Enabling Virtual Sensing as a Service
Abstract
:1. Introduction
2. Background and Related Work
2.1. Sensor Data Management Systems
2.2. Collaboration and Crowdsourcing for Sensors
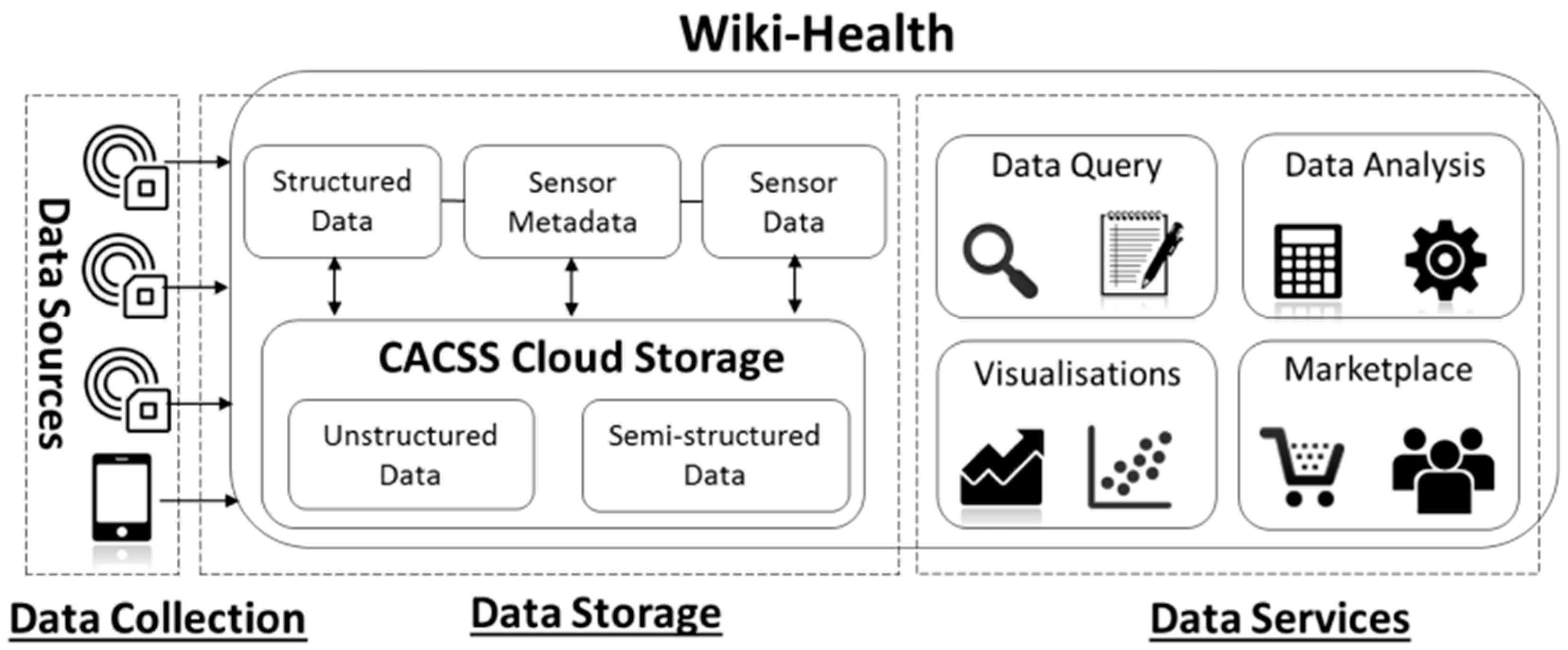
3. Wiki-Health
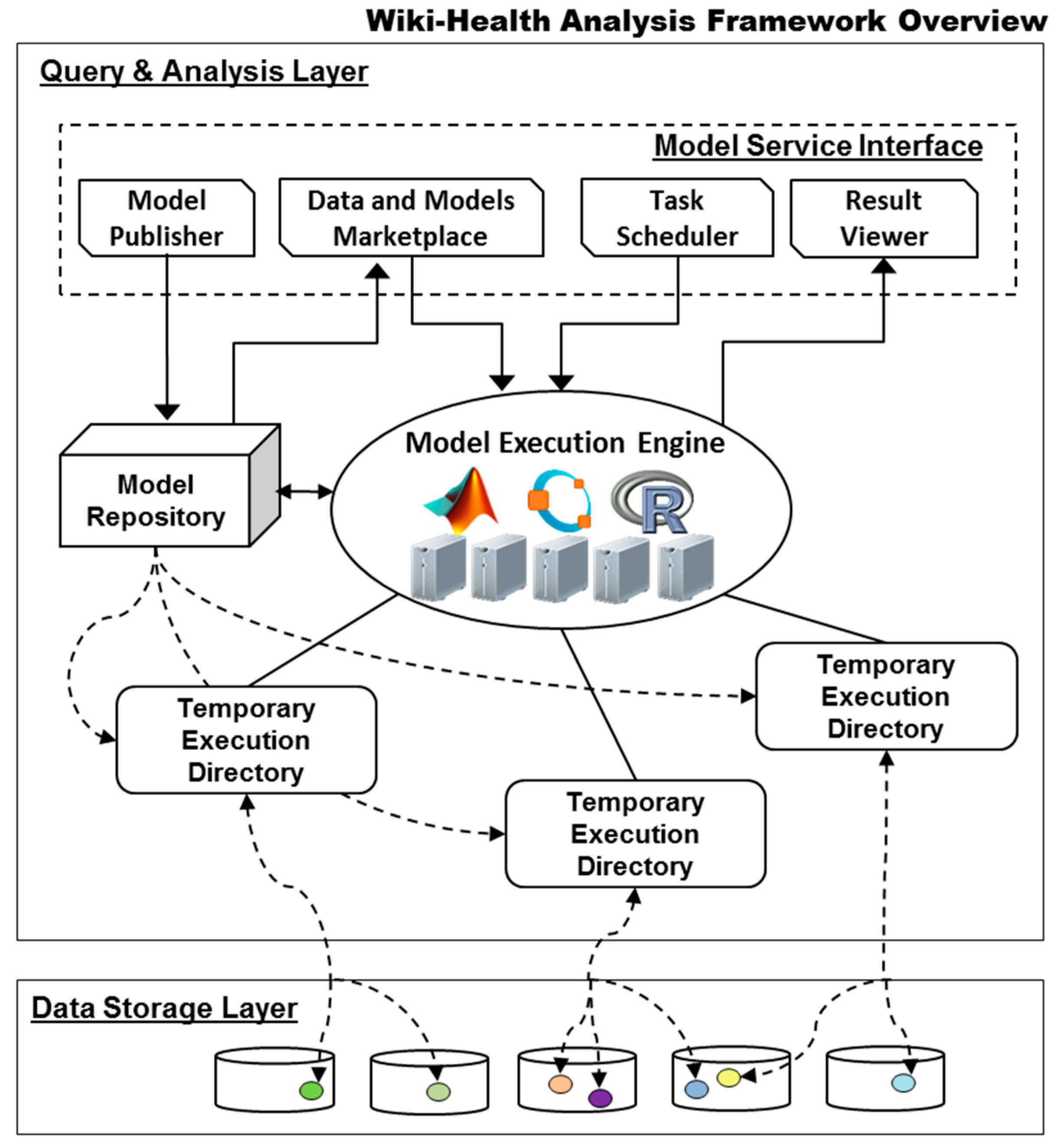
3.1. Wiki-Health Analysis Framework
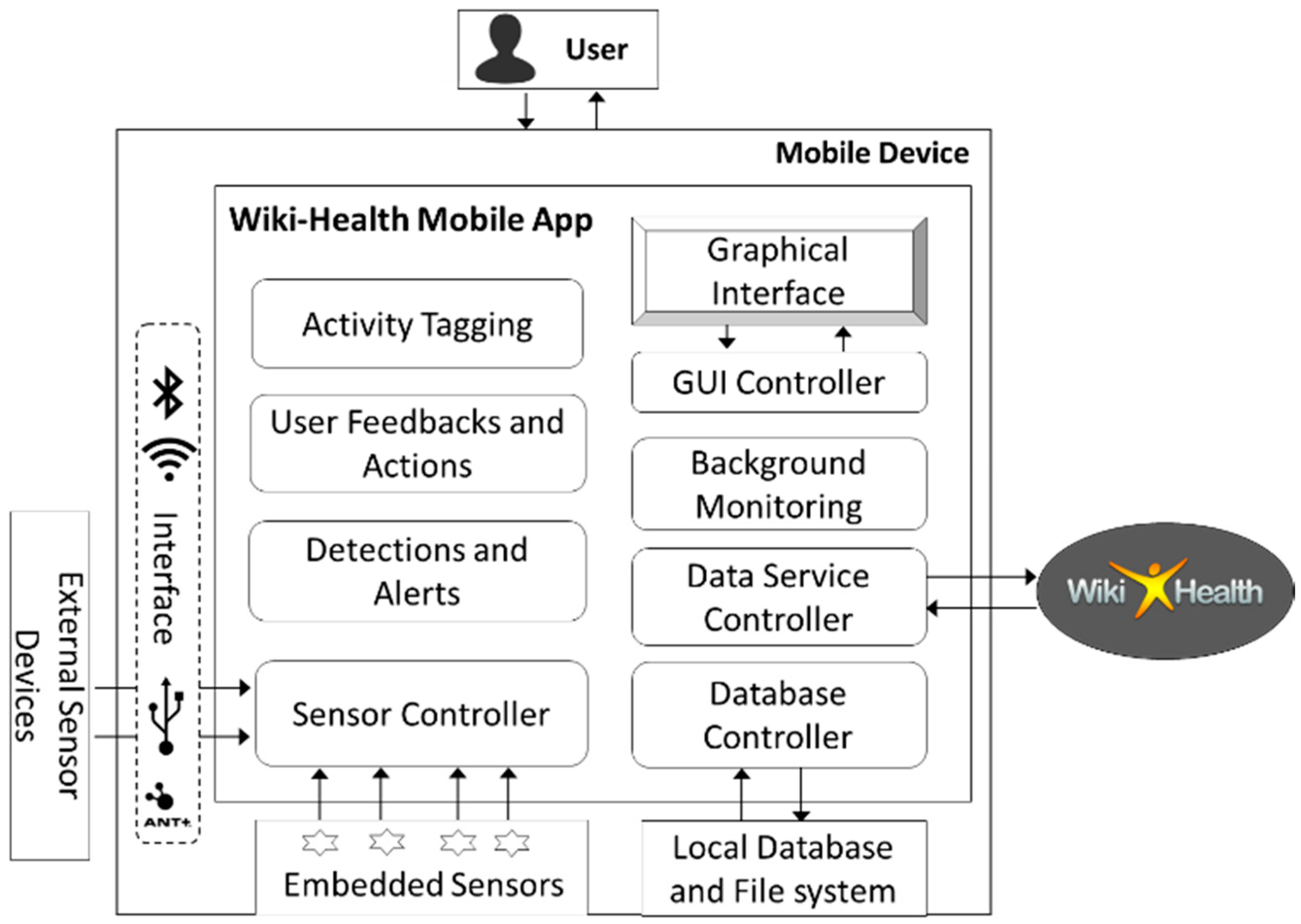
3.2. Wiki-Health Mobile App
3.3. Virtual Sensing as a Service Overview
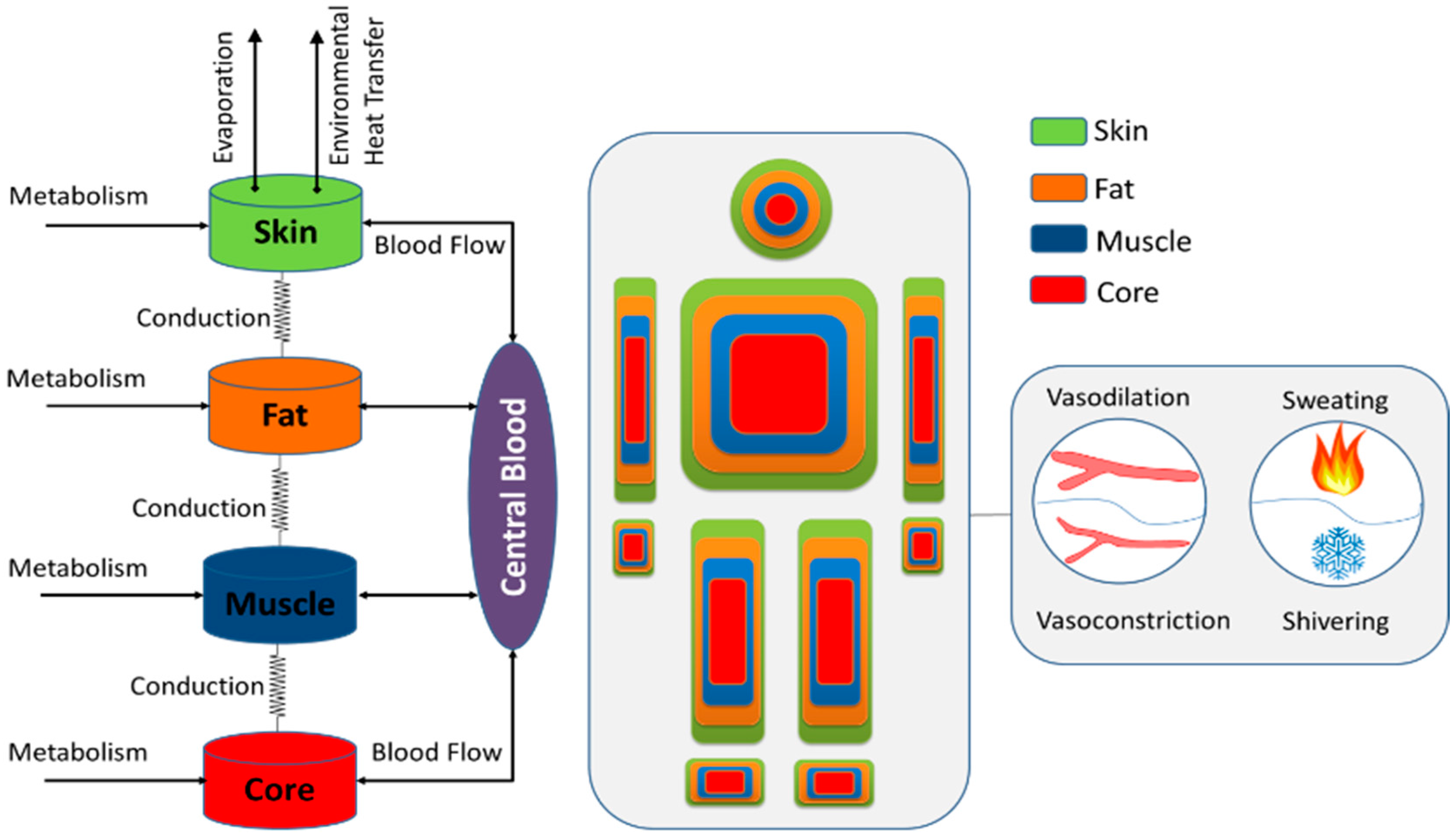
4. Full Body Model Associated with Human Temperature and Energy Transformations
4.1. The Controlled System
4.2. The Controlling System
5. Model Integration and Implementation
5.1. Heart Rate Based Metabolic Rate Estimation
5.2. Basal Metabolic Rate Estimation
5.3. Personal Sensor Data
5.4. Environmental and Geographic Data
5.5. Virtual Sensing Service
6. Experimental Evaluation
6.1. Participants and Setup
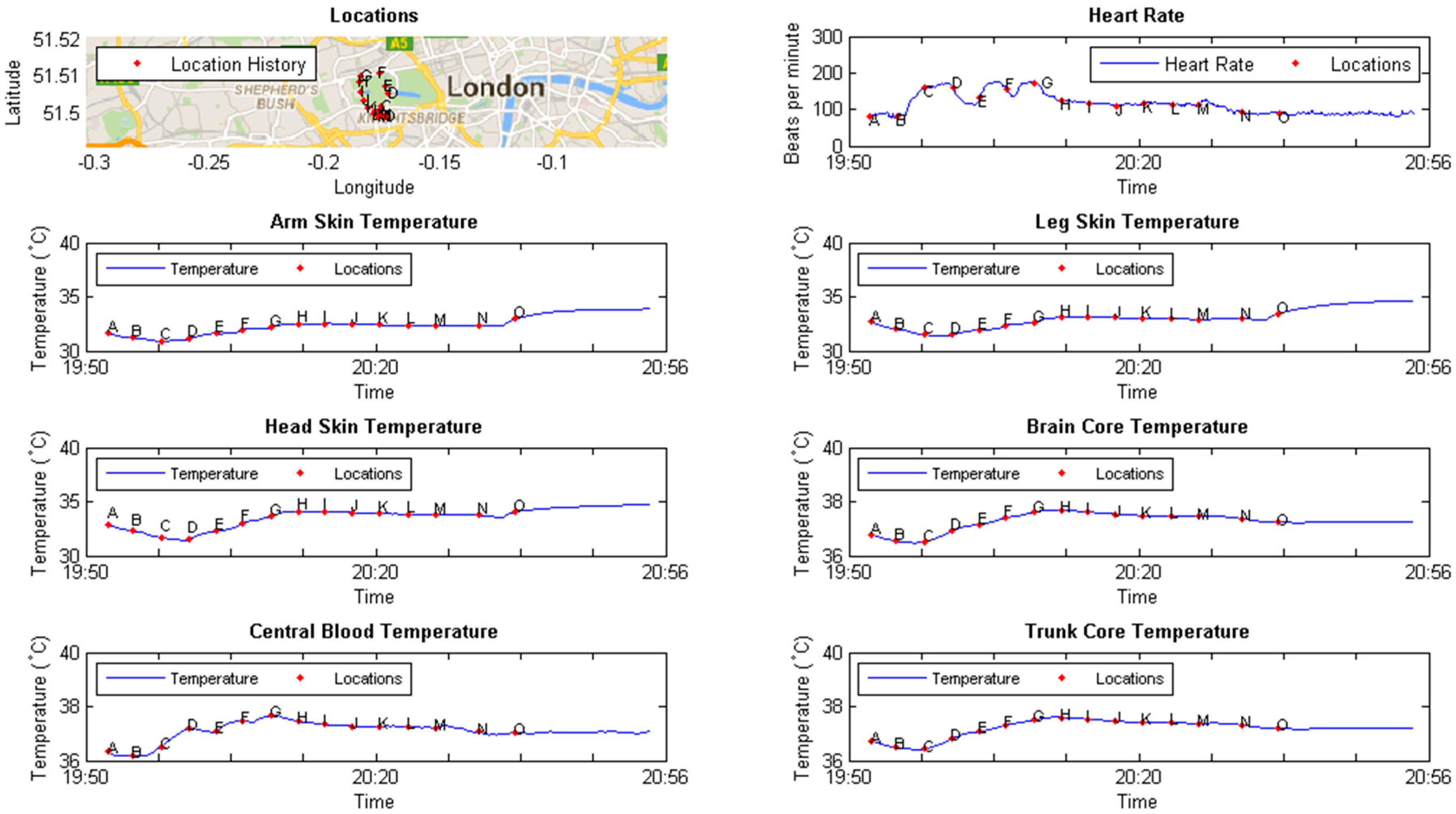
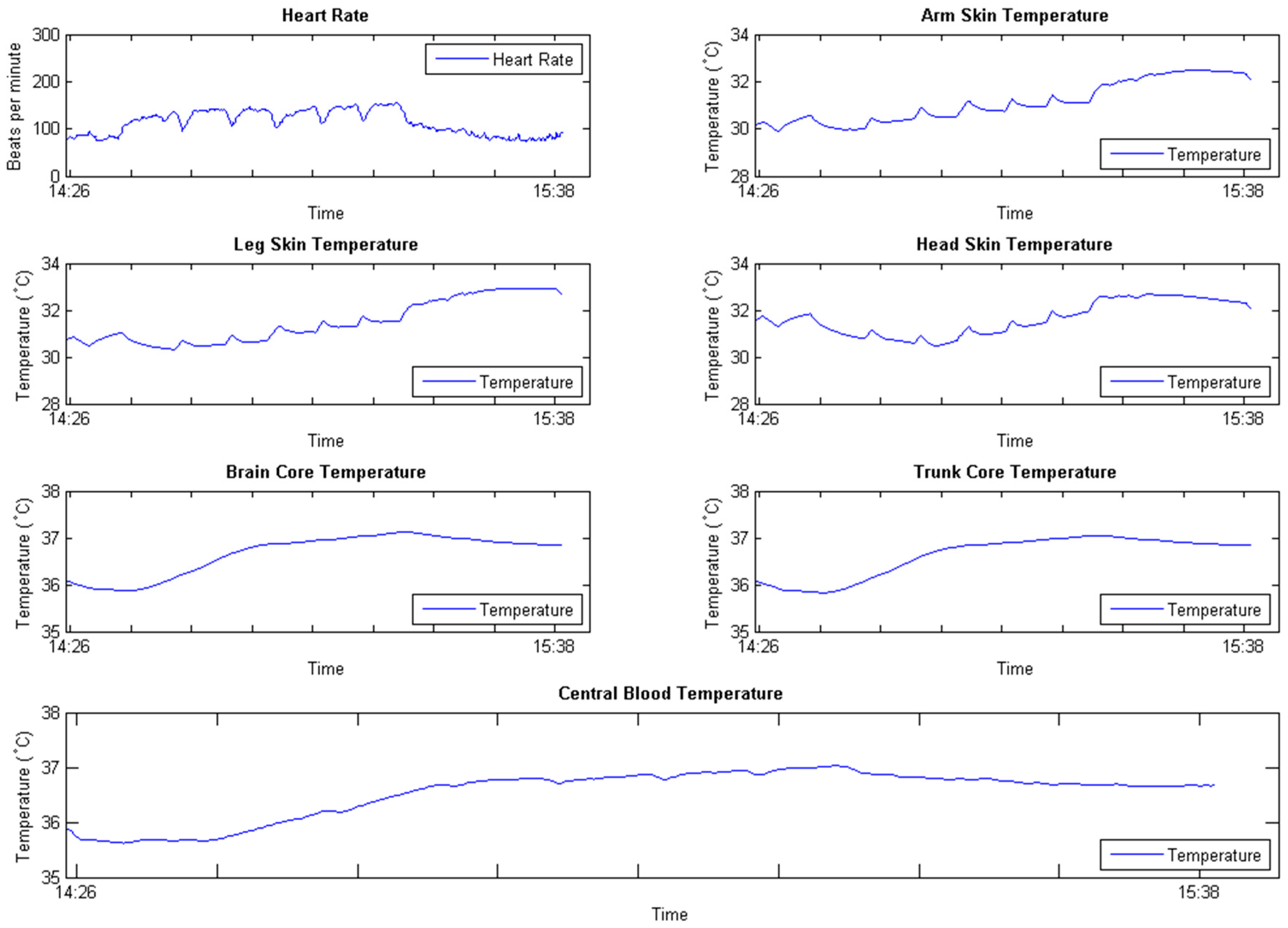
6.2. Results
7. Conclusion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Stephant, J.; Charara, A.; Meizel, D. Virtual sensor: Application to vehicle sideslip angle and transversal forces. IEEE Trans. Ind. Electron. 2004, 51, 278–289. [Google Scholar] [CrossRef]
- Kusiak, A.; Zheng, H.; Zhang, Z. Virtual wind speed sensor for wind turbines. J. Energy Eng. 2010, 137, 59–69. [Google Scholar] [CrossRef]
- Raveendranathan, N.; Galzarano, S.; Loseu, V.; Gravina, R.; Giannantonio, R.; Sgroi, M.; Jafari, R.; Fortino, G. From modeling to implementation of virtual sensors in body sensor networks. IEEE Sens. J. 2012, 12, 583–593. [Google Scholar] [CrossRef]
- Van Beek, J.H.; Supandi, F.; Gavai, A.K.; de Graaf, A.A.; Binsl, T.W.; Hettling, H. Simulating the physiology of athletes during endurance sports events: Modelling human energy conversion and metabolism. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2011, 369, 4295–4315. [Google Scholar] [CrossRef] [PubMed]
- Bouchama, A.; Knochel, J.P. Heat stroke. New Engl. J. Med. 2002, 346, 1978–1988. [Google Scholar] [CrossRef] [PubMed]
- Gunga, H.-C.; Sandsund, M.; Reinertsen, R.E.; Sattler, F.; Koch, J. A non-invasive device to continuously determine heat strain in humans. J. Therm. Biol. 2008, 33, 297–307. [Google Scholar] [CrossRef]
- Yang, L.; Li, G.; Yike, G. Enabling health monitoring as a service in the cloud. In Proceedings of 2014 IEEE/ACM 7th International Conference on Utility and Cloud Computing, UCC’14, London, UK, 8–11 December 2014; pp. 127–136.
- Li, Y.; Guo, Y. Wiki-health: From quantified self to self-understanding. Gener. Comput. Syst. 2015, 56, 333–359. [Google Scholar] [CrossRef]
- Madden, S.R.; Franklin, M.J.; Hellerstein, J.M.; Hong, W. Tinydb: An acquisitional query processing system for sensor networks. ACM Trans. Database Syst. 2005, 30, 122–173. [Google Scholar] [CrossRef]
- Abadi, D.J.; Carney, D.; Çetintemel, U.; Cherniack, M.; Convey, C.; Lee, S.; Stonebraker, M.; Tatbul, N.; Zdonik, S. Aurora: A new model and architecture for data stream management. The VLDB J. 2003, 12, 120–139. [Google Scholar] [CrossRef]
- Yao, Y.; Gehrke, J. The cougar approach to in-network query processing in sensor networks. ACM Sigmod Rec. 2002, 31, 9–18. [Google Scholar] [CrossRef]
- Yuriyama, M.; Kushida, T. Sensor-cloud infrastructure-physical sensor management with virtualized sensors on cloud computing. In Proceedings of 2010 13th International Conference on Network-Based Information Systems (NBiS), Takayama, Japan, 4–16 September 2010; pp. 1–8.
- ThingSpeak. Available online: http://thingspeak.com (accessed on 24 March 2016).
- Xively. Available online: https://xively.com (accessed on 1 July 2015).
- Wang, Y.; Hu, W.; Wu, Y.; Cao, G. Smartphoto: A resource-aware crowdsourcing approach for image sensing with smartphones. In Proceedings of the 15th ACM international symposium on Mobile ad hoc networking and computing, MobiHoc’14, Philadelphia, PA, USA, 11–14 August 2014; pp. 113–122.
- Guo, X.; Chan, E.C.; Liu, C.; Wu, K.; Liu, S.; Ni, L.M. Shopprofiler: Profiling shops with crowdsourcing data. In Proceedings of 2014 IEEE Proceedings, INFOCOM, Toronto, ON, Canada, 27 April–2 May 2014; pp. 1240–1248.
- Artikis, A.; Weidlich, M.; Schnitzler, F.; Boutsis, I.; Liebig, T.; Piatkowski, N.; Bockermann, C.; Morik, K.; Kalogeraki, V.; Marecek, J. Heterogeneous stream processing and crowdsourcing for urban traffic management. In Proceedings of 17th International Conference on Extending Database Technology (EDBT), Athens, Greece, 24–28 March 2014; pp. 712–723.
- Zheng, Y.; Zhang, L.; Xie, X.; Ma, W.-Y. Mining interesting locations and travel sequences from GPS trajectories. In Proceedings of the 18th International Conference on World Wide Web, Madrid, Spain, 20–24 April 2009; pp. 791–800.
- Welbourne, E.; Tapia, E.M. Crowdsignals: A call to crowdfund the community’s largest mobile dataset. In Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct Publication, Seattle, WA, USA, 13–17 September 2014; pp. 873–877.
- Welbourne, E.; Wu, P.; Bao, X.; Munguia-Tapia, E. Crowdsourced mobile data collection: Lessons learned from a new study methodology. In Proceedings of the 15th Workshop on Mobile Computing Systems and Applications, Santa Barbara, CA, USA, 26–27 February 2014; p. 2.
- MathWorks. Matlab: The Language of Technical Computing (Desktop Tools and Development Environment), 7th ed.; The MathWorks Inc.: Natick, MA, USA, 2005; Volume 9. [Google Scholar]
- GNU Octave. Available online: http://www.gnu.org/software/octave/ (accessed on 1 July 2015).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Reith, J.; Jorgensen, H.; Pedersen, P.; Nakamaya, H.; Jeppesen, L.; Olsen, T.; Raaschou, H. Body temperature in acute stroke: Relation to stroke severity, infarct size, mortality, and outcome. Lancet 1996, 347, 422–425. [Google Scholar] [CrossRef]
- Stolwijk, J.A. A Mathematical Model of Physiological Temperature Regulation in Man; National Aeronautics and Space Administration: Washington, DC, USA, 1971.
- Havenith, G. Interaction of clothing and thermoregulation. Exog. Dermatol. 2003, 1, 221–230. [Google Scholar] [CrossRef]
- Keytel, L.; Goedecke, J.; Noakes, T.; Hiiloskorpi, H.; Laukkanen, R.; van der Merwe, L.; Lambert, E. Prediction of energy expenditure from heart rate monitoring during submaximal exercise. J. Sports Sci. 2005, 23, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Mifflin, M.D.; St Jeor, S.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [PubMed]
- Zephyr. Available online: http://www.zephyranywhere.com (accessed on 1 July 2015).
- OpenWeatherMap. Available online: http://www.openweathermap.org (accessed on 1 July 2015).
- Weather Underground. Available online: http://www.wunderground.com (accessed on 1 July 2015).
- Google Map. Available online: http://maps.google.com (accessed on 1 July 2015).
- Haklay, M.; Weber, P. Openstreetmap: User-generated street maps. IEEE Perv. Comput. 2008, 7, 12–18. [Google Scholar] [CrossRef]
- Hardy, J.; Stolwijk, J. Partitional calorimetric studies of man during exposures to thermal transients. J. Appl. Phys. 1966, 21, 1799–1806. [Google Scholar]
- Young, A.J.; Muza, S.R.; Sawka, M.N.; Gonzalez, R.R.; Pandolf, K.B. Human thermoregulatory responses to cold air are altered by repeated cold water immersion. J. Appl. Phys. 1986, 60, 1542–1548. [Google Scholar]
- Houtekamer, P.L.; Mitchell, H.L. Data assimilation using an ensemble kalman filter technique. Mon. Weather Rev. 1998, 126, 796–811. [Google Scholar] [CrossRef]


| Symbol | Meaning | Unit |
|---|---|---|
| Temperature of node | °C | |
| Total metabolic heat production in node | kcal/h | |
| Total evaporative heat loss from node | kcal/h | |
| Convective heat transfer between central blood and node | kcal/h | |
| Conductive heat transfer between node and adjacent node | kcal/h | |
| Radiant heat transfer coefficient of segment | kcal/m2/h/°C | |
| Convective and conductive heat transfer coefficient of segment | kcal/m2/h/°C | |
| Total combined heat transfer coefficient of segment | kcal/h/°C | |
| Total surface area of segment | m2 | |
| Air velocity | m/s | |
| The temperature of surrounding environment | °C |
| Node (N) | Segment (i) | Layer | C (kcal/°C) | QB (kcal/°C) | EB (kcal/°C) | BFB (L/H) | TC (Kcal/H/°C) |
|---|---|---|---|---|---|---|---|
| 1 | Head | Core | 2.22 | 12.84 | 0.00 | 45.00 | 1.38 |
| 2 | Muscle | 0.33 | 0.10 | 0.00 | 0.12 | 11.40 | |
| 3 | Fat | 0.22 | 0.11 | 0.00 | 0.13 | 13.80 | |
| 4 | Skin | 0.24 | 0.08 | 0.63 | 1.44 | 0.00 | |
| 5 | Trunk | Core | 9.82 | 45.38 | 9.00 | 210.00 | 1.37 |
| 6 | Muscle | 16.15 | 5.00 | 0.00 | 6.00 | 4.75 | |
| 7 | Fat | 4.25 | 2.13 | 0.00 | 2.56 | 19.80 | |
| 8 | Skin | 1.21 | 0.40 | 3.25 | 2.10 | 0.00 | |
| 9 | Arm | Core | 1.41 | 0.70 | 0.00 | 0.84 | 1.20 |
| 10 | Muscle | 3.04 | 0.95 | 0.00 | 1.14 | 8.90 | |
| 11 | Fat | 0.58 | 0.17 | 0.00 | 0.20 | 26.20 | |
| 12 | Skin | 0.43 | 0.13 | 1.20 | 0.50 | 0.00 | |
| 13 | Hand | Core | 0.14 | 0.08 | 0.00 | 0.10 | 5.50 |
| 14 | Muscle | 0.06 | 0.20 | 0.00 | 0.24 | 9.65 | |
| 15 | Fat | 0.09 | 0.03 | 0.00 | 0.04 | 9.90 | |
| 16 | Skin | 0.17 | 0.05 | 0.45 | 2.00 | 0.00 | |
| 17 | Leg | Core | 4.24 | 2.23 | 0.00 | 2.69 | 9.00 |
| 18 | Muscle | 9.17 | 2.86 | 0.00 | 3.43 | 12.40 | |
| 19 | Fat | 1.43 | 0.43 | 0.00 | 0.52 | 64.00 | |
| 20 | Skin | 1.08 | 0.32 | 2.85 | 2.85 | 0.00 | |
| 21 | Feet | Core | 0.23 | 0.13 | 0.00 | 0.16 | 14.00 |
| 22 | Muscle | 0.06 | 0.02 | 0.00 | 0.02 | 17.70 | |
| 23 | Fat | 0.13 | 0.04 | 0.00 | 0.05 | 14.10 | |
| 24 | Skin | 0.22 | 0.07 | 0.62 | 3.00 | 0.00 | |
| 25 | Central Blood | 2.25 | n/a | n/a | n/a | n/a | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Pandis, I.; Guo, Y. Enabling Virtual Sensing as a Service. Informatics 2016, 3, 3. https://doi.org/10.3390/informatics3020003
Li Y, Pandis I, Guo Y. Enabling Virtual Sensing as a Service. Informatics. 2016; 3(2):3. https://doi.org/10.3390/informatics3020003
Chicago/Turabian StyleLi, Yang, Ioannis Pandis, and Yike Guo. 2016. "Enabling Virtual Sensing as a Service" Informatics 3, no. 2: 3. https://doi.org/10.3390/informatics3020003
APA StyleLi, Y., Pandis, I., & Guo, Y. (2016). Enabling Virtual Sensing as a Service. Informatics, 3(2), 3. https://doi.org/10.3390/informatics3020003





