GoTO: A Process-Navigation Tool for Telehealth and -Care Solutions, Designed to Ensure an Efficient Trajectory from Goal Setting to Outcome Evaluation
Abstract
:1. Introduction
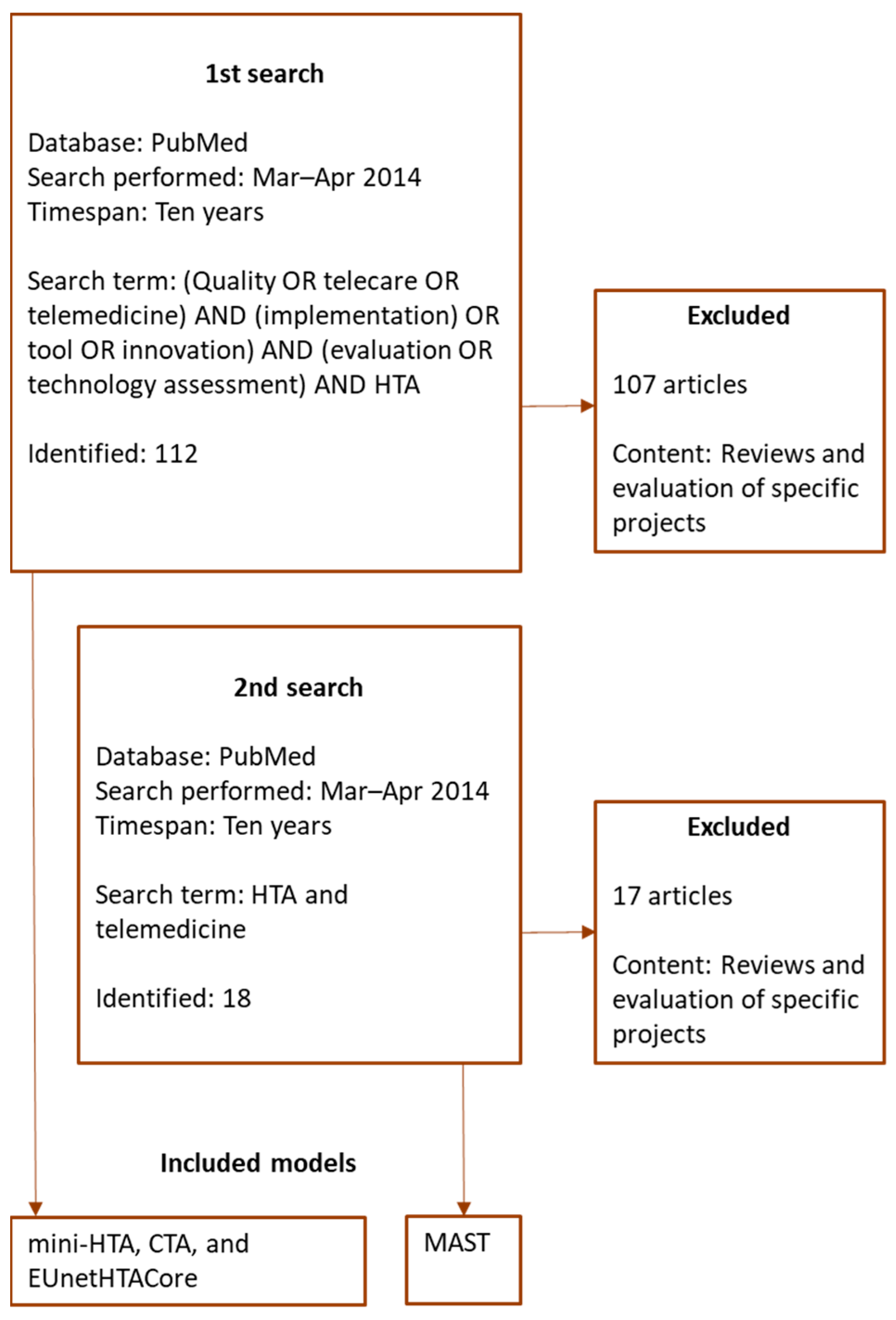
2. Methods
3. Results
3.1. HTA-Inspired Models
3.2. Project Management Models
3.3. Development and Implementation Models
3.3.1. West Midlands Toolkit
3.3.2. The Stanford BioX Biodesign Innovation Process
3.4. Summary
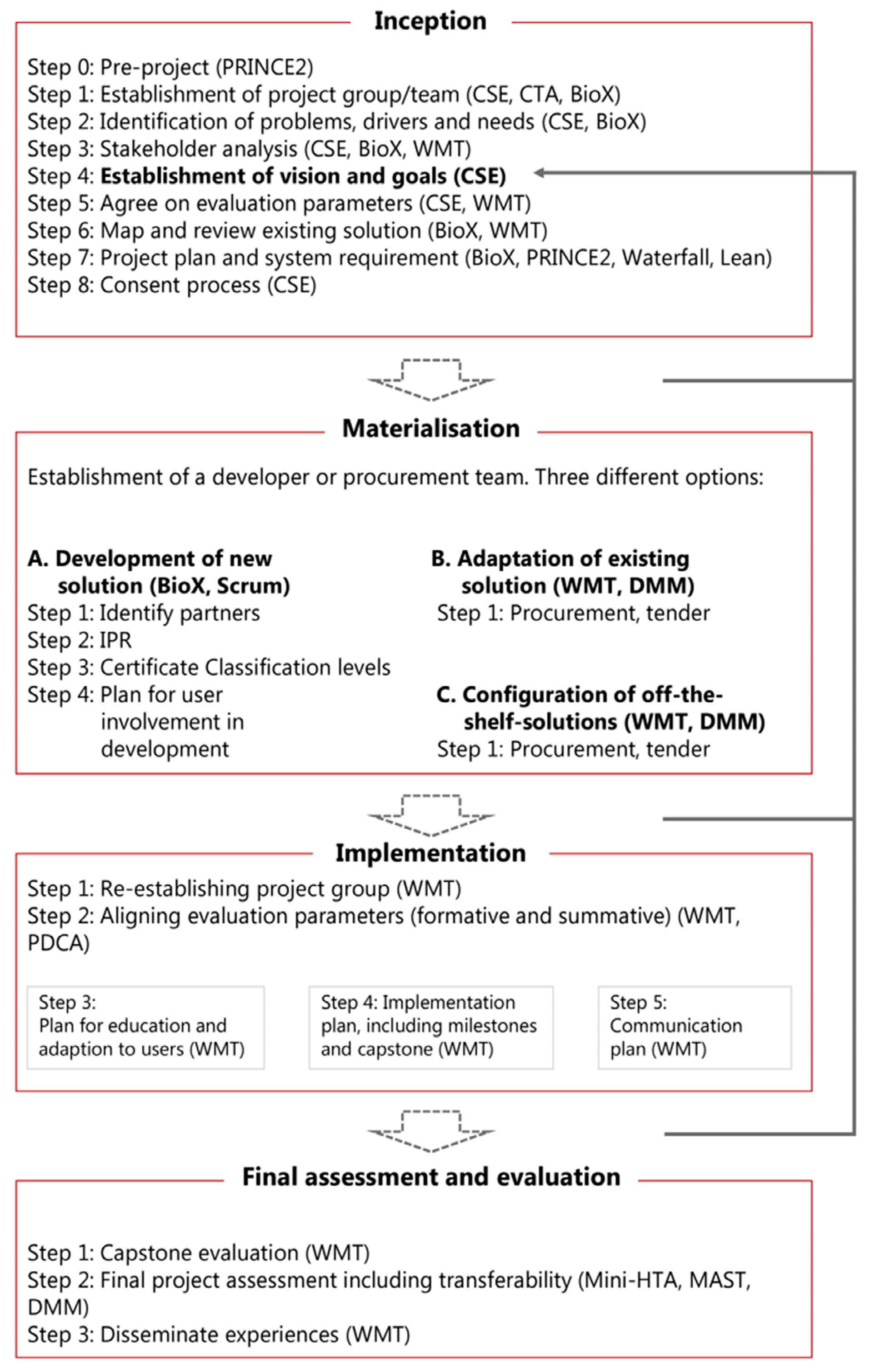
4. Creation of the GoTO Process Navigator
4.1. Part 1—Inception
4.2. Part 2—Materialization
4.3. Part 3—Implementation
4.4. Part 4—Final Assessment and Evaluation
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CSE | Continuous systematic evaluation |
| CTA | Constructive technology assessment |
| DMM | Decision-making model |
| GoTO | Goal to Outcome |
| HTA | Health technology assessment |
| MAST | Model for assessment of telemedicine |
| MRC | Medical Research Council |
| PDCA | Plan do check act |
| PRINCE | Projects in controlled environments |
| SMHO | Small and middle-sized health and care organizations |
| THC | Telehealth and telecare |
| WMT | West Midlands toolkit |
References
- World Health Organization, the Secretariat. WHO Framework on Integrated People-Centred Health Services, A Report by the Secretariat. 2016. Available online: http://www.who.int/servicedeliverysafety/areas/people-centred-care/en (accessed on 11 May 2017).
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros, A.D.; World Health Organization (Eds.) Health Literacy: The Solid Facts; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2013; ISBN 978-92-890-0015-4. [Google Scholar]
- CPME; Donabedian, A.; DCHE; European Commission. PiSCE: Pilot Project on the Promotion of Self-Care Systems in the European Union; European Commission: Brussels, Belgium, 2017. [Google Scholar]
- Samoocha, D.; Bruinvels, D.; Elbers, N.; Anema, J.R.; Van Der Beek, A.J. Effectiveness of Web-based Interventions on Patient Empowerment: A Systematic Review and Meta-analysis. J. Med. Internet Res. 2010, 12, e23. [Google Scholar] [CrossRef] [PubMed]
- Demiris, G. Consumer Health Informatics: Past, Present, and Future of a Rapidly Evolving Domain. Yearb. Med. Inform. 2016, 25, S42–S47. [Google Scholar] [CrossRef] [PubMed]
- Phanareth, K.; Vingtoft, S.; Christensen, A.S.; Nielsen, J.S.; Svenstrup, J.; Berntsen, G.K.R.; Newman, S.P.; Kayser, L. The Epital Care Model: A New Person-Centered Model of Technology-Enabled Integrated Care for People With Long Term Conditions. JMIR Res. Protoc. 2017, 6, e6. [Google Scholar] [CrossRef]
- Szczepanski, M. A Digital Single Market Strategy for Europe; EPRS: European Parliamentary Research Service: Brussels, Belgium, 2015; CID: 20.500.12592/rg03rx. [Google Scholar]
- Kunonga, T.P.; Spiers, G.F.; Beyer, F.R.; Hanratty, B.; Boulton, E.; Hall, A.; Bower, P.; Todd, C.; Craig, D. Effects of Digital Technologies on Older People’s Access to Health and Social Care: Umbrella Review. J. Med. Internet Res. 2021, 23, e25887. [Google Scholar] [CrossRef] [PubMed]
- European Innovation Partnership on Active and Healthy Ageing. Blueprint—Digital Transformation of Health and Care for the Ageing Society. 2017. Available online: https://ec.europa.eu/digital-single-market/en/blueprint-digital-transformation-health-and-care-ageing-society (accessed on 21 August 2022).
- World Economic Forum; Bilbao-Osorio, B.; Dutta, S.; Lanvin, B. (Eds.) The Global Information Technology Report 2014; World Economic Forum: Geneva, Switzerland, 2014; ISBN -13: 978-92-95044-63-0. [Google Scholar]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G. Intervention Mapping: A Process for Developing Theory and Evidence-Based Health Education Programs. Health Educ. Behav. 1998, 25, 545–563. [Google Scholar] [CrossRef] [PubMed]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ 2021, 374, n2061. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed]
- Lindskrog, S.; Christensen, K.B.; Osborne, R.H.; Vingtoft, S.; Phanareth, K.; Kayser, L. Relationship Between Patient-Reported Outcome Measures and the Severity of Chronic Obstructive Pulmonary Disease in the Context of an Innovative Digitally Supported 24-Hour Service: Longitudinal Study. J. Med. Internet Res. 2019, 21, e10924. [Google Scholar] [CrossRef] [PubMed]
- PRINCE2 Explained-PRINCE2.co. 2017. Available online: https://prince2.co/prince2-explained (accessed on 3 July 2017).
- Jakobsen, N.K.; Jensen, L.S.; Kayser, L. Collaborative efforts are needed to ensure proper knowledge dissemination of telemedicine projects. Dan. Med. J. 2014, 61, A4896. [Google Scholar] [PubMed]
- Boonstra, A.; Versluis, A.; Vos, J.F.J. Implementing electronic health records in hospitals: A systematic literature review. BMC Health Serv. Res. 2014, 14, 370. [Google Scholar] [CrossRef] [Green Version]
- NHS Midlands and East. Telehealthcare Commisioning & Evaluation Toolkit (Overview Version); West Midlands NHS: Birmingham, UK, 2012. [Google Scholar]
- MedCom. Det Telemedicinske Landkort. Available online: https://telemedicinsk-landkort.dk (accessed on 29 January 2021).
- European Commission. Directorate General for Health and Food Safety. Opinion on Assessing the Impact of Digital Transformation of Health Services; LU Publications Office: Luxembourg, 2019; Available online: https://data.europa.eu/doi/10.2875/09099 (accessed on 15 August 2022).
- Granja, C.; Janssen, W.; Johansen, M.A. Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature. J. Med. Internet Res. 2018, 20, e10235. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, R.; Ballini, L.; Maltoni, S.; A O’Donnell, C.; Mair, F.S.; Macfarlane, A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci. 2014, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- WHO. Health Technology Assessment. 2018. Available online: http://www.who.int/medical_devices/assessment/en (accessed on 14 June 2018).
- Kidholm, K.; Ekeland, A.G.; Jensen, L.K.; Rasmussen, J.; Pedersen, C.D.; Bowes, A.; Flottorp, S.A.; Bech, M. A model for assessment of telemedicine applications: Mast. Int. J. Technol. Assess. Health Care 2012, 28, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, F.B.; Sigmund, H.; Danmark Sundhedsstyrelsen; Enhed for Medicinsk Teknologivurdering. Health Technology Assessment Handbook; National Board of Health: Copenhagen, Denmark, 2008; ISBN 978-87-7676-649-8. [Google Scholar]
- National Board of Health. Introduction to Mini-HTA: A Management and Decision Support Tool for the Hospital Service; The National Board of Health: Copenhagen, Denmark, 2005; ISBN 978-87-7676-237-7. [Google Scholar]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467. [Google Scholar] [CrossRef]
- Høstgaard, A.M.B.; Bertelsen, P.; Petersen, L.S.; Nøhr, C. Constructive Technology Assessment for HIT development: Learning, Feedback and User Involvement. 2013. Available online: http://vbn.aau.dk/da/publications/constructive-technology-assessment-for-hit-development(4f50eee7-7c49-4b01-be90-d0692190999d).html (accessed on 9 March 2017).
- Kristensen, F.B.; Lampe, K.; Chase, D.L.; Lee-Robin, S.H.; Wild, C.; Moharra, M.; Garrido, M.V.; Nielsen, C.P.; Røttingen, J.-A.; Neikter, S.A.; et al. Practical tools and methods for health technology assessment in Europe: Structures, methodologies, and tools developed by the European network for Health Technology Assessment, EUnetHTA. Int. J. Technol. Assess. Health Care 2009, 25, 1–8. [Google Scholar] [CrossRef]
- Catwell, L.; Sheikh, A. Evaluating eHealth Interventions: The Need for Continuous Systemic Evaluation. PLoS Med. 2009, 6, e1000126. [Google Scholar] [CrossRef]
- Masella, C.; Zanaboni, P. Assessment models for telemedicine services in national health systems. Int. J. Health Technol. Manag. 2008, 9, 446. [Google Scholar] [CrossRef]
- Yock, P.G. (Ed.) Biodesign: The Process of Innovating Medical Technologies, 2nd ed.; Cambridge University Press: Cambridge, NY, USA, 2015; ISBN 978-1-107-08735-4. [Google Scholar]
- Monberg, A.-C.; Furstrand, D.; Jensen, L.S.; Kayser, L. The Benefit Trajectory—A framework to support innovative and beneficial technology based solutions in integrated care. Int. J. Integr. Care 2015, 15. [Google Scholar] [CrossRef] [Green Version]
- Pasternack, I.; Sampietro-Colom, L.; Wasserfallen, J.-B. (Eds.) The AdHopHTA Handbook: A Handbook of Hospital—Based Health Technology Assessment (HB-HTA). 2015. Available online: http://www.adhophta.eu/sites/files/adhophta/media/adhophta_handbook_website.pdf (accessed on 21 August 2022).
- Zanaboni, P.; Lettieri, E.; Gagnon, M.-P. Institutionalizing Telemedicine Applications: The Challenge of Legitimizing Decision-Making. J. Med. Internet Res. 2011, 13, e72. [Google Scholar] [CrossRef] [PubMed]
- Schot, J.; Rip, A. The past and future of constructive technology assessment. Technol. Forecast. Soc. Chang. 1997, 54, 251–268. [Google Scholar] [CrossRef]
- Beauchamp, G.; Thorley, M. Business Analysis: Delivering the Right Solution to the Right Problem. 2007. Available online: www.smart-ba.com/articles/ba_chain_of_reasoning.pdf (accessed on 21 August 2022).
- Moen, R.; Norman, C. Evolution of the PDCA Cycle. 2006. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.470.5465%7B%5C&%7Drep=rep1%7B%5C&%7Dtype=pdf (accessed on 21 August 2022).
- Schwaber, K.; Beedle, M. Agile Software Development with Scrum; Upper Saddle River: Bergen County, NJ, USA, 2001. [Google Scholar]
- Beck, K.; Beedle, M.; van Bennekum, A.; Cockburn, A.; Cunningham, W.; Fowler, M. Manifesto for Agile Software Development, 2001. Available online: http://johnlevyconsulting.com/pdf/SB6-4_Agile_Manifesto.pdf (accessed on 21 August 2022).
- Hughes, B.; Cotterell, M. Software Project Management, 3rd ed.; Tata McGraw-Hill Education: London, UK, 2002. [Google Scholar]
- Womack, J.P.; Jones, D.T.; Roos, D. The Machine That Changed the World: The Story of Lean Production-Toyota’s Secret Weapon in the Global Car Wars That Is Revolutionizing World Industry, 1st ed.; Free Press: London, UK, 2007; ISBN 978-0-7432-9979-4. [Google Scholar]
- Bell, T.E.; Thayer, T.A. Software requirements: Are they really a problem? In Proceedings of the 2nd International Conference on Software Engineering, San Francisco, CA, USA, 13–15 October 1976; IEEE Computer Society Press: Washington, DC, USA. [Google Scholar]
- Takeuchi, H.; Nonaka, I. The New New Product Development Game. Harv. Bus. Rev. 1986, 64, 137–146. [Google Scholar]
- Sutherland, J.V. (Ed.) Business Object Design and Implementation: OOPSLA ’95 Workshop Proceedings, 16 October 1995, Austin, Texas; Springer: London, NY, USA, 1997; ISBN 978-3-540-76096-2. [Google Scholar]
- Cruickshank, J. Healthcare without Walls: A Framework for Delivering Telehealth at Scale; 2020health: London, UK, 2010; ISBN 978-1-907635-12-0. [Google Scholar]
- Sundhedsdatastyrelsen. Arkitekturprincipper for Sundhedsområdet-en Ramme for Udformning af Fremtidens Nationale it-Arkitektur for Sundhedsvæse-net; Sundhedsdatastyrelsen: Copenhagen, Denmark, 2009. [Google Scholar]
- Campbell, B.; Sedrakyan, A. Patient involvement in regulation: An unvalued imperative. Lancet 2021, 397, 2147–2148. [Google Scholar] [CrossRef]
- Kayser, L.; Kushniruk, A.; Osborne, R.H.; Norgaard, O.; Turner, P. Enhancing the Effectiveness of Consumer-Focused Health Information Technology Systems Through eHealth Literacy: A Framework for Understanding Users’ Needs. JMIR Hum. Factors 2015, 2, e9. [Google Scholar] [CrossRef] [PubMed]
- Monkman, H.; Kushniruk, A.W. The Consumer Health Information System Adoption Model. Stud. Health Technol. Inform. 2015, 218, 26–31. [Google Scholar] [PubMed]
- Imai, M. Kaizen: The Key to Japan’s Competitive Success; McGraw-Hill: New York, NY, USA, 1986. [Google Scholar]
- Clemensen, J.; Rothmann, M.J.; Smith, A.C.; Caffery, L.J.; Danbjorg, D.B. Participatory design methods in telemedicine research. J. Telemed. Telecare 2017, 23, 780–785. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Procter, R.; Wherton, J.; Sugarhood, P.; Hinder, S.; Rouncefield, M. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med. 2015, 13, 91. [Google Scholar] [CrossRef] [Green Version]
- Ward, J.; Daniel, E. (Eds.) Benefits Management: How to Increase the Business Value of Your IT Projects; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012. [Google Scholar]
- SMILE, Developing the SMILE Digital Care Facilitator and Conversational Agent: Workshop on User Requirements and Co-creation Design Process. Available online: https://smileehealth.eu/developing-the-smile-digital-care-facilitator-and-conversational-agent-workshop-on-user-requirements-and-co-creation-design-process/ (accessed on 10 April 2022).
- Gutenberg, J.; Kayser, L. A Practical Toolkit for Researchers Working with Digital Health Interventions for Patients. 2018. Available online: https://www.cancer.dk/dyn/resources/File/file/9/7639/1581342636/2018_a-tractical-toolkit-for-researchers.pdf (accessed on 29 January 2021).
| Name and Origin | Objective | Components |
|---|---|---|
| Constructive technology assessment for health information technology (CTA). CTA for health IT was developed in the late 00s based on the CTA described by the Netherlands Organization of Technology Assessment (NOTA) in 1987 [30,38]. | To handle the complexity and varying needs of the healthcare sector, offering agile implementation and formative evaluation to enable an adaptive implementation of new technologies. | Five stages:
|
| A continuous systematic evaluation model (CSE), proposed by Catwell et al. in 2009 [32] and based on a seven-step implementation model proposed by Thorley [39]. | A continuous, systematic evaluation of e-health projects to ensure quality, safety, and efficiency. | Four phases:
|
| Mini health technology assessment for hospitals (Mini-HTA), proposed by the Danish National Board of Health in 2005 [26,36]. | A time-effective model to be used in hospitals by managers in decision making when new technologies are being considered. It is evidence-based and cross-disciplinary. | Four dimensions:
|
| EUnetHTA framework (EUnetHTA), developed in 2006–2008 by the European network for HTA [31]. | To provide a glossary and tools, including lists and additional resources, to ensure the relevance, reliability, and transferability of data and information from existing HTA reports and to identify areas in need of further development. | Nine dimensions for assessment:
|
| Model for assessment of telemedicine (MAST), developed by Kidholm et al. in 2009 and commissioned by the European Commission [24]. | A framework to assist organizations in deciding whether a specific telemedical technology is suitable for implementation. | Three steps:
health and technology aspects, safety, clinical effect, patient perspective, economics, organization and sociocultural aspects, and ethics and law. |
| Decision-making model (DMM), proposed by Zanaboni et al. in 2011 [37]. | To support decision makers in the acquisition of scalable telemedical solutions. The intention of the model was to evaluate solutions or technologies presented by vendors in a competing process. | Two stages:
|
| Name and Origin | Objective | Components |
|---|---|---|
| Plan do check act (PDCA). Originates from Deming in 1950 [40]. | Intended as a problem-solving model. Ensures development and implementation processes that lead to a product suitable for the market. | Four steps:
|
| The lean approach (LEAN). The term ‘lean production’ was first introduced in 1990 by Womack, Jonas, and Ross [44]. | A production system that produces more and better products using less time, less space, and fewer labor hours. The goal of LEAN is to deliver the product while maximizing value and minimizing waste in the production process. | Five overlapping phases:
|
| The waterfall model. The term ‘waterfall model’ was first introduced in 1976 by Bell and Thayer [45], based on Royce’s conceptualization of H.D Bennington’s model for software development [43]. | An intuitive linear approach with steady requirements, most suitable for mature and stable environments. | Seven steps:
|
| Scrum. Described by Nonaka and Takeuochi in 1986 [46], introduced for object-oriented development in 1995 and described as an agile methodology in 2001 [41,47]. | An agile method for software development based on key characteristics identified in successful companies. | Three phases:
|
| PRojects IN Controlled Environments (PRINCE-2). Named PRINCE-2 in 1986, derived from PROMT used by the Central Computer and Telecommunications Agency since 1979 as the standard to be used for IT projects [15]. | The method is based on seven principles, with a project involving four stages, seven processes, and seven themes, which make it possible to tailor the PRINCE2 method to any size or type of project. | Four stages:
continued business justification, learn from experience, defined roles and responsibilities, manage by stages, manage by exception, focus on products, and tailor to suit the project environment. The seven processes are: starting up a project, initiating a project, directing a project, controlling a stage, managing product delivery, managing a stage boundary, and closing a project. The seven themes are: business case, organization, quality, plans, risk, change, and progress. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kayser, L.; Furstrand, D.; Nyman Rasmussen, E.; Monberg, A.-C.; Karnoe, A. GoTO: A Process-Navigation Tool for Telehealth and -Care Solutions, Designed to Ensure an Efficient Trajectory from Goal Setting to Outcome Evaluation. Informatics 2022, 9, 69. https://doi.org/10.3390/informatics9030069
Kayser L, Furstrand D, Nyman Rasmussen E, Monberg A-C, Karnoe A. GoTO: A Process-Navigation Tool for Telehealth and -Care Solutions, Designed to Ensure an Efficient Trajectory from Goal Setting to Outcome Evaluation. Informatics. 2022; 9(3):69. https://doi.org/10.3390/informatics9030069
Chicago/Turabian StyleKayser, Lars, Dorthe Furstrand, Emil Nyman Rasmussen, Ann-Catrine Monberg, and Astrid Karnoe. 2022. "GoTO: A Process-Navigation Tool for Telehealth and -Care Solutions, Designed to Ensure an Efficient Trajectory from Goal Setting to Outcome Evaluation" Informatics 9, no. 3: 69. https://doi.org/10.3390/informatics9030069





