A Systematic Investigation of American Vaccination Preference via Historical Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Household Pulse Survey Dataset on COVID-19 Vaccination
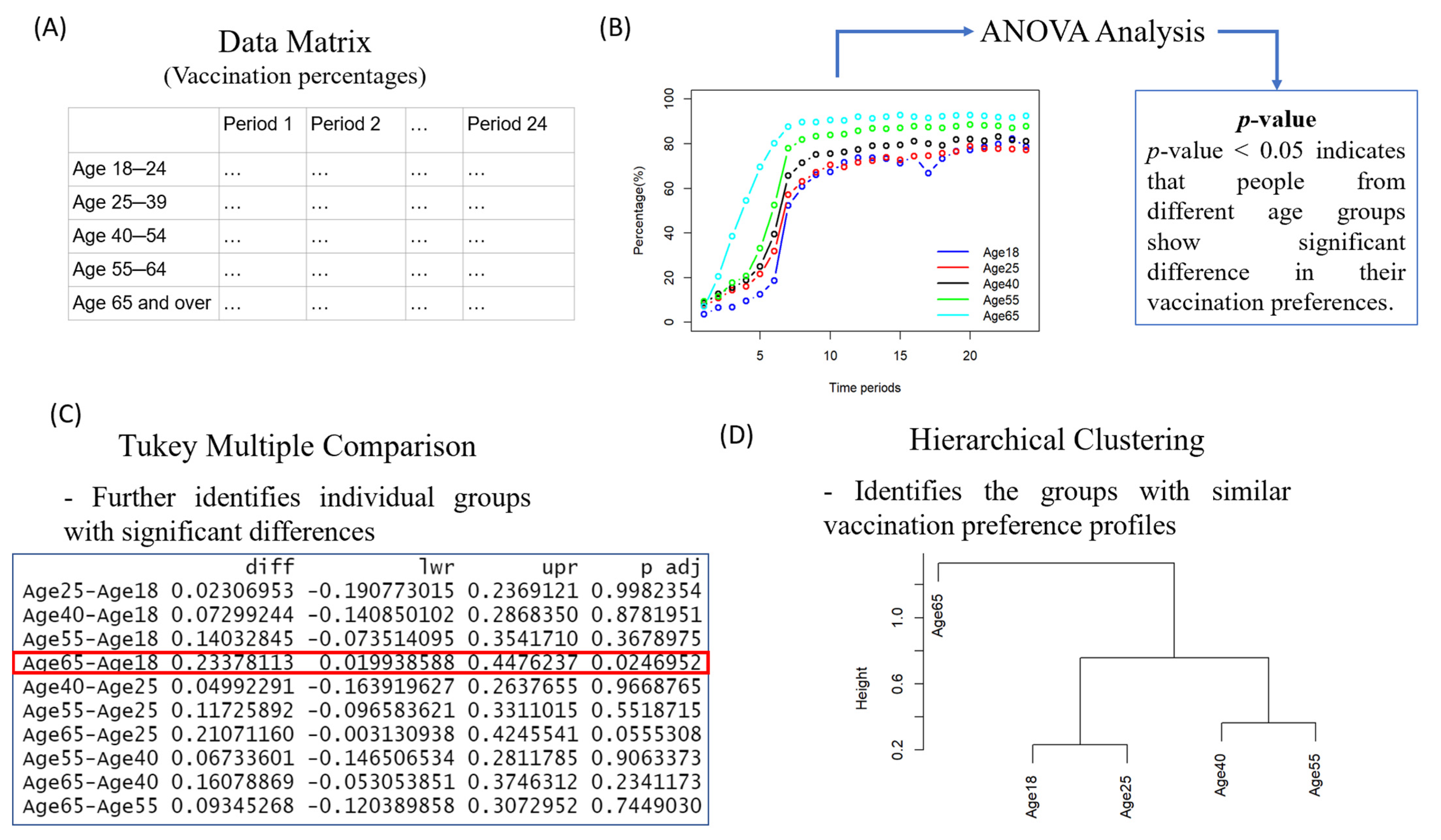
2.2. Statistical Analysis of the Dataset to Identify Factors for Vaccination Preference in the U.S.
3. Results
3.1. The Preferences of People from Different Ages for Vaccination
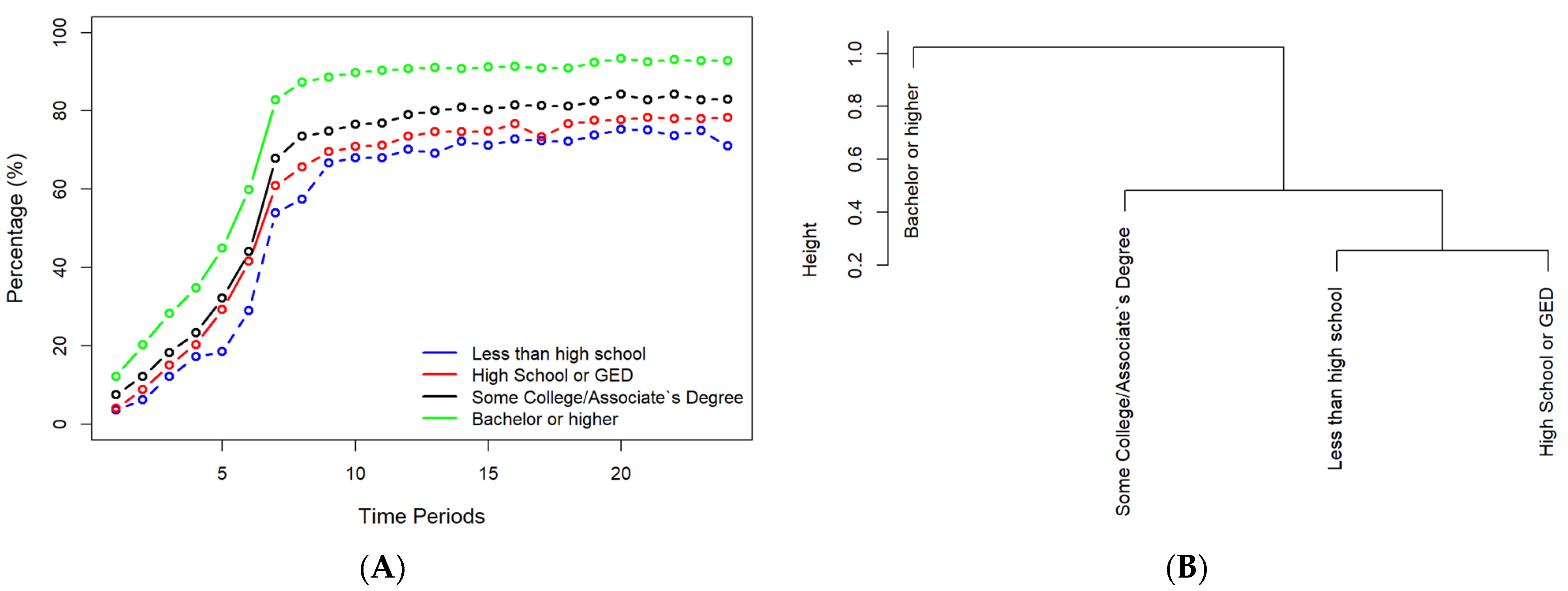
3.2. The Preferences of People with Different Education Levels towards Vaccination
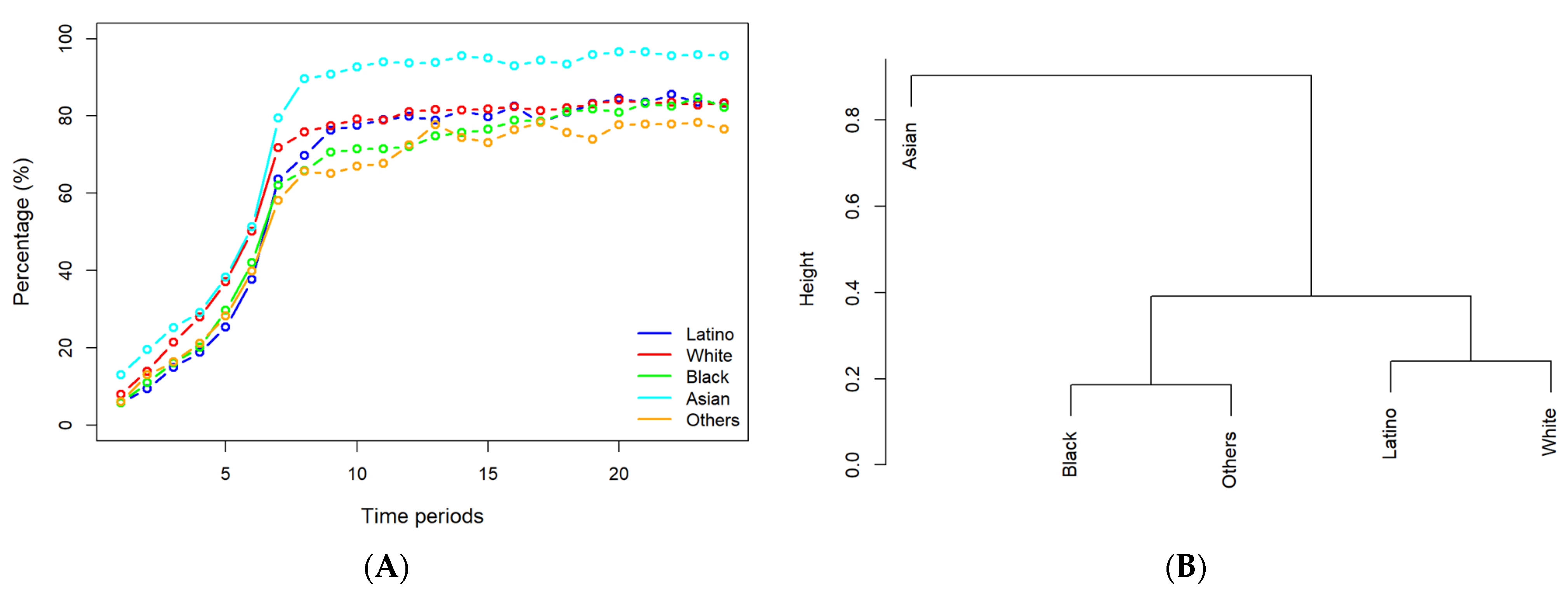
3.3. The Preferences of People of Different Races for Vaccination
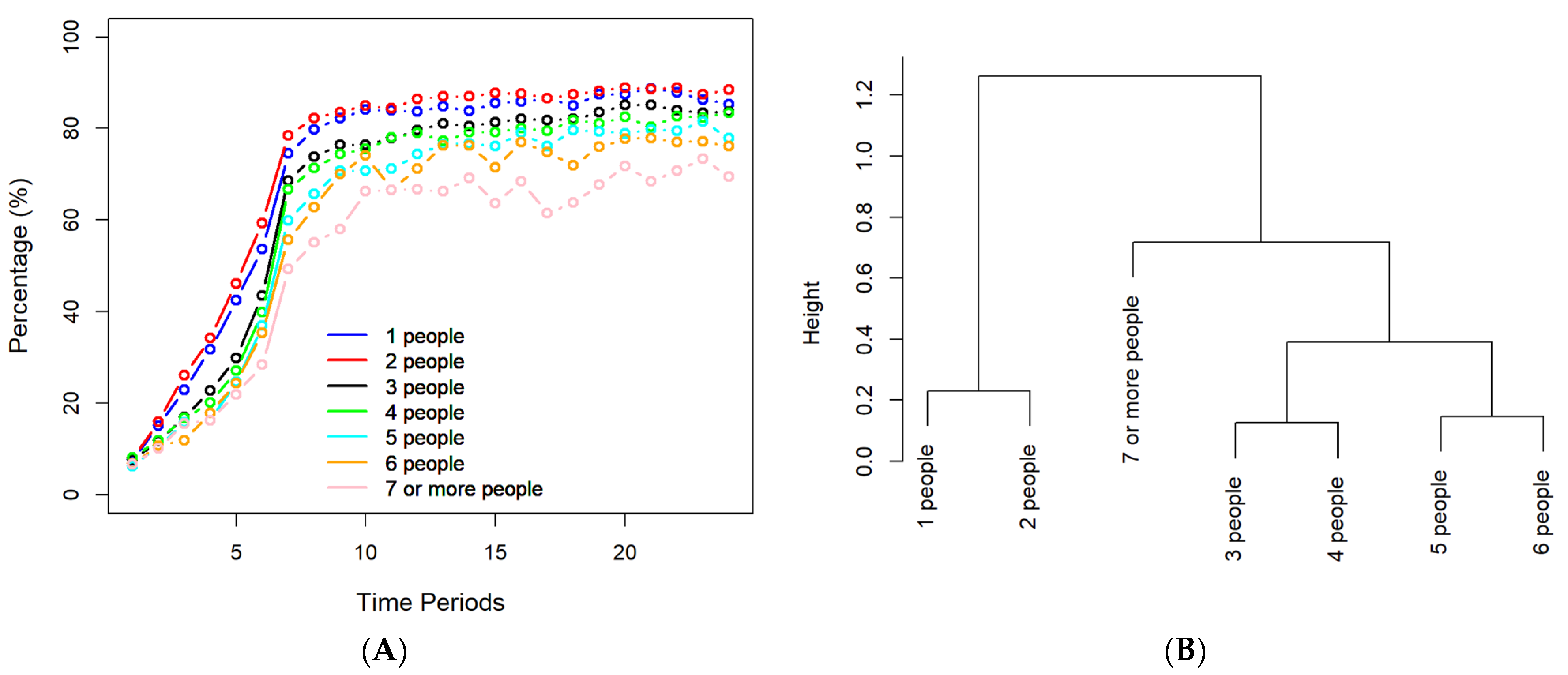
3.4. The Preferences of People with different Household Sizes forf Vaccination
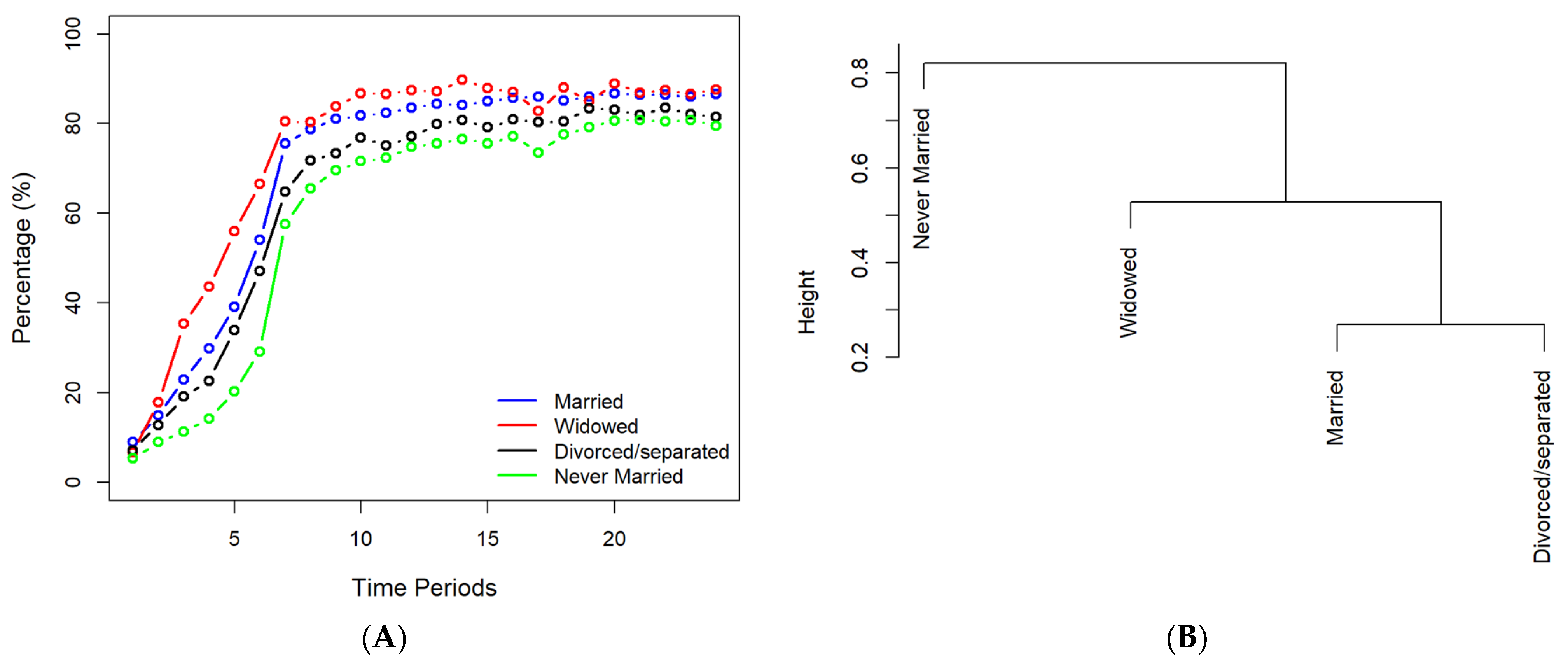
3.5. The Preferences of People with Different Marital Statuses for Vaccination
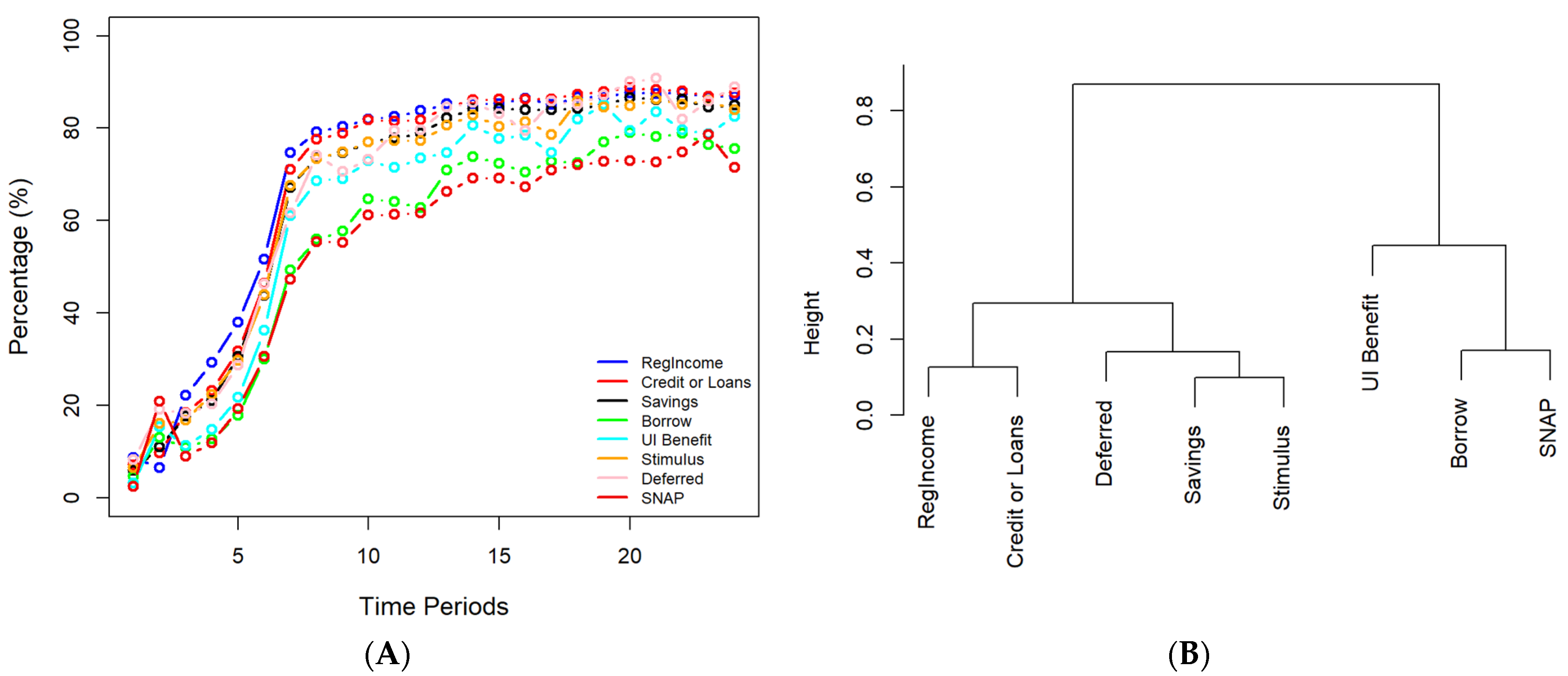
3.6. The Preferences of People with Different Income Sources for Vaccination
3.7. The Vaccination Preferences of People with Different Household Incomes
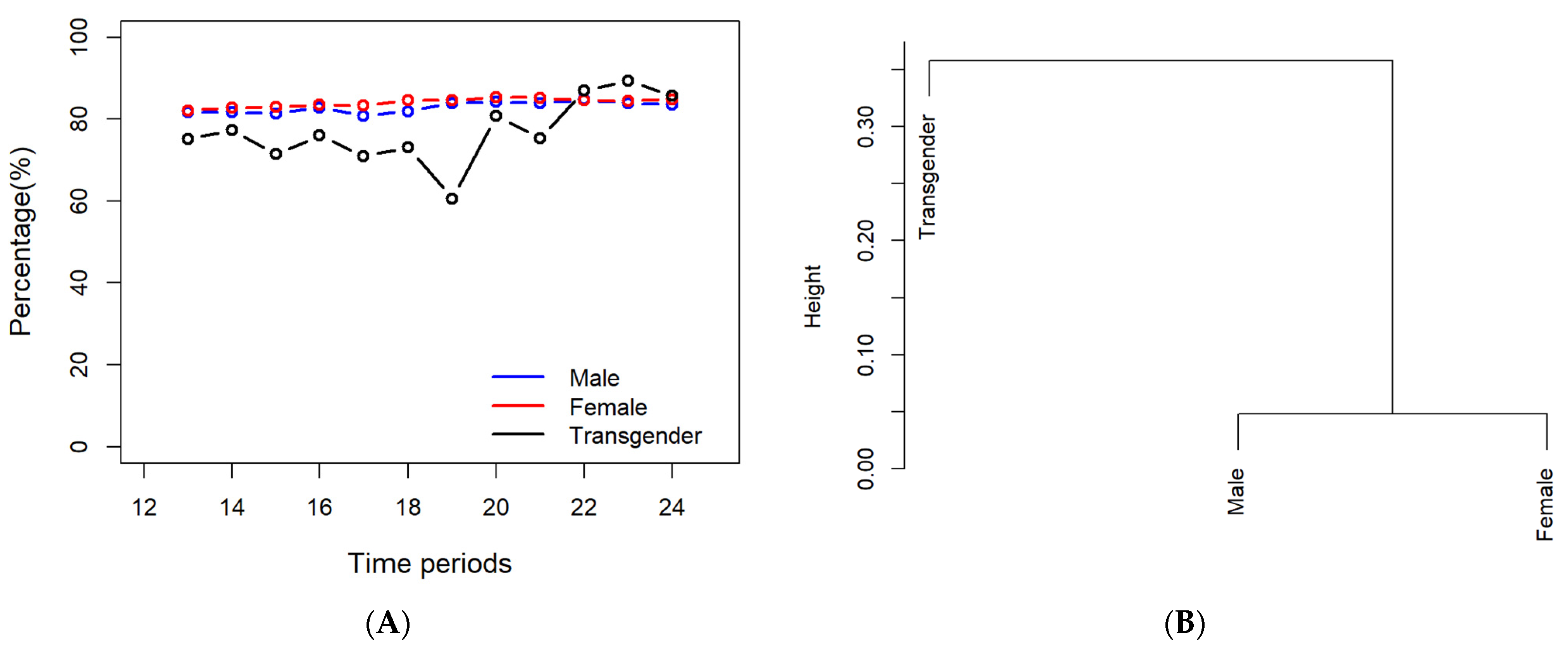
3.8. The Preferences of People with Different Genders for Vaccination
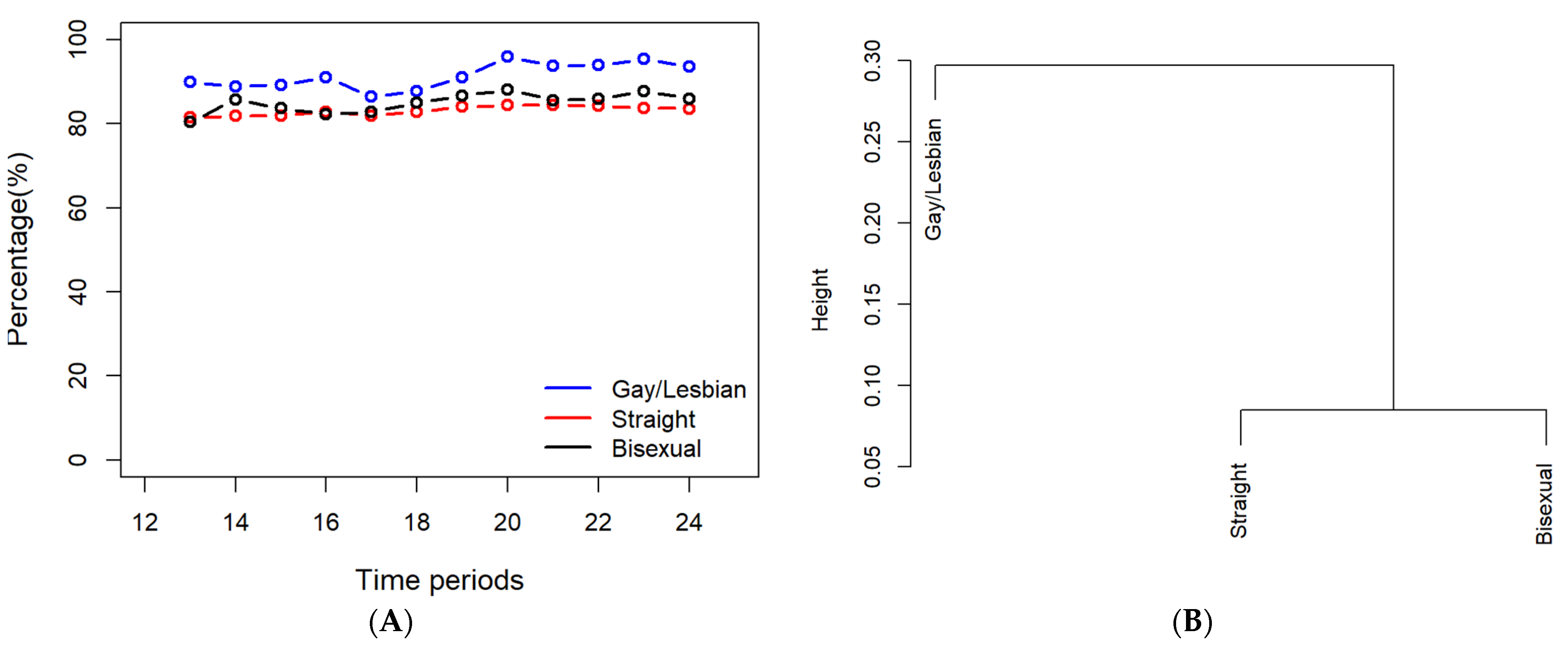
3.9. The Preferences of People with Different Sexual Orientations for Vaccination
3.10. Reason for Not Receiving or Planning to Receive Vaccines
4. Discussion
4.1. Factors with Significant Impacts on Respondents’ Vaccination Preferences
4.2. Major Reasons for Respondents’ Vaccination Hesitancy
4.3. Limitation of This Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef] [PubMed]
- Bansal, P.; Raj, A.; Shukla, D.M.; Sunder, N. COVID-19 vaccine preferences in India. Vaccine 2022, 40, 2242–2246. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; He, Z.; Liu, T.; Huang, J.; Zhang, C.J.P.; Akinwunmi, B.; Ming, W.-K. Acceptance of and Preference for COVID-19 Vaccination in India, the United Kingdom, Germany, Italy, and Spain: An International Cross-Sectional Study, Germany, Italy, and Spain. Vaccines 2022, 10, 832. [Google Scholar] [CrossRef] [PubMed]
- Leng, A.; Maitland, E.; Wang, S.; Nicholas, S.; Liu, R.; Wang, J. Individual preferences for COVID-19 vaccination in China. Vaccine 2020, 39, 247–254. [Google Scholar] [CrossRef]
- Dong, D.; Xu, R.H.; Wong, E.L.; Hung, C.; Feng, D.; Feng, Z.; Yeoh, E.; Wong, S.Y. Public preference for COVID-19 vaccines in China: A discrete choice experiment. Health Expect. 2020, 23, 1543–1578. [Google Scholar] [CrossRef]
- Huynh, H.P.; Senger, A.R. A little shot of humility: Intellectual humility predicts vaccination attitudes and intention to vaccinate against COVID-19. J. Appl. Soc. Psychol. 2021, 51, 449–460. [Google Scholar] [CrossRef]
- Guillon, M.; Kergall, P. Factors associated with COVID-19 vaccination intentions and attitudes in France. Public Health 2021, 198, 200–207. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Toshkov, D. What Accounts for the Variation in COVID-19 Vaccine Hesitancy in Eastern, Southern and Western Europe? Center for Open Science: Charlottesville, VA, USA, 2022. [Google Scholar] [CrossRef]
- Steinert, J.I.; Sternberg, H.; Prince, H.; Fasolo, B.; Galizzi, M.M.; Büthe, T.; Veltri, G.A. COVID-19 vaccine hesitancy in eight European countries: Prevalence, determinants, and heterogeneity. Sci. Adv. 2022, 8, abm9825. [Google Scholar] [CrossRef]
- Paul, K.T.; Zimmermann, B.M.; Corsico, P.; Fiske, A.; Geiger, S.; Johnson, S.; Kuiper, J.M.; Lievevrouw, E.; Marelli, L.; Prainsack, B.; et al. Anticipating hopes, fears and expectations towards COVID-19 vaccines: A qualitative interview study in seven European countries. SSM Qual. Res. Health 2022, 2, 100035. [Google Scholar] [CrossRef]
- Velikonja, N.K.; Dobrowolska, B.; Stanisavljević, S.; Erjavec, K.; Velikonja, V.G.; Verdenik, I. Attitudes of Nursing Students towards Vaccination and Other Preventive Measures for Limitation of COVID-19 Pandemic: Cross-Sectional Study in Three European Countries. Healthcare 2021, 9, 781. [Google Scholar] [CrossRef]
- Warren, G.W.; Lofstedt, R. COVID-19 vaccine rollout risk communication strategies in Europe: A rapid response. J. Risk Res. 2021, 24, 369–379. [Google Scholar] [CrossRef]
- Wawrzuta, D.; Jaworski, M.; Gotlib, J.; Panczyk, M. What Arguments against COVID-19 Vaccines Run on Facebook in Poland: Content Analysis of Comments. Vaccines 2021, 9, 481. [Google Scholar] [CrossRef]
- Rzymski, P.; Zeyland, J.; Poniedziałek, B.; Małecka, I.; Wysocki, J. The Perception and Attitudes toward COVID-19 Vaccines: A Cross-Sectional Study in Poland. Vaccines 2021, 9, 382. [Google Scholar] [CrossRef]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef]
- Kozak, A.; Nienhaus, A. COVID-19 Vaccination: Status and Willingness to Be Vaccinated among Employees in Health and Welfare Care in Germany. Int. J. Environ. Res. Public Health 2021, 18, 6688. [Google Scholar] [CrossRef]
- Abdou, M.S.; Kheirallah, K.A.; Aly, M.O.; Ramadan, A.; Elhadi, Y.A.M.; Elbarazi, I.; Deghidy, E.A.; El Saeh, H.M.; Salem, K.M.; Ghazy, R.M. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: An online survey in 13 Arab countries. PLoS ONE 2021, 16, e0260321. [Google Scholar] [CrossRef]
- Magadmi, R.M.; Kamel, F.O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health 2021, 21, 1438. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- A Qunaibi, E.; Helmy, M.; Basheti, I.; Sultan, I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. eLife 2021, 10, 68038. [Google Scholar] [CrossRef]
- Alzubaidi, H.; Samorinha, C.; Saddik, B.; Saidawi, W.; Abduelkarem, A.R.; Abu-Gharbieh, E.; Sherman, S.M. A mixed-methods study to assess COVID-19 vaccination acceptability among university students in the United Arab Emirates. Hum. Vaccines Immunother. 2021, 17, 4074–4082. [Google Scholar] [CrossRef]
- Kaadan, M.I.; Abdulkarim, J.; Chaar, M.; Zayegh, O.; Keblawi, M.A. Determinants of COVID-19 vaccine acceptance in the Arab world: A cross-sectional study. Glob. Health Res. Policy 2021, 6, 23. [Google Scholar] [CrossRef]
- Albahri, A.H.; Alnaqbi, S.A.; Alshaali, A.O.; Shahdoor, S.M. COVID-19 Vaccine Acceptance in a Sample from the United Arab Emirates General Adult Population: A Cross-Sectional Survey, 2020. Front. Public Health 2021, 9, 614499. [Google Scholar] [CrossRef]
- Ghazy, R.M.; ElHafeez, S.A.; Shaaban, R.; Elbarazi, I.; Abdou, M.S.; Ramadan, A.; Kheirallah, K.A. Determining the Cutoff Points of the 5C Scale for Assessment of COVID-19 Vaccines Psychological Antecedents among the Arab Population: A Multinational Study. J. Prim. Care Commun. Health 2021, 12, 34018891. [Google Scholar] [CrossRef]
- Al-Zalfawi, S.M.; Rabbani, S.I.; Asdaq, S.M.B.; Alamri, A.S.; Alsanie, W.F.; Alhomrani, M.; Mohzari, Y.; Alrashed, A.A.; AlRifdah, A.H.; Almagrabe, T. Public Knowledge, Attitude, and Perception towards COVID-19 Vaccination in Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 10081. [Google Scholar] [CrossRef]
- Roberts, C.H.; Brindle, H.; Rogers, N.T.; Eggo, R.M.; Enria, L.; Lees, S. Vaccine Confidence and Hesitancy at the Start of COVID-19 Vaccine Deployment in the UK: An Embedded Mixed-Methods Study. Front. Public Health 2021, 9, 745630. [Google Scholar] [CrossRef]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021, 1–12. [Google Scholar] [CrossRef]
- Bacon, A.M.; Taylor, S. Vaccination Hesitancy and Conspiracy Beliefs in the UK during the SARS-CoV-2 (COVID-19) Pandemic. Int. J. Behav. Med. 2021, 29, 448–455. [Google Scholar] [CrossRef]
- Woolf, K.; McManus, I.C.; A Martin, C.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg. Health Eur. 2021, 9, 100180. [Google Scholar] [CrossRef]
- Cook, E.J.; Elliott, E.; Gaitan, A.; Nduka, I.; Cartwright, S.; Egbutah, C.; Randhawa, G.; Waqar, M.; Ali, N. Vaccination against COVID-19: Factors That Influence Vaccine Hesitancy among an Ethnically Diverse Community in the UK. Vaccines 2022, 10, 106. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Yu, L.-M.; Freeman, J.; Chadwick, A.; Vaccari, C.; Shanyinde, M.; Harris, V.; Waite, F.; Rosebrock, L.; et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. Lancet Public Health 2021, 6, e416–e427. [Google Scholar] [CrossRef]
- Sonawane, K.; Troisi, C.L.; Deshmukh, A.A. COVID-19 vaccination in the UK: Addressing vaccine hesitancy. Lancet Reg. Health Eur. 2021, 1, 100016. [Google Scholar] [CrossRef]
- Lu, X.; Wang, J.; Hu, L.; Li, B.; Lu, Y. Association between Adult Vaccine Hesitancy and Parental Acceptance of Childhood COVID-19 Vaccines: A Web-Based Survey in a Northwestern Region in China. Vaccines 2021, 9, 1088. [Google Scholar] [CrossRef]
- Gao, X.; Li, H.; He, W.; Zeng, W. COVID-19 Vaccine Hesitancy Among Medical Students: The Next COVID-19 Challenge in Wuhan, China. Disaster Med. Public Health Prep. 2021, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, Q.; Tarimo, C.S.; Wang, M.; Gu, J.; Wei, W.; Ma, M.; Zhao, L.; Mu, Z.; Miao, Y. COVID-19 Vaccine Hesitancy Among Chinese Population: A Large-Scale National Study. Front. Immunol. 2021, 12, 781161. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, X.; Gao, J.; Liu, X.; Mao, Y.; Wang, R.; Zheng, P.; Xiao, Q.; Jia, Y.; Fu, H.; et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021, 23, e29329. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Xie, M.; Liu, J.; Zheng, H.; Zhang, S.; et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2021, 39, 2833–2842. [Google Scholar] [CrossRef]
- Jacob, J.; Stephen, S.; Issac, A.; Krishnan, N.; Radhakrishnan, R.V.; Dhandapani, M.; Jose, S.; Sm, A.; Nair, A.S. Determinants of Willingness for COVID-19 Vaccine: Implications for Enhancing the Proportion of Vaccination Among Indians. Cureus 2021, 13, 15271. [Google Scholar] [CrossRef]
- Sharun, K.; Rahman, C.K.F.; Haritha, C.V.; Jose, B.; Tiwari, R.; Dhama, K. COVID-19 Vaccine Acceptance: Beliefs and Barriers Associated with Vaccination among the General Population in India. J. Exp. Biol. Agric. Sci. 2020, 8, S210–S218. [Google Scholar] [CrossRef]
- Jain, J.; Saurabh, S.; Kumar, P.; Verma, M.K.; Goel, A.D.; Gupta, M.K.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 2021, 149, 34011421. [Google Scholar] [CrossRef]
- Okubo, T.; Inoue, A.; Sekijima, K. Who Got Vaccinated for COVID-19? Evidence from Japan. Vaccines 2021, 9, 1505. [Google Scholar] [CrossRef]
- Kawata, K.; Nakabayashi, M. Determinants of COVID-19 vaccine preference: A survey study in Japan. SSM Popul. Health. 2021, 15, 100902. [Google Scholar] [CrossRef]
- Askarian, M.; Fu, L.; Taghrir, M.H.; Borazjani, R.; Shayan, Z.; Taherifard, E.; Taherifard, E.; Akbarialiabad, H.; Longtin, Y.; Askarian, A.; et al. Factors Affecting COVID-19 Vaccination Intent among Iranians: COVID-19 Vaccination Acceptance. 3 December 2020. Available online: https://ssrn.com/abstract=3741968 (accessed on 30 June 2022).
- Tahir, M.J.; Saqlain, M.; Tariq, W.; Waheed, S.; Tan, S.H.S.; Nasir, S.I.; Ullah, I.; Ahmed, A. Population preferences and attitudes towards COVID-19 vaccination: A cross-sectional study from Pakistan. BMC Public Health 2021, 21, 34565351. [Google Scholar] [CrossRef]
- Goodwin, R.; Nguyen Luu, L.A.; Wiwattanapantuwong, J.; Kovács, M.; Suttiwan, P.; Levin, Y. Two-TailTwo-Tailed Dogs, Social Unrest and COVID-19 Vaccination: Politics, Hesitancy and Vaccine Choice in Hungary and Thailanded Dogs, Social Unrest and COVID-19 Vaccination: Politics, Hesitancy and Vaccine Choice in Hungary and Thailand. Vaccines 2022, 10, 789. [Google Scholar] [CrossRef]
- Conklin, M. Racial Preferences in COVID-19 Vaccination: Legal and Practical Implications. SSRN Electron. J. 2021, 5, 141. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef]
- Liu, T.; He, Z.; Huang, J.; Yan, N.; Chen, Q.; Huang, F.; Zhang, Y.; Akinwunmi, O.; Akinwunmi, B.; Zhang, C.; et al. A Comparison of Vaccine Hesitancy of COVID-19 Vaccination in China and the United States. Vaccines 2021, 9, 649. [Google Scholar] [CrossRef]
- Nehal, K.R.; Steendam, L.M.; Ponce, M.C.; van der Hoeven, M.; Smit, G.S.A. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2021, 9, 1071. [Google Scholar] [CrossRef]
- Cai, C.; Woolhandler, S.; Himmelstein, D.U.; Gaffney, A. Trends in Anxiety and Depression Symptoms During the COVID-19 Pandemic: Results from the US Census Bureau’s Household Pulse Survey. J. Gen. Intern. Med. 2021, 36, 1841–1843. [Google Scholar] [CrossRef]
- Morales, D.X.; Morales, S.A.; Beltran, T.F. Racial/Ethnic Disparities in Household Food Insecurity During the COVID-19 Pandemic: A Nationally Representative Study. J. Racial Ethn. Health Disp. 2020, 8, 1300–1314. [Google Scholar] [CrossRef]
- Marsal, D. Introduction to the Analysis of Variance (ANOVA). Stat. Geosci. 1987, 141–143. [Google Scholar] [CrossRef]
- Rees, D. An Introduction to the Analysis of Variance (ANOVA). In Essential Statistics, 4th ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2001; ISBN 9781315273174. [Google Scholar]
- Singh, G. “Analysis of Variance (ANOVA)|Introduction, Types & Techniques,” Analytics Vidhya. 2018. Available online: https://www.analyticsvidhya.com/blog/2018/01/anova-analysis-of-variance/ (accessed on 30 June 2022).
- Armstrong, R. An introduction to analysis of variance (ANOVA) with special reference to data from clinical experiments in optometry. Ophthalm. Physiol. Opt. 2000, 20, 235–241. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Tukey Multiple Comparison test. J. Clin. Nurs. 1999, 8, 299–304. Available online: http://www.blackwellpublishing.com/specialarticles/jcn_8_304.pdf (accessed on 30 June 2022).
- Jafarzadegan, M.; Safi-Esfahani, F.; Beheshti, Z. Combining hierarchical clustering approaches using the PCA method. Exp. Syst. Appl. 2019, 137, 64. [Google Scholar] [CrossRef]
- Yang, W.; Wang, X.; Lu, J.; Dou, W.; Liu, S. Interactive Steering of Hierarchical Clustering. IEEE Trans. Vis. Comput. Graph. 2020, 27, 3953–3967. [Google Scholar] [CrossRef]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2021, 31, 62–86. [Google Scholar] [CrossRef]
- Craig, B.M. United States COVID-19 Vaccination Preferences (CVP): 2020 Hindsight. Patient 2021, 14, 309–318. [Google Scholar] [CrossRef]
- Head, K.J.; Kasting, M.L.; Sturm, L.A.; Hartsock, J.A.; Zimet, G.D. A National Survey Assessing SARS-CoV-2 Vaccination Intentions: Implications for Future Public Health Communication Efforts. Sci. Commun. 2020, 42, 698–723. [Google Scholar] [CrossRef]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatr. Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.-Y.; Cheung, A.W.-L.; Yau, P.S.-Y.; Chung, V.C.-H.; Wong, C.H.-L.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Influence of Vaccination Characteristics on COVID-19 Vaccine Acceptance Among Working-Age People in Hong Kong, China: A Discrete Choice Experiment. Front. Public Health 2021, 9, 793533. [Google Scholar] [CrossRef] [PubMed]
- Petersen, F.; Errore, A.; Karaca-Mandic, P. Lifting Statewide Mask Mandates and COVID-19 Cases. Med. Care 2022, 60, 538–544. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Chen, A.; Shi, Y.; Chen, K.; Zhao, K.H.; Xu, M.; He, R.; Huang, Z. A Systematic Investigation of American Vaccination Preference via Historical Data. Processes 2022, 10, 1665. https://doi.org/10.3390/pr10081665
Chen J, Chen A, Shi Y, Chen K, Zhao KH, Xu M, He R, Huang Z. A Systematic Investigation of American Vaccination Preference via Historical Data. Processes. 2022; 10(8):1665. https://doi.org/10.3390/pr10081665
Chicago/Turabian StyleChen, Jason, Angie Chen, Youran Shi, Kathryn Chen, Kevin Han Zhao, Morwen Xu, Ricky He, and Zuyi Huang. 2022. "A Systematic Investigation of American Vaccination Preference via Historical Data" Processes 10, no. 8: 1665. https://doi.org/10.3390/pr10081665




