Choosing a Model for eConsult Specialist Remuneration: Factors to Consider
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. The Champlain BASE eConsult Service
2.4. Data Collection
2.5. The Remuneration Models
- Prorated hourly rate: Specialists are compensated $200 per hour prorated to the length of time it takes them to complete each eConsult. This model is currently used to remunerate specialists who use the Champlain BASE eConsult service and has been in existence since project inception in 2009.
- Incentive model: On top of the standard prorated hourly rate as above, specialists receive a $10 bonus for eConsults completed within 24 h and a $5 bonus for eConsults completed within 48 h. An incentive model is currently being tested for similar eConsult services operating within our province of Ontario.
- Fee-for-Service (Billing code): Specialists are paid a flat fee of $44.50 per eConsult, regardless of how long it takes to complete. This fee code was based on an existing store-forward telemedicine fee code. Additionally, PCPs are remunerated $16.00 for the referral. These fees are based on existing fee codes in Ontario [19].
- Flat weekly fee: Specialists block off a set time each week to devote to answering eConsults. The costs were calculated under two scenarios: (1) each specialty blocks one three-hour period per week at $200 per hour regardless of the number of eConsults they are assigned; or (2) each specialty blocks a minimum of one hour, with the option to increase in one hour increments, if the volume of assigned eConsults is high enough.
2.6. Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| PCP | Primary care provider |
| BASE | Building Access to Specialists through eConsultation |
References
- Barua, B.; Esmail, N. Waiting Your Turn: Wait Times for Health Care in Canada; Fraser Institute: Vancouver, BC, Canada, 2013. [Google Scholar]
- Vidberg, N.; Forsberg, B.C.; Borowitz, M.; Molin, R. International comparisons of waiting times in health care—Limitations and prospects. Health Policy 2013, 112, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Kim-Hwang, J.E.; Chen, A.H.; Bell, D.S.; Guzman, D.; Yee, H.F., Jr.; Kushel, M.B. Evaluating electronic referrals for specialty care at a public hospital. J. Gen. Int. Med. 2010, 25, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- North, F.; Uthke, L.D.; Tulledge-Scheitel, S.M. Integration of e-consultations into the outpatient care process at a tertiary medical centre. J. Telemed. Telecare 2014, 20, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Harno, K.; Paavola, T.; Carlson, C.; Viikinkoski, P. Patient referral by telemedicine: Effectiveness and cost analysis of an Intranet system. J. Telemed. Telecare 2000, 6, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Keely, E.; Liddy, C.; Afkham, A. Utilization, Benefits, and Impact of an e-Consultation Service across Diverse Specialties and Primary Care Providers. Telemed. J. e-Health 2013, 19, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.H.; Murphy, E.J.; Yee, H.F., Jr. eReferral—A new model for integrated care. N. Engl. J. Med. 2013, 368, 2450–2453. [Google Scholar] [CrossRef] [PubMed]
- Straus, S.G.; Chen, A.H.; Yee, H.F., Jr.; Kushel, M.B.; Bell, D.S. Implementation of an electronic referral system for outpatient specialty care. AMIA Ann. Symp. Proc. 2011, 2011, 1337–1346. [Google Scholar]
- Eminovic, N.; de Keizer, N.F.; Wyatt, J.C.; ter Riet, G.; Peek, N.; van Weert, H.C.; Bruijnzeel-Koomen, C.A.; Bindels, P.J. Teledermatologic consultation and reduction in referrals to dermatologists: A cluster randomized controlled trial. Arch. Dermatol. 2009, 145, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Afkham, A.; Drosinis, P.; Joschko, J.; Keely, E. Impact of and satisfaction with a new eConsult service: A mixed methods study of primary care providers. J. Am. Board Fam. Med. 2015, 28, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Pak, H.S.; Datta, S.K.; Triplett, C.A.; Lindquist, J.H.; Grambow, S.C.; Whited, J.D. Cost minimization analysis of a store-and-forward teledermatology consult system. Telemed. J. e-Health 2009, 15, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Whited, J.D.; Hall, R.P.; Foy, M.E.; Marbrey, L.E.; Grambow, S.C.; Dudley, T.K.; Datta, S.; Simel, D.L.; Oddone, E.Z. Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed. J. e-Health 2002, 8, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Rowan, M.S.; Afkham, A.; Maranger, J.; Keely, E. Building access to specialist care through e-consultation. Open Med. 2013, 7, e1–e8. [Google Scholar] [PubMed]
- Chen, A.H.; Kushel, M.B.; Grumback, K.; Yee, H.F., Jr. Practice profile. A safety-net system gains efficiencies through ‘eReferrals’ to specialists. Health Aff. 2010, 29, 969–971. [Google Scholar] [CrossRef] [PubMed]
- Whited, J.D.; Datta, S.; Hall, R.P.; Foy, M.E.; Marbrey, L.E.; Grambow, S.C.; Dudley, T.K.; Simel, D.L.; Oddone, E.Z. An economic analysis of a store and forward teledermatology consult system. Telemed. J. e-Health 2003, 9, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Vimalananda, V.G.; Gupte, G.; Seraj, S.M.; Orlander, J.; Berlowitz, D.; Fincke, B.G.; Simon, S.R. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J. Telemed. Telecare 2015, 21, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Liddy, C.; Maranger, J.; Afkham, A.; Keely, E. Ten steps to establishing an e-consultation service to improve access to specialist care. Telemed. J. e-Health 2013, 19, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Bains, N.; Dall, K.; Hay, C.; Pacey, M.; Sarkella, J.; Ward, M. Population Health Profile: Champlain LHIN; Ministry of Health and Long-Term Care: Toronto, ON, Canada, 2008.
- Ministry of Health and Long-Term Care. Schedule of Benefits for Physician Services under the Health Insurance Act; Ministry of Health and Long-Term Care: Toronto, ON, Canada, 2015.
- Keely, E.; Drosinis, P.; Afkham, A.; Liddy, C. Perspectives of Champlain BASE Specialist Physicians: Their Motivation, Experiences and Recommendations for Providing eConsultations to Primary Care Providers. Stud. Health Technol. Inform. 2015, 209, 38–45. [Google Scholar] [PubMed]
- Berghout, R.M.; Eminovic, N.; de Keizer, N.F.; Birnie, E. Evaluation of general practitioner’s time investment during a store-and-forward teledermatology consultation. Int. J. Med. Inform. 2007, 76, S384–S391. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.W.; Kwong, M.W.; Ledo, L.; Nesbitt, T.S.; Shewry, S.L. Practice models and challenges in teledermatology: A study of collective experiences from teledermatologists. PLoS ONE 2011, 6, e28687. [Google Scholar] [CrossRef] [PubMed]
- Devlin, R.A.; Sarma, S.; Hogg, W. Remunerating primary care physicians: Emerging directions and policy options for Canada. Healthc. Q. 2005, 9, 34–42. [Google Scholar] [CrossRef]
| Distribution (n = 3670) | |
|---|---|
| Median Specialist Response Time (in Days) | 0.78 (IQR: 0.15–3.2) |
| Time to Complete eConsult | Percentage (n) |
| <10 mins | 48.8 (1790) |
| 10–15 mins | 32.0 (1175) |
| 15–20 mins | 15.3 (563) |
| >20 mins | 3.9 (142) |
| Day of Week Submitted | Percentage (n) |
| Sun | 4.3 (156) |
| Mon | 17.9 (656) |
| Tue | 21.4 (785) |
| Wed | 19.4 (711) |
| Thu | 20.4 (749) |
| Fri | 13.8 (505) |
| Sat | 2.9 (108) |
| Day of Week Answered * | Percentage (n) |
| Sun | 7.5 (277) |
| Mon | 18.2 (669) |
| Tue | 17.3 (636) |
| Wed | 19.7 (724) |
| Thu | 17.5 (643) |
| Fri | 13.1 (481) |
| Sat | 6.5 (239) |
| Model | Cost ($) | Average Cost per eConsult ($) |
|---|---|---|
| Prorated hourly rate | 167,783 | 45.72 |
| Prorated hourly rate + incentive | 190,488 | 51.90 |
| Fee-for-service | 222,035 | 60.50 |
| Flat weekly sessional fee | - | - |
| Booked clinic time | 1,238,400 | 337.44 |
| 1-h increments | 489,600 | 133.41 |
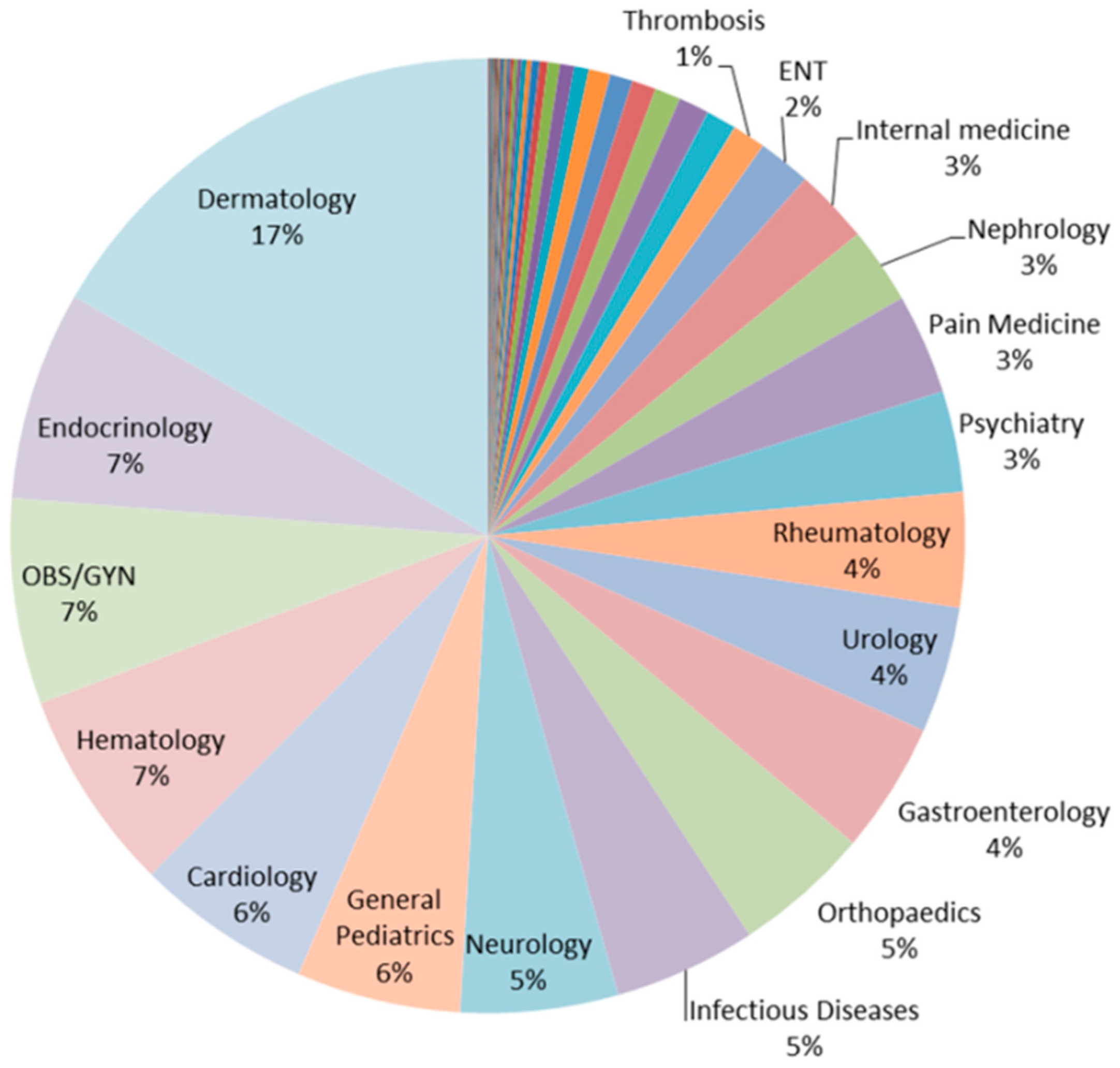
| Specialty | <1 Day | <2 Days | Total |
|---|---|---|---|
| Dermatology | 90.67% (554) | 6.55% (40) | 611 |
| Endocrinology | 78.33% (206) | 12.17% (32) | 263 |
| OBS/GYN | 37.50% (96) | 16.41% (42) | 256 |
| Hematology | 29.08% (73) | 11.55% (29) | 251 |
| Cardiology | 40.18% (88) | 14.16% (31) | 219 |
| General Pediatrics | 42.72% (88) | 9.71% (20) | 206 |
| Neurology | 78.06% (153) | 6.63% (13) | 196 |
| Infectious Diseases | 62.56% (122) | 7.18% (14) | 195 |
| Orthopaedics | 24.86% (43) | 13.87% (24) | 173 |
| Gastroenterology | 38.04% (62) | 14.72% (24) | 163 |
| Model | Pros | Cons |
|---|---|---|
| Prorated hourly rate | Allows for more specialty services to be available and payment only when specialist responds; Allows for flexibility with respect to case volume and complexity | Managed service that is separate from usual funding model |
| Prorated hourly rate with incentive | Has the potential to promote faster responses from specialists | Quality of the specialist response may be lower; Questionable added cost given: non-urgent nature of eConsult; measured median [average] response intervals without the incentive |
| Physician billing code | More aligned with usual payment for traditional consultations | Does not take into account case complexity; Physicians have to complete the billing process themselves; Less flexibility when addressing payment for non-physician specialties |
| Flat weekly sessional fee | Simplified planning and payment mechanism for specialists and payer | Not cost-efficient for low-volume specialties; May negatively impact response time |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liddy, C.; Deri Armstrong, C.; McKellips, F.; Drosinis, P.; Afkham, A.; Keely, E. Choosing a Model for eConsult Specialist Remuneration: Factors to Consider. Informatics 2016, 3, 8. https://doi.org/10.3390/informatics3020008
Liddy C, Deri Armstrong C, McKellips F, Drosinis P, Afkham A, Keely E. Choosing a Model for eConsult Specialist Remuneration: Factors to Consider. Informatics. 2016; 3(2):8. https://doi.org/10.3390/informatics3020008
Chicago/Turabian StyleLiddy, Clare, Catherine Deri Armstrong, Fanny McKellips, Paul Drosinis, Amir Afkham, and Erin Keely. 2016. "Choosing a Model for eConsult Specialist Remuneration: Factors to Consider" Informatics 3, no. 2: 8. https://doi.org/10.3390/informatics3020008






