Identification of Predictors for Weight Reduction in Children and Adolescents with Overweight and Obesity (IDA-Insel Survey)
Abstract
:1. Introduction
2. Patients and Methods
- In all patients, physical examinations were performed (t0 and t1).
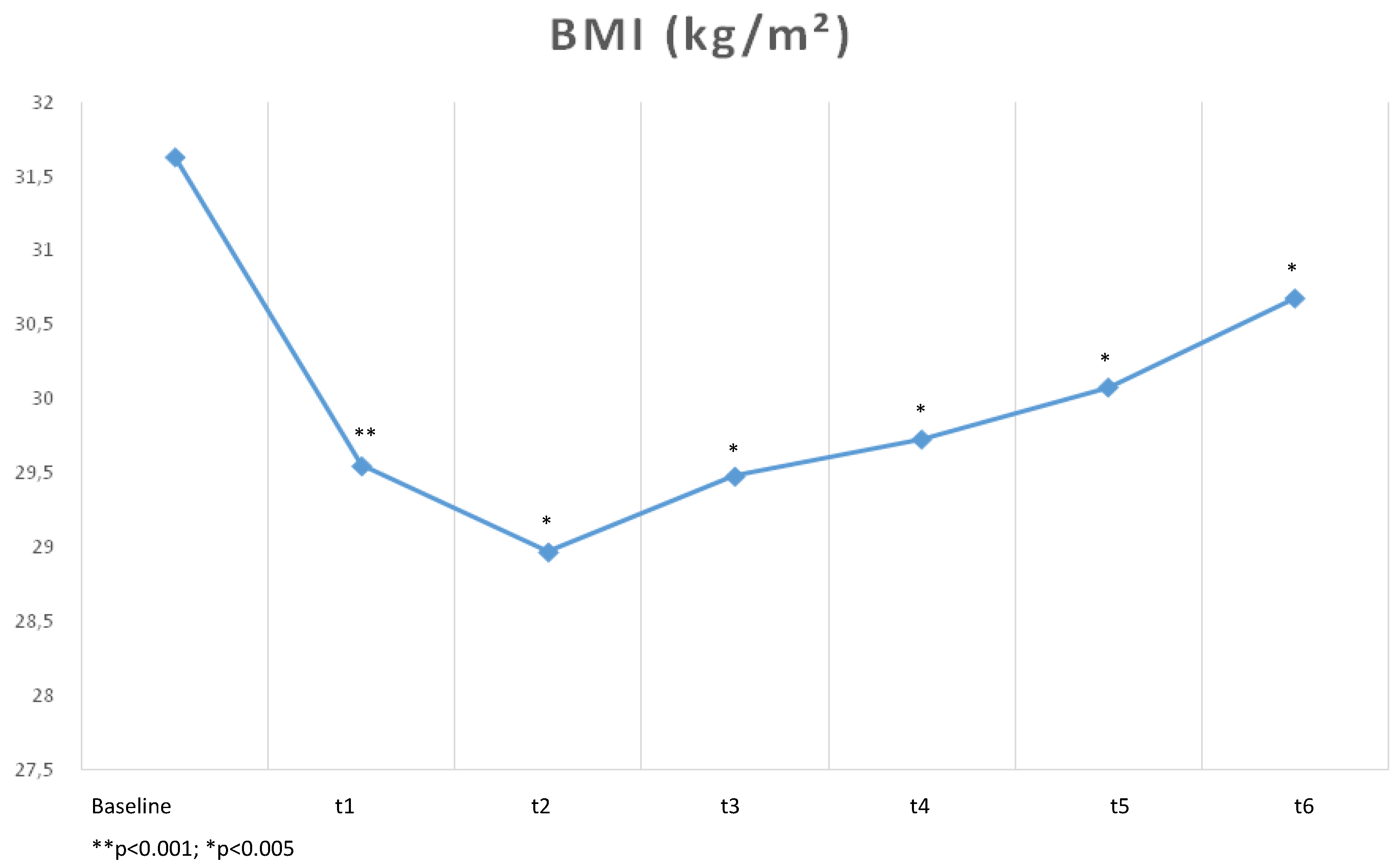
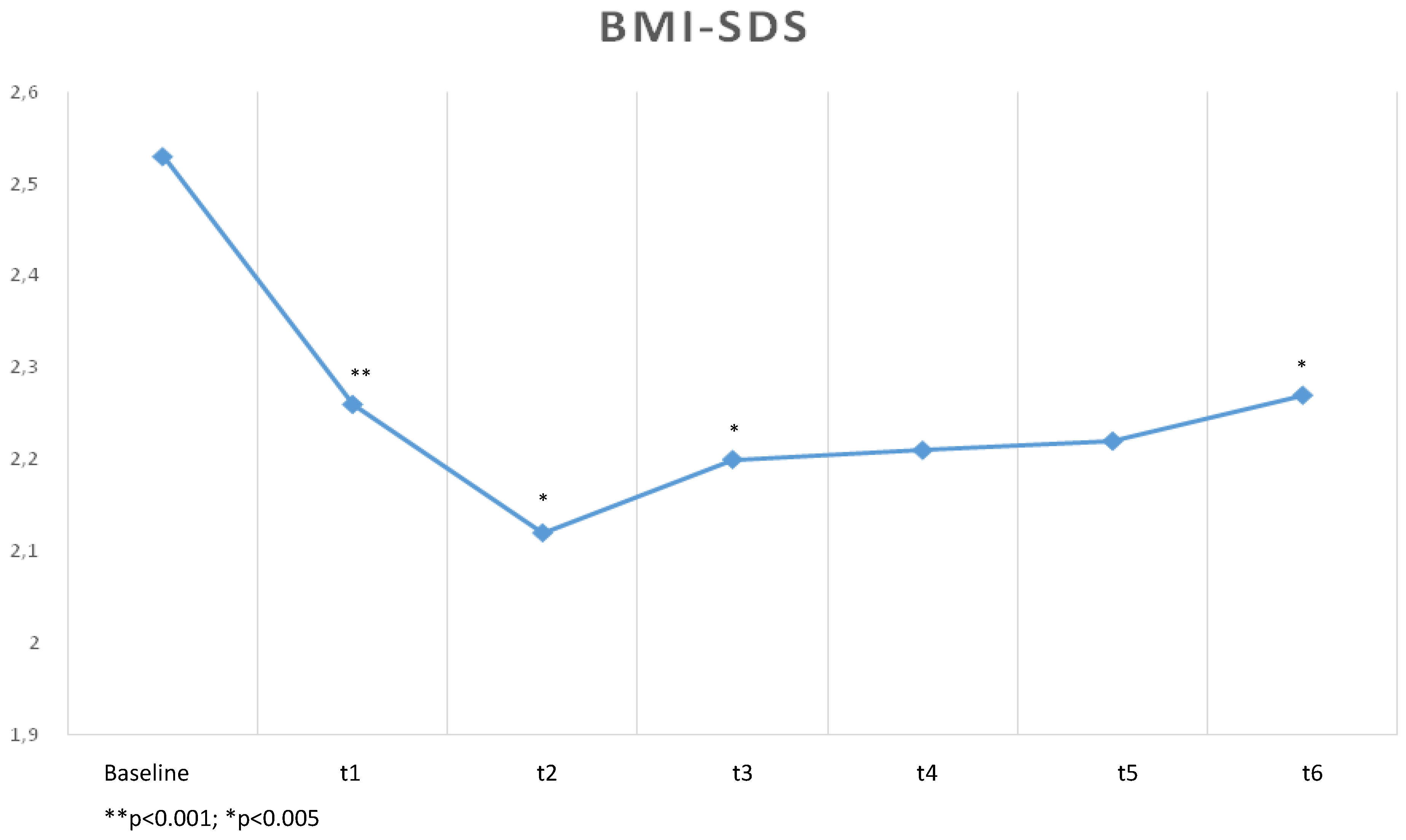
- Measurements of height and weight were assessed with patients wearing light clothing and without shoes. BMI and BMI-SDS were calculated according to the formulae “BMI = kg/m2” and “BMI-SDS = ([BMI/M(t)]L(t) − 1)/(L(t) × S(t))” (M(t), L(t) and S(t) are pre-defined parameters depending on age(t) and sex [20]) (t0, t1, t2, t3, t4, t5, and t6).
- Body composition analyses were done using a Body composition analyzer (BC418MA, TANITA Europe GmbH, Sindelfingen, Germany) (t0 and t1).
- Quantitative B-mode ultrasound (Toshiba, Type SSA-350A “Corevision PRO”, 8 MHz, Linear Sonde Type PLF-805 St, Toshiba Medical Systems, Neuss, Germany) measurement of carotid intima-media thickness (IMT) were done by one physician performing 5 measurements on each side and calculating the mean (t0). Definition of age-adjusted normal values was according to the German standard [22].
- Laboratory parameters (TSH (chemiluminescence-assay), total cholesterol (enzymatically), LDL-cholesterol (enzymatically), triglyzerides (enzymatically), uric acid (enzymatically), C-reactive protein (CRP) (turbidimetry), fasting blood glucose (enzymatically) and glucose values (enzymatically)) following an oral glucose tolerance test (75 g glucose, oGTT [23]) (t0).
- Blood pressure in the sitting position was measured after the patients had rested for 10 min by using a standard sphygmomanometer according to the World Health Organization (WHO) recommendations [24]. In all patients, a 24-h-monitoring was performed (Premo Trend, Zimmer Elektromedizin, Neu-Ulm, Germany) (t0).
- All patients completed standardized questionnaires to assess socio-demographic and socio-economic parameters (family history and status; social status; education; profession of parents; and time spent using a computer, watching TV, and playing sports), eating behavior (kind and amounts of food and liquids in respect of mean main meals), well-being, quality of life (disease-related and weight-related), motivation (intrinsic and extrinsic), intelligence, intrafamilial conflicts (i.e., conflicts with parents and siblings), self-efficacy, resilience, sense of coherence, stress-management, social support and actual body shape (Table 1) (t0, t1, t6).
| Variable | Questionnaire | Cronbach‘s Alpha * |
|---|---|---|
| Well-being | Well-being questionnaire (Berner Fragebogen zum Wohlbefinden (BFW)) [25] | 0.84 |
| Quality of life | Questionnaire for the assessment of disease-related quality of life (Fragebogen zur Erfassung der gesundheitsbezogenen Lebensqualität von Kindern und Jugendlichen (Kindl-R)) [26] | 0.49–0.86 |
| Weight-related quality of life | Questionnaire for the assessment of weight-related quality of life (Gewichtsbezogener Lebensqualitätsfragebogen (GW-LQ-KJ)) [27] | 0.83 |
| Motivation | Questionnaire for the assessment of intrinsic and extrinsic motivation [28] | - |
| Intelligence | Assessment of individual‘s intelligence (Wortschatztest, Zahlenfolgetest aus Grundintelligenztest Skala 2—CFT 20) [29] | - |
| Intrafamilial conflicts | Questionnaire for the assessment of intrafamilial conflicts (Familienklimaskalen (FKS)) [30] | 0.60–0.73 |
| Self-efficacy | Assessment of general self-efficacy (Allgemeine Selbstwirksamkeitserfahrung (SWE)) [31] | 0.82 |
| Resilience | Assessment of resilience (Resilienzskala (RS-11)) [32] | 0.76 |
| Sense of coherence | Children’s sense of coherence scale (CSOC) [33] | 0.64 |
| Stress-management | Questionnaire for the assessment of stress and its management (Fragebogen zur Erhebung von Streßerleben und Streßbewältigung im Kindesalter (SSK)) [34] | 0.77–0.92 |
| Social support | Berliner social support Scale (BSSS) [35] | 0.60–0.87 |
| Actual body shape | Figures of gender-specific body shape | - |
2.1. Ethics Vote
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics (t0)
| Parameter | MW ± SD | Min. | Max. |
|---|---|---|---|
| Number (n) | 143 | - | - |
| Age (years) | 13.9 ± 2.4 | 9.3 | 18.4 |
| Females (%) | 62 | - | - |
| Height (m) | 1.62 ± 0.12 | 1.30 | 1.97 |
| Weight (kg) | 84.1 ± 22.6 | 40.8 | 155.2 |
| BMI (kg/m2) | 31.2 ± 5.4 | 20.3 | 51.4 |
| BMI-SDS | 2.51 ± 0.57 | 0.6 | 4.0 |
| Obesity (%) | 56 | - | - |
| Duration of inhouse treatment (days) | 40.4 ± 4.1 | 28 | 49 |
| Fasting blood-glucose (mmol/L) | 4.17 ± 0.5 | 2.0 | 5.1 |
| oGTT: Blood-glucose 2 h after glucose-loading (mmol/L) | 5.2 ± 0.8 | 3.0 | 6.9 |
| Pathological oGTT (%) | 0 | - | - |
| Total cholesterol (mmol/L) | 4.5 ± 0.9 | 2.6 | 7.4 |
| Total cholesterol ≥ 5.2 mmol/L (%) | 25 | - | - |
| LDL-cholesterol (mmol/L) | 2.8 ± 0.8 | 1.2 | 5.8 |
| LDL-cholesterol ≥ 2.6 mmol/L (%) | 73 | - | - |
| HDL-cholesterol (mmol/L) | 1.6 ± 0.3 | 0.9 | 2.6 |
| HDL-cholesterol < 1.0 mmol/L (%) | 5 | - | - |
| Triglycerides (mmol/L) | 1.1 ± 0.5 | 0.4 | 2.9 |
| Triglycerides ≥ 1.70 mmol/L (%) | 18 | - | - |
| TSH (μIU/mL) | 2.9 ± 1.3 | 0.2 | 7.8 |
| Hypothyreosis (TSH > 4.00 μIU/mL) (%) | 21 | - | - |
| Uric acid (μmol/L) | 359.8 ± 83.3 | 191.0 | 631.0 |
| Hyperuricaemia (≥ 440 μmol/L) (%) | 24 | - | - |
| CRP (mg/dL) | 0.5 * | 0.5 | 4.0 |
| CRP > 0.5 mg/dL (%) | 34 | - | - |
| Systolic blood pressure (mmHg) | 121.7±9.2 | 99 | 150 |
| Systolic blood pressure > 140 mmHg (%) | 4 | - | - |
| Diastolic blood pressure (mmHg) | 68.3 ± 6.5 | 55 | 84 |
| Diastolic blood pressure > 80 mmHg (%) | 2 | - | - |
| 24-h-blood pressure systolic (mmHg) | 119.0 ± 9.4 | 95 | 150 |
| 24-h-blood pressure diastolic (mmHg) | 65.9 ± 6.5 | 51 | 81 |
| Systolic day-/night-difference (mmHg) | 16.1 ± 9.1 | 2 | 35 |
| Diastolic day-/night-difference (mmHg) | 11.5 ± 7.6 | 0 | 24 |
| Parameter | Number (n) | Percentage (%) |
|---|---|---|
| Father | ||
| Educational level | ||
| High | 19 | 13 |
| Medium | 70 | 49 |
| Low | 33 | 23 |
| Unknown | 21 | 15 |
| Body weight | ||
| Normal | 70 | 49 |
| Overweight/obese | 73 | 51 |
| Mother | ||
| Educational level | ||
| High | 19 | 13 |
| Medium | 90 | 63 |
| Low | 26 | 18 |
| Unknown | 8 | 6 |
| Body weight | ||
| Normal | 43 | 30 |
| Overweight/obese | 100 | 70 |
| Parameter | Baseline (t0) | At the End of Inpatient Treatment (t1) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| MW ± SD | Min. | Max. | MW ± SD | Min. | Max. | ||
| Weight (kg) | 84.1 ± 22.6 | 41 | 155 | 78.7 ± 20.5 | 38 | 144 | <0.01 |
| BMI (kg/m2) | 31.2 ± 5.4 | 20 | 51,4 | 29.3 ± 4.9 | 19 | 47 | <0.01 |
| BMI-SDS | 2.51 ± 0.57 | 0.6 | 4,0 | 2.25 ± 0.57 | 0.13 | 3.8 | <0.01 |
| Body composition | |||||||
| Percentage of body fat (%) | 38.6 ± 6.5 | 24 | 53 | 35.2 ± 6.6 | 19.4 | 50.8 | <0.01 |
| Fat mass (kg) | 34.2 ± 12.6 | 12 | 82 | 29.2 ± 10.3 | 10.3 | 61.2 | <0.01 |
| Fat-free mass (kg) | 52.4 ± 12.9 | 29 | 90 | 51.8 ± 13.2 | 25.6 | 89.3 | <0.01 |
3.2. Socio-Psychological Parameters
| Parameter | Correlation Coefficient (r) | p-Value |
|---|---|---|
| Reduction of BMI-SDS 6 months after inpatient treatment (t3) | 0.25 | 0.018 |
| Reduction of BMI-SDS 9 months after inpatient treatment (t4) | 0.39 | <0.001 |
| Reduction of BMI-SDS 12 months after inpatient treatment (t5) | 0.52 | <0.001 |
| Breakfast—low caloric intake at baseline (t0) | −0.23 | 0.036 |
| Breakfast—medium caloric intake at baseline (t0) | −0.24 | 0.025 |
| Lunch–low caloric intake at baseline (t0) | −0.29 | 0.007 |
| Lunch–medium caloric intake at baseline (t0) | −0.23 | 0.030 |
| Dinner–low caloric intake at baseline (t0) | −0.26 | 0.017 |
| Dinner–medium caloric intake at baseline (t0) | −0.23 | 0.035 |
| Low daily caloric intake at baseline (t0) | −0.26 | 0.013 |
| Medium daily caloric intake at baseline (t0) | −0.32 | 0.003 |
| Structured daily schedule at baseline (t0) | 0.26 | 0.015 |
| Time spending with computer/TV per day at baseline (t0) | −0.27 | 0.028 |
| Resilience at baseline (t0) | 0.24 | 0.024 |
| Parameter | β | T | p-Value |
|---|---|---|---|
| Daily caloric intake (t0) | 0.24 | 2.72 | 0.008 |
| Intrafamilial conflicts (t6) | 0.32 | 2.59 | 0.012 |
| Well-being (t6) | −0.54 | −4.70 | <0.001 |
| Resilience (t0) | 0.43 | 3.67 | <0.001 |
| BMI at the end of inpatient treatment (t1) | 0.25 | 2.88 | 0.005 |
| Caloric intake at breakfast (t0) | 0.25 | 2.86 | 0.006 |
| Stress management (t6) | 0.24 | 2.60 | 0.011 |
| Duration of overweight/obesity (t0) | 0.19 | 2.25 | 0.027 |
| Mother‘s profession (t0) * | 0.18 | 2.07 | 0.043 |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000; p. 894. [Google Scholar]
- Müller, S.D. Ernährung für übergewichtige Kinder und Jugendliche; Grin Verlag: München, Germany, 2013. (In German) [Google Scholar]
- Daniels, S.R. Complications ob obesity in children and adolesecents. Int. J. Obes. 2009, 33, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Juonala, M.; Magnussen, C.G.; Berenson, G.S.; Venn, A.; Burns, T.L.; Sabin, M.A.; Srinivasan, S.R.; Daniels, S.R.; Davis, P.H.; Chen, W.; et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N. Engl. J. Med. 2011, 355, 1876–1885. [Google Scholar] [CrossRef] [PubMed]
- Vander Wal, J.S.; Mitchell, E.R. Psychological complications of pediatric obesity. Pediatr. Clin. N. Am. 2011, 58, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Moran, M.; Salazar-Vazques, B.; Violante, R.; Guerrero-Romero, F. Metabolic syndrome among children and adolescents aged 10–18 years. Diabetes Care 2004, 313, 779–784. [Google Scholar] [CrossRef] [Green Version]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J.; et al. Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Carroll, M.D.; Ogden, C.L.; Johnson, C.L. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002, 288, 1723–1727. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.M.; Li, L.; Chinn, S.; Rona, R.J. Trends in growth in England and Scotland, 1972 to 1994. Arch. Dis. Child 1997, 76, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Schiel, R.; Beltschikow, W.; Kramer, G.; Stein, G. Overweight, obesity and elevated pressure in children and adolescents. Eur. J. Med. Res. 2006, 11, 97–101. [Google Scholar] [PubMed]
- Pierce, J.W.; Wardle, J. Cause and effect beliefs and self-esteem of overweight children. J. Child Psychol. Psychiatry 1997, 38, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P. Psychologische Aspekte der Adipositas. Bundesgesundh. Gesundh. Gesundh. 2011, 54, 562–569. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Redegeld, M.; Bullinger, M. Quality of life after in-patient rehabilitation in children with obesity. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 63–65. [Google Scholar] [CrossRef] [PubMed]
- Schwimmer, J.B.; Burwinkle, T.M.; Varni, J.W. Health-related quality of life of severely obese children and adolescents. JAMA 2003, 289, 1813–1818. [Google Scholar] [CrossRef] [PubMed]
- Metcalf, H.; Henley, W.; Wilkin, T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes. BMJ 2012. [Google Scholar] [CrossRef] [PubMed]
- Wieland, L.S.; Falzon, L.; Sciamanna, C.N.; Trudeau, K.J.; Schwartz, J.E.; Davidson, K.W. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Schiel, R.; Beltschikow, W.; Radón, S.; Kramer, G.; Schmiedel, R.; Berndt, R.D.; Stein, G. Long-term treatment of obese children and adolescents using a telemedicine support programme. J. Telemed. Telecare 2008, 14, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Martin, P.D.; White, M.A.; Newton, R.; Walden, H.; York-Crowe, E.; Alfonso, A.S.; Ryan, D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat. Weight Disord. 2005, 10, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Hoffmeister, U.; Molz, E.; Bullinger, M.; van Egmond-Fröhlich, A.; Goldopp, C.; Mann, R.; Ravens-Sieberer, U.; Reinehr, T.; Westenöfer, J.; Wille, N.; et al. Evaluation von Therapienangeboten für adipöse Kinder und Jugendliche (EvAKuJ-Projekt). Bundesgesundh. Gesundh. Gesundh. 2011, 54, 603–610. (In German) [Google Scholar] [CrossRef] [PubMed]
- Arbeitsgemeinschaft Adipositas im Kindes- und Jugendalter [AGA]. Leitlinien. Verabschiedung auf der Konsensuskonferenz der AGA am 04.10.2012. 2012. Available online: http://www.adipositas-gesellschaft.de/fileadmin/PDF/Leitlinien/AGA_S2_Leitlinie.pdf (accessed on 11 August 2014).
- Schiel, R.; Radón, S.; Beltschikow, W. Telemedizinisches Therapiekonzept bei Stoffwechselerkrankungen (Übergewicht und Adipositas) bei Kindern und Jugendlichen (TeleAdi); MEDIGREIF Inselklinik Heringsdorf GmbH: Ostseebad Heringsdorf, Germany, 2006. (In German) [Google Scholar]
- Buck, M. Die Intima-Media-Thickness (IMT) der Arteria carotis communis bei gesunden Kindern und Jugendlichen—Sonographische Methodik, Anwendbarkeit und Referenzwerte. Dissertation, Technische Universität, Müchen, Germany, 2013. Available online: https://mediatum.ub.tum.de/doc/1093329/1093329.pdf (accessed on 14 November 2014). [Google Scholar]
- American Diabetes Association. The expert committee on the diagnosis and classification of diabetes mellitus: Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 1997, 22, 1183–1197. [Google Scholar]
- Subcommittee, G. 1999 World Health Organization—International society of hypertension guidelines for the management of hypertension. J. Hypertens. 1999, 17, 151–183. [Google Scholar]
- Grob, A.; Lüthi, R.; Kaiser, F.G.; Flammer, A.; Mackinnon, A.; Wearing, A.J. Berner Fragebogen zum Wohlbefinden Jugendlicher. Diagnostica 1991, 37, 66–75. (In German) [Google Scholar]
- Ravens-Sieberer, U. Der Kindl-R Fragebogen zur Erfassung der gesundheitsbezogenen Lebensqualität bei Kindern und Jugendlichen—Revidierte Form. In Diagnostische Verfahren zu Lebensqualität und Wohlbefinden; Schumacher, J., Klaiberg, A., Brähler, E., Eds.; Hogrefe Verlag: Göttingen, Geramny, 2003; pp. 184–188. (In German) [Google Scholar]
- Warschburger, P.; Fromme, C.; Petermann, F. Gewichtsbezogene Lebensqualität bei Schulkindern: Validität des GW-LQ-KJ. Z. Gesundheitspsychol. 2004, 12, 159–166. (In German) [Google Scholar] [CrossRef]
- Zimbardo, P.G.; Gerrig, R.J. Psychologie; Springer-Verlag: Berlin, Germany, 1999. [Google Scholar]
- Weiß, R.H. Grundintelligenztest Skala 2 (CFT 20); Hogrefe Verlag: Göttingen, Germany, 1998. (In German) [Google Scholar]
- Roth, M. Entwicklung und Überprüfung einer Kurzform der Familienklimaskalen für Jugendliche. Z. Differ. Diagn. Psychol. 2002, 23, 225–234. (In German) [Google Scholar] [CrossRef]
- Jerusalem, M.; Schwarzer, R. Skala zur Allgemeinen Selbstwirksamkeitserwartung. In Diagnostische Verfahren in der Psychotherapie; Brähler, E., Schumacher, J., Strauß, B., Eds.; Hogrefe Verlag: Göttingen, Germany, 2002. (In German) [Google Scholar]
- Leppert, K. RS—Resilienzskala. In Diagnostische Verfahren in der Psychotherapie; Brähler, E., Schumacher, J., Strauß, B., Eds.; Hogrefe-Verlag: Göttingen, Germany, 2002. (In German) [Google Scholar]
- Kern, R.; Rasky, E.; Noack, R.H. Indikatoren für Gesundheitsförderung in der Volksschule. Forschungsbericht 95/1; Karl-Franzens-Universität: Graz, Austria, 1995. (In German) [Google Scholar]
- Lohaus, A.; Fleer, B.; Freytag, P.; Klein-Hessling, J. Fragebogen zur Erhebung von Streßerleben und Streßbewältigung im Kindesalter (SSK); Hogrefe-Verlag: Göttingen, Germany, 1996. (In German) [Google Scholar]
- Schwarzer, R.; Schulz, U. Berlin Social Support Scales (BSSS). Available online: http://userpage.fu-berlin.de/~health/bsss.htm (accessed on 13 March 2015).
- GmbH, S. Nettoeinkommen und verfügbares Nettoeinkommen privater Haushalte in Deutschland nach sozialer Stellung in Euro. Available online: http://de.statista.com/themen/293/durchschnittseinkommen/ (accessed on 14 November 2014). (In German)
- Riis, J.; Grason, H.; Strobino, D.; Ahmed, S.; Minkovitz, C. State school policies and youth, obesity. Matern. Child Health J. 2012, 16, S111–S118. [Google Scholar] [CrossRef] [PubMed]
- Conrad, D.; Capwell, S. Associations between deprivation and rates of childhood overweight and obesity in England, 2007–2010: An ecological study. BMJ 2012. [Google Scholar] [CrossRef] [PubMed]
- Gettys, F.K.; Jackson, J.B.; Frick, S.L. Obesity in pediatric orthopaedics. Orthop. Clin. N. Am. 2012, 42, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar] [PubMed]
- Singh, G.H.; Kogan, M.D.; van Dyck, P.C. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch. Pediatr. Adolesc. Med. 2010, 164, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Schiel, R.; Beltschikow, W.; Radon, S.; Kramer, G.; Perenthaler, T.; Stein, G. Increased carotid intima-media thickness and associations with cardiovascular risk factors in obese and overweight children and adolescents. Eur. J. Med. Res. 2007, 12, 503–508. [Google Scholar] [PubMed]
- Meyer, A.A.; Kundt, G.; Steiner, M.; Schuff-Werner, P.; Kienast, W. Impaired flow-mediated vasodilatation, carotid artery intima-media thickening, and elevated endothelial plasma markers in obese children: The impact of cardiovascular factors. Pediatrics 2006, 117, 1560–1567. [Google Scholar] [CrossRef] [PubMed]
- Iannuzzi, A.; Licenziati, M.R.; Acampora, C.; Salvatore, V.; Auriemma, L.; Romano, M.; Panico, S.; Rubba, P.; Trevisan, M. Increased carotid intima-media thickness and stiffness in obese children. Diabetes Care 2004, 27, 2506–2508. [Google Scholar] [CrossRef] [PubMed]
- Kapiotis, S.; Holzer, G.; Schaller, G.; Haumer, M.; Widhalm, H.; Weghuber, D.; Jilma, B.; Roggla, G.; Wolzt, M.; Widhalm, K.; et al. A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 2541–2546. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Kiess, W.; de Sousa, G.; Stoffel-Wagner, B.; Wunsch, R. Intima media thickness in childhood obesity: Relations to inflammatory markers, glucose metabolism, and blood pressure. Metabolism 2006, 55, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Van Egmond-Fröhlich, A.; Brauer, W.; Goldschmidt, H.; Hoff-Emden, H.; Oepen, J.; Zimmermann, E. Effects of a programme for structured outpatient follow-up care after inpatient rehabilitation of obese children and adolescents. A multicentre, randomized study. Rehabilitation 2006, 45, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Böhler, T.; Bengel, J.; Goldapp, C.; Mann, R.; Bullinger, M.; Egmond-Fröhlich, A.; Hoffmeister, U.; Holl, R.; Reinehr, T.; Westenhöfer, J.; et al. Bericht zur EvAKuJ-Studie im Rahmen des Qualitätssicherungsprozesses der BZgA zur Prävention und Therapie von Übergewicht bei Kindern und Jugendlichen; Bundeszentrale für gesundheitliche Aufklärung: Köln, Germany, 2012. (In German) [Google Scholar]
- Kurth, B.M.; Schaffrath-Rosario, A. Übergewicht und Adipositas bei Kindern und Jugendlichen in Deutschland. Bundesgesundh. Gesundh. Gesundh. 2010, 53, 643–652. (In German) [Google Scholar] [CrossRef] [PubMed]
- Benecke, A.; Vogel, H. Übergewicht und Adipositas. Gesundheitsberichtserstattung des Bundes; Robert Koch-Institut: Berlin, Germany, 2005; p. 16. (In German) [Google Scholar]
- Tugade, M.M.; Fredrickson, B.L.; Barrett, L.F. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J. Pers. 2004, 72, 1161–1190. [Google Scholar] [CrossRef] [PubMed]
- Friborg, O.; Barlang, D.; Martinussen, M.; Rosenvinge, J.H.; Odin, H. Resilience in relation to personality and intelligence. Int. J. Methods Psychiatr. Res. 2005, 14, 19–42. [Google Scholar] [CrossRef]
- Dowrick, C.; Kokanovic, R.; Hegarty, K.; Griffiths, F.; Gunn, J. Resilience and depression: Perspectives from primary care. Health 2008, 12, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.P.; Vitaliano, P.P.; Smith, R.E.; Yi, J.C.; Weinger, K. The role of resilience on psychological adjustment and physical health in patients with diabetes. Br. J. Health Psychol. 2008, 13, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Crawford, D. Socio-economic factors in obesity: A case of slim chance in a fat world? Asia Pac. J. Clin. Nutr. 2006, 15, 15–20. [Google Scholar] [PubMed]
- Bundeszentrale für Gesundheitliche Aufklärung. Erkennen-Bewerten-Handeln: Zur Gesundheit von Kindern und Jugendlichen in Deutschland; Robert Koch-Institut: Berlin, Germany, 2008. (In German) [Google Scholar]
- Ravens-Sieberer, U.; Wille, N.; Erhart, M.; Bettge, S.; Wittchen, H.; Rothenberger, A.; Herpertz-Dahlmann, B.; Resch, F.; Hölling, H.; Bullinger, M.; et al. BELLA study group: Prevalence of mental health problems among children and adolescents in Germany: Results of the BELLA study within the National Health Interview and Examination Survey. Eur. Child Adolesc. Psychiatr. 2008, 17, S22–S33. [Google Scholar] [CrossRef] [PubMed]
- George, C.; Herman, K.; Ostrander, R. The family environment and developmental psychopathology: The unique and interactive effects of depression, attention, and conduct problems. Child Psychiatr. Hum. Dev. 2006, 37, 163–177. [Google Scholar] [CrossRef] [PubMed]
- Bengel, J.; Meinders-Lückering, F.; Rottmann, N. Gesundheitliche Schutzfaktoren bei Kindern und Jugendlichen. Stand der Forschung zu psychosozialen Schutzfaktoren für Gesundheit, Forschung und Praxis der Gesundheitsförderung; Bundeszentrale für gesundheitliche Aufklärung: Köln, Germany, 2009; p. 35. (In German) [Google Scholar]
- Cox, M.J.; Brooks-Gunn, J. The advances in family research series. In Conflict and Cohesion in Families: Causes and Consequences; Guildford Press: Oxford, UK, 1998. [Google Scholar]
- AOK-Bundesverband. AOK-Familienstudie 2014. Forschungsbericht des SINUS-Instituts, 2014. Available online: http://www.aok-bv.de/imperia/md/aokbv/presse/pressemitteilungen/archiv/2014/aok_familienstudie_2014_gesamtbericht_band_1.pdf (accessed on 11 August 2014).
- Nicklas, T.A.; Morales, M.; Linares, A.; Yang, S.J.; Baranowski, T.; Se Moor, C.; Berenson, G. Children’s meal patterns have changed over a 21-year period: The Bogalusa Heart Study. J. Am. Diet. Assoc. 2004, 1004, 753–761. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiel, R.; Kaps, A.; Stein, G.; Steveling, A. Identification of Predictors for Weight Reduction in Children and Adolescents with Overweight and Obesity (IDA-Insel Survey). Healthcare 2016, 4, 5. https://doi.org/10.3390/healthcare4010005
Schiel R, Kaps A, Stein G, Steveling A. Identification of Predictors for Weight Reduction in Children and Adolescents with Overweight and Obesity (IDA-Insel Survey). Healthcare. 2016; 4(1):5. https://doi.org/10.3390/healthcare4010005
Chicago/Turabian StyleSchiel, Ralf, Alexander Kaps, Günter Stein, and Antje Steveling. 2016. "Identification of Predictors for Weight Reduction in Children and Adolescents with Overweight and Obesity (IDA-Insel Survey)" Healthcare 4, no. 1: 5. https://doi.org/10.3390/healthcare4010005
APA StyleSchiel, R., Kaps, A., Stein, G., & Steveling, A. (2016). Identification of Predictors for Weight Reduction in Children and Adolescents with Overweight and Obesity (IDA-Insel Survey). Healthcare, 4(1), 5. https://doi.org/10.3390/healthcare4010005





