Carvacrol Selective Pressure Allows the Occurrence of Genetic Resistant Variants of Listeria monocytogenes EGD-e
Abstract
:1. Introduction
2. Materials and Methods
2.1. Microorganisms and Growth Conditions
2.2. Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC)
2.3. Carvacrol Evolution Assays
2.4. Survival Curves to Lethal Concentrations of Carvacrol and Heat Treatments
2.5. Antibiotic Susceptibility Test
2.6. Statistical Analysis
2.7. Whole Genome Sequencing (WGS)
3. Results
3.1. Isolation of RVs of L. monocytogenes against Carvacrol
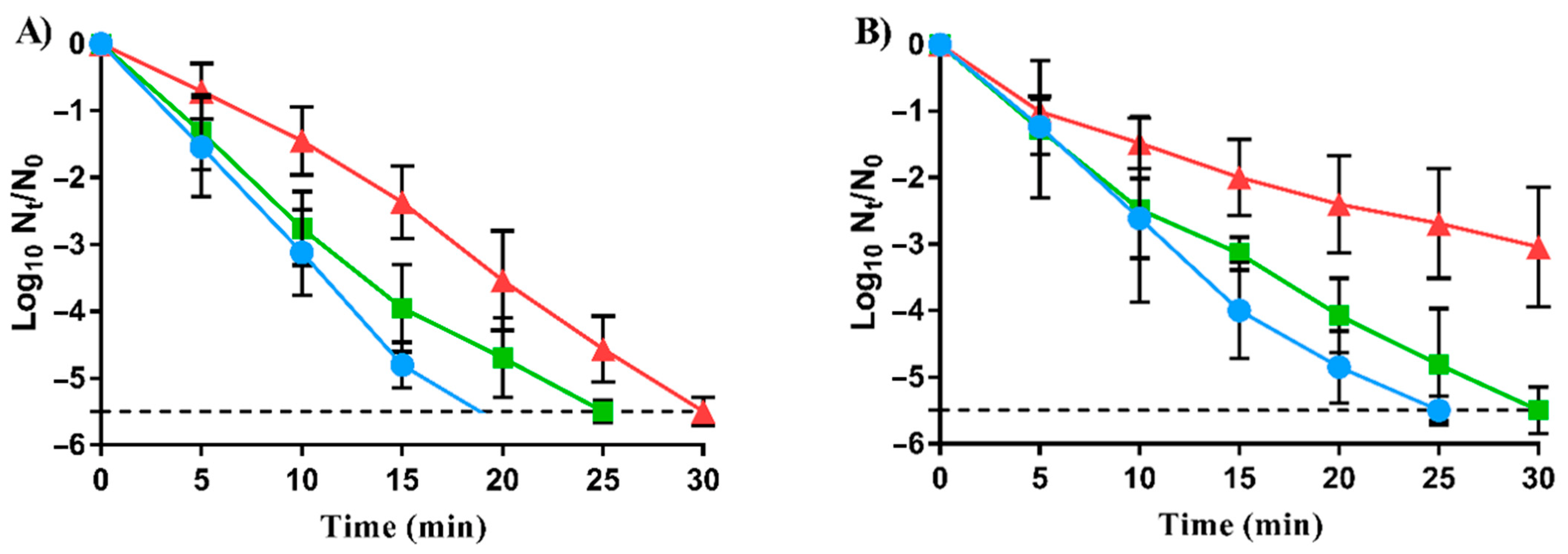
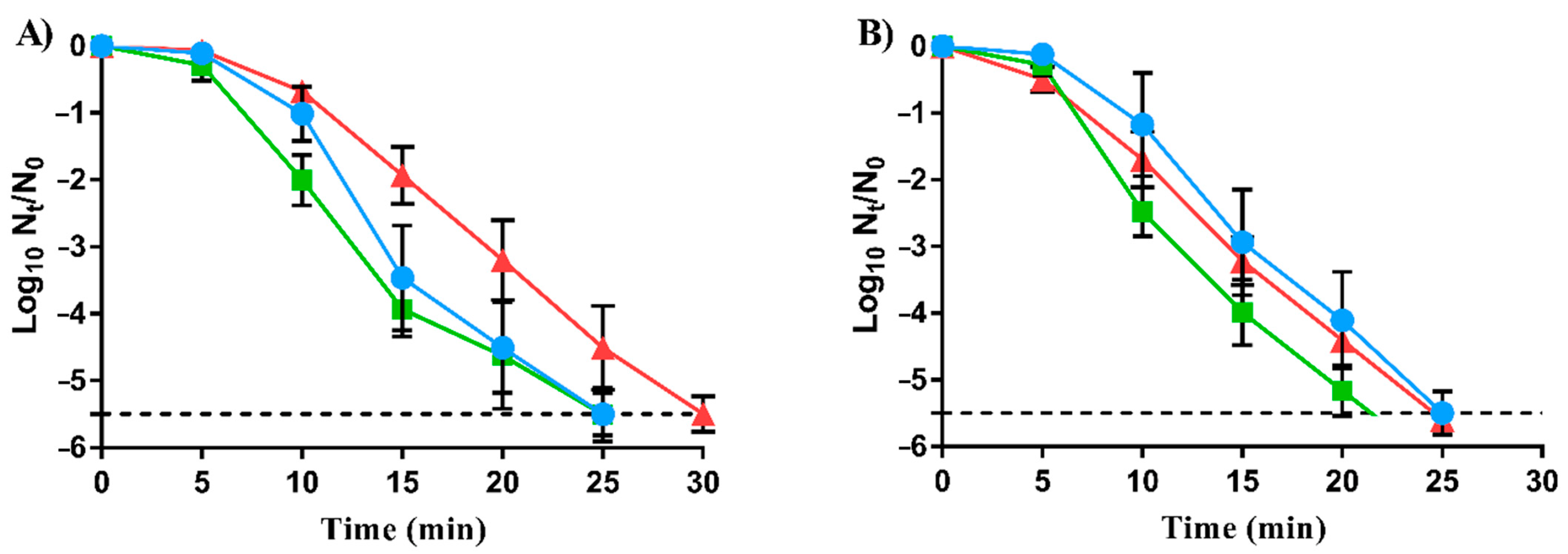
3.2. Decreased Lethal Efficacy of Carvacrol against RVs
3.3. Slight Increased Cross-Resistance to Heat of RVs to Carvacrol
3.4. Ampicillin Resistance Changes in RVs to Carvacrol
3.5. Whole-Genome Sequencing of RVs to Carvacrol
- (i)
- A transversion from thymine to guanine at position 287 bp (T287G) of lmo0785 led to the substitution of leucine (Leu) by arginine (Arg) at amino acid 96. The missense mutation was located in the manR gene, which encodes a transcriptional activator of a phosphotransferase system domain.
- (ii)
- An insertion at position 423 bp of lmo1539 produced a reading frameshift in the transcription of a glycerol transporter.
- (iii)
- A frameshift mutation at position 123 bp of lmo1921, which function has not been evidenced in vivo.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Carocho, M.; Barreiro, M.F.; Morales, P.; Ferreira, I.C.F.R. Adding molecules to food, pros and cons: A review on synthetic and natural food additives. Compr. Rev. Food Sci. Food Saf. 2014, 13, 377–399. [Google Scholar] [CrossRef]
- Quinto, E.J.; Caro, I.; Villalobos-Delgado, L.H.; Mateo, J.; De-Mateo-Silleras, B.; Redondo-Del-Río, M.P. Food safety through natural antimicrobials. Antibiotics 2019, 8, 208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faleiro, M.L.; Miguel, G. Antimicrobial and antioxidant activities of natural compounds: Enhance the safety and quality of food. Foods 2020, 9, 1145. [Google Scholar] [CrossRef] [PubMed]
- Nostro, A.; Papalia, T. Antimicrobial activity of carvacrol: Current progress and future prospectives. Recent Pat. Anti-Infect. Drug Disc. 2012, 7, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Espina, L.; García-Gonzalo, D.; Pagán, R. Impact of essential oils on the taste acceptance of tomato juice, vegetable soup, or poultry burgers. J. Food Sci. 2014, 79, S1575–S1583. [Google Scholar] [CrossRef]
- Falleh, H.; Ben Jemaa, M.; Saada, M.; Ksouri, R. Essential oils: A promising eco-friendly food preservative. Food Chem. 2020, 330, 127268. [Google Scholar] [CrossRef]
- Martínez, A.; Manrique-Moreno, M.; Klaiss-Luna, M.C.; Stashenko, E.; Zafra, G.; Ortiz, C. Effect of essential oils on growth inhibition, biofilm formation and membrane integrity of Escherichia coli and Staphylococcus aureus. Antibiotics 2021, 10, 1474. [Google Scholar] [CrossRef]
- Larsson, D.G.J.; Flach, C.-F. Antibiotic resistance in the environment. Nat. Rev. Microbiol. 2022, 20, 257–269. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Miethke, M.; Pieroni, M.; Weber, T.; Brönstrup, M.; Hammann, P.; Halby, L.; Arimondo, P.B.; Glaser, P.; Aigle, B.; Bode, H.B.; et al. Towards the sustainable discovery and development of new antibiotics. Nat. Rev. Chem. 2021, 5, 726–749. [Google Scholar] [CrossRef]
- León-Buitimea, A.; Garza-Cárdenas, C.R.; Garza-Cervantes, J.A.; Lerma-Escalera, J.A.; Morones-Ramírez, J.R. The demand for new antibiotics: Antimicrobial peptides, nanoparticles, and combinatorial therapies as future strategies in antibacterial agent design. Front. Microbiol. 2020, 11, 1669. [Google Scholar] [CrossRef] [PubMed]
- Yap, P.S.X.; Yiap, B.C.; Ping, H.C.; Lim, S.H.E. Essential oils, a new horizon in combating bacterial antibiotic resistance. Open Microbiol. J. 2014, 8, 6–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Souza, E.L. The effects of sublethal doses of essential oils and their constituents on antimicrobial susceptibility and antibiotic resistance among food-related bacteria: A review. Trends Food Sci. Technol. 2016, 56, 1–12. [Google Scholar] [CrossRef]
- Hashemi, S.M.B.; Khorram, S.B.; Sohrabi, M. Antioxidant activity of essential oils in foods. In Essential Oils in Food Processing; Hashemi, S.M.B., Khaneghah, A.M., de Souza Sant’Ana, A., Eds.; Wiley Blackwell: New Hoboken, NJ, USA, 2017; pp. 247–265. [Google Scholar]
- Chueca, B.; Berdejo, D.; Gomes-Neto, N.J.; Pagán, R.; García-Gonzalo, D. Emergence of hyper-resistant Escherichia coli MG1655 derivative strains after applying sub-Inhibitory doses of individual constituents of essential oils. Front. Microbiol. 2016, 7, 273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nostro, A.; Marino, A.; Ginestra, G.; Cellini, L.; Di Giulio, M.; Bisignano, G. Effects of adaptation to carvacrol on Staphylococcus aureus in the planktonic and biofilm phases. Biofouling 2017, 33, 470–480. [Google Scholar] [CrossRef]
- Berdejo, D.; Merino, N.; Pagán, E.; García-Gonzalo, D.; Pagán, R. Genetic variants and phenotypic characteristics of Salmonella Typhimurium-resistant mutants after exposure to carvacrol. Microorganisms 2020, 8, 937. [Google Scholar] [CrossRef]
- Berdejo, D.; Chueca, B.; Pagan, E.; Renzoni, A.; Kelley, W.L.; Pagan, R.; Garcia-Gonzalo, D. Sub-inhibitory doses of individual constituents of essential oils can select for Staphylococcus aureus resistant mutants. Molecules 2019, 24, 170. [Google Scholar] [CrossRef] [Green Version]
- Berdejo, D.; Pagán, E.; Merino, N.; García-Gonzalo, D.; Pagán, R. Emerging mutant populations of Listeria monocytogenes EGD-e under selective pressure of Thymbra capitata essential oil question its use in food preservation. Food Res. Int. 2021, 145, 110403. [Google Scholar] [CrossRef]
- Chueca, B.; Renzoni, A.; Berdejo, D.; Pagan, R.; Kelley, W.L.; Garcia-Gonzalo, D. Whole-genome sequencing and genetic analysis reveal novel stress responses to individual constituents of essential oils in Escherichia coli. Appl. Environ. Microbiol. 2018, 84, e02538-17. [Google Scholar] [CrossRef] [Green Version]
- Berdejo, D.; Pagán, E.; Merino, N.; Botello-Morte, L.; Pagán, R.; García-Gonzalo, D. Salmonella enterica serovar Typhimurium genetic variants isolated after lethal treatment with Thymbra capitata essential oil (TCO) showed increased resistance to TCO in milk. Int. J. Food Microbiol. 2021, 360, 109443. [Google Scholar] [CrossRef]
- Toledo-Arana, A.; Dussurget, O.; Nikitas, G.; Sesto, N.; Guet-Revillet, H.; Balestrino, D.; Loh, E.; Gripenland, J.; Tiensuu, T.; Vaitkevicius, K.; et al. The Listeria transcriptional landscape from saprophytism to virulence. Nature 2009, 459, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Glaser, P.; Frangeul, L.; Buchrieser, C.; Rusniok, C.; Amend, A.; Baquero, F.; Berche, P.; Bloecker, H.; Brandt, P.; Chakraborty, T.; et al. Comparative genomics of Listeria species. Science 2001, 294, 849–852. [Google Scholar] [CrossRef] [Green Version]
- Lachtara, B.; Wieczorek, K.; Osek, J. Genetic diversity and relationships of Listeria monocytogenes serogroup IIa isolated in Poland. Microorganisms 2022, 10, 532. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests For Bacteria That Grow Aerobically Approved Standard, 10th ed; CLSI Doc. M07-A10; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2015. [Google Scholar]
- Kohanski, M.A.; DePristo, M.A.; Collins, J.J. Sublethal antibiotic treatment leads to multidrug resistance via radical-induced mutagenesis. Mol. Cell 2010, 37, 311–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lallemand, E.A.; Lacroix, M.Z.; Toutain, P.-L.; Boullier, S.; Ferran, A.A.; Bousquet-Melou, A. In vitro degradation of antimicrobials during use of broth microdilution method can increase the measured minimal inhibitory and minimal bactericidal concentrations. Front. Microbiol. 2016, 7, 2051. [Google Scholar] [CrossRef] [Green Version]
- Berdejo, D.; Pagán, E.; Merino, N.; García-Gonzalo, D.; Pagán, R. Evolution assays for the isolation of mutant bacteria resistant to natural antimicrobials. In Detection and Enumeration of Bacteria, Yeast, Viruses, and Protozoan in Foods and Freshwater; Magnani, M., Ed.; Springer: New York, NY, USA, 2021; pp. 65–75. [Google Scholar]
- Andersson, D.I.; Hughes, D. Microbiological effects of sublethal levels of antibiotics. Nat. Rev. Microbiol. 2014, 12, 465–478. [Google Scholar] [CrossRef]
- Levin-Reisman, I.; Ronin, I.; Gefen, O.; Braniss, I.; Shoresh, N.; Balaban, N.Q. Antibiotic tolerance facilitates the evolution of resistance. Science 2017, 355, 826–830. [Google Scholar] [CrossRef]
- Dawson, R.M.C.; Elliott, D.C.; Elliott, W.H.; Jones, K.M. Data for Biochemical Research; Clarendon Press: Oxford, UK, 1989. [Google Scholar]
- Clinical and Laboratory Standards Institute. CLSI Doc. M100-S24; Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fourth Informational Supplement; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2014. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests, Approved Standard, 11th ed; CLSI Document M02-A11; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012. [Google Scholar]
- Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria, Approved Standard, 2nd ed; CLSI Document M45-A2; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2010. [Google Scholar]
- Yehia, H.M.; Elkhadragy, M.F.; Aljahani, A.H.; Alarjani, K.M. Prevalence and antibiotic resistance of Listeria monocytogenes in camel meat. Biosci. Rep. 2020, 40, BSR20201062. [Google Scholar] [CrossRef]
- de Souza, E.L.; da Cruz Almeida, E.T.; de Sousa Guedes, J.P. The potential of the incorporation of essential oils and their individual constituents to improve microbial safety in juices: A review. Compr. Rev. Food Sci. Food Saf. 2016, 15, 753–772. [Google Scholar] [CrossRef] [Green Version]
- Miladi, H.; Zmantar, T.; Chaabouni, Y.; Fedhila, K.; Bakhrouf, A.; Mahdouani, K.; Chaieb, K. Antibacterial and efflux pump inhibitors of thymol and carvacrol against food-borne pathogens. Microb. Pathog. 2016, 99, 95–100. [Google Scholar] [CrossRef]
- Abed, A.H.; Hegazy, E.F.; Omar, S.A.; Abd El-Baky, R.M.; El-Beih, A.A.; Al-Emam, A.; Menshawy, A.M.S.; Khalifa, E. Carvacrol essential oil: A natural antibiotic against zoonotic multidrug-resistant Staphylococcus species isolated from diseased livestock and humans. Antibiotics 2021, 10, 1328. [Google Scholar] [CrossRef]
- De Vincenzi, M.; Stammati, A.; De Vincenzi, A.; Silano, M. Constituents of aromatic plants: Carvacrol. Fitoterapia 2004, 75, 801–804. [Google Scholar] [CrossRef] [PubMed]
- Merino, N.; Berdejo, D.; Bento, R.; Salman, H.; Lanz, M.; Maggi, F.; Sánchez-Gómez, S.; García-Gonzalo, D.; Pagán, R. Antimicrobial efficacy of Thymbra capitata (L.) Cav. essential oil loaded in self-assembled zein nanoparticles in combination with heat. Ind. Crops Prod. 2019, 133, 98–104. [Google Scholar] [CrossRef]
- FDA; Hazard Analysis and Critical Control Point (HACCP). Procedures for the Safe and Sanitary Processing and Importing of Juice; Food and Drug Administration: Silver Spring, MD, USA, 2001; Volume 63, pp. 20450–20486. [Google Scholar]
- Cantón, R.; Morosini, M.-I. Emergence and spread of antibiotic resistance following exposure to antibiotics. FEMS Microbiol. Rev. 2011, 35, 977–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ait-Ouazzou, A.; Cherrat, L.; Espina, L.; Lorán, S.; Rota, C.; Pagán, R. The antimicrobial activity of hydrophobic essential oil constituents acting alone or in combined processes of food preservation. Innov. Food Sci. Emerg. Technol. 2011, 12, 320–329. [Google Scholar] [CrossRef]
- Field, D.; Daly, K.; O’Connor, P.M.; Cotter, P.D.; Hill, C.; Ross, R.P. Efficacies of nisin A and nisin V semipurified preparations alone and in combination with plant essential oils for controlling Listeria monocytogenes. Appl. Environ. Microbiol. 2015, 81, 2762–2769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, W.; Seng, Z.J.; Kohli, G.S.; Yang, L.; Yuk, H.-G. Stress resistance development and genome-wide transcriptional response of Escherichia coli O157:H7 adapted to sublethal thymol, carvacrol, and trans-cinnamaldehyde. Appl. Environ. Microbiol. 2018, 84, e01616–e01618. [Google Scholar] [CrossRef] [Green Version]
- Al-Mnaser, A.A.; Woodward, M.J. Sub-lethal concentrations of phytochemicals (carvacrol and oregano) select for reduced susceptibility mutants of Escherichia coli O23:H52. Pol. J. Microbiol. 2020, 69, 121–125. [Google Scholar] [CrossRef] [Green Version]
- Hauser, A.R. Antibiotic Basics for Clinicians: The ABCs of Choosing the Right Antibacterial Agent, 2nd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2018. [Google Scholar]
- Chaturongakul, S.; Boor Kathryn, J. RsbT and RsbV contribute to σB-dependent survival under environmental, energy, and intracellular stress conditions in Listeria monocytogenes. Appl. Environ. Microbiol. 2004, 70, 5349–5356. [Google Scholar] [CrossRef] [Green Version]
- Gomes Neto, N.J.; Magnani, M.; Chueca, B.; García-Gonzalo, D.; Pagán, R.; de Souza, E.L. Influence of general stress-response alternative sigma factors σS (RpoS) and σB (SigB) on bacterial tolerance to the essential oils from Origanum vulgare L. and Rosmarinus officinalis L. and pulsed electric fields. Int. J. Food Microbiol. 2015, 211, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-M.; Rock, C.O. Membrane lipid homeostasis in bacteria. Nat. Rev. Microbiol. 2008, 6, 222–233. [Google Scholar] [CrossRef] [PubMed]
- Bouyahya, A.; Abrini, J.; Dakka, N.; Bakri, Y. Essential oils of Origanum compactum increase membrane permeability, disturb cell membrane integrity, and suppress quorum-sensing phenotype in bacteria. J. Pharm. Anal. 2019, 9, 301–311. [Google Scholar] [CrossRef]
- Wijesundara, N.M.; Lee, S.F.; Cheng, Z.; Davidson, R.; Rupasinghe, H.P.V. Carvacrol exhibits rapid bactericidal activity against Streptococcus pyogenes through cell membrane damage. Sci. Rep. 2021, 11, 1487. [Google Scholar] [CrossRef] [PubMed]
- Churklam, W.; Chaturongakul, S.; Ngamwongsatit, B.; Aunpad, R. The mechanisms of action of carvacrol and its synergism with nisin against Listeria monocytogenes on sliced bologna sausage. Food Control 2020, 108, 106864. [Google Scholar] [CrossRef]
- Xue, J.; Miller, K.W. Regulation of the mpt operon in Listeria innocua by the ManR protein. Appl. Environ. Microbiol. 2007, 73, 5648–5652. [Google Scholar] [CrossRef] [Green Version]
- Buck, M.; Gallegos, M.T.; Studholme, D.J.; Guo, Y.; Gralla, J.D. The bacterial enhancer-dependent σ54(54) (σN) transcription factor. J. Bacteriol. 2000, 182, 4129–4136. [Google Scholar] [CrossRef] [Green Version]
- Arous, S.; Dalet, K.; Héchard, Y. Involvement of the mpo operon in resistance to class IIa bacteriocins in Listeria monocytogenes. FEMS Microbiol. Lett. 2004, 238, 37–41. [Google Scholar] [CrossRef]
- Vu-Khac, H.; Miller, K.W. Regulation of mannose phosphotransferase system permease and virulence gene expression in Listeria monocytogenes by the EIItMan transporter. Appl. Environ. Microbiol. 2009, 75, 6671–6678. [Google Scholar] [CrossRef] [Green Version]
- Gravesen, A.; Ramnath, M.; Rechinger, K.B.; Andersen, N.; Jänsch, L.; Héchard, Y.; Hastings, J.W.; Knøchel, S. High-level resistance to class IIa bacteriocins is associated with one general mechanism in Listeria monocytogenes. Microbiol. Read. Engl. 2002, 148, 2361–2369. [Google Scholar] [CrossRef] [Green Version]
- Joseph, B.; Mertins, S.; Stoll, R.; Schär, J.; Umesha, K.R.; Luo, Q.; Müller-Altrock, S.; Goebel, W. Glycerol metabolism and PrfA activity in Listeria monocytogenes. J. Bacteriol. 2008, 190, 5412–5430. [Google Scholar] [CrossRef] [PubMed]
| Strains | MIC (µL/L) 1 | MBC (µL/L) 1 |
|---|---|---|
| LmWT | 150 | 250 |
| LmSCar | 175 | 300 |
| LmLCar | 200 | 350 |
| Antibiotics | Strains | ||
|---|---|---|---|
| LmWT | LmSCar | LmLCar | |
| Kanamycin | 22.86 ± 0.99 | 23.20 ± 0.34 | 23.77 ± 1.80 |
| Tetracycline | 35.43 ± 0.76 | 37.99 ± 1.18 | 35.07 ± 0.40 |
| Chloramphenicol | 24.28 ± 0.92 | 25.99 ± 2.44 | 23.41 ± 0.97 |
| Nalidixic acid | 21.62 ± 1.22 | 21.21 ± 0.86 | 19.92 ± 1.14 |
| Rifampicin | 33.91 ± 0.97 | 33.71 ± 0.71 | 34.79 ± 1.12 |
| Norfloxacin | 22.03 ± 1.16 | 23.50 ± 0.43 | 24.52 ± 1.49 |
| Novobiocin | 31.18 ± 0.41 | 33.06 ± 0.51 | 33.38 ± 1.32 |
| Trimethoprim | 35.30 ± 1.05 | 34.94 ± 2.43 | 34.19 ± 0.44 |
| Ampicillin | 20.28 ± 0.14 | 23.94 ± 0.34 * | 18.47 ± 0.20 * |
| Cephalexin | 21.97 ± 1.32 | 25.04 ± 1.03 | 20.63 ± 1.61 |
| Genome Position | Locus Tag | Gene | Mutation * | Change | Information |
|---|---|---|---|---|---|
| 928,651 | lmo0891 | rsbT | SNV: T341C | Phe114Ser | Positive regulation of sigma-B activity |
| 2,291,818 | lmo2202 | SNV: C110A | Thr37Asn | 3-oxoacyl ACP synthase |
| Genome Position | Locus Tag | Gene | Mutation * | Change | Information |
|---|---|---|---|---|---|
| 810,506 | lmo0785 | manR | SNV: T287G | Leu96Arg | Transcriptional regulator |
| 1,575,317 | lmo1539 | glpF1 | Ins: +T 423 | Gly142 Frameshift | Glycerol transporter |
| 1,870,663 | lmo1799 | SNV: G1581T | Silent mutation (Ala527) | Peptidoglycan binding protein | |
| 1,996,626 | lmo1921 | Del: -T 123 | Ile41 Frameshift | Hypothetical protein |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berdejo, D.; Gayán, E.; Pagán, E.; Merino, N.; Campillo, R.; Pagán, R.; García-Gonzalo, D. Carvacrol Selective Pressure Allows the Occurrence of Genetic Resistant Variants of Listeria monocytogenes EGD-e. Foods 2022, 11, 3282. https://doi.org/10.3390/foods11203282
Berdejo D, Gayán E, Pagán E, Merino N, Campillo R, Pagán R, García-Gonzalo D. Carvacrol Selective Pressure Allows the Occurrence of Genetic Resistant Variants of Listeria monocytogenes EGD-e. Foods. 2022; 11(20):3282. https://doi.org/10.3390/foods11203282
Chicago/Turabian StyleBerdejo, Daniel, Elisa Gayán, Elisa Pagán, Natalia Merino, Raúl Campillo, Rafael Pagán, and Diego García-Gonzalo. 2022. "Carvacrol Selective Pressure Allows the Occurrence of Genetic Resistant Variants of Listeria monocytogenes EGD-e" Foods 11, no. 20: 3282. https://doi.org/10.3390/foods11203282





