation myocardial infarction patients in Thailand. J. Med. Assoc. Thail. 2007, 90, 65–73. [Google Scholar]
- Suttirut, P.; Panthong, S.; Kittipibul, V.; Lertsuwunseri, V.; Srimahachota, S.; Ariyachaipanich, A. Impact of Gender on Outcomes Among Patients with Acute Coronary Syndrome Undergoing Primary Percutaneous Coronary Intervention in Southeast Asia. J. Am. Coll. Cardiol. 2017, 69, 2540. [Google Scholar] [CrossRef]
- Sella, Y.O.; Manistamara, H.; Apriliawan, S.; Lukitasari, M.; Rohman, M.S. Characteristic differences of chest pain in male and female patients with acute coronary syndrome: A pilot study. J. Public Health Res. 2021, 10, 2242. [Google Scholar] [CrossRef]
- Bachelet, B.C.; Hyun, K.; D’Souza, M.; Chow, C.K.; Redfern, J.; Brieger, D.B. Sex differences in the management and outcomes of non-ST-elevation acute coronary syndromes. Med. J. Aust. 2022, 216, 153–155. [Google Scholar] [CrossRef]
- Worrall-Carter, L.; MacIsaac, A.; Scruth, E.; Rahman, M.A. Gender difference in the use of coronary interventions for patients with acute coronary syndrome: Experience from a major metropolitan hospital in Melbourne, Australia. Aust. Crit. Care 2017, 30, 3–10. [Google Scholar] [CrossRef]
- Kam, R.; Cutter, J.; Chew, S.K.; Tan, A.; Emmanuel, S.; Mak, K.H.; Chan, C.N.S.; Koh, T.H.; Lim, Y.L. Gender differences in outcome after an acute myocardial infarction in Singapore. Singap. Med. J. 2002, 43, 243–248. [Google Scholar]
- Levy, M.; Chen, Y.; Clarke, R.; Guo, Y.; Lv, J.; Yu, C.; Li, L.; Chen, Z.; Mihaylova, B. Gender differences in use of invasive diagnostic and therapeutic procedures for acute ischaemic heart disease in Chinese adults. Heart 2022, 108, 292–299. [Google Scholar] [CrossRef]
- Hong, J.S.; Kang, H.C. Sex Differences in the Treatment and Outcome of Korean Patients with Acute Myocardial Infarction Using the Korean National Health Insurance Claims Database. Medicine 2015, 94, e1401. [Google Scholar] [CrossRef]
- Kawano, H.; Soejima, H.; Kojima, S.; Kitagawa, A.; Ogawa, H. Sex differences of risk factors for acute myocardial infarction in Japanese patients. Circ. J. 2006, 70, 513–517. [Google Scholar] [CrossRef] [Green Version]
- Kosuge, M.; Kimura, K.; Kojima, S.; Sakamoto, T.; Ishihara, M.; Asada, Y.; Tei, C.; Miyazaki, S.; Sonoda, M.; Tsuchihashi, K.; et al. Sex Differences in Early Mortality of Patients Undergoing Primary Stenting for Acute Myocardial Infarction. Circ. J. 2006, 70, 217–221. [Google Scholar] [CrossRef]
- Vaccarino, V.; Parsons, L.; Peterson, E.D.; Rogers, W.J.; Kiefe, C.I.; Canto, J. Sex differences in mortality after acute myocardial infarction: Changes from 1994 to 2006. Arch. Intern. Med. 2009, 169, 1767–1774. [Google Scholar] [CrossRef] [Green Version]
- Yan, A.T.; Yan, R.T.; Tan, M.; Fung, A.; Cohen, E.A.; Fitchett, D.H.; Langer, A.; Goodman, S.G. Management patterns in relation to risk stratification among patients with non-ST elevation acute coronary syndromes. Arch. Intern. Med. 2007, 167, 1009–1016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chest Pain MI Registry. Available online: https://cvquality.acc.org/NCDR-Home/registries/hospital-registries/chest-pain-mi-registry#:~:text=The%20Chest%20Pain%20%2D%20MI%20Registry%20offers%20a%20wealth%20of%20reporting,performance%20measures%20and%20quality%20metrics (accessed on 15 June 2022).
- Get with The Guidelines®–Coronary Artery Disease|American Heart Association. Available online: https://www.heart.org/en/professional/quality-improvement/get-with-the-guidelines/get-with-the-guidelines-coronary-artery-disease (accessed on 15 June 2022).
- Peterson, E.D.; Lansky, A.J.; Kramer, J.; Anstrom, K.; Lanzilotta, M.J. Effect of gender on the outcomes of contemporary percutaneous coronary intervention. Am. J. Cardiol. 2001, 88, 359–364. [Google Scholar] [CrossRef]
- Akhter, N.; Milford-Beland, S.; Roe, M.T.; Piana, R.N.; Kao, J.; Shroff, A. Gender differences among patients with acute coronary syndromes undergoing percutaneous coronary intervention in the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Am. Heart J. 2009, 157, 141–148. [Google Scholar] [CrossRef] [PubMed]
- de Matos Soeiro, A.; de Barros e Silva, P.G.M.; de Castro Roque, E.A.; Bossa, A.S.; Biselli, B.; de Carvalho Andreucci Torres Leal, T.; de Almeida Soeiro, M.C.F.; Pitta, F.G.; Serrano, C.V.; Oliveira, M.T. Prognostic Differences between Men and Women with Acute Coronary Syndrome. Data from a Brazilian Registry. Arq. Bras. Cardiol. 2018, 111, 648–653. [Google Scholar]
- Mariani, J.A.; Antonietti, L.; Tajer, C.D.; De Abreu, M.; Charask, A.; Silberstein, M.; Gagliardi, J.; Doval, H.C. Diferencias de género en el tratamiento de síndromes coronarios agudos: Resultados del registro Epi-Cardio [Internet]. Rev. Argent. Cardiol. 2013, 81, 307–315. [Google Scholar] [CrossRef]
- Pelletier, R.; Humphries, K.H.; Shimony, A.; Bacon, S.L.; Lavoie, K.L.; Rabi, D.; Karp, I.; Avgil Tsadok, M.; Pilote, L. Sex-related differences in access to care among patients with premature acute coronary syndrome. CMAJ 2014, 186, 497–504. [Google Scholar] [CrossRef] [Green Version]
- Johnston, N.; Bornefalk-Hermansson, A.; Schenck-Gustafsson, K.; Held, C.; Goodman, S.G.; Yan, A.T.; Bierman, A.S. Do clinical factors explain persistent sex disparities in the use of acute reperfusion therapy in STEMI in Sweden and Canada? Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 350–358. [Google Scholar] [CrossRef] [Green Version]
- Quesada, O.; Van Hon, L.; Yildiz, M.; Madan, M.; Sanina, C.; Davidson, L.; Htun, W.W.; Saw, J.; Garcia, S.; Dehghani, P.; et al. Sex Differences in Clinical Characteristics, Management Strategies, and Outcomes of STEMI with COVID-19: NACMI Registry. J. Soc. Cardiovasc. Angiogr. Interv. 2022; 100360, in press. [Google Scholar] [CrossRef]
- Vogel, B.; Farhan, S.; Hahne, S.; Kozanli, I.; Kalla, K.; Freynhofer, M.K.; Jarai, R.; Kautzky-Willer, A.; Huber, K. Sex-related differences in baseline characteristics, management and outcome in patients with acute coronary syndrome without ST-segment elevation. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 347–353. [Google Scholar]
- Leifheit-Limson, E.C.; D’Onofrio, G.; Daneshvar, M.; Geda, M.; Bueno, H.; Spertus, J.A.; Krumholz, H.M.; Lichtman, J.H. Sex Differences in Cardiac Risk Factors, Perceived Risk, and Health Care Provider Discussion of Risk and Risk Modification Among Young Patients with Acute Myocardial Infarction: The VIRGO Study. J. Am. Coll. Cardiol. 2015, 66, 1949–1957. [Google Scholar] [CrossRef] [Green Version]
- Chandrasekhar, J.; Gill, A.; Mehran, R. Acute myocardial infarction in young women: Current perspectives. Int. J. Women’s Health 2018, 10, 267–284. [Google Scholar] [CrossRef] [Green Version]
- Ya’qoub, L.; Lemor, A.; Dabbagh, M.; O’Neill, W.; Khandelwal, A.; Martinez, S.C.; Ibrahim, N.E.; Grines, C.; Voeltz, M.; Basir, M.B. Racial, Ethnic, and Sex Disparities in Patients with STEMI and Cardiogenic Shock. JACC Cardiovasc. Interv. 2021, 14, 653–660. [Google Scholar] [CrossRef]
- Ghadri, J.R.; Sarcon, A.; Jaguszewski, M.; Diekmann, J.; Bataiosu, R.D.; Hellermann, J.; Csordas, A.; Baumann, L.; Schöni, A.A.; Lüscher, T.F.; et al. Gender disparities in acute coronary syndrome: A closing gap in the short-term outcome. J. Cardiovasc. Med. 2015, 16, 355–362. [Google Scholar] [CrossRef] [Green Version]
- Neumann, J.T.; Goßling, A.; Sörensen, N.A.; Blankenberg, S.; Magnussen, C.; Westermann, D. Sex-Specific Outcomes in Patients with Acute Coronary Syndrome. J. Clin. Med. 2020, 9, 2124. [Google Scholar] [CrossRef]
- Ruiz-Nodar, J.M.; Ferreiro, J.L.; Ribera, A.; Marsal, J.R.; García Acuña, J.M.; Agra Bermejo, R.; Raposeiras-Roubín, S.; Abu-Assi, E.; Cordero, A.; Bertomeu-González, V.; et al. Sex differences in the management of patients with acute coronary syndrome: A population-based ecological cross-sectional study in Spain. REC CardioClin. 2021, 56, 168–178. [Google Scholar] [CrossRef]
- Isorni, M.A.; Blanchard, D.; Teixeira, N.; Le Breton, H.; Renault, N.; Gilard, M.; Lefèvre, T.; Mulak, G.; Danchin, N.; Spaulding, C.; et al. Impact of gender on use of revascularization in acute coronary syndromes: The national observational study of diagnostic and interventional cardiac catheterization (ONACI). Catheter. Cardiovasc. Interv. 2015, 86, E58–E65. [Google Scholar] [CrossRef]
- Johnston, N.; Jönelid, B.; Christersson, C.; Kero, T.; Renlund, H.; Schenck-Gustafsson, K.; Lagerqvist, B. Effect of Gender on Patients With ST-Elevation and Non-ST-Elevation Myocardial Infarction Without Obstructive Coronary Artery Disease. Am. J. Cardiol. 2015, 115, 1661–1666. [Google Scholar] [CrossRef]
- Pizzi, C.; Xhyheri, B.; Costa, G.M.; Faustino, M.; Flacco, M.E.; Gualano, M.R.; Fragassi, G.; Grigioni, F.; Manzoli, L. Nonobstructive versus obstructive coronary artery disease in acute coronary syndrome: A meta-analysis. J. Am. Heart Assoc. 2016, 5, e004185. [Google Scholar] [CrossRef] [Green Version]
- Kunadian, V.; Qiu, W.; Lagerqvist, B.; Johnston, N.; Sinclair, H.; Tan, Y.; Ludman, P.; James, S.; Sarno, G. Gender Differences in Outcomes and Predictors of All-Cause Mortality After Percutaneous Coronary Intervention (Data from United Kingdom and Sweden). Am. J. Cardiol. 2017, 119, 210–216. [Google Scholar] [CrossRef]
- Spirito, A.; Gragnano, F.; Corpataux, N.; Vaisnora, L.; Galea, R.; Svab, S.; Gargiulo, G.; Siontis, G.C.M.; Praz, F.; Lanz, J.; et al. Sex-based differences in bleeding risk after percutaneous coronary intervention and implications for the academic research consortium high bleeding risk criteria. J. Am. Heart Assoc. 2021, 10, 21965. [Google Scholar] [CrossRef]
- Bugiardini, R.; Badimon, L.; Manfrini, O.; Boytsov, S.; Božidarka, K.; Daullxhiu, I.; Dilic, M.; Dorobantu, M.; Erglis, A.; Gafarov, V.; et al. Perspectives: Rationale and design of the ISACS-TC (International Survey of Acute Coronary Syndromes in Transitional Countries) project. Eur. Heart J. Suppl. 2014, 16, A1–A6. [Google Scholar] [CrossRef]
- Cenko, E.; Ricci, B.; Kedev, S.; Vasiljevic, Z.; Dorobantu, M.; Gustiene, O.; Knežević, B.; Miličić, D.; Dilic, M.; Manfrini, O.; et al. Invasive versus conservative strategy in acute coronary syndromes: The paradox in women’s outcomes. Int. J. Cardiol. 2016, 222, 1110–1115. [Google Scholar] [CrossRef] [PubMed]
- Vasiljevic- Pokrajcic, Z.; Mickovski, N.; Davidovic, G.; Asanin, M.; Stefanovic, B.; Krljanac, G.; Radosavljevic-Radovanovic, M.; Radovanovic, N.; Lasica, R.; Milanović, S.; et al. Sex and age differences and outcomes in acute coronary syndromes. Int. J. Cardiol. 2016, 217, S27–S31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cenko, E.; van der Schaar, M.; Yoon, J.; Kedev, S.; Valvukis, M.; Vasiljevic, Z.; Ašanin, M.; Miličić, D.; Manfrini, O.; Badimon, L.; et al. Sex-Specific Treatment Effects After Primary Percutaneous Intervention: A Study on Coronary Blood Flow and Delay to Hospital Presentation. J. Am. Heart Assoc. 2019, 8, e011190. [Google Scholar] [CrossRef] [Green Version]
- Cenko, E.; van der Schaar, M.; Yoon, J.; Manfrini, O.; Vasiljevic, Z.; Vavlukis, M.; Kedev, S.; Miličić, D.; Badimon, L.; Bugiardini, R. Sex-Related Differences in Heart Failure After ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2019, 74, 2379–2389. [Google Scholar] [CrossRef] [PubMed]
- Cepas-Guillen, P.L.; Echarte-Morales, J.; Flores-Umanzor, E.; Fernandez-Valledor, A.; Caldentey, G.; Viana-Tejedor, A.; Martinez Gomez, E.; Tundidor-Sanz, E.; Borrego-Rodriguez, J.; Vidal, P.; et al. Sex-gender disparities in nonagenarians with acute coronary syndrome. Clin. Cardiol. 2021, 44, 371–378. [Google Scholar] [CrossRef]
- De Carlo, M.; Morici, N.; Savonitto, S.; Grassia, V.; Sbarzaglia, P.; Tamburrini, P.; Cavallini, C.; Galvani, M.; Ortolani, P.; De Servi, S.; et al. Sex-Related Outcomes in Elderly Patients Presenting with Non-ST-Segment Elevation Acute Coronary Syndrome: Insights from the Italian Elderly ACS Study. JACC. Cardiovasc. Interv. 2015, 8, 791–796. [Google Scholar] [CrossRef]
- Piątek, Ł.; Wilczek, K.; Kurzawski, J.; Gierlotka, M.; Gąsior, M.; Poloński, L.; Sadowski, M. Gender-related disparities in the treatment and outcomes in patients with non-ST-segment elevation myocardial infarction: Results from the Polish Registry of Acute Coronary Syndromes (PL-ACS) in the years 2012–2014. Arch. Med. Sci. 2020, 16, 781–788. [Google Scholar] [CrossRef]
- Ruiz-Pizarro, V.; Ferrera, C.; Gómez-Polo, J.C.; Palacios-Rubio, J.; Rico-García Amado, C.; Fernández-Ortiz, A.; Viana-Tejedor, A. Sex differences in treatment and prognosis of acute coronary syndrome with interventional management. Cardiovasc. Revasc. Med. 2019, 20, 183–186. [Google Scholar] [CrossRef]
- Healy, B. The Yentl syndrome. N. Engl. J. Med. 1991, 325, 274–276. [Google Scholar] [CrossRef]
- Jin, X.; Chandramouli, C.; Allocco, B.; Gong, E.; Lam, C.S.P.; Yan, L.L. Women’s participation in cardiovascular clinical trials from 2010 to 2017. Circulation 2020, 141, 540–548. [Google Scholar] [CrossRef]
- Cushman, M.; Shay, C.M.; Howard, V.J.; Jiménez, M.C.; Lewey, J.; McSweeney, J.C.; Newby, L.K.; Poudel, R.; Reynolds, H.R.; Rexrode, K.M.; et al. Ten-Year Differences in Women’s Awareness Related to Coronary Heart Disease: Results of the 2019 American Heart Association National Survey: A Special Report from the American Heart Association. Circulation 2021, 143, E239–E248. [Google Scholar] [CrossRef]
- Suero-Abreu, G.A.; Barajas-Ochoaa, A.; Perez-Peralta, A.; Rojas, E.; Berkowitz, R. Assessment of the Effect of the Go Red for Women Campaign on Search Engine Queries for Cardiovascular Disease in Women. Cardiol. Res. 2020, 11, 351–352. [Google Scholar] [CrossRef]
- Banerjee, S.; Aaysha Cader, F.; Gulati, M.; Capers, Q. Racism and Cardiology: A Global Call to Action. CJC Open 2021, 3, S165–S173. [Google Scholar] [CrossRef]
- Bairey Merz, C.N.; Andersen, H.; Sprague, E.; Burns, A.; Keida, M.; Walsh, M.N.; Greenberger, P.; Campbell, S.; Pollin, I.; McCullough, C.; et al. Knowledge, Attitudes, and Beliefs Regarding Cardiovascular Disease in Women: The Women’s Heart Alliance. J. Am. Coll. Cardiol. 2017, 70, 123–132. [Google Scholar] [CrossRef]
- Han, J.E.D.; Liu, X.; Bunce, C.; Douiri, A.; Vale, L.; Blandford, A.; Balaskas, K. Tele-opHthalmology-enablEd and ARtificial Intelligence-ready referral pathway for coMmunity optomEtry referralS of retinal disease: The HERMES study—A Cluster Randomised Superiority Trial with a linked Observational Diagnostic Accuracy Study—NIHR Funding and Awards [Internet]. BMJ Open 2022, 12, e055845. [Google Scholar]
- Kannel, W.B.; Sorlie, P.; Mcnamara, P.M. Prognosis after initial myocardial infarction: The Framingham study. Am. J. Cardiol. 1979, 44, 53–59. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cader, F.A.; Banerjee, S.; Gulati, M. Sex Differences in Acute Coronary Syndromes: A Global Perspective. J. Cardiovasc. Dev. Dis. 2022, 9, 239. https://doi.org/10.3390/jcdd9080239
Cader FA, Banerjee S, Gulati M. Sex Differences in Acute Coronary Syndromes: A Global Perspective. Journal of Cardiovascular Development and Disease. 2022; 9(8):239. https://doi.org/10.3390/jcdd9080239
Chicago/Turabian StyleCader, F Aaysha, Shrilla Banerjee, and Martha Gulati. 2022. "Sex Differences in Acute Coronary Syndromes: A Global Perspective" Journal of Cardiovascular Development and Disease 9, no. 8: 239. https://doi.org/10.3390/jcdd9080239





