Insights into the Chemical Biology of Childhood Embryonal Solid Tumors by NMR-Based Metabolomics
Abstract
:1. Introduction
2. Embryonal Solid Tumors
2.1. Neuroblastoma (NB)
2.2. Nephroblastoma or Wilms Tumor (WT)
2.3. Hepatoblastoma (HB)
2.4. Retinoblastoma (RB)
2.5. Central Nervous System (CNS) Tumors
2.5.1. Medulloblastoma (MB)
2.5.2. Astrocytoma (ACs)
2.5.3. Ependymoma (ED)
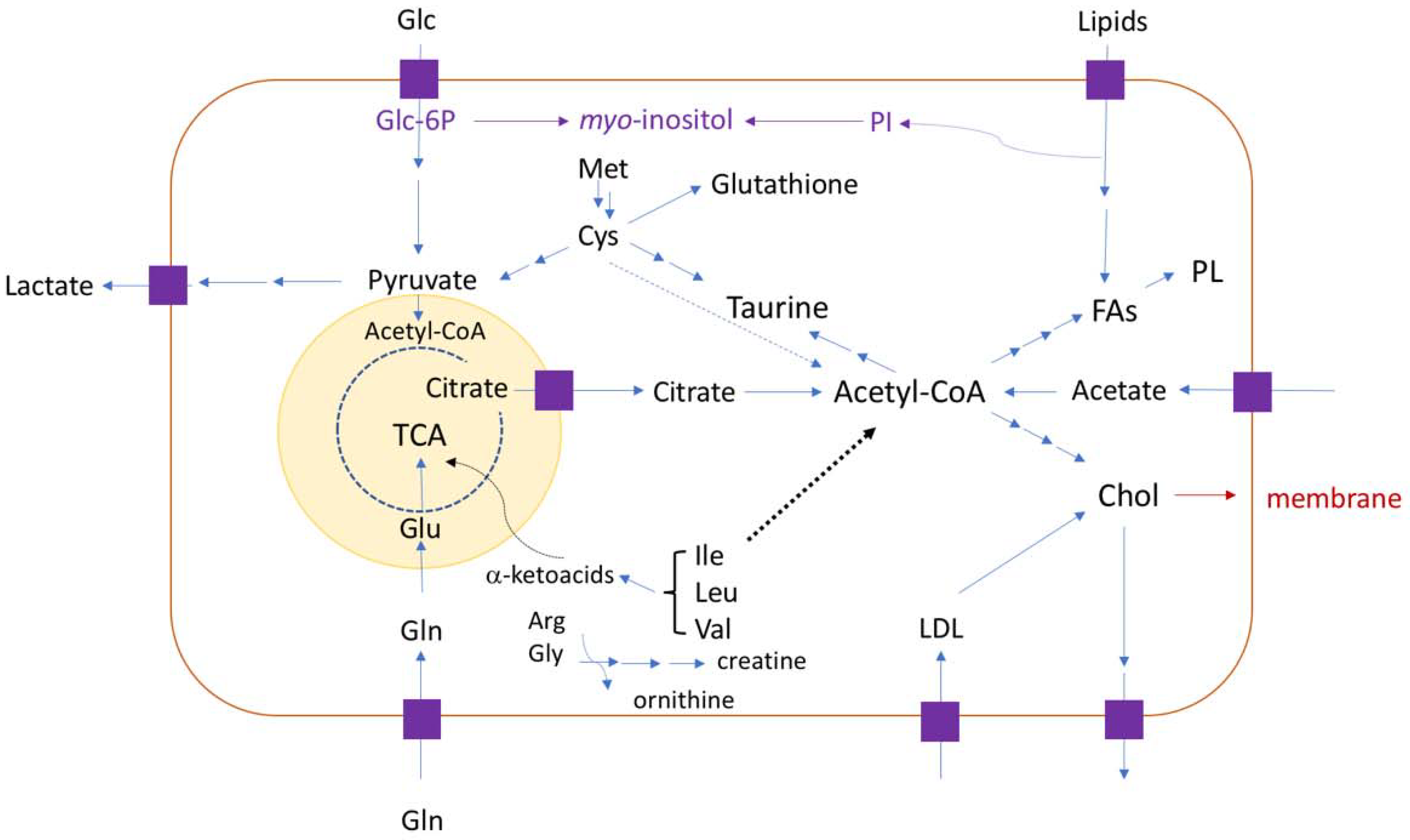
3. Metabolomics on Embryonal Solid Tumors
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Trivedi, D.K.; Hollywood, K.A. Metabolomics for the masses: The future of metabolomics in a personalized world. New Horiz. Transl. Med. 2017, 3, 294–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanos, V.; Van den Anker, J.; Noto, A.; Mussap, M.; Atzori, L. Metabolomics in neonatology: Fact or fiction? Semin. Fetal Neonatal. Med. 2013, 18, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Hanna, M.H.; Brophy, P.D. Metabolomics in pediatric nephrology: Emerging concepts. Pediatr. Nephrol. 2015, 30, 881–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramsden, J.J. Bioinformatics: An Introduction, 2nd ed.; Springer: London, UK, 2009; pp. 239–244. ISBN 978-1-84800-256-2. [Google Scholar]
- Čuperlović-Culf, M. NMR Metabolomics in Cancer Research, 1st ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 1–14. ISBN 978-1-907568-84-8. [Google Scholar]
- Moco, S.; Collino, S.; Rezzi, S.; Martin, F.P. Metabolomics perspectives in pediatric research. Pediatr. Res. 2013, 73, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Shulaev, V. Metabolomics technology and bioinformatics. Brief Bioinform. 2006, 7, 128–139. [Google Scholar] [CrossRef]
- Griffin, J.L.; Shockcor, J.P. Metabolic profiles of cancer cells. Nat. Rev. Cancer 2004, 4, 551–561. [Google Scholar] [CrossRef]
- Beger, R.D. A review of applications of metabolomics in cancer. Metabolites 2013, 3, 552–574. [Google Scholar] [CrossRef] [Green Version]
- Gowda, G.A.; Zhang, S.; Gu, H.; Asiago, V.; Shanaiah, N.; Raftery, D. Metabolomics-based methods for early disease diagnostics: A review. Expert Rev. Mol. Diagn. 2008, 8, 617–633. [Google Scholar] [CrossRef] [Green Version]
- Fuss, T.L.; Cheng, L.L. Evaluation of cancer metabolomics using ex vivo High Resolution Magic Angle Spinning (HRMAS) Magnetic Resonance Spectroscopy (MRS). Metabolites 2016, 6, 11. [Google Scholar] [CrossRef] [Green Version]
- Moestue, S.A.; Sitter, B.; Bathen, T.; Tessem, M.; Gribbestad, I.S. HR MAS MR spectroscopy in metabolic characterization in cancer. Curr. Top Med. Chem. 2011, 11, 2–26. [Google Scholar] [CrossRef]
- Spiga, L.; Atzori, L.; Noto, A.; Moretti, C.; Mussap, M.; Masile, A.; Lussu, M.; Fanos, V. Metabolomics in pediatric oncology: A potential still to be exploited. J. Matern. Fetal Neonatal. Med. 2013, 26, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Piotto, M.; Saudek, V.; Sklenar, V. Gradient-tailored excitation for single-quantum NMR spectroscopy of aqueous solutions. J. Biomol. NMR 1992, 2, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.D.; Meng, X.; Donovan, K.J.; Shaka, A.J. SOGGY: Solvent-optimized double gradient spectroscopy for water suppression. A comparison with some existing techniques. J. Magn. Reson. 2007, 184, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Larive, C.K.; Barding, G.A.; Dinges, M.M. NMR spectroscopy for metabolomics and metabolic profiling. Anal. Chem. 2015, 87, 133–146. [Google Scholar] [CrossRef]
- Parsons, S.K.; Skapek, S.X.; Neufeld, E.J.; Kuhlman, C.; Young, M.L.; Donnelly, M.; Brunzell, J.D.; Otvos, J.D.; Sallan, S.E.; Rifai, N. Asparaginase-associated lipid abnormalities in children with acute lymphoblastic leukemia. Blood 1997, 89, 1886–1895. [Google Scholar] [CrossRef] [Green Version]
- Tiziani, S.; Kang, Y.; Harjanto, R.; Axelrod, J.; Piermarocchi, C.; Roberts, W.; Paternostro, G. Metabolomics of the tumor microenvironment in pediatric acute lymphoblastic leukemia. PLoS ONE 2013, 8, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Bennett, C.D.; Kohe, S.E.; Gill, S.K.; Davies, N.P.; Wilson, M.; Storer, L.C.D.; Ritzmann, T.; Paine, S.M.L.; Scott, I.S.; Nicklaus-Wollenteit, I.; et al. Tissue metabolite profiles for the characterisation of pediatric cerebellar tumours. Sci. Rep. 2018, 8, 1–10. [Google Scholar] [CrossRef]
- Sutton, L.N.; Wehrli, S.L.; Gennarelli, L.; Wang, Z.; Zimmerman, R.; Bonner, K.; Rorke, L.B. High-resolution 1H-magnetic resonance spectroscopy of pediatric posterior fossa tumors in vitro. J. Neurosurg. 1994, 81, 443–448. [Google Scholar] [CrossRef]
- Tzika, A.A.; Cheng, L.L.; Goumnerova, L.; Madsen, J.R.; Zurakowski, D.; Astrakas, L.G.; Zarifi, M.K.; Scott, R.M.; Anthony, D.C.; Gonzalez, R.G.; et al. Biochemical characterization of pediatric brain tumors by using in vivo and ex vivo magnetic resonance spectroscopy. J. Neurosurg. 2002, 96, 1–11. [Google Scholar] [CrossRef]
- Wilson, M.; Davies, N.P.; Brundler, M.; Mcconville, C.; Grundy, R.G.; Peet, A.C. High resolution magic angle spinning 1H NMR of childhood brain and nervous system tumours. Mol. Cancer 2009, 8, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Cuellar-Baena, S.; Morales, J.; Martinetto, H.; Calvar, J.; Sevlever, G.; Castellano, G.; Cerdá-Nicolás, M.; Celda, B.; Monleon, D. Comparative metabolic profiling of paediatric ependymoma, medulloblastoma and pilocytic astrocytoma. Int. J. Mol. Med. 2010, 26, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Davies, N.; Wilson, M.; Harris, L.M.; Natarajan, K.; Lateef, S.; MacPherson, L.; Sgouros, S.; Grundy, R.G.; Arvanitis, T.N.; Peet, A.C. Identification and characterisation of childhood cerebellar tumours by in vivo proton MRS. NMR Biomed. 2008, 21, 908–918. [Google Scholar] [CrossRef] [PubMed]
- Baykal, A.T.; Jain, M.R.; Li, H. Aberrant regulation of choline metabolism by mitochondrial electron transport system inhibition in neuroblastoma cells. Metabolomics 2008, 4, 347–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imperiale, A.; Elbayed, K.; Moussallieh, F.M.; Neuville, A.; Piotto, M.; Bellocq, J.P.; Lutz, P.; Namer, I.J. Metabolomic pattern of childhood neuroblastoma obtained by 1H-High-Resolution Magic Angle Spinning (HRMAS) NMR Spectroscopy. Pediatr. Blood Cancer 2011, 56, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Duarte, I.F.; Lamego, I.; Marques, J.; Marques, M.P.M.; Blaise, B.J.; Gil, A.M. Nuclear magnetic resonance (NMR) study of the effect of cisplatin on the metabolic profile of MG-63 osteosarcoma cells. J. Proteome Res. 2010, 9, 5877–5886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen-Rhoades, W.; Whittle, S.B.; Rainusso, N. Pediatric solid tumors of infancy: An overview. Pediatr. Rev. 2018, 39, 57. [Google Scholar] [CrossRef]
- de Paula Silva, N.; de Souza Reis, R.; Garcia Cunha, R.; Pinto Oliveira, J.F.; de Oliveira Santos, M.; Pombo-de-Oliveira, M.S.; de Camargo, B. Maternal and birth characteristics and childhood embryonal solid tumors: A population-based report from Brazil. PLoS ONE 2016, 11, e0164398. [Google Scholar] [CrossRef]
- Corbett, R. Childhood solid tumours occurring in adolescents and young adults. Cancer Forum. 2009, 33, 13–17. [Google Scholar]
- Scotting, P.J.; Walker, D.A.; Perilongo, G. Childhood solid tumours: A developmental disorder. Nat. Rev. Cancer 2005, 5, 481–488. [Google Scholar] [CrossRef]
- Singal, A.K.; Agarwala, S. Tumour markers in pediatric solid tumours. J. Indian Assoc. Pediatr. Surg. 2005, 10, 183–190. [Google Scholar] [CrossRef]
- Hauser, P. Malignant solid tumors. Med. Ped. Oncol. 2003, 41, 590–591. [Google Scholar] [CrossRef] [PubMed]
- Stewart, E.; Federico, S.; Karlstrom, A.; Shelat, A.; Sablauer, A.; Pappo, A.; Dyer, M.A. The Childhood Solid Tumor Network: A new resource for the developmental biology and oncology research communities. Dev. Biol. 2016, 411, 287–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandoval, J.A.; Malkas, L.H.; Hickey, R.J. Clinical significance of serum biomarkers in pediatric solid mediastinal and abdominal tumors. Int. J. Mol. Sci. 2012, 13, 1126–1153. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.; Heney, D.; Jones, D.R.; Sutton, A.J.; Lambert, P.C.; Abrams, K.R.; Young, B.; Wailoo, A.J.; Burchill, S.A. A systematic review of molecular and biological tumor markers in neuroblastoma. Clin. Cancer Res. 2004, 10, 4–12. [Google Scholar] [CrossRef] [Green Version]
- Newman, E.A.; Nuchtern, J.G. Seminars in pediatric surgery recent biologic and genetic advances in neuroblastoma: Implications for diagnostic, risk stratification, and treatment strategies. Semin. Pediatr. Surg. 2016, 25, 257–264. [Google Scholar] [CrossRef]
- Newman, E.A.; Abdessalam, S.; Aldrink, J.H.; Austin, M.; Heaton, T.E.; Bruny, J.; Ehrlich, P.; Dasgupta, R.; Baertschiger, R.M.; Lautz, T.B.; et al. Update on neuroblastoma. Pediatr. Surg. 2019, 54, 383–389. [Google Scholar] [CrossRef]
- Lindskog, M.; Spenger, C.; Klason, T.; Jarvet, J.; Gräslund, A.; Johnsen, J.I.; Ponthan, F.; Douglas, L.; Nordell, B.; Kogner, P. Proton magnetic resonance spectroscopy in neuroblastoma: Current status, prospects and limitations. Cancer Lett. 2005, 228, 247–255. [Google Scholar] [CrossRef]
- Lindskog, M.; Jarvet, J.; Graslund, A.; Kogner, P. Monitoring intracellular metabolites in neuroblastoma with 1H NMR spectroscopy: Effects of growth factor withdrawal and modulation of lipid metabolism. Spectroscopy 2004, 18, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Kohe, S.E.; Bennett, C.D.; Gill, S.K.; Wilson, M.; Mcconville, C.; Peet, A.C. Metabolic profiling of the three neural derived embryonal pediatric tumors retinoblastoma, neuroblastoma and medulloblastoma, identifies distinct metabolic profiles. Oncotarget 2018, 9, 11336–11351. [Google Scholar] [CrossRef] [Green Version]
- Marshall, G.M.; Carter, D.R.; Cheung, B.B.; Liu, T.; Mateos, M.K.; Meyerowitz, J.G.; Weiss, W.A. The prenatal origins of cancer. Nat. Rev. Cancer 2014, 14, 277–289. [Google Scholar] [CrossRef] [Green Version]
- Aminzadeh, S.; Vidali, S.; Sperl, W.; Kofler, B.; Feichtinger, R.G. Energy metabolism in neuroblastoma and Wilms tumor. Trans. Pediatr. 2015, 4, 20–32. [Google Scholar] [CrossRef]
- Cresswell, G.D.; Apps, J.R.; Chagtai, T.; Mifsud, B.; Bentley, C.C.; Maschietto, M.; Popov, S.D.; Weeks, M.E.; Olsen, Ø.E.; Sebire, N.J.; et al. Intra-tumor genetic heterogeneity in Wilms tumor: Clonal evolution and clinical implications. EBioMedicine 2016, 9, 120–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maschietto, M.; de Camargo, B.; Brentani, H.; Grundy, P.; Sredni, S.T.; Torres, C.; Mota, L.D.; Cunha, I.W.; Patrão, D.F.; Costa, C.M.; et al. Molecular profiling of isolated histological components of Wilms tumor implicates a common role for the Wnt signaling pathway in kidney and tumor development. Oncology 2008, 75, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Brok, J.; Treger, T.D.; Gooskens, S.L.; van den Heuvel-Eibrink, M.M.; Pritchard-Jones, K. Biology and treatment of renal tumours in childhood. Eur. J. Cancer 2016, 68, 179–195. [Google Scholar] [CrossRef] [Green Version]
- Charlton, J.; Pavasovic, V.; Pritchard-Jones, K. Biomarkers to detect Wilms tumors in pediatric patients: Where are we now? Future Neurol. 2015, 11, 2221–2234. [Google Scholar] [CrossRef]
- Cone, E.B.; Dalton, S.S.; Van Noord, M.; Tracy, E.; Rice, H.E.; Routh, J.C. Biomarkers for Wilms tumor: A systematic review. J. Urol. 2016, 196, 1530–1535. [Google Scholar] [CrossRef] [Green Version]
- Phelps, H.M.; Kaviany, S.; Borinstein, S.C.; Lovvorn, H.N. Biological drivers of Wilms tumor prognosis and treatment. Children 2018, 5, 145. [Google Scholar] [CrossRef] [Green Version]
- MacLellan, D.; Karakach, T.; Naranjo, A.; Fernandez, C.V. Urinary metabolite profiling by nuclear magnetic resonance spectroscopy to distinguish control patients from Wilms tumor (WT) and WT tumor by stage. J. Clin. Oncol. 2014, 15. [Google Scholar] [CrossRef]
- Lopes, R.I.; Lorenzo, A. Recent advances in the management of Wilms’ tumor. F1000Research 2017, 6, 1–11. [Google Scholar] [CrossRef]
- Aronson, D.C.; Meyers, R.L. Seminars in Pediatric Surgery Malignant tumors of the liver in children. Semin. Pediatr. Surg. 2016, 25, 265–275. [Google Scholar] [CrossRef]
- Cohen, M.J. Beckwith-Wiedemann syndrome: Historical, clinicopathological, and etiopathogenetic perspectives. Pediatr. Dev. Pathol. 2005, 8, 287–304. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.; Li, F.P.; Kingston, J.E.; Krush, A.J.; Strong, L.C.; Finegold, M.J.; Bertario, L.; Bülow, S.; Filippone, A.; Gedde-Dahl, T.; et al. Hepatoblastoma and familial adenomatous polyposis. J. Natl. Cancer Inst. 1989, 80, 1626–1628. [Google Scholar] [CrossRef] [PubMed]
- Maschietto, M.; Rodrigues, T.C.; Kashiwabara, A.Y.; de Araujo, É.S.S.; Marques Aguiar, T.F.; da Costa, C.M.L.; da Cunha, I.W.; Dos Reis Vasques, L.; Cypriano, M.; Brentani, H.; et al. DNA methylation landscape of hepatoblastomas reveals arrest at early stages of liver differentiation and cancer-related alterations. Oncotarget 2016, 8, 97871–97889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguiar Marques Ferreira, T.; Carneiro, T.N.; Lima da costa, C.M.; Rosenberg, C.; Werneck da cunha, I.; Krepischi, A.C.V. The genetic and epigenetic landscapes of hepatoblastomas. Appl. Cancer Res. 2017, 37, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Hiyama, E. Pediatric hepatoblastoma: Diagnosis and treatment. Transl. Pediatr. 2014, 3, 293–299. [Google Scholar] [CrossRef]
- Meyers, R.L.; Maibach, R.; Hiyama, E.; Häberle, B.; Krailo, M.; Rangaswami, A.; Aronson, D.C.; Malogolowkin, M.H.; Perilongo, G.; von Schweinitz, D.; et al. Risk-stratifi ed staging in paediatric hepatoblastoma: A unified analysis from the Children’s Hepatic tumors International Collaboration. Lancet Oncol. 2017, 18, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Kohe, S.; Brundler, M.; Jenkinson, H.; Parulekar, M.; Wilson, M.; Peet, A.C. Metabolite profiling in retinoblastoma identifies novel clinicopathological subgroups. Br. J. Cancer 2015, 113, 1216–1224. [Google Scholar] [CrossRef] [Green Version]
- Pandey, R.; Caflisch, L.; Lodi, A.; Brenner, A.J.; Tiziani, S. Metabolomic signature of brain cancer. Mol. Carcinog. 2017, 56, 2355–2371. [Google Scholar] [CrossRef]
- Cheng, L.; Ma, M.; Becerra, L.; Ptak, T.; Tracey, I.; Lackner, A.; González, R.G. Quantitative neuropathology by high resolution magic angle spinning proton magnetic resonance spectroscopy. Proc. Natl. Acad. Sci. USA 1997, 94, 6408–6413. [Google Scholar] [CrossRef] [Green Version]
- Tsang, T.; Griffin, J.; Haselden, J.; Fish, C.; Holmes, E. Metabolic characterization of distinct neuroanatomical regions in rats by magic angle spinning 1H nuclear magnetic resonance spectroscopy. Magn. Reson. Med. 2005, 53, 1018–1024. [Google Scholar] [CrossRef]
- Kool, M.; Korshunov, A.; Remke, M.; Jones, D.T.; Schlanstein, M.; Northcott, P.A.; Cho, Y.J.; Koster, J.; Schouten-van Meeteren, A.; van Vuurden, D.; et al. Molecular subgroups of medulloblastoma: An international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 2012, 123, 473–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bluml, S.; Margol, A.S.; Sposto, R.; Kennedy, R.J.; Robison, N.J.; Vali, M.; Hung, L.T.; Muthugounder, S.; Finlay, J.L.; Erdreich-Epstein, A.; et al. Molecular subgroups of medulloblastoma identification using noninvasive magnetic resonance spectroscopy. Neuro Oncol. 2016, 18, 126–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerges, N.; Fontebasso, A.M.; Albrecht, S.; Faury, D.; Jabado, N. Pediatric high-grade astrocytomas: A distinct neuro-oncological paradigm. Genome Med. 2013, 5, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Majos, C.; Bruna, J.; Julia-Sape, M.; Cos, M.; Camins, A.; Gil, M.; Acebes, J.J.; Aguilera, C.; Arús, C. Proton MR spectroscopy provides relevant prognostic information in high-grade astrocytomas. AJNR Am. J. Neuroradiol. 2011, 32, 74–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venkatesh, H.S.; Chaumeil, M.M.; Ward, C.S.; Haas-Kogan, D.A.; James, C.D.; Ronen, S. Reduced phosphocholine and hyperpolarized lactate provide magnetic resonance biomarkers of PI3K/Akt/mTOR inhibition in glioblastoma. Neuro Oncol. 2012, 14, 315–325. [Google Scholar] [CrossRef] [Green Version]
- Paulino, A.C.; Wen, B.C.; Buatti, J.M.; Hussey, D.H.; Zhen, W.K.; Mayr, N.A.; Menezes, A.H. Intracranial ependymomas: An analysis of prognostic factors and patterns of failure. Am. J. Clin. Oncol. 2002, 25, 117–122. [Google Scholar] [CrossRef]
- Marinoff, A.E.; Ma, C.; Guo, D.; Snuderl, M.; Wright, K.D.; Manley, P.E.; Al-Sayegh, H.; Sinai, C.E.; Ullrich, N.J.; Marcus, K.; et al. Rethinking childhood ependymoma: A retrospective, multi-center analysis reveals poor long-term overall survival. J. Neurooncol. 2017, 135, 201–211. [Google Scholar] [CrossRef]
- Pontes, J.G.M.; Brasil, A.J.M.; Cruz, G.C.F.; de Souza, R.N.; Tasic, L. NMR-based metabolomics strategies: Plants, animals and humans. Anal. Methods 2017, 9, 1078–1096. [Google Scholar] [CrossRef]
- Lu, Y.; Delijani, K.; Mecum, A.; Goldkorn, A. Current status of liquid biopsies for the detection and management of prostate cancer. Cancer Manag. Res. 2019, 11, 5271–5291. [Google Scholar] [CrossRef] [Green Version]
- Clark, A.R.; Calligans, D.; Regan, M.S.; Krummel, D.P.; Agar, J.N.; Kallay, L.; MacDonald, T.; Schiniderjan, M.; Santagata, S.; Pomeroy, S.L.; et al. Rapid discrimination of pediatric brain tumors by mass spectrometry imaging. J. Neurooncol. 2018, 140, 269–279. [Google Scholar] [CrossRef] [Green Version]
- Paine, M.R.L.; Liu, J.; Huang, D.; Ellis, S.R.; Trede, D.; Kobarg, J.H.; Heeren, R.M.A.; Fernández, F.M.; MacDonald, T.J. Three-dimensional mass spectrometry imaging identifies lipid markers of medulloblastoma metastasis. Sci. Rep. 2019, 9, 2205. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Pediatric Tumor Type | Sample Type | Analytical Platforms | Research Area |
|---|---|---|---|
| Acute lymphoblastic leukemia (ALL) | Plasma | 1H-NMR | Lipids [17] |
| Acute lymphoblastic leukemia (ALL) | Blood | HR-MAS | Tumor microenvironment [18] |
| Atypical teratoid /rhabdoid tumors | Tissue | HR-MAS | Metabolic profiles [19] |
| Brain tumor (astrocytomas and medulloblastoma) | Tissue | 1H-NMR, HR-MAS | Metabolic characterization [20,21] |
| Brain and nervous system | Tissue | HR-MAS | Metabolic differences [22] |
| Cerebellar ependymoma | Tissue | HR-MAS | Metabolic profiles [19] |
| Ependymoma | Tissue | HR-MAS | Metabolic characterization [19,23] |
| Medulloblastoma | Tissue | HR-MAS, 1H-NMR | Metabolic characterization [19,23,24] |
| Neuroblastoma | Cell Cultures | 1H-NMR | Anomalous choline metabolic patterns [25] |
| Neuroblastoma | Serum | 1H-NMR | Utility of metabolomics in xenograft models |
| Neuroblastoma | Tissue | HR-MAS | Metabolomic profile [26] |
| Osteosarcoma | Cell Cultures | HR-MAS | Effect of cisplatin on the metabolic profile [27] |
| Osteosarcoma | Cell Cultures | 1H-NMR | Metabonomics to monitor anticancer drugs [24,25] |
| Pilocytic astrocytoma | Tissue | HR-MAS, 1H-MRS | Metabolic characterization [18] |
| Localization | Pediatric Tumor Type | Age of Presentation (Year) |
|---|---|---|
| Central Nervous System | Medulloblastoma, astrocytoma, ependymoma Atypical teratoid/rhabdoid tumors (ATRT) | 0–25 0–2 |
| Liver | Hepatoblastoma | 0–2 |
| Kidney | Nephroblastoma or Wilms tumor Rhabdoid tumor | 2–3 0–2 |
| Sympathetic Nervous System | Neuroblastoma | 0–4 |
| Bone | Osteosarcoma Ewing Sarcoma | 10–18 |
| Soft Tissue | Rhabdomyosarcoma | 2–8 |
| Eye | Retinoblastoma | 0–2 |
| Tumor Type | Sample | Metabolic Changes | Observations | Ref |
|---|---|---|---|---|
| Neuroblastoma | Tissue * | ↑acetate, lysine | >12 months | [21] |
| ↑glycine, glutamine, glutamate, myo-inositol, serine, citric acid | <12 months | [21] | ||
| glutamine/glutamate ratio, ↑aspartate, creatine, glycine, myo-inositol | Stages I–II | [21] | ||
| ↑acetate and creatine | Stage IV | [21] | ||
| ↑acetate and taurine | Poor prognosis | [21] | ||
| ↑aspartate, succinate, glutathione ↑lipids, NAA, myo-inositol, aspartate ↑taurine | Better prognosis Poor prognosis Poor prognosis | [21] [36] [21] | ||
| Cell lines ** | phosphatidylcholine, choline, glutamate, glutamine and branched chain amino acids ↑lipids/choline ratio and phospholipids ↑↓lipids | Mitochondria dysfunction Drug sensitive cells, when treated with cytotoxic agents Growth factor modulations | [20] [34] [35] | |
| Hepatoblastoma | HepG2 cells | ↑acyl groups of fatty acids, cholesterol, lactate, glycine, choline, phosphocholine, glycerophosphocholine (GPC), betaine, trimethylamine N-oxide (TMAO), hydroxyproline, branched-chain amino acids (BCAA), and glutamate ↓formiate ↑amino acids and energy metabolites ↓glutathione | Aflatoxin M1 Effects Metabolic modulations by Bisphenol A and 17β-Estradiol | [37] [38] |
| Central nervous system Medulloblastoma | Tissue * | ↑glutamate ↑citrate, aspartate, ↑phosphocholine, taurine glucose, scyllo-inositol ↑phosphocholine, glycine, creatine ↓glutamine ↓NAA | Prognostic brain marker Developmental stages Possible markers of malignancy Developmental stages | [17] [18] [36] [23] [18] |
| Astrocytoma | Tissue * | ↑glutamine ↑NAA, fatty acids, amino acids (Ile, Leu and Val), GABA, Glu ↓Cr, myo-inositol, taurine | Tumor identification Prognostic biomarker | [23] [18] |
| Ependymoma | Tissue * | ↑myo-inositol, glutathione ↓leucine, glutamine ↓taurine | Developmental stages Prognostic biomarker | [18] [19] |
| Retinoblastoma | Tissue * | ↑taurine ↑lipids ↓phosphocholine ↑GABA, Creatine ↓myo-inositol ↓glycine, NAA | Differentiation Necrosis Invasion Energy Metabolism Cell signaling Poor survival | [36] [36] [36] [37] [37] [37] [37] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quintero Escobar, M.; Maschietto, M.; Krepischi, A.C.V.; Avramovic, N.; Tasic, L. Insights into the Chemical Biology of Childhood Embryonal Solid Tumors by NMR-Based Metabolomics. Biomolecules 2019, 9, 843. https://doi.org/10.3390/biom9120843
Quintero Escobar M, Maschietto M, Krepischi ACV, Avramovic N, Tasic L. Insights into the Chemical Biology of Childhood Embryonal Solid Tumors by NMR-Based Metabolomics. Biomolecules. 2019; 9(12):843. https://doi.org/10.3390/biom9120843
Chicago/Turabian StyleQuintero Escobar, Melissa, Mariana Maschietto, Ana C. V. Krepischi, Natasa Avramovic, and Ljubica Tasic. 2019. "Insights into the Chemical Biology of Childhood Embryonal Solid Tumors by NMR-Based Metabolomics" Biomolecules 9, no. 12: 843. https://doi.org/10.3390/biom9120843






