Prenatal Exposure to Ambient Pesticides and Preterm Birth and Term Low Birthweight in Agricultural Regions of California
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
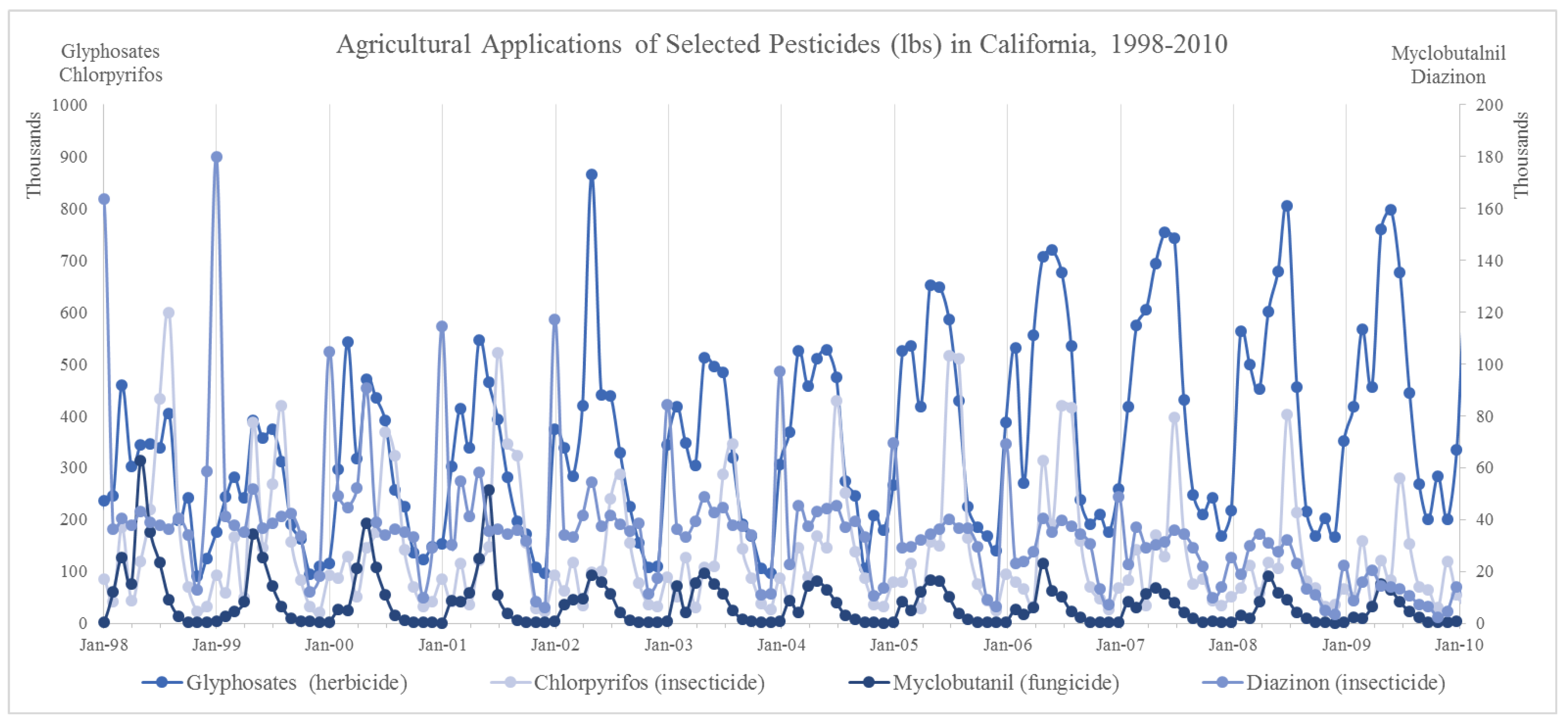
2.2. Exposure Assessment
2.3. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
Appendix A.1. Supplementary Materials and Methods
Appendix A.1.1. Exposure Assessment
Appendix A.1.2. Sensitivity Analyses
Appendix A.2. Supplementary Results
References
- United Health Foundation America’s Health Rankings. Available online: https://www.americashealthrankings.org/explore/2015-annual-report/measure/birthweight/state/ALL (accessed on 12 September 2017).
- Saigal, S.; Doyle, L.W. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008, 371, 261–269. [Google Scholar] [CrossRef]
- Mu, M.; Ye, S.; Bai, M.-J.; Liu, G.-L.; Tong, Y.; Wang, S.-F.; Sheng, J. Birth weight and subsequent risk of asthma: A systematic review and meta-analysis. Heart. Lung Circ. 2014, 23, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Valsamakis, G.; Kanaka-Gantenbein, C.; Malamitsi-Puchner, A.; Mastorakos, G. Causes of intrauterine growth restriction and the postnatal development of the metabolic syndrome. In Annals of the New York Academy of Sciences; Blackwell Publishing Inc.: Hoboken, NJ, USA, 2006; Volume 1092, pp. 138–147. [Google Scholar]
- Barker, D.J.P.; Hales, C.N.; Fall, C.H.D.; Smond, C.O.; Phipps, K.; Clark, P.M.S. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): Relation to reduced fetal growth. Diabetologia 1993, 36, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Luyckx, V.A.; Brenner, B.M. Birth weight, malnutrition and kidney-associated outcomes-a global concern. Nat. Rev. Nephrol. 2015, 11, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Culhane, J.F. Low birth weight in the United States. Am. J. Clin. Nutr. 2007, 85, 584S–590S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- California Department of Pesticide Regulation Summary of Pesticide Use Report Data; California Department of Pesticide Regulation: Sacramento, USA, 2015.
- Quirós-Alcalá, L.; Bradman, A.; Nishioka, M.; Harnly, M.E.; Hubbard, A.; McKone, T.E.; Ferber, J.; Eskenazi, B. Pesticides in house dust from urban and farmworker households in California: An observational measurement study. Environ. Heal. 2011, 10, 19. [Google Scholar] [CrossRef] [PubMed]
- Milczarek, R.; Sokolowska, E.; Rybakowska, I.; Kaletha, K.; Klimek, J. Paraquat inhibits progesterone synthesis in human placental mitochondria. Placenta 2016, 43, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Bretveld, R.W.; Thomas, C.M.G.; Scheepers, P.T.J.; Zielhuis, G.A.; Roeleveld, N. Pesticide exposure: The hormonal function of the female reproductive system disrupted? Reprod. Biol. Endocrinol. 2006, 4, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neta, G.; Goldman, L.R.; Barr, D.; Apelberg, B.J.; Witter, F.R.; Halden, R.U. Fetal exposure to chlordane and permethrin mixtures in relation to inflammatory cytokines and birth outcomes. Environ. Sci. Technol. 2011, 45, 1680–1687. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, V.; Mustafa, M.D.; Sharma, T.; Banerjee, B.D.; Ahmed, R.S.; Tripathi, A.K.; Guleria, K. Association of organochlorine pesticides with the mRNA expression of tumour necrosis factor-alpha (TNF-α) & cyclooxygenase-2 (COX-2) genes in idiopathic preterm birth. Indian J. Med. Res. 2016, 143, 731–738. [Google Scholar] [CrossRef] [PubMed]
- De Siqueira, M.T.; Braga, C.; Cabral-Filho, J.E.; Augusto, L.G.D.S.; Figueiroa, J.N.; Souza, A.I. Correlation between pesticide use in agriculture and adverse birth outcomes in Brazil: An ecological study. Bull. Environ. Contam. Toxicol. 2010, 84, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Maldonado, B.; Sánchez-Ramírez, B.; Reza-López, S.; Levario-Carrillo, M. Effects of exposure to pesticides during pregnancy on placental maturity and weight of newborns: A cross-sectional pilot study in women from the Chihuahua State, Mexico. Hum. Exp. Toxicol. 2009, 28, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Rezende Chrisman, J.; Mattos, I.E.I.E.; Koifman, R.J.; Koifman, S.; Moraes Mello Boccolini, P.; Meyer, A. Prevalence of very low birthweight, malformation, and low Apgar score among newborns in Brazil according to maternal urban or rural residence at birth. J. Obstet. Gynaecol. Res. 2016, 42, 496–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Figà-Talamanca, I. Occupational risk factors and reproductive health of women. Occup. Med. (Lond.) 2006, 56, 521–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sathyanarayana, S.; Basso, O.; Karr, C.J.; Lozano, P.; Alavanja, M.; Sandler, D.P.; Hoppin, J.A. Maternal pesticide use and birth weight in the agricultural health study. J. Agromed. 2010, 15, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Mayhoub, F.; Berton, T.; Bach, V.; Tack, K.; Deguines, C.; Floch-Barneaud, A.; Desmots, S.; Stéphan-Blanchard, E.; Chardon, K.; Ronique Bach, V.; et al. Self-reported parental exposure to pesticide during pregnancy and birth outcomes: The MecoExpo cohort study. PLoS ONE 2014, 9, e99090. [Google Scholar] [CrossRef] [PubMed]
- Saunders, L.; Kadhel, P.; Costet, N.; Rouget, F.; Monfort, C.; Thomé, J.P.; Guldner, L.; Cordier, S.; Multigner, L. Hypertensive disorders of pregnancy and gestational diabetes mellitus among French Caribbean women chronically exposed to chlordecone. Environ. Int. 2014, 68, 171–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, P.; Tian, Y.; Wang, X.-J.; Gao, Y.; Shi, R.; Wang, G.-Q.; Hu, G.-H.; Shen, X.-M. Organophosphate pesticide exposure and perinatal outcomes in Shanghai, China. Environ. Int. 2012, 42, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Wolff, M.S.; Engel, S.; Berkowitz, G.; Teitelbaum, S.; Siskind, J.; Barr, D.B.; Wetmur, J. Prenatal pesticide and PCB exposures and birth outcomes. Pediatr. Res. 2007, 61, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Shirangi, A.; Nieuwenhuijsen, M.; Vienneau, D.; Holman, C.D.J. Living near agricultural pesticide applications and the risk of adverse reproductive outcomes: A review of the literature. Paediatr. Perinat. Epidemiol. 2011, 25, 172–191. [Google Scholar] [CrossRef] [PubMed]
- Gemmill, A.; Gunier, R.B.; Bradman, A.; Eskenazi, B.; Harley, K.G. Residential proximity to methyl bromide use and birth outcomes in an agricultural population in California. Environ. Health Perspect. 2013, 121, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Winchester, P.; Proctor, C.; Ying, J. County-level pesticide use and risk of shortened gestation and preterm birth. Acta Paediatr. 2016, 105, e107–e115. [Google Scholar] [CrossRef] [PubMed]
- Kramer, J. Label Review Manual Chapter 7: Precautionary Statements Label Review Manual; DIANE Publishing: Collingdale, PA, USA, 2014. [Google Scholar]
- Larsen, A.E.; Gaines, S.D.; Deschênes, O. Agricultural pesticide use and adverse birth outcomes in the San Joaquin Valley of California. Nat. Commun. 2017, 8, 302. [Google Scholar] [CrossRef] [PubMed]
- Shaw, G.M.; Yang, W.; Roberts, E.M.; Kegley, S.E.; Stevenson, D.K.; Carmichael, S.L.; English, P.B. Residential Agricultural Pesticide Exposures and Risks of Spontaneous Preterm Birth. Epidemiology 2018, 29, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Shaw, G.M.; Yang, W.; Roberts, E.M.; Aghaeepour, N.; Mayo, J.A.; Weber, K.A.; Maric, I.; Carmichael, S.L.; Winn, V.D.; Stevenson, D.K.; et al. Residential agricultural pesticide exposures and risks of preeclampsia. Environ. Res. 2018, 164, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Von Ehrenstein, O.S.; Ling, C.; Cui, X.; Cockburn, M.; Park, A.S.; Yu, F.; Wu, J.; Ritz, B. Prenatal and Infant Exposure to Agricultural Pesticides and Autism Spectrum Disorder in Children. Jama 2018. [Google Scholar]
- Heck, J.E.; Lombardi, C.A.; Cockburn, M.; Meyers, T.J.; Wilhelm, M.; Ritz, B. Epidemiology of rhabdoid tumors of early childhood. Pediatr. Blood Cancer 2013, 60, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.W.; Wilson, J.P.; Knoblock, C.A.; Ritz, B.; Cockburn, M.G. An effective and efficient approach for manually improving geocoded data. Int. J. Health Geogr. 2008, 7, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rull, R.P.; Ritz, B. Historical pesticide exposure in California using pesticide use reports and land-use surveys: An assessment of misclassification error and bias. Environ. Health Perspect. 2003, 111, 1582–1589. [Google Scholar] [CrossRef] [PubMed]
- Cockburn, M.; Mills, P.; Zhang, X.; Zadnick, J.; Goldberg, D.; Ritz, B. Prostate Cancer and Ambient Pesticide Exposure in Agriculturally Intensive Areas in California. Am. J. Epidemiol. 2011, 173, 1280–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arbuckle, T.E.; Lin, Z.; Mery, L.S. An exploratory analysis of the effect of pesticide exposure on the risk of spontaneous abortion in an Ontario farm population. Environ. Health Perspect. 2001, 109, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Whyatt, R.M.; Rauh, V.; Barr, D.B.; Camann, D.E.; Andrews, H.F.; Garfinkel, R.; Hoepner, L.A.; Diaz, D.; Dietrich, J.; Reyes, A.; et al. Prenatal insecticide exposures and birth weight and length among an urban minority cohort. Environ. Health Perspect. 2004. [Google Scholar] [CrossRef]
- Eskenazi, B.; Harley, K.; Bradman, A.; Weltzien, E.; Jewell, N.P.; Barr, D.B.; Furlong, C.E.; Holland, N.T. Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ. Health Perspect. 2004, 112, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Carmichael, S.L.; Roberts, E.M.; Kegley, S.E.; Padula, A.M.; English, P.B.; Shaw, G.M. Residential agricultural pesticide exposures and risk of neural tube defects and orofacial clefts among offspring in the San Joaquin Valley of California. Am. J. Epidemiol. 2014, 179, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Guiñazú, N.; Rena, V.; Genti-Raimondi, S.; Rivero, V.; Magnarelli, G. Effects of the organophosphate insecticides phosmet and chlorpyrifos on trophoblast JEG-3 cell death, proliferation and inflammatory molecule production. Toxicol. Vitr. 2012, 26, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Bell, E.M.; Hertz-Picciotto, I.; Beaumont, J.J. Case-cohort analysis of agricultural pesticide applications near maternal residence and selected causes of fetal death. Am. J. Epidemiol. 2001, 154, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Ding, G.; Cui, C.; Chen, L.; Gao, Y.; Zhou, Y.; Shi, R.; Tian, Y. Prenatal exposure to pyrethroid insecticides and birth outcomes in Rural Northern China. J. Expo. Sci. Environ. Epidemiol. 2014, 25, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Wilhelm, M.; Chung, J.; Ritz, B. Comparing exposure assessment methods for traffic-related air pollution in an adverse pregnancy outcome study. Environ. Res. 2011, 111, 685–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilhelm, M.; Ghosh, J.K.; Su, J.; Cockburn, M.; Jerrett, M.; Ritz, B. Traffic-related air toxics and preterm birth: A population-based case-control study in Los Angeles County, California. Environ. Health 2011, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Ritz, B.; Wilhelm, M.; Hoggatt, K.J.; Ghosh, J.K.C. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am. J. Epidemiol. 2007, 166, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Valero De Bernabé, J.; Soriano, T.; Albaladejo, R.; Juarranz, M.; Calle, M.E.; Martínez, D.; Domínguez-Rojas, V. Risk factors for low birth weight: A review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 116, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Bashore, C.J.; Geer, L.A.; He, X.; Puett, R.; Parsons, P.J.; Palmer, C.D.; Steuerwald, A.J.; Abulafia, O.; Dalloul, M.; Sapkota, A. Maternal mercury exposure, season of conception and adverse birth outcomes in an urban immigrant community in Brooklyn, New York, U.S.A. Int. J. Environ. Res. Public Health 2014, 11, 8414–8442. [Google Scholar] [CrossRef] [PubMed]
- Yost, K.; Perkins, C.; Cohen, R.; Morris, C.; Wright, W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 2001, 12, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Trunnelle, K.J.; Bennett, D.H.; Tancredi, D.J.; Gee, S.J.; Stoecklin-Marois, M.T.; Hennessy-Burt, T.E.; Hammock, B.D.; Schenker, M.B. Pyrethroids in house dust from the homes of farm worker families in the MICASA study. Environ. Int. 2013, 61, 57–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ingemarsson, I. Gender aspects of preterm birth. In BJOG: An International Journal of Obstetrics and Gynaecology; Blackwell Science Ltd.: Hoboken, NJ, USA, 2003; Volume 110, pp. 34–38. [Google Scholar]
- Challis, J.; Newnham, J.; Petraglia, F.; Yeganegi, M.; Bocking, A. Fetal sex and preterm birth. Placenta 2013, 34, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Kadhel, P.; Monfort, C.; Costet, N.; Rouget, F.; Thome, J.-P.; Multigner, L.; Cordier, S.; Thomé, J.-P.P.; Multigner, L.; Cordier, S. Chlordecone exposure, length of gestation, and risk of preterm birth. Am. J. Epidemiol. 2014, 179, 536–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadler, T.W. Langman’s Medical Embryology; William & Wilkins: Cambridge, UK, 1995. [Google Scholar]
- Chang, H.H.; Warren, J.L.; Darrow, L.A.; Reich, B.J.; Waller, L.A.; Chang, H.H. Assessment of critical exposure and outcome windows in time-to-event analysis with application to air pollution and preterm birth study. Biostatistics 2015, 16, 509–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liew, Z.; Olsen, J.; Cui, X.; Ritz, B.; Arah, O.A. Bias from conditioning on live birth in pregnancy cohorts: An illustration based on neurodevelopment in children after prenatal exposure to organic pollutants. Int. J. Epidemiol. 2015, 44, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Bell, E.M.; Hertz-Picciotto, I.; Beaumont, J.J. A case-control study of pesticides and fetal death due to congenital anomalies. Epidemiology 2001, 12, 148–156. [Google Scholar] [CrossRef] [PubMed]
- White, F.M.; Cohen, F.G.; Sherman, G.; McCurdy, R. Chemicals, birth defects and stillbirths in New Brunswick: Associations with agricultural activity. CMAJ 1988, 138, 117–124. [Google Scholar] [PubMed]
- Kraemer, S. The fragile male. Br. Med. J. 2000, 321, 1609–1612. [Google Scholar] [CrossRef]
- Senthilkumaran, B. Pesticide- and sex steroid analogue-induced endocrine disruption differentially targets hypothalamo–hypophyseal–gonadal system during gametogenesis in teleosts—A review. Gen. Comp. Endocrinol. 2015, 219, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Dallegrave, E.; Mantese, F.D.; Oliveira, R.T.; Andrade, J.M.A.; Dalsenter, P.R.; Langeloh, A. Pre-and postnatal toxicity of the commercial glyphosate formulation in Wistar rats. Arch Toxicol. 2007, 81, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Beuret, C.J.; Zirulnik, F.; Sofía Giménez, M. Effect of the herbicide glyphosate on liver lipoperoxidation in pregnant rats and their fetuses. Reprod. Toxicol. 2005, 19, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Bechi, N.; Sorda, G.; Spagnoletti, A.; Bhattacharjee, J.; Vieira Ferro, E.A.; de Freitas Barbosa, B.; Frosini, M.; Valoti, M.; Sgaragli, G.; Paulesu, L.; et al. Toxicity assessment on trophoblast cells for some environment polluting chemicals and 17β-estradiol. Toxicol. In Vitro 2013, 27, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, S.; Jin, H.; Lee, K.; Bae, J. Impaired development of female mouse offspring maternally exposed to simazine. Environ. Toxicol. Pharmacol. 2014, 38, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Saulsbury, M.D.; Heyliger, S.O.; Wang, K.; Round, D. Characterization of chlorpyrifos-induced apoptosis in placental cells. Toxicology 2008, 244, 98–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mustafa, M.; Garg, N.; Banerjee, B.D.; Sharma, T.; Tyagi, V.; Dar, S.A.; Guleria, K.; Ahmad, R.S.; Vaid, N.; Tripathi, A.K. Inflammatory-mediated pathway in association with organochlorine pesticides levels in the etiology of idiopathic preterm birth. Reprod. Toxicol. 2015, 57, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.J.; Liu, Y.L.; Sytwu, H.K. Immunologic regulation in pregnancy: From mechanism to therapeutic strategy for immunomodulation. Clin. Dev. Immunol. 2012, 2012, 258391. [Google Scholar] [CrossRef] [PubMed]
- Villarejo, D.; McCurdy, S.A. The California Agricultural Workers Health Survey. J. Agric. Saf. Health 2008, 14, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Vinikoor-Imler, L.C.; Davis, J.A.; Meyer, R.E.; Messer, L.C.; Luben, T.J. Associations between prenatal exposure to air pollution, small for gestational age, and term low birthweight in a state-wide birth cohort. Environ. Res. 2014, 132, 132–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R. Toxicology of Organophosphate & Carbamate Compounds; Academic Press: Cambridge, MA, USA, 2006; ISBN 9780120885237. [Google Scholar]
- Rauch, S.A.; Braun, J.M.; Barr, D.B.; Calafat, A.M.; Khoury, J.; Montesano, A.M.; Yolton, K.; Lanphear, B.P. Associations of Prenatal Exposure to Organophosphate Pesticide Metabolites with Gestational Age and Birth Weight. Environ. Health Perspect. 2012, 120, 1055–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dabrowski, S.; Hanke, W.; Polańska, K.; Makowiec-Dabrowska, T.; Sobala, W. Pesticide exposure and birthweight: An epidemiological study in Central Poland. Int. J. Occup. Med. Environ. Health 2003, 16, 31–39. [Google Scholar] [PubMed]
- Huen, K.; Bradman, A.; Harley, K.; Yousefi, P.; Boyd Barr, D.; Eskenazi, B.; Holland, N. Organophosphate pesticide levels in blood and urine of women and newborns living in an agricultural community. Environ. Res. 2012, 117, 8–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Bennett, D.H.; Ritz, B.; Frost, J.; Cassady, D.; Lee, K.; Hertz-Picciotto, I. Residential insecticide usage in northern California homes with young children. J. Expo. Sci. Environ. Epidemiol. 2011, 21, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Belanger, K. Review of research on residential mobility during pregnancy: Consequences for assessment of prenatal environmental exposures. J. Expo. Sci. Environ. Epidemiol. 2012, 22, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Costello, S.; Cockburn, M.; Zhang, X.; Bronstein, J.; Ritz, B. Parkinson’s disease risk from ambient exposure to pesticides. Eur. J. Epidemiol. 2011, 26, 547–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, A.; Cockburn, M.; Ly, T.T.; Bronstein, J.M.; Ritz, B. The association between ambient exposure to organophosphates and Parkinson’s disease risk. Occup. Environ. Med. 2014, 71, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Costello, S.; Cockburn, M.; Bronstein, J.; Zhang, X.; Ritz, B. Parkinson’s disease and residential exposure to maneb and paraquat from agricultural applications in the central valley of California. Am. J. Epidemiol. 2009, 169, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, S.L.; Yang, W.; Roberts, E.; Kegley, S.E.; Brown, T.J.; English, P.B.; Lammer, E.J.; Shaw, G.M. Residential agricultural pesticide exposures and risks of selected birth defects among offspring in the San Joaquin Valley of California. Birth Defects Res. Part A - Clin. Mol. Teratol. 2016, 106, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Rull, R.P.; Gunier, R.; Von Behren, J.; Hertz, A.; Crouse, V.; Buffler, P.A.; Reynolds, P. Residential proximity to agricultural pesticide applications and childhood acute lymphoblastic leukemia. Environ. Res. 2009, 109, 891–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritz, B.; Costello, S. Geographic model and biomarker-derived measures of pesticide exposure and Parkinson’s disease. Ann. N. Y. Acad. Sci. 2006, 1076, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Gunier, R.B.; Ward, M.H.; Airola, M.; Bell, E.M.; Colt, J.; Nishioka, M.; Buffler, P.A.; Reynolds, P.; Rull, R.P.; Hertz, A.; Metayer, C.; Nuckols, J.R. Determinants of agricultural pesticide concentrations in carpet dust. Environ. Health Perspect. 2011, 119, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Wofford, P.; Segawa, R.; Schreider, J.; Federighi, V.; Neal, R.; Brattesani, M. Community air monitoring for pesticides. Part 3: using health-based screening levels to evaluate results collected for a year. Environ. Monit. Assess. 2013, 186, 1355–1370. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, J.K.C.; Wilhelm, M.; Su, J.; Goldberg, D.; Cockburn, M.; Jerrett, M.; Ritz, B. Assessing the influence of traffic-related air pollution on risk of term low birth weight on the basis of land-use-based regression models and measures of air toxics. Am. J. Epidemiol. 2012, 175, 1262–1274. [Google Scholar] [CrossRef] [PubMed]
- Ritz, B.; Wilhelm, M. Ambient air pollution and adverse birth outcomes: methodologic issues in an emerging field. Basic Clin. Pharmacol. Toxicol. 2008, 102, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Ritz, B.; Qiu, J.; Lee, P.-C.; Lurmann, F.; Penfold, B.; Erin Weiss, R.; McConnell, R.; Arora, C.; Hobel, C.; Wilhelm, M. Prenatal air pollution exposure and ultrasound measures of fetal growth in Los Angeles, California. Environ. Res. 2014, 130, 7–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benson, P. CALINE4—A Dispersion Model for Predicting Air Pollutant Concentrations Near Roadways; Report No. FHWA/CA/TL-84/15; California Department of Transportation, Office of Transportation Laboratory: Sacramento, CA, USA, 1989.
- Chen, H.; Bai, S.; Eisinger, D.; Niemeier, D.; Claggett, M. Predicting Near-Road PM2.5 Concentrations. Transp. Res. Rec. J. Transp. Res. Board 2009, 2123, 26–37. [Google Scholar] [CrossRef]
- Lewis, C.; Hoggatt, K.J.; Ritz, B. The impact of different causal models on estimated effects of disinfection by-products on preterm birth. Environ. Res. 2011, 111, 371–376. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists Medically indicated late-preterm and early-term deliveries. ACOG Committee opinion no. 560. Obs. Gynecol 2013, 121, 908–910. [Google Scholar]
- Xiong, X.; Saunders, L.D.; Wang, F.L.; Demianczuk, N.N. Gestational diabetes mellitus: Prevalence, risk factors, maternal and infant outcomes. Int. J. Gynecol. Obstet. 2001, 75, 221–228. [Google Scholar] [CrossRef]
- Sendag, F.; Terek, M.C.; Itil, I.M.; Oztekin, K.; Bilgin, O. Maternal and perinatal outcomes in women with gestational diabetes mellitus as compared to nondiabetic controls. J. Reprod. Med. 2001, 46, 1057–1062. [Google Scholar] [PubMed]
| Characteristic | Preterm Birth | Term Birth | Term Low Birthweight | Term Normal Birthweight | ||||
|---|---|---|---|---|---|---|---|---|
| N = 24,693 | % | N = 220,297 | % | N = 4412 | % | N = 194,732 | % | |
| Infant sex | ||||||||
| Males | 18,586 | 75.3 | 161,076 | 73.1 | 2972 | 67.4 | 140,308 | 72.1 |
| Females | 6107 | 24.7 | 59,221 | 26.9 | 1440 | 32.6 | 54,424 | 27.9 |
| Year of Birth | ||||||||
| 1998 | 1393 | 5.6 | 12,327 | 5.6 | 262 | 5.9 | 10,728 | 5.5 |
| 1999 | 1483 | 6.0 | 12,599 | 5.7 | 228 | 5.2 | 10,944 | 5.6 |
| 2000 | 1504 | 6.1 | 14,190 | 6.4 | 293 | 6.6 | 12,381 | 6.4 |
| 2001 | 1661 | 6.7 | 14,759 | 6.7 | 279 | 6.3 | 12,856 | 6.6 |
| 2002 | 1808 | 7.3 | 15,882 | 7.2 | 319 | 7.2 | 13,846 | 7.1 |
| 2003 | 2043 | 8.3 | 17,993 | 8.2 | 365 | 8.3 | 15,684 | 8.1 |
| 2004 | 2127 | 8.6 | 18,030 | 8.2 | 385 | 8.7 | 15,924 | 8.2 |
| 2005 | 2127 | 8.6 | 18,860 | 8.6 | 361 | 8.2 | 16,824 | 8.6 |
| 2006 | 2200 | 8.9 | 19,797 | 9.0 | 409 | 9.3 | 17,680 | 9.1 |
| 2007 | 2440 | 9.9 | 20,616 | 9.4 | 448 | 10.2 | 18,412 | 9.5 |
| 2008 | 2359 | 9.6 | 21,950 | 10.0 | 445 | 10.1 | 19,696 | 10.1 |
| 2009 | 2063 | 8.4 | 19,155 | 8.7 | 349 | 7.9 | 17,160 | 8.8 |
| 2010 | 1485 | 6.0 | 14,139 | 6.4 | 269 | 6.1 | 12,597 | 6.5 |
| Maternal Age | ||||||||
| 19 or less | 2976 | 12.1 | 21,126 | 9.6 | 593 | 13.4 | 19,711 | 10.1 |
| 20–24 | 5772 | 23.4 | 50,362 | 22.9 | 1045 | 23.7 | 45,392 | 23.3 |
| 25–29 | 5922 | 24.0 | 59,782 | 27.1 | 1139 | 25.8 | 52,667 | 27.0 |
| 30–34 | 5590 | 22.6 | 53,719 | 24.4 | 938 | 21.3 | 46,661 | 24.0 |
| 35 and older | 4432 | 17.9 | 35,306 | 16.0 | 696 | 15.8 | 30,299 | 15.6 |
| Missing | 1 | 0.0 | 2 | 0.0 | 1 | 0.0 | 2 | 0.0 |
| Maternal Education | ||||||||
| <12 years | 8238 | 33.4 | 62,459 | 28.4 | 1351 | 30.6 | 55,856 | 28.7 |
| 12 years | 6955 | 28.2 | 58,683 | 26.6 | 1249 | 28.3 | 51,883 | 26.6 |
| 13–15 years | 4949 | 20.0 | 45,809 | 20.8 | 866 | 19.6 | 40,122 | 20.6 |
| 16+ years | 3984 | 16.1 | 48,252 | 21.9 | 827 | 18.7 | 42,367 | 21.8 |
| Missing | 567 | 2.3 | 5094 | 2.3 | 119 | 2.7 | 4504 | 2.3 |
| Maternal Race/Ethnicity | ||||||||
| White, non-Hispanic | 5919 | 24.0 | 64,600 | 29.3 | 928 | 21.0 | 55,036 | 28.3 |
| Hispanic, any race | 13,801 | 55.9 | 116,509 | 52.9 | 2278 | 51.6 | 103,428 | 53.1 |
| Black | 1691 | 6.8 | 9639 | 4.4 | 392 | 8.9 | 8843 | 4.5 |
| Asian/PI | 2437 | 9.9 | 21,570 | 9.8 | 587 | 13.3 | 20,193 | 10.4 |
| Other/Refused | 845 | 3.4 | 7979 | 3.6 | 227 | 5.1 | 7232 | 3.7 |
| Parity | ||||||||
| 1 | 9319 | 37.7 | 84,535 | 38.4 | 2238 | 50.7 | 76,877 | 39.5 |
| 2 | 7060 | 28.6 | 70,977 | 32.2 | 1087 | 24.6 | 62,329 | 32.0 |
| 3 or more | 8306 | 33.6 | 64,736 | 29.4 | 1084 | 24.6 | 55,484 | 28.5 |
| Missing | 8 | 0.0 | 49 | 0.0 | 3 | 0.1 | 42 | 0.0 |
| Prenatal care in first trimester | ||||||||
| Yes | 19,821 | 80.3 | 186,741 | 84.8 | 3533 | 80.1 | 164,640 | 84.5 |
| No | 4580 | 18.5 | 32,233 | 14.6 | 834 | 18.9 | 28,891 | 14.8 |
| Missing | 292 | 1.2 | 1323 | 0.6 | 45 | 1.0 | 1201 | 0.6 |
| Payment type of prenatal care | ||||||||
| Private/ Health Maintenance Organization/Blue Cross Blue Shield | 10,731 | 43.5 | 110,816 | 50.3 | 1961 | 44.4 | 96,650 | 49.6 |
| MediCal/Govt/self-pay | 13,591 | 55.0 | 108,385 | 49.2 | 2401 | 54.4 | 97,085 | 49.9 |
| Missing | 371 | 1.5 | 1096 | 0.5 | 50 | 1.1 | 997 | 0.5 |
| Maternal birthplace | ||||||||
| US | 13,585 | 55.0 | 119,055 | 54.0 | 2337 | 53.0 | 104,048 | 53.4 |
| Non-US countries | 11,093 | 44.9 | 101,169 | 45.9 | 2072 | 47.0 | 90,618 | 46.5 |
| Missing | 15 | 0.1 | 73 | 0.0 | 3 | 0.1 | 66 | 0.0 |
| Quintiles of neighborhood socioeconomic status | ||||||||
| 1 (Lowest) | 7157 | 29.0 | 55,746 | 25.3 | 1254 | 28.4 | 49,635 | 25.5 |
| 2 | 6403 | 25.9 | 55,227 | 25.1 | 1174 | 26.6 | 48,916 | 25.1 |
| 3 | 5143 | 20.8 | 45,378 | 20.6 | 883 | 20.0 | 39,879 | 20.5 |
| 4 | 3451 | 14.0 | 35,467 | 16.1 | 627 | 14.2 | 31,215 | 16.0 |
| 5 (Highest) | 2525 | 10.2 | 28,364 | 12.9 | 474 | 10.7 | 24,980 | 12.8 |
| Missing | 14 | 0.1 | 115 | 0.1 | . | . | 107 | 0.1 |
| Pesticide | First Trimester | Second Trimester | ||||||
|---|---|---|---|---|---|---|---|---|
| Preterm Birth * | Term Birth * | OR 1 | OR 2 | Preterm Birth * | Term Birth * | OR 1 | OR 2 | |
| Fungicide | ||||||||
| Myclobutanil | 5307 (22.0%) | 47,755 (21.6%) | 1.02 (0.99, 1.05) | 1.02 (0.99, 1.06) | 5366 (22.2%) | 48,337 (21.9%) | 1.02 (0.98, 1.05) | 1.02 (0.99, 1.06) |
| Chlorothalonil | 5511 (22.8%) | 49,183 (22.3%) | 1.03 (1.00, 1.06) | 1.02 (0.99, 1.05) | 5585 (23.1%) | 49,070 (22.2%) | 1.05 (1.02, 1.08) | 1.04 (1.01, 1.08) |
| Mancozeb | 3600 (14.9%) | 32,779 (14.8%) | 1.00 (0.96, 1.04) | 0.98 (0.95, 1.02) | 3588 (14.8%) | 33,038 (15.0%) | 0.99 (0.95, 1.02) | 0.97 (0.94, 1.01) |
| Herbicide | ||||||||
| Glyphosate compounds | 14,346 (59.3%) | 127,703 (57.8%) | 1.07 (1.04, 1.10) | 1.05 (1.02, 1.08) | 14,295 (59.1%) | 127,672 (57.8%) | 1.06 (1.03, 1.09) | 1.04 (1.01, 1.07) |
| Paraquat dichloride | 3850 (15.9%) | 32,073 (14.5%) | 1.11 (1.07, 1.16) | 1.07 (1.03, 1.11) | 3823 (15.8%) | 32,009 (14.5%) | 1.11 (1.07, 1.15) | 1.06 (1.02, 1.10) |
| Simazine | 2613 (10.8%) | 23,310 (10.6%) | 1.02 (0.98, 1.07) | 1.02 (0.97, 1.06) | 2684 (11.1%) | 22,978 (10.4%) | 1.07 (1.03, 1.12) | 1.06 (1.02, 1.11) |
| Insecticide | ||||||||
| Chlorpyrifos | 8511 (35.2%) | 74,414 (33.7%) | 1.06 (1.04, 1.10) | 1.03 (1.00, 1.06) | 8390 (34.7%) | 74,037 (33.5%) | 1.05 (1.02, 1.08) | 1.02 (0.99, 1.05) |
| Abamectin | 7715 (31.9%) | 68,819 (31.2%) | 1.04 (1.01, 1.07) | 1.02 (0.99, 1.05) | 7736 (32.0%) | 69,606 (31.5%) | 1.02 (0.99, 1.05) | 1.01 (0.98, 1.04) |
| Malathion | 5696 (23.6%) | 51,530 (23.3%) | 1.01 (0.98, 1.04) | 0.99 (0.96, 1.03) | 5715 (23.6%) | 51,429 (23.3%) | 1.02 (0.99, 1.05) | 1.00 (0.97, 1.03) |
| Imidacloprid | 6107 (25.3%) | 53,105 (24.0%) | 1.07 (1.04, 1.10) | 1.06 (1.03, 1.10) | 6139 (25.4%) | 54,444 (24.6%) | 1.04 (1.01, 1.08) | 1.04 (1.00, 1.07) |
| Diazinon | 5319 (22.0%) | 46,514 (21.1%) | 1.05 (1.01, 1.08) | 1.02 (0.99, 1.06) | 5185 (21.4%) | 45,430 (20.6%) | 1.05 (1.01, 1.08) | 1.02 (0.99, 1.06) |
| Permethrin | 4597 (19.0%) | 40,300 (18.2%) | 1.05 (1.02, 1.09) | 1.03 (1.00, 1.07) | 4465 (18.5%) | 40,533 (18.3%) | 1.01 (0.97, 1.04) | 0.99 (0.95, 1.02) |
| Dimethoate | 3223 (13.3%) | 27,905 (12.6%) | 1.06 (1.02, 1.10) | 1.04 (1.00, 1.08) | 3216 (13.3%) | 27,874 (12.6%) | 1.06 (1.02, 1.10) | 1.03 (0.99, 1.07) |
| Methyl bromide | 2448 (10.1%) | 21,398 (9.7%) | 1.04 (1.00, 1.09) | 1.05 (1.00, 1.10) | 2337 (9.7%) | 20,851 (9.4%) | 1.02 (0.98, 1.07) | 1.01 (0.96, 1.06) |
| Carbaryl | 2241 (9.3%) | 20,285 (9.2%) | 1.00 (0.96, 1.05) | 1.00 (0.96, 1.05) | 2150 (8.9%) | 20,160 (9.1%) | 0.97 (0.92, 1.01) | 0.96 (0.92, 1.01) |
| Phosmet | 1154 (4.8%) | 9995 (4.5%) | 1.05 (0.99, 1.12) | 1.01 (0.95, 1.08) | 1099 (4.5%) | 9875 (4.5%) | 1.01 (0.95, 1.08) | 0.97 (0.91, 1.04) |
| Methyl parathion | 448 (1.9%) | 3660 (1.7%) | 1.11 (1.01, 1.23) | 1.05 (0.95, 1.17) | 402 (1.7%) | 3715 (1.7%) | 0.98 (0.88, 1.08) | 0.91 (0.82, 1.01) |
| Chemical Class | First Trimester | Second Trimester | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Preterm Birth * | Term Birth * | OR 1 | OR 2 | OR 3 | Preterm Birth * | Term Birth * | OR 1 | OR 2 | OR 3 | |
| No. of carbamates ever exposed to | ||||||||||
| 0 (ref.) | 15,419 (63.8%) | 143,956 (65.2%) | 15,343 (63.5%) | 143,806 (65.1%) | ||||||
| 1 | 4519 (18.7%) | 40,328 (18.3%) | 1.04 (1.01, 1.08) | 1.03 (0.99, 1.07) | 1.01 (0.98, 1.05) | 4604 (19.0%) | 40,390 (18.3%) | 1.07 (1.03, 1.10) | 1.04 (1.01, 1.08) | 1.03 (0.99, 1.07) |
| 2+ | 4237 (17.5%) | 36,613 (16.6%) | 1.08 (1.04, 1.11) | 1.04 (1.00, 1.08) | 1.01 (0.97, 1.06) | 4227 (17.5%) | 36,702 (16.6%) | 1.07 (1.04, 1.11) | 1.04 (1.00, 1.08) | 1.03 (0.98, 1.08) |
| No. of organophosphates ever exposed to | ||||||||||
| 0 (ref.) | 9523 (39.4%) | 90,246 (40.9%) | 9469 (39.2%) | 90,715 (41.1%) | ||||||
| 1 | 5105 (21.1%) | 46,306 (21.0%) | 1.04 (1.01, 1.08) | 1.01 (0.98, 1.05) | 1.00 (0.96, 1.04) | 5263 (21.8%) | 46,494 (21.0%) | 1.08 (1.04, 1.12) | 1.06 (1.02, 1.10) | 1.04 (1.00, 1.08) |
| 2+ | 9546 (39.5%) | 84,346 (38.2%) | 1.07 (1.03, 1.10) | 1.02 (0.99, 1.06) | 0.98 (0.94, 1.02) | 9442 (39.1%) | 83,688 (37.9%) | 1.07 (1.04, 1.11) | 1.03 (1.00, 1.06) | 0.99 (0.95, 1.03) |
| No. of pyrethroids ever exposed to | ||||||||||
| 0 (ref.) | 11,938 (49.4%) | 112,936 (51.1%) | 11,906 (49.3%) | 112,617 (51.0%) | ||||||
| 1 | 4965 (20.5%) | 44,681 (20.2%) | 1.05 (1.01, 1.09) | 1.03 (0.99, 1.06) | 1.03 (0.99, 1.07) | 4977 (20.6%) | 44,247 (20.0%) | 1.06 (1.02, 1.10) | 1.04 (1.00, 1.08) | 1.03 (0.99, 1.07) |
| 2+ | 7272 (30.1%) | 63,281 (28.6%) | 1.09 (1.05, 1.12) | 1.06 (1.02, 1.09) | 1.06 (1.01, 1.11) | 7291 (30.2%) | 64,034 (29.0%) | 1.08 (1.04, 1.11) | 1.05 (1.01, 1.08) | 1.04 (0.99, 1.08) |
| Chemical Class | First Trimester | Second Trimester | ||||||
|---|---|---|---|---|---|---|---|---|
| Preterm Birth * | Term Birth * | OR 1 | OR 2 | Preterm Birth * | Term Birth * | OR 1 | OR 2 | |
| Males | ||||||||
| No. of carbamates ever exposed to | ||||||||
| 0 (ref.) | 11,978 (64.4%) | 104,716 (64.9%) | 11,937 (64.2%) | 104,618 (64.8%) | ||||
| 1 | 3408 (18.3%) | 29,803 (18.5%) | 1.00 (0.96, 1.04) | 0.99 (0.95, 1.03) | 3466 (18.6%) | 29,761 (18.4%) | 1.02 (0.98, 1.06) | 1.01 (0.97, 1.05) |
| 2+ | 3215 (17.3%) | 26,835 (16.6%) | 1.05 (1.00, 1.09) | 1.01 (0.97, 1.06) | 3198 (17.2%) | 26,974 (16.7%) | 1.04 (1.00, 1.08) | 1.00 (0.96, 1.05) |
| No. of organophosphates ever exposed to | ||||||||
| 0 (ref.) | 7352 (39.5%) | 65,519 (40.6%) | 7320 (39.4%) | 65,953 (40.9%) | ||||
| 1 | 3973 (21.4%) | 33,934 (21.0%) | 1.04 (1.00, 1.09) | 1.02 (0.97, 1.06) | 4055 (21.8%) | 34,148 (21.2%) | 1.07 (1.03, 1.11) | 1.05 (1.01, 1.09) |
| 2+ | 7276 (39.1%) | 61,901 (38.4%) | 1.05 (1.01, 1.08) | 1.01 (0.97, 1.04) | 7226 (38.8%) | 61,253 (38.0%) | 1.06 (1.02, 1.10) | 1.02 (0.98, 1.06) |
| No. of pyrethroids ever exposed to | ||||||||
| 0 (ref.) | 9239 (49.7%) | 82,215 (51.0%) | 9281 (49.9%) | 82,055 (50.9%) | ||||
| 1 | 3902 (21.0%) | 32,699 (20.3%) | 1.06 (1.02, 1.10) | 1.03 (0.99, 1.08) | 3822 (20.5%) | 32,618 (20.2%) | 1.03 (0.99, 1.08) | 1.01 (0.97, 1.06) |
| 2+ | 5460 (29.4%) | 46,440 (28.8%) | 1.04 (1.01, 1.08) | 1.01 (0.98, 1.05) | 5498 (29.6%) | 46,681 (28.9%) | 1.04 (1.00, 1.08) | 1.01 (0.97, 1.05) |
| Females | ||||||||
| No. of carbamates ever exposed to | ||||||||
| 0 (ref.) | 3861 (63.1%) | 38,769 (65.5%) | 3835 (62.6%) | 38,723 (65.4%) | ||||
| 1 | 1171 (19.1%) | 10,682 (18.0%) | 1.09 (1.02, 1.17) | 1.08 (1.00, 1.15) | 1195 (19.5%) | 10,731 (18.1%) | 1.12 (1.05, 1.20) | 1.09 (1.01, 1.17) |
| 2+ | 1090 (17.8%) | 9783 (16.5%) | 1.11 (1.03, 1.19) | 1.07 (1.00, 1.15) | 1091 (17.8%) | 9778 (16.5%) | 1.12 (1.04, 1.20) | 1.08 (1.01, 1.17) |
| No. of organophosphates ever exposed to | ||||||||
| 0 (ref.) | 2402 (39.2%) | 24,352 (41.1%) | 2385 (39.0%) | 24,443 (41.3%) | ||||
| 1 | 1276 (20.8%) | 12,375 (20.9%) | 1.04 (0.97, 1.12) | 1.01 (0.94, 1.09) | 1331 (21.7%) | 12,396 (20.9%) | 1.10 (1.02, 1.18) | 1.07 (1.00, 1.15) |
| 2+ | 2444 (39.9%) | 22,506 (38.0%) | 1.09 (1.03, 1.16) | 1.04 (0.98, 1.11) | 2406 (39.3%) | 22,394 (37.8%) | 1.09 (1.03, 1.16) | 1.04 (0.98, 1.11) |
| No. of pyrethroids ever exposed to | ||||||||
| 0 (ref.) | 3003 (49.0%) | 30,390 (51.3%) | 2969 (48.5%) | 30,277 (51.1%) | ||||
| 1 | 1226 (20.0%) | 11,958 (20.2%) | 1.04 (0.97, 1.11) | 1.02 (0.95, 1.09) | 1263 (20.6%) | 11,751 (19.8%) | 1.09 (1.02, 1.17) | 1.08 (1.00, 1.16) |
| 2+ | 1893 (30.9%) | 16,886 (28.5%) | 1.14 (1.07, 1.21) | 1.11 (1.04, 1.18) | 1889 (30.9%) | 17,206 (29.0%) | 1.12 (1.05, 1.19) | 1.09 (1.02, 1.16) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ling, C.; Liew, Z.; Von Ehrenstein, O.S.; Heck, J.E.; Park, A.S.; Cui, X.; Cockburn, M.; Wu, J.; Ritz, B. Prenatal Exposure to Ambient Pesticides and Preterm Birth and Term Low Birthweight in Agricultural Regions of California. Toxics 2018, 6, 41. https://doi.org/10.3390/toxics6030041
Ling C, Liew Z, Von Ehrenstein OS, Heck JE, Park AS, Cui X, Cockburn M, Wu J, Ritz B. Prenatal Exposure to Ambient Pesticides and Preterm Birth and Term Low Birthweight in Agricultural Regions of California. Toxics. 2018; 6(3):41. https://doi.org/10.3390/toxics6030041
Chicago/Turabian StyleLing, Chenxiao, Zeyan Liew, Ondine S. Von Ehrenstein, Julia E. Heck, Andrew S. Park, Xin Cui, Myles Cockburn, Jun Wu, and Beate Ritz. 2018. "Prenatal Exposure to Ambient Pesticides and Preterm Birth and Term Low Birthweight in Agricultural Regions of California" Toxics 6, no. 3: 41. https://doi.org/10.3390/toxics6030041





