Implementation of Competency-Based Pharmacy Education (CBPE)
Abstract
:1. Introduction
If you want to grow a worthwhile plant: a rose, a fruit tree, a vine of paan, then you need effort.You must water, apply manure, weed it, prune it.It is not simple.So it is with the world.Vikram Seth: A suitable boy
2. Competency-Based Pharmacy Education
3. Terminology and Definitions
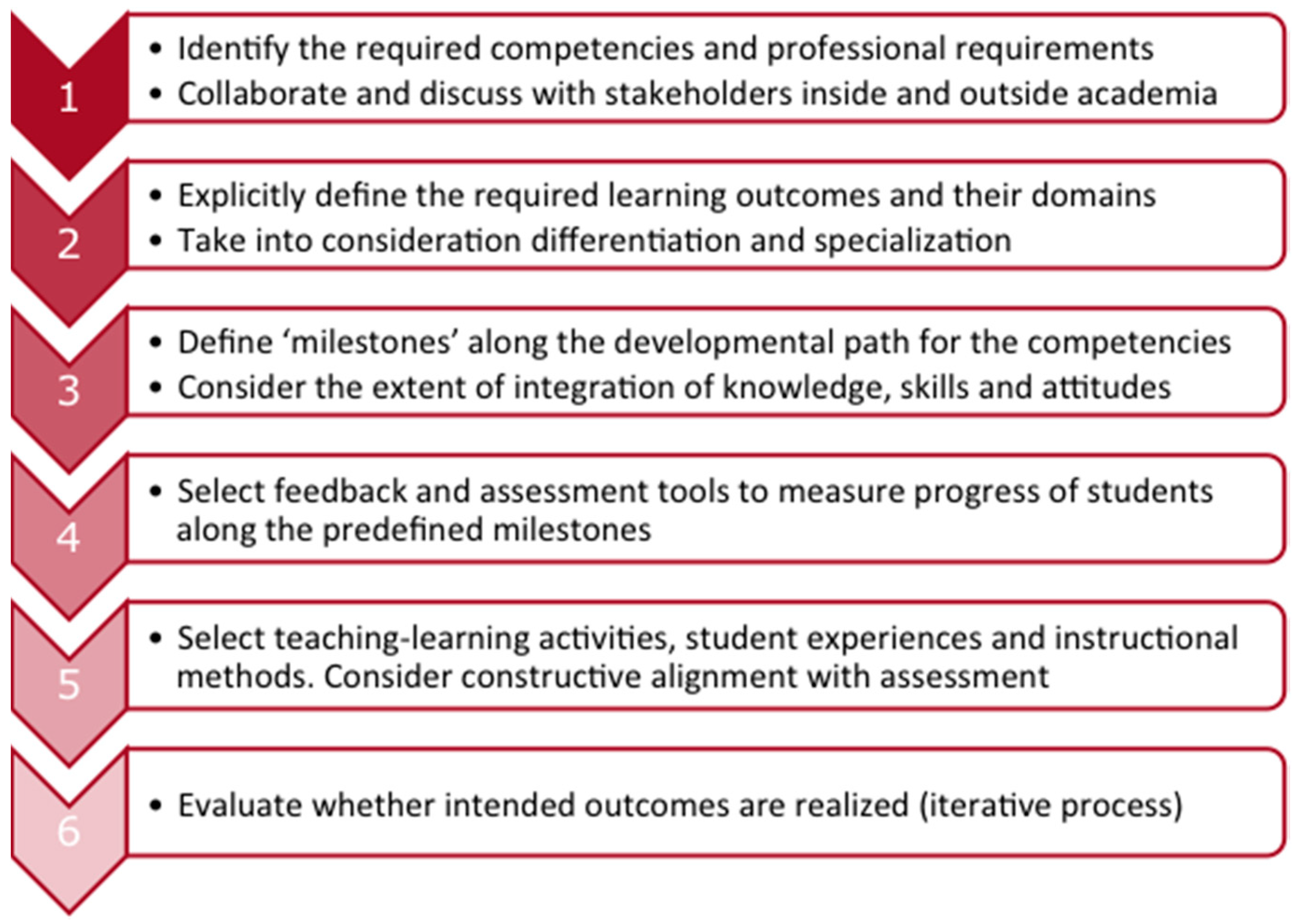
4. Curriculum Design Process
- Tip 1: Use a competency framework. Several competency frameworks are available (see Appendix A). All can be used as a starting point for curriculum development but interpretation and fine-tuning to the local situation is necessary.
- Tip 2: Consult all your stakeholders. In designing a new curriculum consultation of the outside world is necessary to align the competences of recent graduates to the local professional and healthcare needs.
- Tip 3: Think forward (scenarios). Curriculum changes are usually implemented gradually, starting from the first year of the program. This means, that your newly-educated graduates will enter practice at least five years from now!
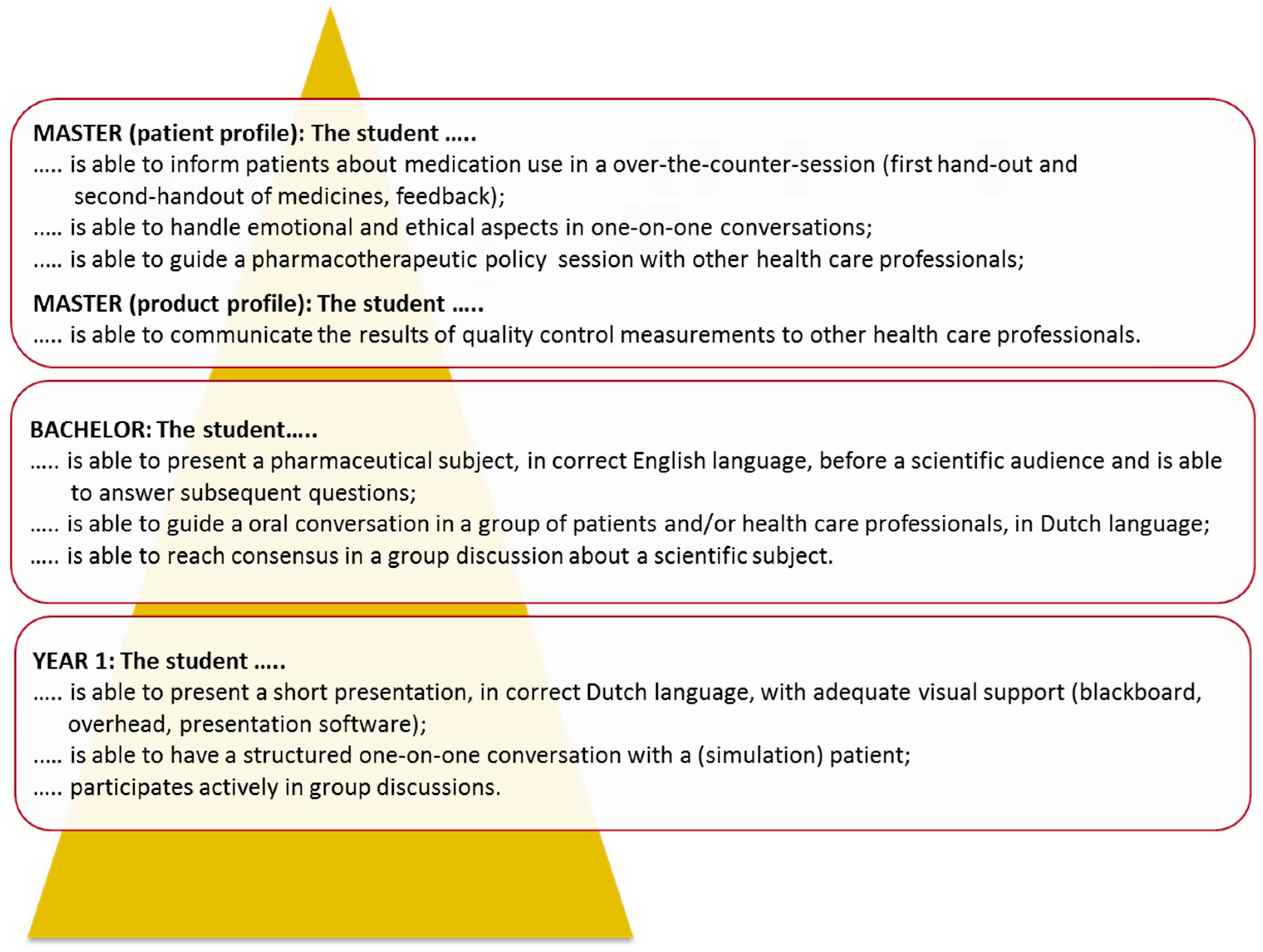
5. Curriculum Construction
- Tip 4: Integrate content and skills as far as possible. Skills can initially be trained in isolation, but must be integrated with course content as the curriculum advances. Professional activities usually require that knowledge, cognitive skills, and non-cognitive skills are used in an integrated way.
- Tip 5: Appoint curriculum coordinators. CBPE requires that the longitudinal development of knowledge and skills progresses gradually from relatively simple and isolated to more complex and integrated. This requires monitoring and readjustment of the curriculum structure by skills consultants and/or stream coordinators.
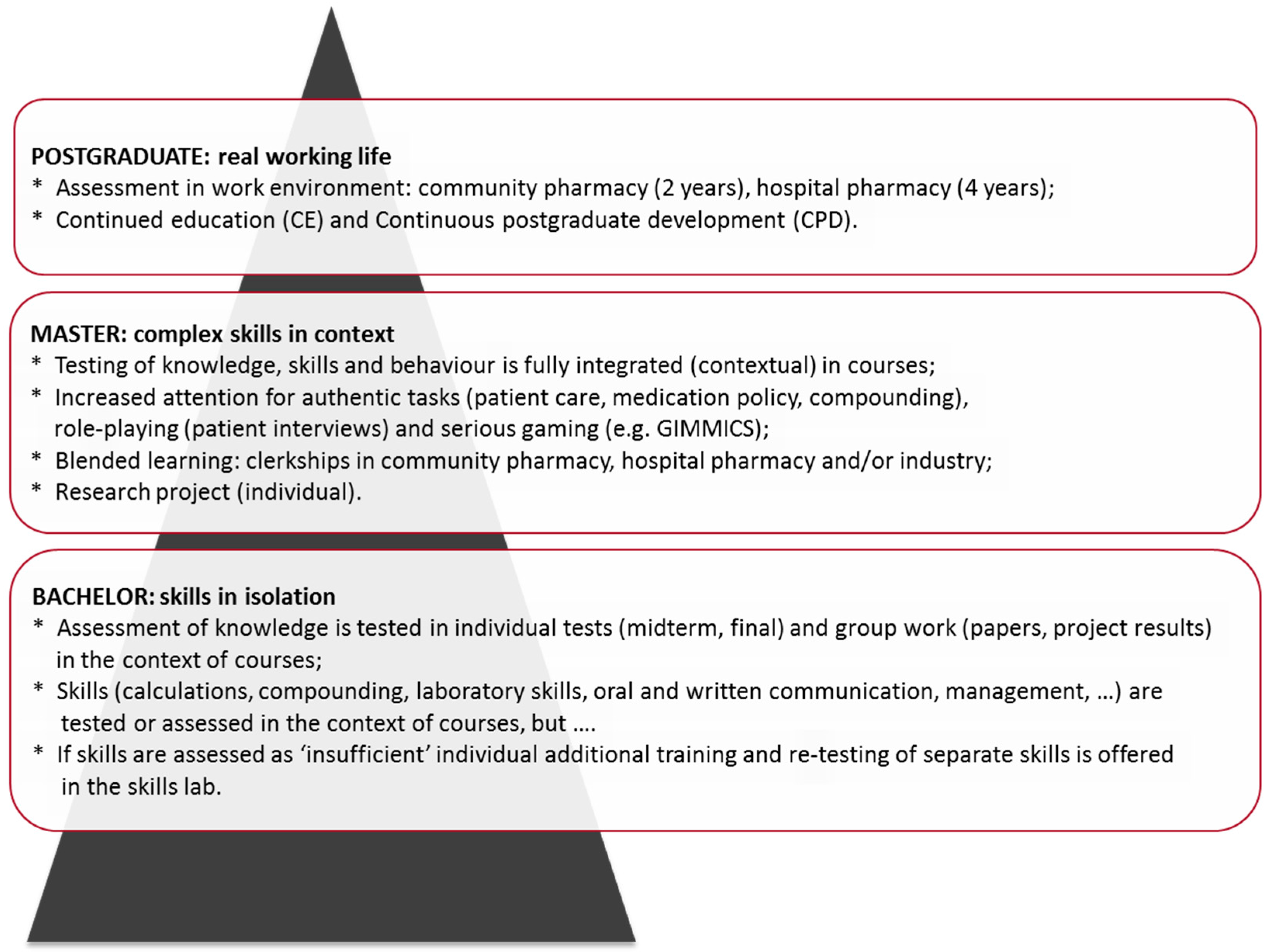
6. Student Assessment
- Tip 6: Less is more, in particular for summative assessment. A pharmacy curriculum is easily overburdened; this can lead to burnout of students and teachers. Restrict contact hours and high-stakes examinations to a well-chosen minimum; concentrate on non-summative feedback.
- Tip 7: Use authentic assessment tasks. Authentic learning activities and assessment tasks (cases, OSCE), simulations (serious gaming) and the use of entrustable professional activities (EPAs) can motivate students and can prepare them for their professional life.
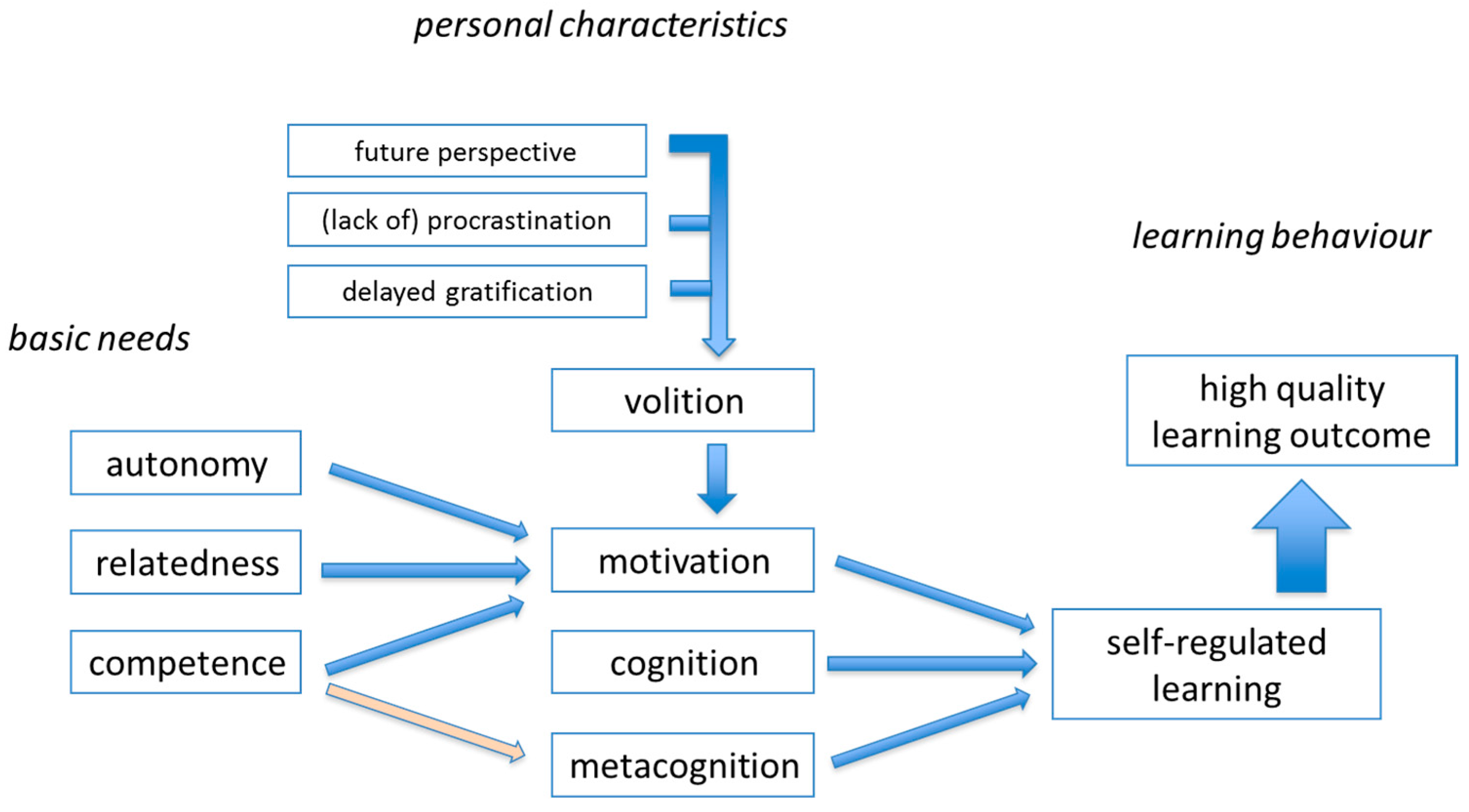
7. Effective Learning and Constructive Alignment
- Tip 8: Adopt frameworks for cognitive and skills development. An explicit, evidence-based, educational model can guide choices for assessments, learning tasks, and can protect against counterproductive measures.
- Tip 9: Use curriculum mapping for internal quality enhancement. Mapping the various curricular elements (course, etc.) against existing frameworks can be very helpful in identifying curricular gaps, overlaps, and discontinuities.
8. Management and Quality Enhancement
- Tip 10: Assure management continuity. Development and optimization of CBPE requires a long-term perspective and continuity in the educational development. This is best achieved by appointing a director of education and/or by forming a curriculum management team.
- Tip 11: Develop educational expertise and specialization. A competency-based curriculum requires teachers to develop expertise in the fields of autonomy-supportive teaching and competency assessment.
- Tip 12: Develop scholarship of teaching and learning (SoTL). Building a competence-based curriculum requires the development and testing of non-standard teaching-learning activities and novel assessment formats. Teachers and curriculum developers can benefit from a scholarly approach, using educational literature, exchange of good practices and training or coaching in (inter)national networks.
9. Summary and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A. Competency- or Outcome-Based Frameworks
References
- Girot, E.A. Assessment of Competence in Clinical Practice—A Review of the Literature. Nurse Educ. Today 1993, 13, 83–90. [Google Scholar] [CrossRef]
- Spielman, A.I.; Fulmer, T.; Eisenberg, E.S.; Alfano, M.C. Dentistry, Nursing, and Medicine: A Comparison of Core Competencies. J. Dent. Educ. 2005, 69, 1257–1271. [Google Scholar] [PubMed]
- Frank, J.R.; Snell, L.S.; Cate, O.T.; Holmboe, E.S.; Carraccio, C.; Swing, S.R.; Harris, P.; Glasgow, N.J.; Campbell, C.; Dath, D.; et al. Competency-Based Medical Education: Theory to Practice. Med. Teach. 2010, 32, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Bruno, A.; Bates, I.; Brock, T.; Anderson, C. Towards a Global Competency Framework. Am. J. Pharm. Educ. 2010, 74, 56. [Google Scholar] [CrossRef] [PubMed]
- Nash, R.E.; Chalmers, L.; Brown, N.; Jackson, S.; Peterson, G. An International Review of the use of Competency Standards in Undergraduate Pharmacy Education. Pharm. Educ. 2015, 15, 131–141. [Google Scholar]
- Hepler, C.D. Clinical Pharmacy, Pharmaceutical Care, and the Quality of Drug Therapy. Pharmacotherapy 2004, 24, 1491–1498. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.M.; Moore, D.E.; Stead, W.W.; Balser, J.R. Beyond Flexner: A New Model for Continuous Learning in the Health Professions. Acad. Med. 2010, 85, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Van Mil, J.W.F.; Schulz, M.; Tromp, T.F.J. Pharmaceutical Care, European Developments in Concepts, Implementation, Teaching, and Research: A Review. Pharm. World Sci. 2004, 26, 303–311. [Google Scholar] [PubMed]
- Atkinson, J.; De Paepe, K.; Sanchez Pozo, A.; Rekkas, D.; Volmer, D.; Hirvonen, J.; Bozic, B.; Skowron, A.; Mirciou, C.; Marcincal, A.; et al. The Second Round of the Phar-QA Survey of Competences for Pharmacy Practice. Pharmacy 2016, 4, 27. [Google Scholar] [CrossRef]
- Medina, M.S.; Plaza, C.M.; Stowe, C.D.; Robinson, E.T.; DeLander, G.; Beck, D.E.; Melchert, R.B.; Supernaw, R.B.; Roche, V.F.; Gleason, B.L.; et al. Center for the Advancement of Pharmacy Education 2013 Educational Outcomes. Am. J. Pharm. Educ. 2013, 77, 162. [Google Scholar] [CrossRef] [PubMed]
- Pearson, M.L.; Hubball, H.T. Curricular Integration in Pharmacy Education. Am. J. Pharm. Educ. 2012, 76, 204. [Google Scholar] [CrossRef] [PubMed]
- Meijerman, I.; Nab, J.; Koster, A.S. Designing and Implementing an Inquiry-Based Undergraduate Curriculum in Pharmaceutical Sciences. Curr. Pharm. Teach. Learn. 2016, 8, 905–919. [Google Scholar] [CrossRef]
- Koster, A.S.; Meijerman, I.; Blom, L.T.G.; Schalekamp, T. Pharmacy Education at Utrecht University: An Educational Continuum. Dosis Sci. J. Pharm. 2009, 25, 85–93. [Google Scholar]
- Gibbs, G.; Knapper, C.; Piccinin, S. Disciplinary and Contextually Appropriate Approaches to Leadership of Teaching in Research-Intensive Academic Departments in Higher Education. High. Educ. Q. 2008, 62, 416–436. [Google Scholar] [CrossRef]
- Stupans, I.; McAllister, S.; Clifford, R.; Hughes, J.; Krass, I.; March, G.; Owen, S.; Woulfe, J. Nationwide Collaborative Development of Learning Outcomes and Exemplar Standards for Australian Pharmacy Programmes. Int. J. Pharm. Pract. 2015, 23, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.E. The Assessment of Clinical Skills/Competence/Performance. Acad. Med. 1990, 65, S63–S67. [Google Scholar] [CrossRef] [PubMed]
- Stupans, I.; Atkinson, J.; Mestrovic, A.; Nash, R.; Rouse, M.J. A Shared Focus: Comparing the Australian, Canadian, United Kingdom and United States Pharmacy Learning Outcome Frameworks and the Global Competency Framework. Pharmacy 2016, 4, 26. [Google Scholar] [CrossRef]
- Ried, L.D.; Doty, R.E.; Nemire, R.E. A Psychometric Evaluation of an Advanced Pharmacy Practice Experience Clinical Competency Framework. Am. J. Pharm. Educ. 2015, 79, 19. [Google Scholar] [CrossRef] [PubMed]
- Ramia, E.; Salameh, P.; Btaiche, I.F.; Saad, A.H. Mapping and Assessment of Personal and Professional Development Skills in a Pharmacy Curriculum. BMC Med. Educ. 2016, 16, 533. [Google Scholar] [CrossRef] [PubMed]
- Midlöv, P.; Höglund, P.; Eriksson, T.; Diehl, A.; Edgren, G. Developing a Competency-Based Curriculum in Basic and Clinical Pharmacology—A Delphi Study among Physicians. Basic Clin. Pharm. Toxicol. 2015, 117, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Silva, H.; Stonier, P.; Buhler, F.; Deslypere, J.-P.; Criscuolo, D.; Nell, G.; Massud, J.; Geary, S.; Schenk, J.; Kerpel-Fronius, S.; et al. Core Competencies for Pharmaceutical Physicians and Drug Development Scientists. Front. Pharm. 2013, 4, 105. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.E.; Welcher, C.M.; Holmboe, E.S.; Kirk, L.M.; Norcini, J.J.; Simons, K.B.; Skochelak, S.E. Implementation of Competency-Based Medical Education: Are We Addressing the Concerns and Challenges? Med. Educ. 2015, 49, 1086–1102. [Google Scholar] [CrossRef] [PubMed]
- Ten Cate, O.; Scheele, F. Viewpoint: Competency-Based Postgraduate Training: Can We Bridge the Gap between Theory and Clinical Practice? Acad. Med. 2007, 82, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; van den Broek, W.E.S.; Ten Cate, O. The Case for use of Entrustable Professional Activities in Undergraduate Medical Education. Acad. Med. 2015, 90, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Pittenger, A.L.; Chapman, S.A.; Frail, C.K.; Moon, J.Y.; Undeberg, M.R.; Orzoff, J.H. Entrustable Professional Activities for Pharmacy Practice. Am. J. Pharm. Educ. 2016, 80, 57. [Google Scholar] [CrossRef] [PubMed]
- Buurma, H.J. Advanced Community Pharmacist Education Programme; Royal Dutch Pharmacists Association: The Hague, The Netherlands, 2012. [Google Scholar]
- Biggs, J.; Tang, C. Teaching for Quality Learning at University, 4th ed.; SRHE and Open University Press, McGraw-Hill: Maidenhead, UK, 2011. [Google Scholar]
- Harden, R.M. Learning Outcomes as a Tool to Assess Progression. Med. Teach. 2007, 29, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Al-Eraky, M.M. Curriculum Navigator: Aspiring Towards a Comprehensive Package for Curriculum Planning. Med. Teach. 2012, 34, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Farris, K.B.; Demb, A.; Janke, K.K.; Kelley, K.; Scott, S.A. Assessment to Transform Competency-Based Curricula. Am. J. Pharm. Educ. 2009, 73, 158. [Google Scholar] [CrossRef] [PubMed]
- Katajavuori, N.; Hakkarainen, K.; Kuosa, T.; Airaksinen, M.; Hirvonen, J.; Holm, Y. Curriculum Reform in Finnish Pharmacy Education. Am. J. Pharm. Educ. 2009, 73, 151. [Google Scholar] [CrossRef] [PubMed]
- Boyce, E.G.; Lawson, L.A. Preprofessional Curriculum in Preparation for Doctor of Pharmacy Educational Programs. Am. J. Pharm. Educ. 2009, 73, 155. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.S.; Kember, D.; Lau, C.B.S.; Au Yeung, M.Y.M.; Leung, D.Y.P.; Chow, M.S.S. An Outcomes-Based Approach to Curriculum Development in Pharmacy. Am. J. Pharm. Educ. 2009, 73, 14. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Allison, S.D.; McCollum, M.; Luckey, S.W.; Clark, D.R.; Paulsen, S.M.; Malhotra, J.; Brunner, L.J. The Regis Model for Pharmacy Education: A Highly Integrated Curriculum Delivered by Team-Based Learning™ (TBL). Curr. Pharm. Teach. Learn. 2013, 5, 555–563. [Google Scholar] [CrossRef]
- Poloyac, S.M.; Empey, K.M.; Rohan, L.C.; Skledar, S.J.; Empey, P.E.; Nolin, T.D.; Bies, R.R.; Gibbs, R.B.; Folan, M.; Kroboth, P.D. Core Competencies for Research Training in the Clinical Pharmaceutical Sciences. Am. J. Pharm. Educ. 2011, 75, 27. [Google Scholar] [CrossRef] [PubMed]
- Newble, D.; Stark, P.; Bax, N.; Lawson, M. Developing an Outcome-Focused Core Curriculum. Med. Educ. 2005, 39, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Mak-Van Der Vossen, M.; Peerdeman, S.; Kleinveld, J.; Kusurkar, R. How We Designed and Implemented Teaching, Training, and Assessment of Professional Behaviour at VUmc School of Medical Sciences Amsterdam. Med. Teach. 2013, 35, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Mulder, H.; Cate, O.T.; Daalder, R.; Berkvens, J. Building a Competency-Based Workplace Curriculum around Entrustable Professional Activities: The Case of Physician Assistant Training. Med. Teach. 2010, 32, e453–e459. [Google Scholar] [CrossRef] [PubMed]
- Husband, A.K.; Todd, A.; Fulton, J. Integrating Science and Practice in Pharmacy Curricula. Am. J. Pharm. Educ. 2014, 78, 63. [Google Scholar] [CrossRef] [PubMed]
- Van der Werf, J.J.; Dekens-Konter, J.; Brouwers, J.R.B.J. A New Model for Teaching Pharmaceutical Care Services Management. Pharm. Educ. 2004, 4, 165–169. [Google Scholar] [CrossRef]
- Conway, S.E.; Medina, M.S.; Letassy, N.A.; Britton, M.L. Assessment of Streams of Knowledge, Skill, and Attitude Development across the Doctor of Pharmacy Curriculum. Am. J. Pharm. Educ. 2011, 75, 83. [Google Scholar] [CrossRef] [PubMed]
- Malone, D.T.; Short, J.L.; Naidu, S.; White, P.J.; Kirkpatrick, C.M. Mapping of the Australian Qualifications Framework Standards Onto an Undergraduate Bachelor of Pharmacy Course. Pharm. Educ. 2015, 15, 261–269. [Google Scholar]
- Van Der Vleuten, C.P.M.; Schuwirth, L.W.T.; Driessen, E.W.; Dijkstra, J.; Tigelaar, D.; Baartman, L.K.J.; van Tartwijk, J. A Model for Programmatic Assessment Fit for Purpose. Med. Teach. 2012, 34, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Nicol, D.; MacFarlane-Dick, D. Formative Assessment and Selfregulated Learning: A Model and Seven Principles of Good Feedback Practice. Stud. High. Educ. 2006, 31, 199–218. [Google Scholar] [CrossRef]
- Schuwirth, L.W.T.; Van der Vleuten, C.P.M. Programmatic Assessment: From Assessment of Learning to Assessment for Learning. Med. Teach. 2011, 33, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Stupans, I.; March, G.; Owen, S.M. Enhancing Learning in Clinical Placements: Reflective Practice, Self-Assessment, Rubrics and Scaffolding. Assess. Eval. High. Educ. 2013, 38, 507–519. [Google Scholar] [CrossRef]
- Allen, S.; Waterfield, J.; Rivers, P. An Investigation of Pharmacy Student Perception of Competence-Based Learning using the Individual Skills Evaluation and Development Program, iSED®. Pharm. Educ. 2016, 16, 72–80. [Google Scholar]
- Branch, C. An Assessment of Students’ Performance and Satisfaction with an OSCE Early in an Undergraduate Pharmacy Curriculum. Curr. Pharm. Teach. Learn. 2014, 6, 22–31. [Google Scholar] [CrossRef]
- Ten Cate, O.; Snell, L.; Mann, K.; Vermunt, J. Orienting Teaching toward the Learning Process. Acad. Med. 2004, 79, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, P. Maximizing Learning through Course Alignment and Experience with Different Types of Knowledge. Innov. High. Educ. 2009, 34, 93–103. [Google Scholar] [CrossRef]
- Kaartinen-Koutaniemi, M.; Katajavuori, N. Enhancing the Development of Pharmacy Education by Changing Pharmacy Teaching. Pharm. Educ. 2006, 6, 197–208. [Google Scholar] [CrossRef]
- Ten Cate, T.J.; Kusurkar, R.A.; Williams, G.C. How Self-Determination Theory can Assist our Understanding of the Teaching and Learning Processes in Medical Education. AMEE Guide No. 59. Med. Teach. 2011, 33, 961–973. [Google Scholar] [PubMed]
- Niemiec, C.P.; Ryan, R.M. Autonomy, Competence, and Relatedness in the Classroom: Applying Self-Determination Theory to Educational Practice. Theor. Res. Educ. 2009, 7, 133–144. [Google Scholar] [CrossRef]
- Remington, T.L.; Hershock, C.; Klein, K.C.; Niemer, R.K.; Bleske, B.E. Lessons from the Trenches: Implementing Team-Based Learning Across several Courses. Curr. Pharm. Teach. Learn. 2015, 7, 121–130. [Google Scholar] [CrossRef]
- Plaza, C.M.; Draugalis, J.R.; Slack, M.K.; Skrepnek, G.H.; Sauer, K.A. Curriculum Mapping in Program Assessment and Evaluation. Am. J. Pharm. Educ. 2007, 71, 20. [Google Scholar] [CrossRef] [PubMed]
- Zelenitsky, S.; Vercaigne, L.; Davies, N.M.; Davis, C.; Renaud, R.; Kristjanson, C. Using Curriculum Mapping to Engage Faculty Members in the Analysis of a Pharmacy Program. Am. J. Pharm. Educ. 2014, 78, 139. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, M.A.F.; Pugh, C.B. Assessment of Curricular Competency Outcomes. Am. J. Pharm. Educ. 2001, 65, 217–224. [Google Scholar]
- Kleijnen, J.; Dolmans, D.; Willems, J.; van Hout, H. Effective Quality Management Requires a Systematic Approach and a Flexible Organisational Culture: A Qualitative Study among Academic Staff. Q. High Educ. 2014, 20, 103–126. [Google Scholar] [CrossRef]
- Andurkar, S.; Fjortoft, N.; Sincak, C.; Todd, T. Development of a Center for Teaching Excellence. Am. J. Pharm. Educ. 2010, 74, 123. [Google Scholar] [CrossRef] [PubMed]
- Al-Eraky, M.M.; Donkers, J.; Wajid, G.; Van Merrienboer, J.J.G. Faculty Development for Learning and Teaching of Medical Professionalism. Med. Teach. 2015, 37, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Tofade, T.; Abate, M.; Fu, Y. Perceptions of a Continuing Professional Development Portfolio Model to Enhance the Scholarship of Teaching and Learning. J. Pharm. Pract. 2014, 27, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Grunefeld, H.; van Tartwijk, J.; Jongen, H.; Wubbels, T. Design and Effects of an Academic Development Programme on Leadership for Educational Change. Int. J. Acad. Dev. 2015, 20, 306–318. [Google Scholar] [CrossRef]
- Vos, S.S.; Trewet, C.B. A Comprehensive Approach to Preceptor Development. Am. J. Pharm. Educ. 2012, 76, 47. [Google Scholar] [CrossRef] [PubMed]
- Mårtensson, K.; Roxå, T.; Olsson, T. Developing a Quality Culture through the Scholarship of Teaching and Learning. High. Educ. Res. Dev. 2011, 30, 51–62. [Google Scholar] [CrossRef]
- Medina, M.; Hammer, D.; Rose, R.; Scott, S.; Creekmore, F.M.; Pittenger, A.; Soltis, R.; Bouldin, A.; Schwarz, L.; Piascik, P. Demonstrating Excellence in Pharmacy Teaching through Scholarship. Curr. Pharm. Teach. Learn. 2011, 3, 255–259. [Google Scholar] [CrossRef]
- Dolmans, D.H.J.M.; Tigelaar, D. Building Bridges between Theory and Practice in Medical Education using a Design-Based Research Approach: AMEE Guide No. 60. Med. Teach. 2012, 34, 1–10. [Google Scholar] [CrossRef] [PubMed]

| Curriculum | Description | Reference |
|---|---|---|
| B.Sc. | Content and generic skills for a pre-professional curriculum (nationwide, USA) | [32] |
| B.Pharm. | Design of an outcomes-based Pharmacy curriculum (Hong-Kong, China) | [33] |
| B.Pharm.Sc. | Undergraduate honours programme for the training of pharmaceutical researchers (Utrecht, the Netherlands) | [12] |
| Pharm.D. | An integrated professional pharmacy curriculum (Denver, USA) | [34] |
| B.Sc. + M.Sc. | Design of a complete bachelor and master programme (Helsinki, Finland) | [31] |
| Ph.D. | Research training for clinical pharmaceutical sciences: assessments and rubrics (Pittsburgh, USA) | [35] |
| M.D. | Content and skills for the core curriculum of a medical school (Sheffield, United Kingdom) | [36] |
| M.D. | Teaching, training, and assessment of professional behaviour in medicine (Amsterdam, The Netherlands ) | [37] |
| Physician assistants | Teaching, training and assessment for physician assistants (Utrecht, The Netherlands) | [38] |
| 1 | The curriculum is designed as a coherent program. |
| 2 | The program stimulates active study behaviour, is challenging and varied. |
| 3 | Acquisition, application and integration of knowledge and skills take place in a context relevant for the future profession. |
| 4 | Within the program systematic and explicit attention is paid to the development of academic and personal skills and values. |
| 5 | Direction of the learning process is gradually shifted from teacher to student. |
| 6 | The program enables students to follow individual interests by offering elective courses and a patient- or product-oriented profile. |
| 7 | A well-balanced system of mentoring and assessment is used, which takes into account the steering effects of testing. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koster, A.; Schalekamp, T.; Meijerman, I. Implementation of Competency-Based Pharmacy Education (CBPE). Pharmacy 2017, 5, 10. https://doi.org/10.3390/pharmacy5010010
Koster A, Schalekamp T, Meijerman I. Implementation of Competency-Based Pharmacy Education (CBPE). Pharmacy. 2017; 5(1):10. https://doi.org/10.3390/pharmacy5010010
Chicago/Turabian StyleKoster, Andries, Tom Schalekamp, and Irma Meijerman. 2017. "Implementation of Competency-Based Pharmacy Education (CBPE)" Pharmacy 5, no. 1: 10. https://doi.org/10.3390/pharmacy5010010







