Determinants of Body Mass Index and Intelligence Quotient of Elementary School Children in Mountain Area of Nepal: An Explorative Study
Abstract
:1. Background
2. Experimental Section
2.1. Study Design and Sampling

2.2. Study Setting and Measurement
2.2.1. Intelligence Quotient (IQ)
2.2.2. BMI
2.2.3. Semi-Structure Questionnaire
2.3. Classification of BMI and IQ
2.4. Characteristics of Variables
2.5. Data Management
2.6. Data Analysis
2.7. Research Equation Model
2.8. Validity and Reliability
2.9. Ethical Consideration
3. Results
3.1. Characteristics of Elementary School Students and Their Households
| Characteristics | Category | Frequency (%) | BMI | IQ Score | ||
|---|---|---|---|---|---|---|
| Mean ±SD | pValue | Mean ±SD | pValue | |||
| Gender | Boys | 95 (54.9) | 16.3 ± 3.1 | 0.221 | 95.2 ± 11.3 | 0.582 |
| Girls | 78 (45.1) | 16.6 ± 3.9 | 93.2 ± 10.2 | |||
| Age | Up to 12 years | 109 (63.0) | 19.6 ± 2.7 | 0.012 | 96.7 ± 14.6 | 0.795 |
| >12 years | 64 (37.0) | 20.7 ± 2.9 | 96.1 ± 13.6 | |||
| Personality Attitude | Faithful | 6 (3.5) | 17.8 ± 4.3 | 0.061 | 94.6 ± 9.4 | 0.312 |
| Active | 95 (54.9) | 15.9 ± 3.1 | 94.2 ± 10.8 | |||
| Kind | 45 (26.0) | 16.4 ± 3.7 | 95.4 ± 11.1 | |||
| Shy/Emotional | 27 (15.6) | 17.9 ± 3.8 | 92.8 ± 11.1 | |||
| Grade | 5 | 75 (43.1) | 14.4 ± 2.1 | <0.001 | 92.0 ± 10.5 | 0.041 |
| 6 | 56 (32.7) | 16.9 ± 2.9 | 96.7 ± 10.8 | |||
| 7 | 42 (24.2) | 19.4 ± 3.9 | 95.2 ± 10.8 | |||
| Classroom performance | Excellent | 5 (2.9) | 18.8 ± 4.5 | 0.078 | 96.0 ± 16.9 | 0.143 |
| Good | 101 (58.4) | 15.7 ± 3.1 | 93.7 ± 10.4 | |||
| Average | 60 (34.7) | 17.1 ± 3.9 | 96.1 ± 10.9 | |||
| Poor | 7 (4.0) | 18.0 ± 1.9 | 86.7 ± 9.1 | |||
| Favorite subject | Math | 83 (48.0) | 16.2 ± 3.4 | 0.122 | 94.0 ± 10.7 | 0.757 |
| Science | 52 (30.0) | 17.2 ± 3.7 | 95.3 ± 11.8 | |||
| Social science | 38 (22.0) | 15.8 ± 3.2 | 93.8 ± 9.9 | |||
| Main source of food | Local | 99 (57.6) | 17.9 ± 3.3 | <0.001 | 97.0 ± 9.6 | 0.041 |
| Imported | 74 (42.4) | 14.4 ± 2.7 | 90.6 ± 11.4 | |||
| Living with | Parents | 8 (4.6) | 16.8 ± 4.1 | 0.063 | 92.8 ± 10.0 | 0.701 |
| Parents and grandparents | 95 (54.9) | 15.9 ± 3.1 | 94.2 ± 10.8 | |||
| Grandparents only | 41 (23.6)) | 16.6 ± 3.8 | 95.6 ± 11.3 | |||
| Others | 29 (16.7) | 17.8 ± 3.7 | 93.1 ± 10.8 | |||
| Father’s education | No formal education | 8 (4.6) | 12.8 ± 5.6 | 0.006 | 76.2 ± 3.8 | <0.001 |
| Primary | 62 (35.8) | 15.6 ± 3.8 | 87.9 ± 7.9 | |||
| Secondary | 70 (40.5) | 17.3 ± 3.1 | 95.8 ± 7.8 | |||
| Higher education | 33 (19.1) | 17.0 ± 1.7 | 107.8 ± 5.0 | |||
| Mother’s education | No formal education | 55 (31.7) | 16.2 ± 4.4 | 0.34 | 86.7 ± 8.3 | <0.001 |
| Primary | 71 (41.1) | 15.9 ± 3.5 | 92.5 ± 8.9 | |||
| Secondary | 40 (23.1) | 17.5 ± 1.6 | 106.2 ± 5.2 | |||
| Higher education | 7 (4.1) | 16.6 ± 2.0 | 105.0 ± 5.2 | |||
| Economic category | Ultra poor | 18 (10.4) | 12.1 ± 2.2 | <0.001 | 82.3 ± 12.1 | <0.001 |
| Poor | 49 (28.3) | 14.7 ± 2.0 | 93.1 ± 9.8 | |||
| Relatively non poor | 106 (61.3) | 17.9 ± 3.3 | 96.9 ± 9.7 | |||
| BMI | Thin (<15.3)a | 16 (9.3) | 75.56 ± 1.54 | 0.003 | ||
| Average (15.4–23.9)b | 121 (70.7) | 98.00 ± 13.86 | ||||
| High (>24)c | 36 (21.0) | 100.75 ± 10.38 | ||||
| IQ | Poor (<85) | 53 (30.6) | 19.5 ± 4.9 | 0.08 | ||
| Average (85–115) | 116 (67.1) | 20.8 ± 2.6 | ||||
| Smart (>115) | 4 (2.3) | 21.3 ± 0.4 | ||||

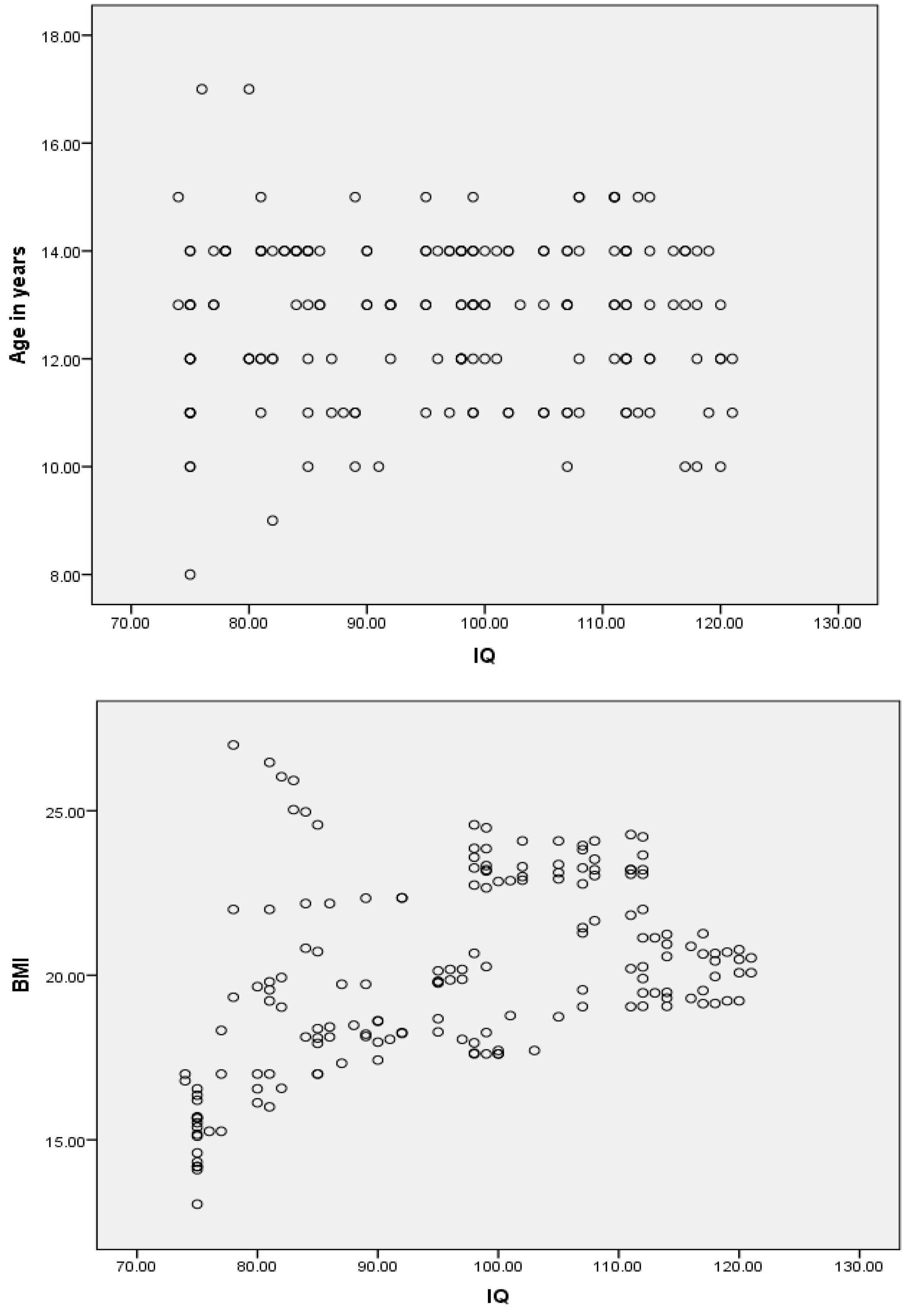
3.2. Regression Analysis
| Determinants | BMI | p Value | IQ Score | p Value |
|---|---|---|---|---|
| Standardized Beta | Standardized Beta | |||
| Intercept | 17.1 | <0.001 | 78.1 | <0.001 |
| Individual Factors | ||||
| Age in years | 0.17 | 0.03 | 0.19 | 0.671 |
| Age2 | −0.22 | 0.03 | −0.21 | 0.632 |
| IQ | 0.13 | 0.22 | ||
| IQ2 | −0.10 | 0.01 | ||
| BMI | 0.29 | 0.062 | ||
| BMI2 | −0.18 | 0.084 | ||
| Frequency of serious illness | −0.15 | 0.11 | −0.15 | 0.004 |
| School Factors | ||||
| School attendance in a year | 0.48 | <0.001 | ||
| Grade of student: 7 (Ref.) | ||||
| 5 | −0.18 | 0.04 | −0.12 | 0.167 |
| 6 | −0.13 | 0.02 | −0.15 | 0.086 |
| Family and social factors | ||||
| Economic status: Non poor (Ref.) | ||||
| Poor | −0.43 | <0.001 | −0.19 | 0.431 |
| Ultra poor | −0.53 | <0.001 | −0.33 | 0.047 |
| Father’s education: Higher (Ref.) | ||||
| No formal education | −0.01 | 0.83 | −0.21 | <0.001 |
| Primary | −0.09 | 0.14 | −0.20 | 0.004 |
| Secondary | 0.03 | 0.58 | −0.12 | 0.045 |
| Mother’s education: Higher (Ref.) | ||||
| No formal education | −0.44 | <0.001 | ||
| Primary | −0.28 | 0.002 | ||
| Secondary | −0.12 | 0.162 | ||
| Food type: Local food (Ref.) | ||||
| Imported food | 0.06 | 0.30 | −0.10 | 0.043 |
| R2/Adjusted R2 | 0.68/0.66 | 0.81/0.79 | ||
| F | 26.8 | 24.5 | ||
| p value | <0.001 | <0.001 | ||
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Global Population of Primary School Age, 2000–2015. Available online: http://huebler.blogspot.kr/2008/03/global-population-of-primary-school-age.html (accessed on 18 August 2015).
- Onis, M. Relationship between physical growth and motor development in the WHO child growth standards. Acta Paediatr. 2006, 95, 96–101. [Google Scholar]
- Zong, X.-N.; Li, H. Physical growth of children and adolescents in China over the past 35 years. Bull. World Health Organ. 2014, 92, 555–564. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Onyango, A.; Borghi, E.; Siyam, A.; Blössner, M.; Lutter, C. Worldwide implementation of the WHO child growth standards. Public Health Nutr. 2012, 15, 1603–1610. [Google Scholar] [CrossRef] [PubMed]
- DeHart, G.; Sroufe, L.A.; Cooper, R.G. Child Development: Its Nature and Course; McGraw-Hill Companies: New York, NY, USA, 2000. [Google Scholar]
- Wachs, T.D. Necessary But Not Sufficient: The Respective Roles of Single and Multiple Influences on Individual Development; American Psychological Association: Washington, DC, USA, 2000. [Google Scholar]
- Brooks-Gunn, J.; Duncan, G.J. The effects of poverty on children. Futur. Child. 1997, 7, 55–71. [Google Scholar] [CrossRef]
- Northstone, K.; Joinson, C.; Emmett, P.; Ness, A.; Paus, T. Are dietary patterns in childhood associated with IQ at 8 years of age? A population-based cohort study. J. Epidemiol. Community Health 2011, 66, 36–95. [Google Scholar] [CrossRef] [PubMed]
- Monette, S.; Bigras, M.; Guay, M.-C. The role of the executive functions in school achievement at the end of Grade 1. J. Exp. Child Psychol. 2011, 109, 158–173. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Vander Hoorn, S.; Murray, C.J. Selected major risk factors and global and regional burden of disease. Lancet 2002, 360, 1347–1360. [Google Scholar] [CrossRef]
- Caballero, B. A nutrition paradox—Underweight and obesity in developing countries. N. Engl. J. Med. 2005, 352, 1514–1516. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Finucane, M.M.; Paciorek, C.J.; Flaxman, S.R.; White, R.A.; Donner, A.J.; Ezzati, M. Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: A systematic analysis of population representative data. Lancet 2012, 380, 824–834. [Google Scholar] [CrossRef]
- Doak, C.M.; Adair, L.S.; Bentley, M.; Monteiro, C.; Popkin, B.M. The dual burden household and the nutrition transition paradox. Int. J. Obes. 2005, 29, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.; Yang, W.; Chen, C.S.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Dhobale, R.V.; Kadam, Y.R.; Gore, A.D.; Dhumale, G.B. Pattern of BMI in school going children from rural area. Innov. J. Med. Health Sci. 2013, 3, 1. [Google Scholar]
- Goon, D.T.; Toriola, A.L.; Shaw, B.S.; Amusa, L.O.; Monyeki, M.A.; Akinyemi, O.; Alabi, O.A. Anthropometrically determined nutritional status of urban primary schoolchildren in Makurdi, Nigeria. BMC Public Health 2011, 11, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Ferrar, K.; Olds, T. Thin adolescents: Who are they? What do they do? Socio-demographic and use-of-time characteristics. Prev. Med. 2010, 51, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, R.; Spagnoli, T.; Galotto, C.; Pugliese, E.; Carta, A.; Cesari, L. Socioeconomic status, overweight and obesity in prepuberal children: A study in an area of Northern Italy. Eur. J. Epidemiol. 2000, 16, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Kimm, S.Y.; Obarzanek, E.; Barton, B.A.; Aston, C.E.; Similo, S.L.; Morrison, J.A.; Sabry, Z.; Schreiber, G.B.; McMahon, R.P. Race, socioeconomic status, and obesity in 9-to 10-year-old girls: The NHLBI growth and health study. Ann. Epidemiol. 1996, 6, 266–275. [Google Scholar] [CrossRef]
- Langnäse, K.; Mast, M.; Müller, M.J. Social class differences in overweight of prepubertal children in northwest Germany. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, F.; Renga, G.; Versino, E. Determinants of social inequalities in health in Italy. Eur. PubMed Cent. 1999, 12 (Suppl. 1), 67–74. [Google Scholar]
- Tomchek, S.D.; Lane, S.J. Full-term low birth weight infants: Etiology and developmental implications. Phys. Occup. Ther. Pediatr. 1994, 13, 43–65. [Google Scholar] [CrossRef]
- Cimadevilla, J.M.; Roldán, L.; París, M.; Arnedo, M.; Roldán, S. Spatial learning in a virtual reality-based task is altered in very preterm children. J. Clin. Exp. Neuropsychol. 2014, 36, 1002–1008. [Google Scholar] [CrossRef] [PubMed]
- Calvin, C.M.; Deary, I.J.; Webbink, D.; Smith, P.; Fernandes, C.; Lee, S.H.; Luciano, M.; Visscher, P.M. Multivariate genetic analyses of cognition and academic achievement from two population samples of 174,000 and 166,000 school children. Behav. Genet. 2012, 42, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Bierkens, J.; Buekers, J.; Van Holderbeke, M.; Torfs, R. Health impact assessment and monetary valuation of IQ loss in pre-school children due to lead exposure through locally produced food. Sci. Total Environ. 2012, 414, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Bose, K. Concept of Human Physical Growth and Development; Vidyasagar University: West Bangal, India, 2007. [Google Scholar]
- Havighurst, R.J. Human Development and Education; Longmans Green: New York, NY, USA, 1953. [Google Scholar]
- Walker, S.P.; Wachs, T.D.; Grantham-McGregor, S.; Black, M.M.; Nelson, C.A.; Huffman, S.L. Inequality in early childhood: Risk and protective factors for early child development. Lancet 2011, 378, 1325–1338. [Google Scholar] [CrossRef]
- Poh, B.K.; Rojroonwasinkul, N.; Le Nyugen, B.K.; Budiman, B.; Ng, L.O.; Soonthorndhada, K.; Xuyen, H.T.; Deurenberg, P.; Parikh, P. Relationship between anthropometric indicators and cognitive performance in South-East Asian school-aged children. Br. J. Nutr. 2013, 110, S57–S64. [Google Scholar]
- Singh, G.P.; Nair, M.; Grubesic, R.B.; Connell, F.A. Factors associated with underweight and stunting among children in rural Terai of eastern Nepal. Asia-Pac. J. Public Health 2009, 21, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Sreeramareddy, C.T.; Ramakrishnareddy, N.; Subramaniam, M. Association between household food access insecurity and nutritional status indicators among children aged <5 years in Nepal. Public Health Nutr. 2015, 18, 2906–2914. [Google Scholar] [PubMed]
- Population PDMoHa. In Nepal Demographic and Health Survey 2011; ICF Macro; New ERA: Kathmandu, Nepal, 2011.
- Chandan, S. Enclusive Economic Growth in Nepal. J. Poverty Allev. Int. Dev. 2014, 4, 77–116. [Google Scholar]
- Potter, N.N.; Hotchkiss, J.H. Food Science; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Bhaat, H.B.; Kim, C.S.; Doh, S.G. Non-government organization (NGOs) and the quality of education in Nepal. Asia Study 2015, 18, 1–37. [Google Scholar]
- Nagoda, S.; Eriksen, S. The Role of Local Power Relations in Household Vulnerability to Climate Change in Humla, Nepal; Routledge: London, UK, 2014. [Google Scholar]
- Thapa, M.; Neopane, A.; Singh, U.; Aryal, N.; Agrawal, K.; Shrestha, B. Nutritional status of children in two districts of the mountain region of Nepal. J. Nepal Health Res. Counc. 2014, 11, 235–239. [Google Scholar]
- Gavin’s Woodpile. Online TBCN: Bruce in Nepal—November 2007. In Guy Clarkson; JPGE (Ed.) USC Canada: Ottawa, ON, Canada, 2007.
- Bracken, B.A.; McCallum, R.S. Universal Nonverbal Intelligence Test (UNIT); Riverside Publishing: Itasca, IL, USA, 1998. [Google Scholar]
- Leong, F.T.L. Biennial Review of Counselling Psychology; SAGE Publication: Thousand Oaks, CA, USA, 2008; Volume 2. [Google Scholar]
- Growth Reference 5–19 Years. Available online: http://www.who.int/growthref/who2007_bmi_for_age/en/ (accessed on 18 August 2015).
- Groth-Marnat, G. Handbook of Psychological Assessment; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Nepal Living Standard Survey. Available online: http://cbs.gov.np/nada/index.php/catalog/37 (accessed on 7 August 2015).
- Nepal Health Research Council. National Ethical Guidelines for Health Research in Nepal and Standard Operating Procedures; Ranshahpath: Kathmandu, Nepal, 2011. [Google Scholar]
- Cameron, N. Body mass index cut offs to define thinness in children and adolescents. Br. Med. J. 2007, 335, 166–167. [Google Scholar] [CrossRef] [PubMed]
- Bartels, M.; van Weegen, F.I.; van Beijsterveldt, C.E.; Carlier, M.; Polderman, T.J.; Hoekstra, R.A.; Boomsma, D.I. The five factor model of personality and intelligence: A twin study on the relationship between the two constructs. Personal. Individ. Differ. 2012, 53, 368–373. [Google Scholar] [CrossRef]
- Gilliland, J.A.; Rangel, C.Y.; Healy, M.A.; Tucker, P.; Loebach, J.E.; Hess, P.M.; He, M.; Irwin, J.D.; Wilk, P. Linking childhood obesity to the built environment: A multi-level analysis of home and school neighbourhood factors associated with body mass index. Can. J. Public Health 2012, 103, eS15–eS21. [Google Scholar] [PubMed]
- Must, A.; Dallal, G.E.; Dietz, W.H. Reference data for obesity: 85th and 95th percentiles of body mass index and triceps skinfold thickness. Am. J. Clin. Nutr. 1991, 53, 839–846. [Google Scholar] [PubMed]
- Rosner, B.; Prineas, R.; Loggie, J.; Daniels, S.R. Percentiles for body mass index in US children 5 to 17 years of age. J. Pediatr. 1998, 132, 211–222. [Google Scholar] [CrossRef]
- Rohner, F.; Tschannen, A.B.; Northrop-Clewes, C.; Kouassi-Gohou, V.; Bosso, P.E.; Nicholas Mascie-Taylor, C. Comparison of a possession score and a poverty index in predicting anaemia and undernutrition in pre-school children and women of reproductive age in rural and urban Côte d’Ivoire. Public Health Nutr. 2012, 15, 1620–1629. [Google Scholar] [CrossRef] [PubMed]
- Klebanov, P.K.; Evans, G.W.; Brooks-Gunn, J. Poverty, ethnicity, and risk of obesity among low birth weight infants. J. Appl. Dev. Psychol. 2014, 35, 245–253. [Google Scholar] [CrossRef]
- O’Dea, J.A.; Wilson, R. Socio-cognitive and nutritional factors associated with body mass index in children and adolescents: Possibilities for childhood obesity prevention. Health Educ. Res. 2006, 21, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Lian, C.W.; Muda, W.A.M.W.; Hussin, Z.A.M.; Thon, C.C. Factors associated with undernutrition among children in a rural district of Kelantan, Malaysia. Asia-Pac. J. Public Health 2012, 24, 330–342. [Google Scholar] [CrossRef] [PubMed]
- Herrador, Z.; Sordo, L.; Gadisa, E.; Moreno, J.; Nieto, J.; Benito, A.; Aseffa, A.; Cañavate, C.; Custodio, E. Cross-sectional study of malnutrition and associated factors among school aged children in rural and urban settings of fogera and Libo Kemkem Districts, Ethiopia. PLoS ONE 2014, 9, e105880. [Google Scholar] [CrossRef] [PubMed]
- Owusu, W.; Lartey, A.; Onis, M.D.; Onyango, A.; Frongillo, E. Factors associated with unconstrained growth among affluent Ghanaian children. Acta Paediatr. 2004, 93, 1115–1119. [Google Scholar] [CrossRef] [PubMed]
- Osei, A.; Pandey, P.; Spiro, D.; Nielson, J.; Shrestha, R.; Talukder, Z.; Quinn, V.; Haselow, N. Household food insecurity and nutritional status of children aged 6 to 23 months in Kailali District of Nepal. Food Nutr. Bull. 2010, 31, 483–494. [Google Scholar] [CrossRef]
- Chandola, T.; Deary, I.J.; Blane, D.; Batty, G.D. Childhood IQ in relation to obesity and weight gain in adult life:The National Child Development (1958) Study. Int. J. Obes. 2006, 30, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Marcus Jenkins, J.V.; Woolley, D.P.; Hooper, S.R.; De Bellis, M.D. Direct and indirect effects of brain volume, socioeconomic status and family stress on child IQ. J. Child Adolesc. Behav. 2013, 1, 1–26. [Google Scholar]
- Eriksen, H.-L.F.; Kesmodel, U.S.; Underbjerg, M.; Kilburn, T.R.; Bertrand, J.; Mortensen, E.L. Predictors of intelligence at the age of 5: Family, pregnancy and birth characteristics, postnatal influences, and postnatal growth. PLoS ONE 2013, 8, e79200. [Google Scholar]
- Gale, C.R.; O’Callaghan, F.J.; Godfrey, K.M.; Law, C.M.; Martyn, C.N. Critical periods of brain growth and cognitive function in children. Brain 2004, 127, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.; Greenstein, D.; Lerch, J.; Clasen, L.; Lenroot, R.; Gogtay, N.; Evans, A.; Rapoport, J.; Giedd, J. Intellectual ability and cortical development in children and adolescents. Nature 2006, 440, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.J.; Brooks-Gunn, J. Consequences of Growing up Poor; Russell Sage Foundation: New York, NY, USA, 1995. [Google Scholar]
- Duncan, G.J.; Brooks-Gunn, J.; Klebanov, P.K. Economic deprivation and early childhood development. Child Dev. 1994, 65, 296–318. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Chowdhury, S.D.; Chandra, A.M.; Ghosh, T. Grades of undernutrition and socioeconomic status influence cognitive development in school children of Kolkata. Am. J. Phys. Anthropol. 2015, 156, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Raine, A.; Venables, P.H.; Dalais, C.; Mednick, S.A. Malnutrition at age 3 years and lower cognitive ability at age 11 years: Independence from psychosocial adversity. Arch. Pediatr. Adolesc. Med. 2003, 157, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Rosales, F.J.; Reznick, J.S.; Zeisel, S.H. Understanding the role of nutrition in the brain and behavioral development of toddlers and preschool children: Identifying and addressing methodological barriers. Nutr. Neurosci. 2009, 12, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Ivanovic, D.M.; Rodríguez, M.D.P.N.; Pérez, H.T.; Alvear, J.A.; Almagia, A.F.; Toro, T.D.; Urrutia, M.S.C.; Cruz, A.L.; Ivanovic, R.M. Impact of nutritional status at the onset of elementary school on academic aptitude test achievement at the end of high school in a multicausal approach. Br. J. Nutr. 2009, 102, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Bradley, R.H.; Corwyn, R.F. Socioeconomic status and child development. Annu. Rev. Psychol. 2002, 53, 371–399. [Google Scholar] [CrossRef] [PubMed]
- Tabriz, A.; Sohrabi, M.; Parsay, S.; Abadi, A.; Kiapour, N.; Aliyari, M.; Ahmadi, F.; Roodaki, A. Relation of intelligence quotient and body mass index in preschool children: A community-based cross-sectional study. Nutr. Diabetes 2015, 5, e176. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, S. Intelligence and obesity: Which way does the causal direction go? Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Azurmendi, A.; Braza, F.; Sorozabal, A.; García, A.; Braza, P.; Carreras, M.R.; Muñoz, J.M.; Cardas, J.; Sánchez-Martín, J.R. Cognitive abilities, androgen levels, and body mass index in 5-year-old children. Horm. Behav. 2005, 48, 187–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benito-León, J.; Mitchell, A.; Hernández-Gallego, J.; Bermejo-Pareja, F. Obesity and impaired cognitive functioning in the elderly: A population-based cross-sectional study (NEDICES). Eur. J. Neurol. 2013, 20, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Halkjær, J.; Holst, C.; Sørensen, T.I. Intelligence test score and educational level in relation to BMI changes and obesity. Obes. Res. 2003, 11, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Van Lenthe, F.; Droomers, M.; Schrijvers, C.; Mackenbach, J. Socio-demographic variables and 6 year change in body mass index: Longitudinal results from the GLOBE study. Int. J. Obes. 2000, 24, 1077–1084. [Google Scholar] [CrossRef]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ranabhat, C.; Kim, C.-B.; Park, M.B.; Kim, C.S.; Freidoony, L. Determinants of Body Mass Index and Intelligence Quotient of Elementary School Children in Mountain Area of Nepal: An Explorative Study. Children 2016, 3, 3. https://doi.org/10.3390/children3010003
Ranabhat C, Kim C-B, Park MB, Kim CS, Freidoony L. Determinants of Body Mass Index and Intelligence Quotient of Elementary School Children in Mountain Area of Nepal: An Explorative Study. Children. 2016; 3(1):3. https://doi.org/10.3390/children3010003
Chicago/Turabian StyleRanabhat, Chhabi, Chun-Bae Kim, Myung Bae Park, Chang Soo Kim, and Leila Freidoony. 2016. "Determinants of Body Mass Index and Intelligence Quotient of Elementary School Children in Mountain Area of Nepal: An Explorative Study" Children 3, no. 1: 3. https://doi.org/10.3390/children3010003







