Correlations of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and Three Panoramic Indices Using Quantitative Ultrasound (QUS) Bone Densitometry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Osteoporosis Self-Assessment Tool for Asians (OSTA)
2.2. Measurement of the Three Panoramic Indices
2.3. Bone Densitometry, Body Mass Index, and Number of Remaining Teeth
2.4. Statistical Analyses
3. Results
4. Discussion
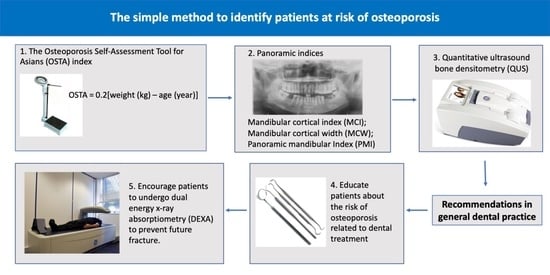
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yu, B.; Wang, C.Y. Osteoporosis and periodontal diseases—An update on their association and mechanistic links. Periodontology 2000 2022, 89, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Kiswanjaya, B.; Saraswati, I.; Wijanarko, A.P.; Syahraini, S.I.; Bachtiar-Iskandar, H.H. Relationship between vertical mandibular bone atrophy and the number of remaining teeth in elderly Indonesian individuals. J. Stomatal. 2018, 71, 333–338. [Google Scholar] [CrossRef]
- Marcello-Machado, R.M.; Faot, F.; Schuster, A.J.; Bielemann, A.M.; Chagas Júnior, O.L.; Del Bel Cury, A.A. How does mandibular bone atrophy influence the masticatory function, OHRQoL and satisfaction in overdenture wearers? Clinical results until 1-year post-loading. J. Oral Rehabil. 2017, 44, 850–859. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Campion, G.; Melton, L.J., III. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef]
- Kusama, T.; Nakazawa, N.; Kiuchi, S.; Kondo, K.; Osaka, K.; Aida, J. Dental prosthetic treatment reduced the risk of weight loss among older adults with tooth loss. J. Am. Geriatr. Soc. 2021, 69, 2498–2506. [Google Scholar] [CrossRef]
- Koh, L.K.H.; Ben Sedrine, W.; Torralba, T.P.; Kung, A.; Fujiwara, S.; Chan, S.P.; Huang, Q.R.; Rajatanavin, R.; Tsai, K.S.; Park, H.M.; et al. A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos. Int. 2001, 12, 699–705. [Google Scholar] [CrossRef]
- Sherchan, B.; Lamichhane, A.; Mahara, D.P. Osteoporosis Self-Assessment Tool for Asians (OSTA) index in comparison to quantitative ultrasound of the calcaneal in predicting low bone density. Nepal Orthop. Assoc. J. 2013, 3, 20–25. [Google Scholar] [CrossRef]
- Patel, S.M.; Jadhav, P.R.; Vieira, A. Association of OSTA index with bone mineral density (BMD) and its comparison with calcaneal quantitative ultrasound for the prediction of low BMD in peri-menopausal Indian women. Int. J. Res. Med. Sci. 2014, 2, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Chin, K.Y.; Low, N.Y.; Kamaruddin, A.A.A.; Dewiputri, W.I.; Soelaiman, I.N. Agreement between calcaneal quantitative ultrasound and Osteoporosis Self-Assessment Tool for Asians in identifying individuals at risk of osteoporosis. Ther. Clin. Risk Manag. 2017, 13, 1333–1341. [Google Scholar] [CrossRef] [Green Version]
- Klemetti, E.; Kolmakov, S.; Kröger, H. Pantomography in assessment of the osteoporosis risk group. Eur. J. Oral Sci. 1994, 102, 68–72. [Google Scholar] [CrossRef]
- Taguchi, A.; Suei, Y.; Ohtsuka, M.; Otani, K.; Tanimoto, K.; Ohtaki, M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women: Width and morphology of inferior cortex of the mandible. Dentomaxillofacial Radiol. 1996, 25, 263–267. [Google Scholar] [CrossRef]
- Benson, B.W.; Prihoda, T.J.; Glass, B.J. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg. Oral Med. Oral Pathol. 1991, 71, 349–356. [Google Scholar] [CrossRef]
- Krugh, M.; Langaker, M.D. Dual Energy X-ray Absorptiometry; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519042/ (accessed on 10 September 2022).
- Consensus Development Statement. Who are candidates for prevention and treatment for osteoporosis? Osteoporos. Int. 1997, 7, 1–6. [Google Scholar] [CrossRef]
- Taguchi, A.; Ohtsuka, M.; Tsuda, M.; Nakamoto, T.; Kodama, I.; Inagaki, K.; Noguchi, T.; Kudo, Y.; Suei, Y.; Tanimoto, K. Risk of vertebral osteoporosis in post-menopausal women with alterations of the mandible. Dentomaxillofacial Radiol. 2007, 36, 143–148. [Google Scholar] [CrossRef]
- Drozdzowska, B.; Pluskiewicz, W.; Tarnawska, B. Panoramic-based mandibular indices in relation to mandibular bone mineral density and skeletal status assessed by dual-energy X-ray absorptiometry and quantitative ultrasound. Dentomaxillofacial Radiol. 2002, 31, 361–367. [Google Scholar] [CrossRef]
- Ledgerton, D.; Horner, K.; Devlin, H.; Worthington, H. Radiomorphometric indices of the mandible in a British female population. Dentomaxillofacial Radiol. 1999, 28, 173–181. [Google Scholar] [CrossRef]
- Taguchi, A.; Suei, Y.; Sanada, M.; Ohtsuka, M.; Nakamoto, T.; Sumida, H.; Ohama, K.; Tanimoto, K. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. Am. J. Roentgenol. 2004, 183, 1755–1760. [Google Scholar] [CrossRef]
- Papamanthos, M.; Varitimidis, S.E.; Dailiana, Z.H.; Kogia, E.I.; Malizos, K.N. Computer-assisted evaluation of mandibular cortical width (MCW) index as an indicator of osteoporosis. Hippokratia 2014, 18, 251–257. [Google Scholar]
- Kiswanjaya, B.; Yoshihara, A.; Deguchi, T.; Hanada, N.; Miyazaki, H. Relationship between the mandibular inferior cortex and bone stiffness in elderly Japanese people. Osteoporos. Int. 2010, 21, 433–438. [Google Scholar] [CrossRef]
- Kiswanjaya, B.; Priaminiarti, M.; Bachtiar-Iskandar, H.H. Three panoramic indices for identification of healthy older people at a high risk of osteoporosis. Saudi Dent. J. 2022, 34, 503–508. [Google Scholar] [CrossRef]
- Chin, K.Y.; Soelaiman, I.N.; Mohamed, I.N.; Ibrahim, S.; Wan Ngah, W.Z. The effects of age, physical activity level, and body anthropometry on calcaneal speed of sound value in men. Arch. Osteoporos. 2012, 7, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Zha, X.Y.; Hu, Y.; Pang, X.N.; Chang, G.L.; Li, L. Diagnostic value of Osteoporosis Self-Assessment Tool for Asians (OSTA) and quantitative bone ultrasound (QUS) in detecting high-risk populations for osteoporosis among elderly Chinese men. J. Bone Miner. Metab. 2015, 33, 230–238. [Google Scholar] [CrossRef] [PubMed]



| Variable | Men (n = 190) | Women (n = 197) | p-Value | ||
|---|---|---|---|---|---|
| Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | ||
| Age (in years) | 58.99 ± 6.7 | 58 (50–70) | 61.97 ± 4.9 | 63 (50–70) | <0.001 * |
| Quantitative ultrasound (QUS) | |||||
| Speed of sound (SOS) (m/s) | 1537.41 ± 21.5 | 1534 (1486–1601) | 1518.36 ± 20.8 | 1515 (1489–1707) | <0.001 * |
| Calcaneus broadband attenuation of sound (BUA) (dB MHz) | 104.59 ± 11.6 | 103.6 (70.2–139.3) | 91.24 ± 7.9 | 90.4 (66.7–124) | <0.001 * |
| Stiffness index (%) | 80.55 ± 13.1 | 78.83 (46.5–113.8) | 66.27 ± 9.1 | 64.79 (45.8–107.7) | <0.001 * |
| z-score | −0.03 ± 1.2 | −0.16 (−3–3.3) | 0.04 ± 0.8 | −0.07 (−2.2–3.4) | not significant |
| t-score | −1.39 ± 1.1 | −1.5 (−4.1–1.7) | −1.99 ± 0.7 | −2.08 (−3.9–1) | <0.001 * |
| Panoramic radiography | |||||
| Mandibular cortical index (MCI) | |||||
| Class 1 | 134 (70.6%) | 34 (17.3%) | <0.001 ** | ||
| Class 2 | 47 (24.7%) | 131 (66.5%) | |||
| Class 3 | 9 (4.7%) | 32 (16.2%) | |||
| Mandibular cortical width (MCW) (mm) | 3.22 ± 0.6 | 3.32 (1.3–4.3) | 3.11 ± 0.6 | 3.17 (1.7–4.6) | <0.001 * |
| Panoramic mandibular index (PMI) | 0.28 ± 0.05 | 0.29 (0.12–0.37) | 0.27 ± 0.05 | 0.28 (0.12–0.37) | not significant |
| Osteoporosis Self-Assessment Tool for Asians (OSTA): | |||||
| Low risk (OSTA > −1) | 110 (57.9%) | 40 (20.3%) | <0.001 ** | ||
| Medium risk (−4 < OSTA < −1) | 61 (32.1%) | 72 (36.6%) | |||
| High risk (OSTA <−4) | 19 (10%) | 85 (43.1%) | |||
| Body mass index (kg/m2) | 21.85 ± 2.8 | 21.96 (14.6–28.5) | 22.16 ± 3.37 | 21.98 (15–31.8) | not significant |
| Number of remaining teeth | 15.41 ± 10 | 16.5 (0–32) | 15.75 ± 9.3 | 17 (0–32) | not significant |
| Variable | Low Risk (OSTA > −1) | Medium Risk (−4 < OSTA < −1) | High Risk (OSTA < −4) | p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | ||
| Age (in years) | 54.9 ± 4.4 | 54 (50–67) | 63.41 ± 5.1 | 65 (52–70) | 68.53 ± 2.6 | 69 (61–70) | <0.001 * |
| Quantitative ultrasound (QUS) | |||||||
| Speed of sound (SOS) (m/s) | 1545.69 ± 18.9 | 1542 (1510–1593) | 1529.28 ± 19.8 | 1526 (1486–1601) | 1515.53 ± 15.1 | 1515 (149–1543) | <0.001 * |
| Calcaneus broadband attenuation of sound (BUA) (dB MHz) | 110.5 ± 9.2 | 108.8 (96–139.3) | 98.76 ± 8.4 | 98.5 (75.2–122.2) | 89.12 ± 9.6 | 90.2 (70.2–110) | <0.001 ** |
| Stiffness index (%) | 86.83 ± 10.7 | 84.58 (69.1–113.8) | 74.37 ± 10.6 | 73.2 (46.5–107.9) | 64.05 ± 9.4 | 63.1 (52.6–85.7) | <0.001 * |
| z-score | 0.56 ± 0.9 | 0.37 (−0.9–3.3) | −0.6 ± 0.9 | −0.69 (−2.8–2) | −1.5 ± 0.8 | −1.5 (−3–0.4) | <0.001 ** |
| t-score | −0.85 ± 0.9 | −1.02 (−2.2–1.7) | −1.9 ± 0.8 | −1.99 (−4–0.5) | −2.77 ± 0.8 | −2.79 (−4.1– −0.9) | <0.001 ** |
| Panoramic radiography | |||||||
| Mandibular cortical index (MCI) | |||||||
| Class 1 | 86 (78.2%) | 38 (62.3%) | 10 (52.6%) | <0.005 *** | |||
| Class 2 | 23 (20.9%) | 19 (31.1%) | 5 (26.3%) | ||||
| Class 3 | 1 (0.9%) | 4 (6.6%) | 4 (21.1%) | ||||
| Mandibular cortical width (MCW) (mm) | 3.36 ± 0.4 | 3.38 (1.6–4.3) | 3.11 ± 0.7 | 3.2 (1.6–4.3) | 2.72 ± 0.7 | 2.85 (1.3–3.8) | <0.005 * |
| Panoramic mandibular index (PMI) | 0.296 ± 0.03 | 0.29 (0.22–0.37) | 0.266 ± 0.05 | 0.275 (0.17–0.35) | 0.253 ± 0.06 | 0.25 (0.12–0.36) | <0.05 * |
| Body mass index (kg/m2) | 23.15 ± 2.1 | 23.1 (18.7–28.5) | 20.46 ± 2.2 | 20.8 (15.7–15.2) | 18.79 ± 3.1 | 18.6 (14.6–25.9) | <0.001 * |
| No. of remaining teeth | 16.64 ± 9.8 | 20 (0–32) | 14.15 ± 9.8 | 14 (0–30) | 12.32 ± 10.6 | 8 (0–31) | Not significant |
| Variable | Low Risk (OSTA > −1) | Medium Risk (−4 < OSTA < −1) | High Risk (OSTA < −4) | p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | ||
| Age (in years) | 55.75 ± 3.86 | 55 (50–63) | 61.14 ± 3.6 | 66 (59–70) | 65.61 ± 2.6 | 66 (59–70) | <0.001 * |
| Quantitative ultrasound (QUS) | |||||||
| Speed of sound (SOS) (m/s) | 1529.48 ± 20.3 | 1527 (1502–1592) | 1521.38 ± 25.4 | 1518 (1492–1707) | 1510.56± 12.1 | 1510 (1489–1556) | <0.001 * |
| Calcaneus broadband attenuation of sound (BUA) (dB MHz) | 100 ± 7.3 | 99.1 (87.1–124) | 91.93 ± 6,2 | 91.8 (72.6–109.8) | 86.49 ± 5.2 | 86.8 (66.7–106.4) | <0.001 * |
| Stiffness index (%) | 86.83 ± 10.7 | 84.58 (69.1–113.8) | 74.37 ± 10.6 | 73.2 (46.5–107.9) | 64.05 ± 9.4 | 63.1 (52.6–85.7) | <0.001 * |
| z-score | 0.95 ± 0.8 | 0.79 (−0.09–3.4) | 0.13 ± 0.6 | 0.07 (−1.6–1.8) | −0.46 ± 0.5 | −0.45 (−2.2–1.8) | <0.001 * |
| t-score | −1.19 ± 0.7 | −1.33 (−2.1–1.02) | −1.91 ± 0.5 | −1.96 (−3.4–−0.4) | −2.43 ± 0.8 | −2.43 (−3.9–−0.4) | <0.001 * |
| Panoramic radiography | |||||||
| Mandibular cortical index (MCI) | Not significant | ||||||
| Class 1 | 7 (17.5%) | 14 (19.4%) | 13 (15.3%) | ||||
| Class 2 | 29 (72.5%) | 49 (68.1%) | 53 (62.4%) | ||||
| Class 3 | 4 (10%) | 9 (12.5%) | 19 (22.4%) | ||||
| Mandibular cortical width (MCW) (mm) | 3.29 ± 0.5 | 3.21 (2.03–4.3) | 3.19 ± 0.5 | 3.27 (2.03–4.3) | 2.94 ± 0.6 | 2.97 (1.7–4.6) | <0.005 ** |
| Panoramic mandibular index (PMI) | 0.3 ± 0.04 | 0.3 (0.18–0.37) | 0.272 ± 0.058 | 0.28 (0.12–0.37) | 0.267± 0.057 | 0.27 (0.12–0.36) | <0.05 * |
| Body mass index (kg/m2) | 25.5 ± 2.6 | 23.35 (21–31.77) | 23.05 ± 2.5 | 23 (18.1–30.6) | 19.8 ± 2.6 | 19.7 (15–27.9) | <0.001 ** |
| Number of remaining teeth | 15.53 ± 9.7 | 16 (0–30) | 15.57 ± 8.9 | 17 (0–29) | 16.01 ± 9.6 | 17 (0–29) | Not significant |
| Variable | z-Score | t-Score | ||
|---|---|---|---|---|
| Correlation Coefficient (r) | p-Value | Correlation Coefficient (r) | p-Value | |
| Age (in years) | −0.774 | <0.001 | −0.895 | <0.001 |
| Sex (1: men; 2: women) | 0.57 | Not significant | −0.339 | <0.001 |
| Quantitative ultrasound (QUS) | ||||
| Speed of sound (SOS) (m/s) | 0.654 | <0.001 | 0.827 | <0.001 |
| Calcaneus broadband attenuation of sound (BUA)(dB MHz) | 0.709 | <0.001 | 0.934 | <0.001 |
| Stiffness index (%) | 0.726 | <0.001 | 0.938 | <0.001 |
| Panoramic radiography | ||||
| Madibular cortical index (MCI) (1: class 1; 2: class 2; 3: class 3) | −0.211 | <0.001 | −0.413 | <0.001 |
| Mandibular cortical width (MCW) (mm) | 0.326 | <0.001 | 0.376 | <0.001 |
| Panoramic mandibular index (PMI) | 0.286 | <0.001 | 0.308 | <0.001 |
| Osteoporosis Self-Assessment Tool for Asians (OSTA) (1: low risk; 2: medium risk; 3: high risk) | −0.563 | <0.001 | −0.740 | <0.001 |
| Body mass index (kg/m2) | 0.301 | <0.001 | 0.270 | <0.001 |
| Number of remaining teeth | 0.116 | <0.05 | 0.102 | <0.05 |
| OSTA Index | Normal (%) | Osteopenia and Osteoporosis (%) | Total | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Men | |||||
| OSTA index > −1 | 55 (50) | 55 (50) | 110 (100%) | 90% | 50% |
| OSTA index ≤ −1 | 8 (10) | 72 (90) | 80 (100%) | ||
| Women | |||||
| OSTA index > −1 | 12 (30) | 28(70) | 40 (100%) | 96.8% | 30% |
| OSTA index ≤ −1 | 5 (3.2) | 152 (96.8) | 157 (100%) | ||
| Men & women | |||||
| OSTA index > −1 | 67 (44.7) | 83 (55.3) | 150 (100%) | 94.5% | 44.7% |
| OSTA index ≤ −1 | 13 (5.5) | 224 (94.5) | 237 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiswanjaya, B.; Bachtiar-Iskandar, H.H.; Yoshihara, A. Correlations of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and Three Panoramic Indices Using Quantitative Ultrasound (QUS) Bone Densitometry. Dent. J. 2023, 11, 34. https://doi.org/10.3390/dj11020034
Kiswanjaya B, Bachtiar-Iskandar HH, Yoshihara A. Correlations of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and Three Panoramic Indices Using Quantitative Ultrasound (QUS) Bone Densitometry. Dentistry Journal. 2023; 11(2):34. https://doi.org/10.3390/dj11020034
Chicago/Turabian StyleKiswanjaya, Bramma, Hanna H. Bachtiar-Iskandar, and Akihiro Yoshihara. 2023. "Correlations of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and Three Panoramic Indices Using Quantitative Ultrasound (QUS) Bone Densitometry" Dentistry Journal 11, no. 2: 34. https://doi.org/10.3390/dj11020034