Attitudes towards Prosthodontic Clinical Decision-Making for Edentulous Patients among South West Deanery Dental Foundation Year One Dentists
Abstract
:1. Introduction
- ⚫
- Paternalism (traditionally the clinician makes decisions for the patient);
- ⚫
- Consumerism (primarily based upon patient preferences); and
- ⚫
- Shared decision making (whereby a consensus is reached).
2. Methods
2.1. Questionnaire Development
2.2. Study Sample
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Charles, C.; Gafni, A.; Whelan, T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Soc. Sci. Med. 1997, 44, 681–692. [Google Scholar] [CrossRef]
- General Dental Council (GDC). Standards for the Dental Team; General Dental Council: London, UK, 2013; Available online: http://www.gdc-uk.org/Dentalprofessionals/Standards/Documents/Standards%20for%20the%20Dental%20Team (accessed on 10 May 2015).
- Montgomery, A.; Fahey, T. How do patients’ treatment preferences compare with those of clinicians? Qual. Health Care 2001, 10, 39–43. [Google Scholar] [CrossRef]
- Brown, R.; Butow, P.; Wilson-Genderson, M.; Bernhard, J.; Ribi, K.; Juraskova, I. Meeting the decision-making preferences of patients with breast cancer in oncology consultations: Impact on decision-related outcomes. J. Clin. Oncol. 2012, 30, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Joosten, E.; Defuentes-Merillas, L.; De Weert, G.; Sensky, T.; Van Der Staak, C.; De Jong, C. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother. Psychosom. 2008, 77, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Feine, J.; Lund, J. Measuring chewing ability in randomized controlled trials with edentulous populations wearing implant prostheses. J. Oral Rehabil. 2006, 33, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Mckay, J.; Quinonez, C. The feminization of dentistry: Implications for the profession. J. Can. Dent. Assoc. 2012, 78, c1. [Google Scholar] [PubMed]
- Roter, D.; Hall, J. Why physician gender matters in shaping the physician-patient relationship. J. Women’s Health 1998, 7, 1093–1097. [Google Scholar] [CrossRef]
- Harris, D.; Hofer, S.; O’Boyle, C.; Sheridan, S.; Marley, J.; Benington, I.; Clifford, T.; Houston, F.; O’Connell, B. A comparison of implant-retained mandibular overdentures and conventional dentures on quality of life in edentulous patients: A randomized, prospective, within-subject controlled clinical trial. Clin. Oral Implant. Res. 2011, 24, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Stoker, G.; Wismeijer, D.; Van Waas, M. An eight-year follow-up to a randomized clinical trial of aftercare and cost-analysis with three types of mandibular implant-retained overdentures. J. Dent. Res. 2007, 86, 276–280. [Google Scholar] [CrossRef] [PubMed]
- McHarg, J.; Kay, E. Designing a dental curriculum for the twenty-first century. Br. Dent. J. 2009, 207, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; McHarg, J.; Kay, E.; Moles, D.; Tredwin, C.; Coombes, L.; Heffernan, E. Academic environment in a newly established dental school with an enquiry-based curriculum: Perceptions of students from the inaugural cohorts. Eur. J. Dent. Educ. 2012, 16, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Koka, S.; Eckert, S.; Choi, Y.; Montoriv, M. Clinical decision-making practices among a subset of North American prosthodontists. Int. J. Prosthodont. 2007, 20, 606–608. [Google Scholar] [PubMed]
- Committee of Postgraduate Dental Deans and Directors (COPDEND). A Curriculum for UK Dental Foundation Programme Training; COPDEND: Manchester, UK, 2012; Available online: http://www.copdend.org/data/files/Foundation/Dental%20Foundation%20Programme%20Curriculum (accessed on 10 May 2015).
- Puleo, E.; Zapka, J.; White, M.; Mouchawar, J.; Somkin, C.; Taplin, S. Caffeine, cajoling, and other strategies to maximize clinician survey response rates. Eval. Health Prof. 2002, 25, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Shelley, A.; Brunton, P.; Horner, K. Questionnaire surveys of dentists on radiology. Dentomaxillofac. Radiol. 2012, 41, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Houtkoop-Steenstra, H. Interaction and the Standardized Survey Interview: The Living Questionnaire; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 22, 1–55. [Google Scholar]
- Ary, D.; Jacob, L.; Razavieh, A.; Sorensen, C. Introduction to Research in Education; Cengage Learning: London, UK, 2009. [Google Scholar]
- Kumar, R. Research Methodology: A Step-By-Step Guide for Beginners; Sage Publications: London, UK, 2010. [Google Scholar]
- Boynton, P. Administering, analysing, and reporting your questionnaire. Br. Med. J. 2004, 328, 1372–1375. [Google Scholar] [CrossRef] [PubMed]
- Podsakoff, P.; Mackenzie, S.; Lee, J.; Podsakoff, N. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]
- Duguid, R.; Drummondm, J. The admission of students to UK dental schools-recent trends (1983–1998). Eur. J. Dent. Educ. 2000, 4, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Adult Dental Health Survey 2009—Summary Report and Thematic Series 2009. The NHS Information Centre: Leeds, UK, 2009. Available online: http://www.ic.nhs.uk/pubs/dentalsurveyfullreport09 (accessed on 10 May 2015).
- Pau, A.; Croucher, R. Emotional intelligence and perceived stress in dental undergraduates. J. Dent. Educ. 2003, 67, 1023–1028. [Google Scholar] [PubMed]
- Chapple, H.; Shah, S.; Caress, A.; Kay, E. Exploring dental patients' preferred roles in treatment decision-making—A novel approach. Br. Dent. J. 2003, 194, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Dental Protection Limited (DPL). Dental Advice Series—Consent. Suitable for UK Excluding Scotland; DPL: London, UK, 2012; Available online: http://www.dentalprotection.org/docs/librariesprovider4/dental-advice-booklets/consent---excluding-scotland.pdf?sfvrsn=10 (accessed on 10 May 2015).
- Furley, P.; Dicks, M.; Memmert, D. Non-verbal behavior in soccer: The influence of dominant and submissive body language on the impression formation and expectancy of success of soccer players. JSEP 2012, 34, 61–82. [Google Scholar]
- Pine, C.; McGoldrick, P. Application of behavioural sciences teaching by UK dental undergraduates. Eur. J. Dent. Educ. 2000, 4, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.; Radord, D.; Juszczyk, A. Current trends in complete denture teaching in British dental schools. Br. Dent. J. 2010, 208, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wieder, M.; Faigenblum, M.; Eder, A.; Louca, C. An investigation of complete denture teaching in the UK: Part 2. The DF1 experience. Br. Dent. J. 2013, 215, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Lynch, C.; Sloan, A.; Gilmour, A. Treatment planning for replacing missing teeth in UK general dental practice: Current trends. J. Oral Rehabil. 2010, 37, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Andrews, K.; Penny, J.; King, P. Are patients referred for NHS-funded dental implant treatment being selected in accordance with national guidelines and subsequently funded by their primary care trust? Ann. R. Coll. Surg. Engl. 2010, 92, 512–514. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ritzer, G. The “McDonaldization” of society. J. Am. Cult. 1983, 6, 100–107. [Google Scholar] [CrossRef]
- Parker, M. A perspective on doctor-patient communication in the dental office. N. C. Med. J. 2007, 68, 365–367. [Google Scholar] [PubMed]
- Shalowitz, D.; Garrett-Mayer, E.; Wendler, D. The accuracy of surrogate decision makers: A systematic review. Arch. Intern. Med. 2006, 166, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Retamero, R.; Galesic, M. Doc, what would you do if you were me? On self-other discrepancies in medical decision making. J. Exp. Psychol. 2012, 18, 38–51. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Retamero, R.; Galesic, M. On defensive decision making: How doctors make decisions for their patients. Health Expect. 2014, 17, 664–669. [Google Scholar] [CrossRef] [PubMed]
- Koele, P.; Hoogstraten, J. Determinants of dentists’ decisions to initiate dental implant treatment: A judgment analysis. J. Prosthet. Dent. 1999, 81, 476–480. [Google Scholar] [CrossRef]

| Question Number | Median Response on Likert Scale (Interquartile Range) | p-Value (Mann-Whitney U Test of Association between Gender and Response) | ||
|---|---|---|---|---|
| Overall | Male | Female | ||
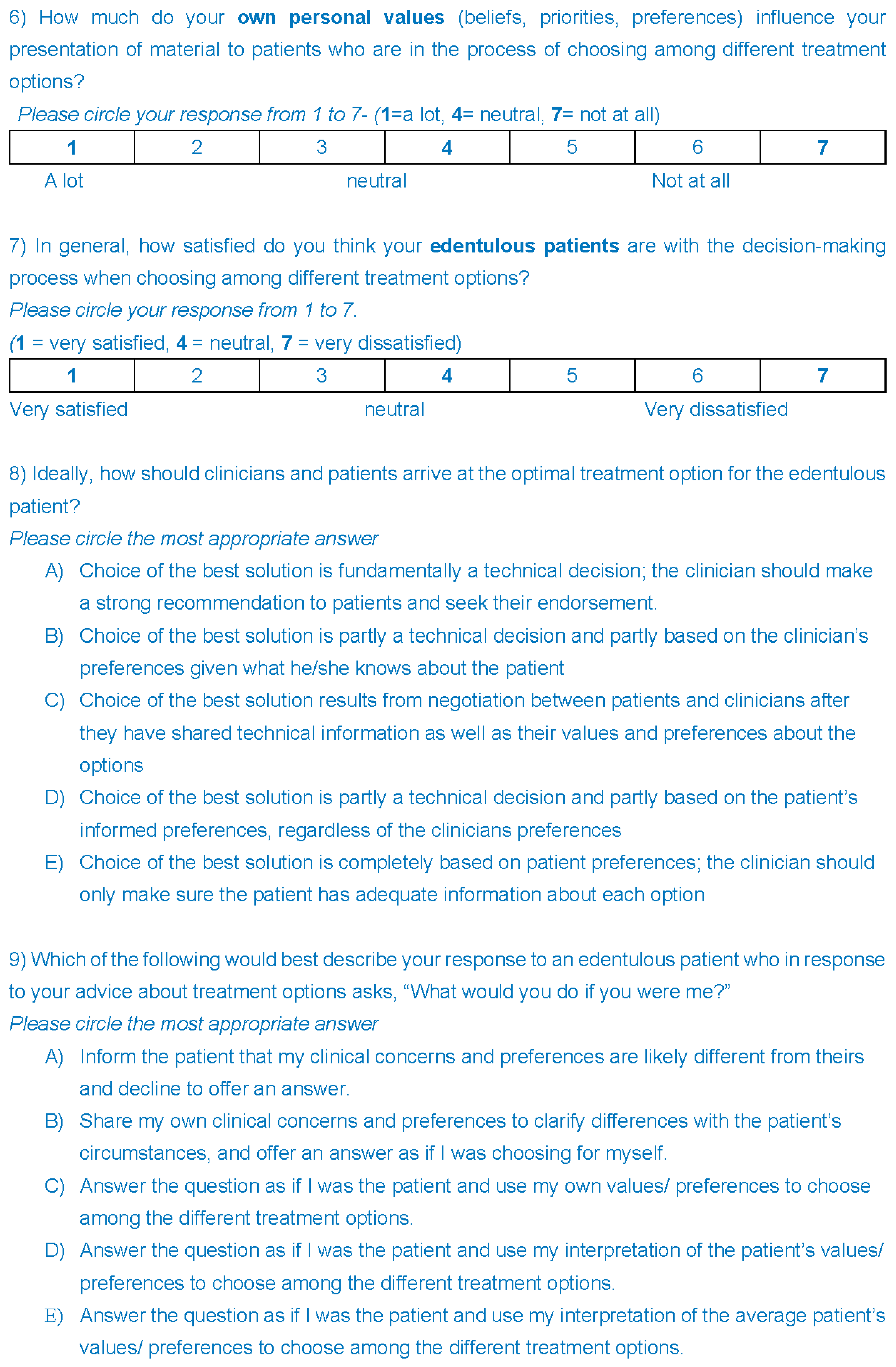
| 3 | 3(2,4) | 3(2,4) | 3.5(2,4) | p = 0.8 |
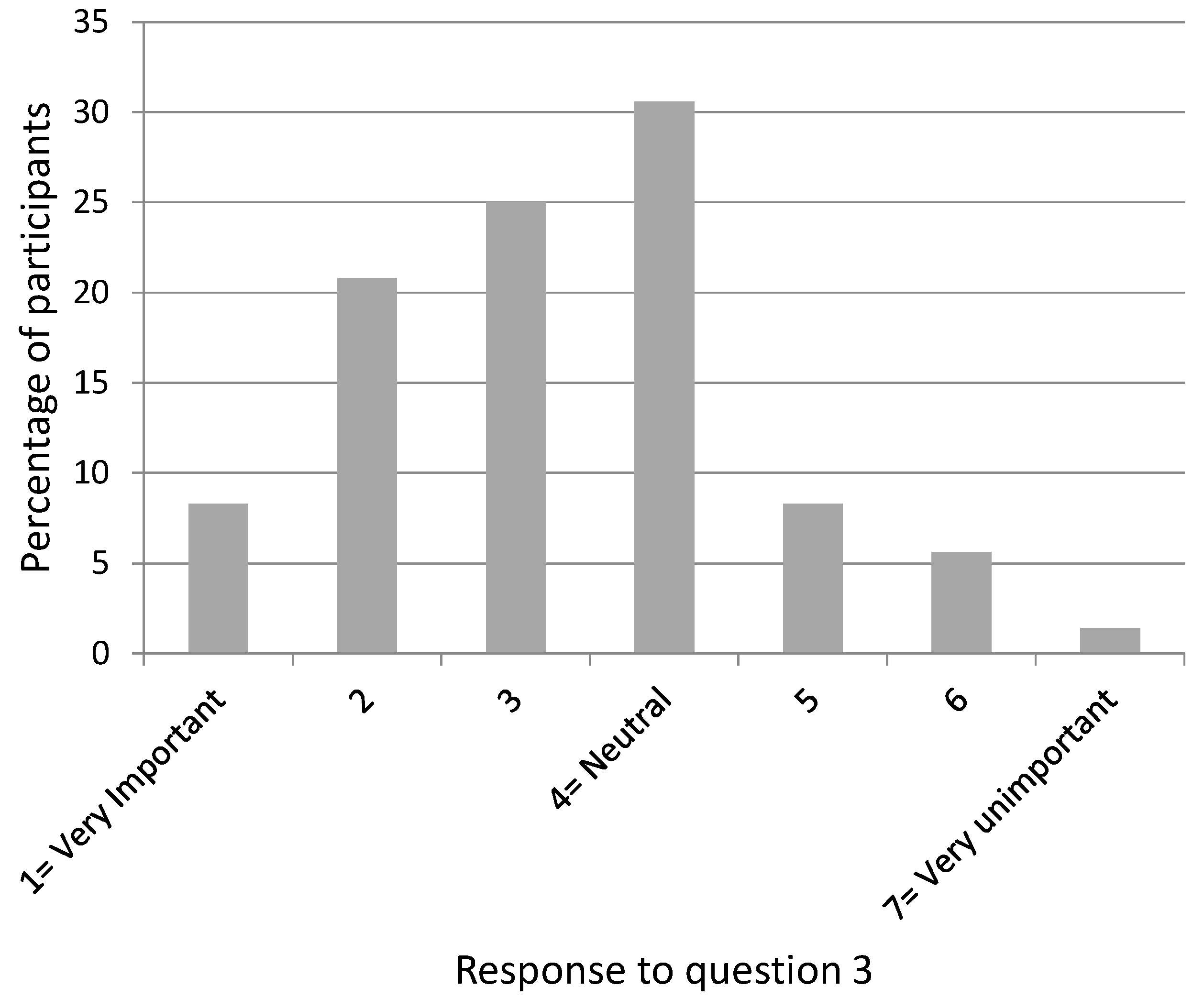
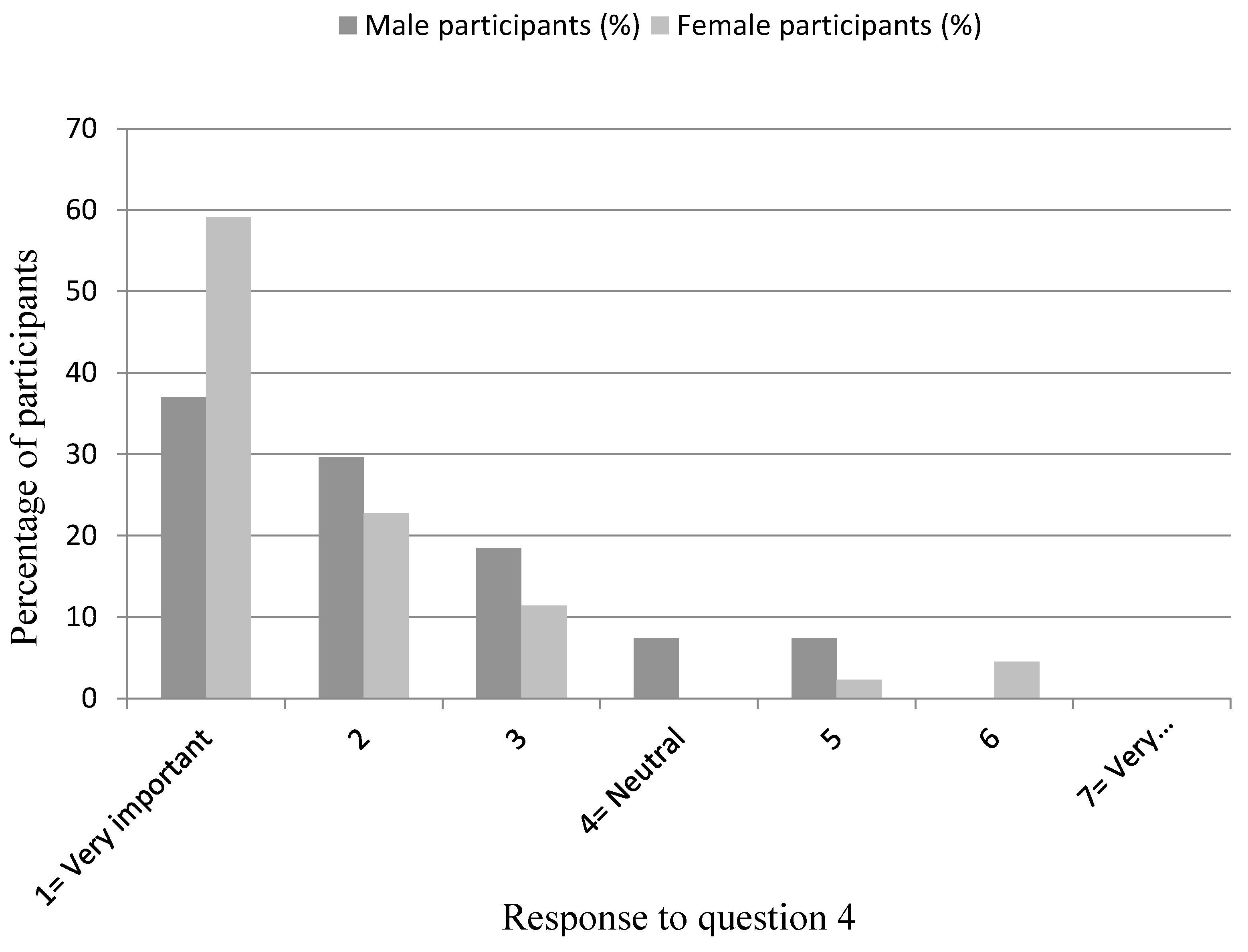
| 4 | 1(1,2) | 2(1,3) | 1(1,2) | p = 0.07 |
| 5 | 3(3,4) | 4(3,5) | 3(2,4) | p = 0.3 |
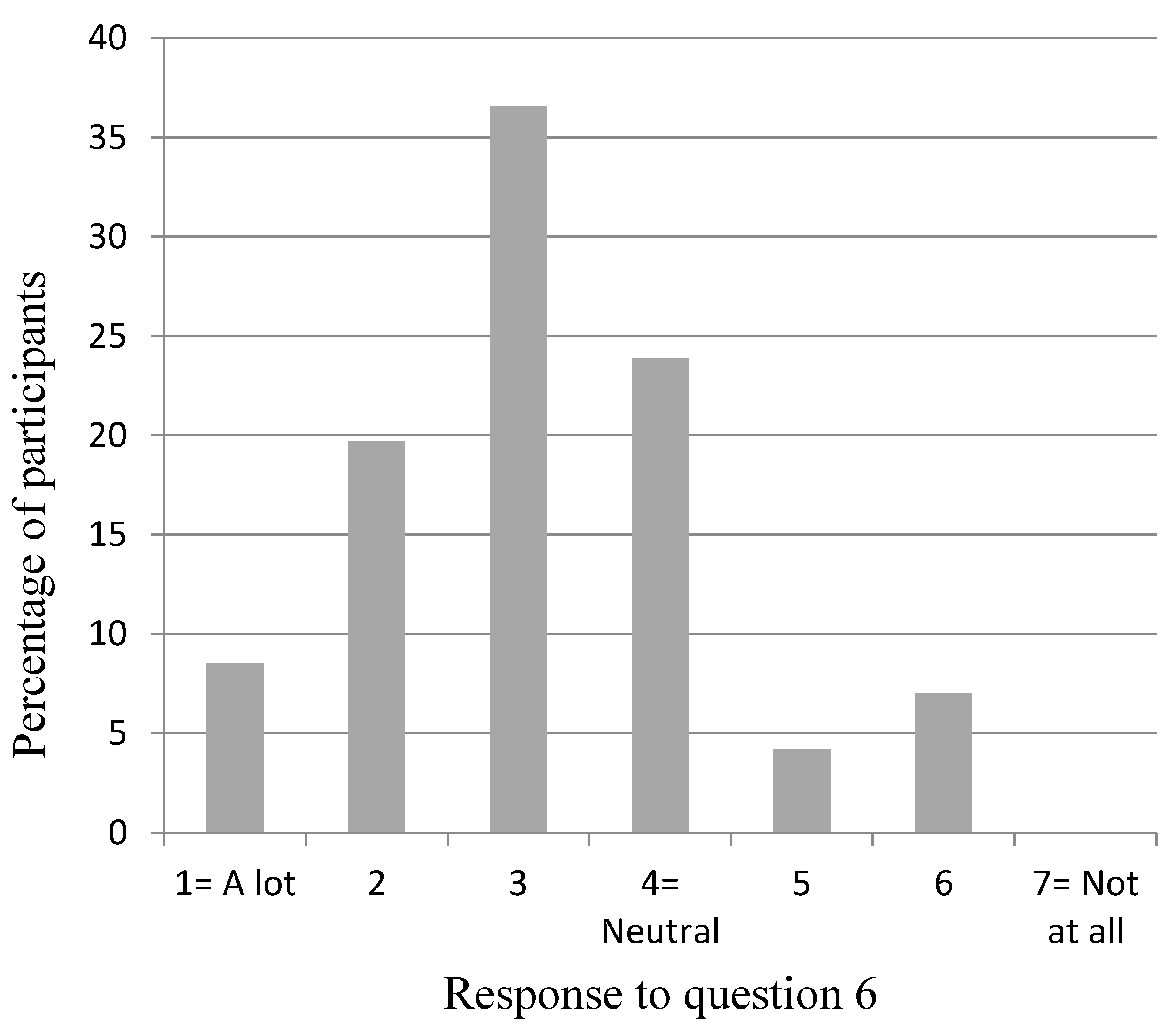
| 6 | 3(2,4) | 3(3,4) | 3(2,4) | p = 0.3 |
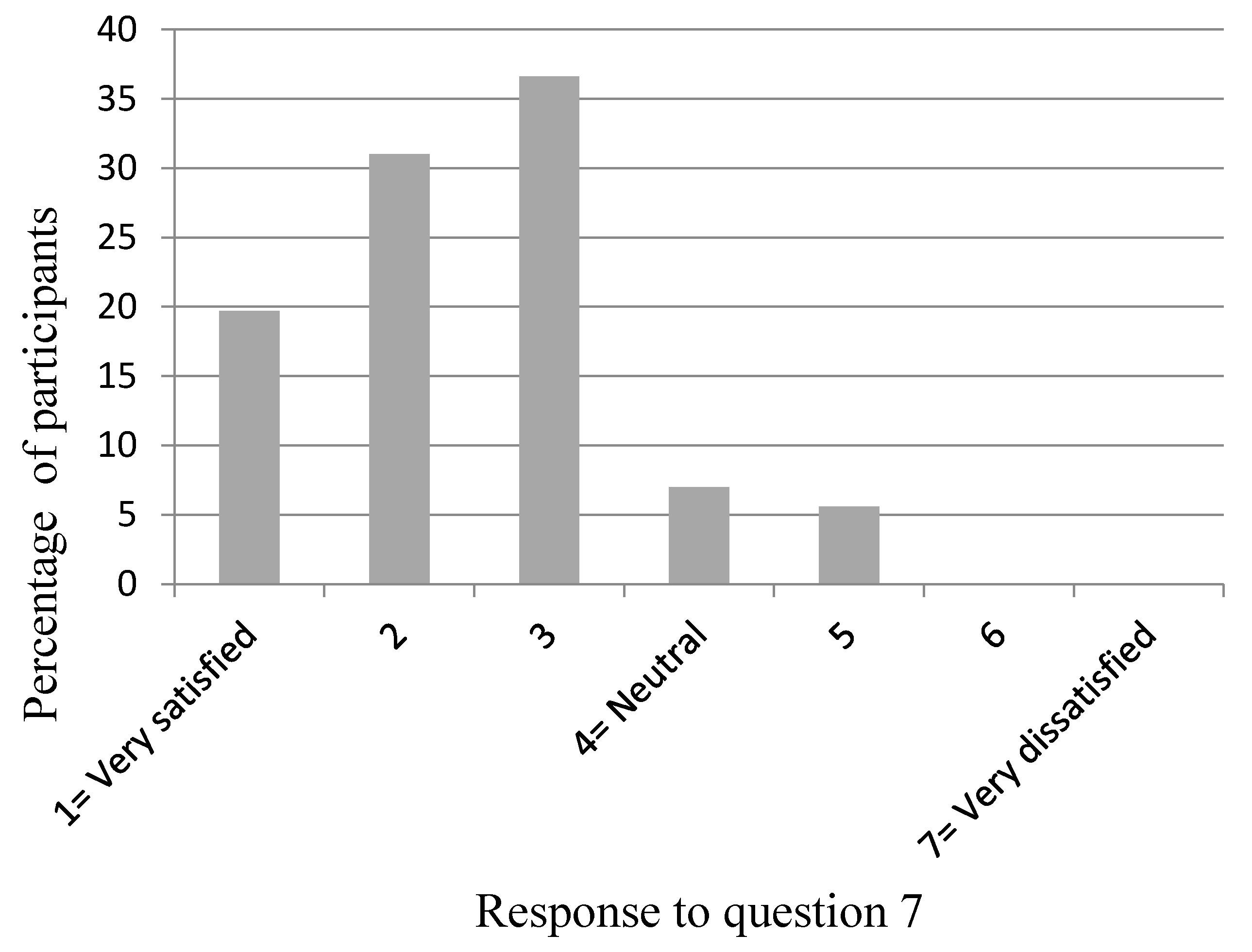
| 7 | 2(2,3) | 2(1,3) | 3(2,3) | p = 0.6 |
| Response Chosen by Participant | Percentage of Participants | ||
|---|---|---|---|
| Overall | Male | Female | |
| No response given | 4.3 | 3.7 | 4.6 |
| (A) Choice of the best solution is fundamentally a technical decision; the clinician should make a strong recommendation to patients and seek their endorsement | 0 | 0 | 0 |
| (B) Choice of the best solution is partly a technical decision and partly based on the clinician’s preferences given what he/she knows about the patient | 2.8 | 7.4 | 0 |
| (C) Choice of the best solution results from negotiation between patients and clinicians after they have shared technical information as well as their values and preferences about the options | 57.7 | 59.3 | 56.8 |
| (D) Choice of the best solution is partly a technical decision and partly based on the patient’s informed preferences, regardless of the clinicians preferences | 28.2 | 25.9 | 29.5 |
| (E) Choice of the best solution is completely based on patient preferences; the clinician should only make sure the patient has adequate information about each option | 7 | 3.7 | 9.1 |
| Response Chosen by Participant | Percentage of Participants | ||
|---|---|---|---|
| Overall | Male | Female | |
| No response given | 4.2 | 3.7 | 4.5 |
| (A) Inform the patient that my clinical concerns and preferences are likely different from theirs and decline to offer an answer. | 23.9 | 22.2 | 25.0 |
| (B) Share my own clinical concerns and preferences to clarify differences with the patient’s circumstances, and offer an answer as if I was choosing for myself. | 38.0 | 40.7 | 36.4 |
| (C) Answer the question as if I was the patient and use my own values/ preferences to choose among the different treatment options. | 16.9 | 11.1 | 20.5 |
| (D) Answer the question as if I was the patient and use my interpretation of the patient’s values/preferences to choose among the different treatment options. | 12.7 | 22.3 | 6.8 |
| (E) Answer the question as if I was the patient and use my interpretation of the average patient’s values/preferences to choose among the different treatment options. | 4.3 | 0 | 6.8 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barber, A.; Puryer, J.; Leary, S.; McNally, L.; O’Sullivan, D. Attitudes towards Prosthodontic Clinical Decision-Making for Edentulous Patients among South West Deanery Dental Foundation Year One Dentists. Dent. J. 2016, 4, 12. https://doi.org/10.3390/dj4020012
Barber A, Puryer J, Leary S, McNally L, O’Sullivan D. Attitudes towards Prosthodontic Clinical Decision-Making for Edentulous Patients among South West Deanery Dental Foundation Year One Dentists. Dentistry Journal. 2016; 4(2):12. https://doi.org/10.3390/dj4020012
Chicago/Turabian StyleBarber, Andrew, James Puryer, Sam Leary, Lisa McNally, and Dominic O’Sullivan. 2016. "Attitudes towards Prosthodontic Clinical Decision-Making for Edentulous Patients among South West Deanery Dental Foundation Year One Dentists" Dentistry Journal 4, no. 2: 12. https://doi.org/10.3390/dj4020012
APA StyleBarber, A., Puryer, J., Leary, S., McNally, L., & O’Sullivan, D. (2016). Attitudes towards Prosthodontic Clinical Decision-Making for Edentulous Patients among South West Deanery Dental Foundation Year One Dentists. Dentistry Journal, 4(2), 12. https://doi.org/10.3390/dj4020012






