Epidemiological and Liver Biomarkers Profile of Epstein-Barr Virus Infection and Its Coinfection with Cytomegalovirus in Patients with Hematological Diseases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Serological Analysis
2.3. Statistical Analysis
3. Results
3.1. Prevalence of EBV Infection and EBV/CMV Coinfection
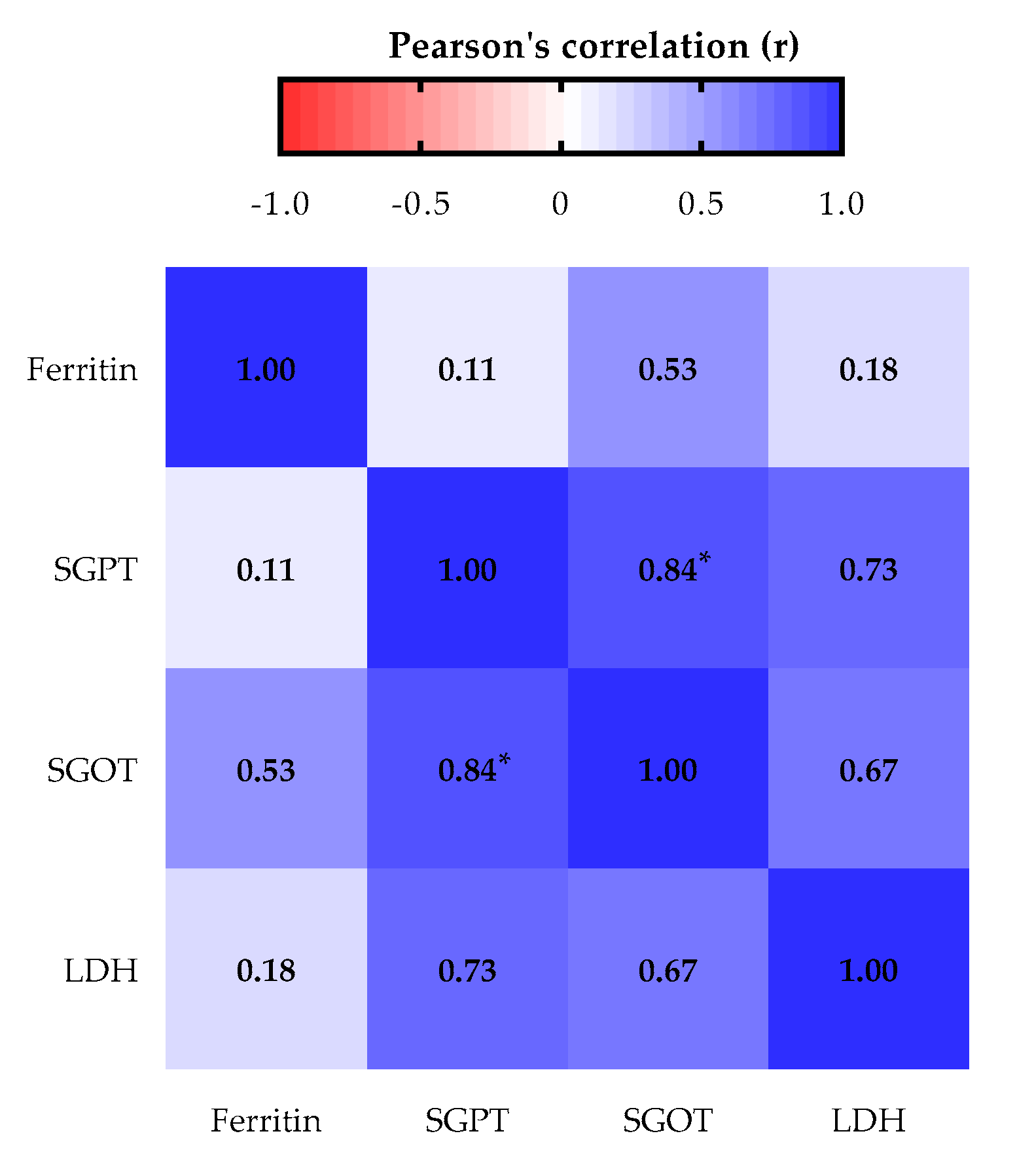
3.2. Liver Biomarkers Profile
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ambinder, R.F. Epstein-barr virus and hodgkin lymphoma. Hematol. Am. Soc. Hematol. Educ. Program 2007, 2007, 204–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolis, V.; Karadedos, C.; Chiotis, I.; Chaliasos, N.; Tsabouri, S. Atypical manifestations of Epstein-Barr virus in children: A diagnostic challenge. J. Pediatr. Rio. J. 2016, 92, 113–121. [Google Scholar] [CrossRef] [Green Version]
- Levine, H.; Balicer, R.D.; Rozhavski, V.; Halperin, T.; Shreberk, M.; Davidovitch, N.; Huerta-Hartal, M.; Ankol, O.E. Seroepidemiology of Epstein-Barr virus and cytomegalovirus among Israeli male young adults. Ann. Epidemiol. 2012, 22, 783–788. [Google Scholar] [CrossRef]
- Balfour, H.H.; Sifakis, F.; Sliman, J.A.; Knight, J.A.; Schmeling, D.O.; Thomas, W. Age-Specific prevalence of epstein-barr virus infection among individuals aged 6-19 years in the United States and factors affecting its acquisition. J. Infect. Dis. 2013, 208, 1286–1293. [Google Scholar] [CrossRef] [Green Version]
- Figueira-Silva, C.M.; Pereira, F.E. Prevalence of Epstein-Barr virus antibodies in healthy children and adolescents in Vitoria, State of Espirito Santo, Brazil. Rev. Soc. Bras. Med. Trop. 2004, 37, 409–412. [Google Scholar] [CrossRef] [Green Version]
- Zamora, M.R. DNA viruses (CMV, EBV, and the herpesviruses). Semin. Respir. Crit. Care Med. 2011, 32, 454–470. [Google Scholar] [CrossRef]
- Mecadon, K.; Jandovitz, N.; Salerno, D.; Martinez, M.; Kato, T. Treatment of Epstein-Barr Virus Viremia in Pediatric Intestinal and Liver Transplant Recipients. Transplantation 2017, 39, 2017. [Google Scholar] [CrossRef]
- Salter, B.; Sehmi, R. Epstein-Barr Virus—Induced Gene 2 and Leukocyte Airway Recruitment in Response to Allergen Challenge When Innate Responses Matter: ILC2s Loom Large in Allergic Airway In fl ammation. Am. J. Respir. Crit. Care Med. 2017, 195, 1543–1544. [Google Scholar] [CrossRef]
- Monteiro, T.A.F.; Costa, I.B.; Costa, I.B.; dos Corrêa, T.L.S.; Coelho, B.M.R.; Silva, A.E.S.; de Ramos, F.L.P.; Filho, A.J.M.; Monteiro, J.L.F.; Siqueira, J.A.M.; et al. Genotypes of Epstein-Barr virus (EBV1/EBV2) in individuals with infectious mononucleosis in the metropolitan area of Belém, Brazil, between 2005 and 2016. Brazilian J. Infect. Dis. 2020, 24, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Dematapitiya, C.; Perera, C.; Chinthaka, W.; Senanayaka, S.; Tennakoon, D.; Ameer, A.; Ranasinghe, D.; Warriyapperuma, U.; Weerarathna, S.; Satharasinghe, R. Cold type autoimmune hemolytic anemia- a rare manifestation of infectious mononucleosis; Serum ferritin as an important biomarker. BMC Infect. Dis. 2019, 19, 1–4. [Google Scholar] [CrossRef]
- Epstein, M.A.; Barr, Y.M.; Achong, B.G. Virus particles in cultured lymphoblasts from Burkitt’s lymphoma. Lancet 1964, 15, 702–703. [Google Scholar] [CrossRef]
- Chen, Y.A.; Wang, R.C.; Yang, Y.; Chuang, S.S. Epstein-Barr virus-positive diffuse large B cell lymphoma arising from a chronic lymphocytic leukemia: Overlapping features with classical Hodgkin lymphoma. Pathol. Int. 2016, 66, 393–397. [Google Scholar] [CrossRef]
- Sarwari, N.M.; Khoury, J.D.; Hernandez, C.M.R. Chronic Epstein Barr virus infection leading to classical Hodgkin lymphoma. BMC Hematol. 2016, 16, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Fujimoto, A.; Suzuki, R. Epstein-barr virus-associated post-transplant lymphoproliferative disorders after hematopoietic stem cell transplantation: Pathogenesis, risk factors and clinical outcomes. Cancers 2020, 12, 328. [Google Scholar] [CrossRef] [Green Version]
- Zuhair, M.; Smit, G.S.A.; Wallis, G.; Jabbar, F.; Smith, C.; Devleesschauwer, B.; Griffiths, P. Estimation of the worldwide seroprevalence of cytomegalovirus: A systematic review and meta-analysis. Rev. Med. Virol. 2019, 29, e2034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smatti, M.K.; Al-Sadeq, D.W.; Ali, N.H.; Pintus, G.; Abou-Saleh, H.; Nasrallah, G.K. Epstein-barr virus epidemiology, serology, and genetic variability of LMP-1 oncogene among healthy population: An update. Front. Oncol. 2018, 8, 211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiguman, G.M.B.; Poll, L.B.; de Castro Alves, C.E.; Pontes, G.S.; Silva, M.T.; Galvao, T.F. Seroprevalence of cytomegalovirus and its coinfection with epstein-barr virus in adult residents from manaus: A population-based study. Rev. Soc. Bras. Med. Trop. 2020, 53, e20190363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuri, A.; Jacobs, B.M.; Vickaryous, N.; Pakpoor, J.; Middeldorp, J.; Giovannoni, G.; Dobson, R. Epidemiology of Epstein-Barr Virus infection and Infectious Mononucleosis in the United Kingdom. BMC Public Health 2020, 20, 912. [Google Scholar] [CrossRef] [PubMed]
- Winter, J.R.; Taylor, G.S.; Thomas, O.G.; Jackson, C.; Lewis, J.E.A.; Stagg, H.R. Factors associated with cytomegalovirus serostatus in young people in England: A cross-sectional study. BMC Infect. Dis. 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Dowd, J.B.; Palermo, T.; Brite, J.; McDade, T.W.; Aiello, A. Seroprevalence of Epstein-Barr Virus Infection in U.S. Children Ages 6–19, 2003–2010. PLoS ONE 2013, 8, e64921. [Google Scholar] [CrossRef] [Green Version]
- Pourahamad, M.; Hooshmand, F.; Olyaee Nezhad, S.; Sepidkar, A. EBV seroepidemiology in married and unmarried women and men in Iran. Reports Biochem. Mol. Biol. 2014, 2, 94–947. [Google Scholar]
- de Melo Silva, J.; Pinheiro-Silva, R.; Dhyani, A.; Pontes, G.S. Cytomegalovirus and Epstein-Barr infections: Prevalence and impact on patients with hematological diseases. Biomed Res. Int. 2020, 2020. [Google Scholar] [CrossRef]
- Zhong, W.; Zhou, J.; Wei, X.; Wang, X.; Li, Y.; Peng, B.; Niu, T.; Niu, T. The role of epstein-barr virus (EBV) and cytomegalovirus (CMV) in immune thrombocytopenia. Hematology 2013, 18, 295–299. [Google Scholar] [CrossRef]
- Hsiao, C.C. Epstein-Barr virus associated with immune thrombocytopenic purpura in childhood: A retrospective study. J. Paediatr. Child Health 2000, 36, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Kogawa, K.; Sato, H.; Asano, T.; Ohga, S.; Kudo, K.; Morimoto, A.; Ohta, S.; Wakiguchi, H.; Kanegane, H.; Oda, M.; et al. Prognostic Factors of Epstein-Barr Virus-Associated Hemophagocytic Lymphohistiocytosis in Children: Report of the Japan Histiocytosis Study Group. Pediatr. Blood Cancer 2014, 61, 1257–1262. [Google Scholar] [CrossRef]
- Demirkol, D.; Kavgacl, U.; Babaoǧlu, B.; Tanju, S.; Oflaz Sözmen, B.; Tekin, S. Cytomegalovirus reactivation in a critically ill patient: A case report. J. Med. Case Rep. 2018, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Atim-Oluk, M. Cytomegalovirus associated haemophagocytic lymphohistiocytosis in the immunocompetent adult managed according to HLH-2004 diagnostic using clinical and sero logical means only. Eur. J. Microbiol. Immunol. 2013, 3, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Bonnecaze, A.; Willeford, W.G.; Lichstein, P.; Ohar, J. Acute Cytomegalovirus (CMV) Infection Associated with Hemophagocytic Lymphohistiocytosis (HLH) in an Immunocompetent Host Meeting All Eight HLH 2004 Diagnostic Criteria. Cureus 2017, 9, e1070. [Google Scholar] [CrossRef] [Green Version]
- Harley, J.B.; Chen, X.; Pujato, M.; Miller, D.; Maddox, A.; Forney, C.; Magnusen, A.F.; Lynch, A.; Chetal, K.; Yukawa, M.; et al. Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity. Nat. Genet. 2018, 50, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Enok Bonong, P.R.; Buteau, C.; Delage, G.; Tanner, J.E.; Lacroix, J.; Duval, M.; Laporte, L.; Tucci, M.; Robitaille, N.; Spinella, P.C.; et al. Transfusion-related Epstein-Barr virus (EBV) infection: A multicenter prospective cohort study among pediatric recipients of hematopoietic stem cell transplants (TREASuRE study). Transfusion 2021, 61, 144–158. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | N (%) | EBV IgG Positive (%) | EBV PR (95% CI) | p-Value a | Coinfection EBV/CMV Positive (%) | Coinfection PR (95% CI) | p-Value a |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 112 (49.12) | 92 (82.14) | 0.93 (0.83–1.04) | 0.149 | 84 (75.00) | 0.92 (0.79–1.05) | 0.134 |
| Female | 116 (50.88) | 102 (87.93) | 1.00 (ref.) | 95 (81.90) | 1.00 (ref.) | ||
| Age | |||||||
| 1–10 | 64 (28.07) | 46 (71.88) | 0.80 (0.66–0.91) | 0.001 * | 37 (57.81) | 0.67 (0.52–0.81) | <0.0001 * |
| 11–20 | 52 (22.81) | 45 (86.54) | 1.00 (ref.) | 41 (78.85) | 1.00 (ref.) | ||
| 21–30 | 28 (12.28) | 26 (92.86) | 1.11 (0.92–1.22) | 0.171 | 25 (89.29) | 1.16 (0.94–1.31) | 0.108 |
| 31–40 | 29 (12.72) | 28 (96.55) | 1.16 (0.99–1.26) | 0.058 | 28 (96.55) | 1.27 (1.08–1.40) | 0.011 * |
| 41–50 | 20 (8.77) | 15 (75.00) | 0.87 (0.62–1.05) | 0.159 | 15 (75.00) | 0.95 (0.67–1.15) | 0.454 |
| 51–60 | 20 (8.77) | 19 (95.00) | 1.13 (0.90–1.23) | 0.165 | 18 (90.00) | 1.16 (0.90–1.31) | 0.153 |
| >60 | 15 (6.58) | 15 (100.00) | 15 (100.00) | ||||
| Ethnicity | |||||||
| White | 64 (28.07) | 54 (84.38) | 0.99 (0.85–1.10) | 0.493 | 49 (76.56) | 0.97 (0.81–1.11) | 0.395 |
| Brown | 146 (64.04) | 125 (85.62) | 1.00 (ref.) | 115 (78.77) | 1.00 (ref.) | ||
| Black | 18 (7.89) | 15 (83.33) | 0.98 (0.71–1.13) | 0.450 | 15 (83.33) | 1.07 (0.77–1.24) | 0.413 |
| Marital status | |||||||
| Single | 168 (73.68) | 137 (81.55) | 1.00 (ref.) | 124 (73.81) | 1.00 (ref.) | ||
| Married | 60 (26.32) | 57 (95.00) | 1.17 (1.04–1.28) | 0.011 * | 55 (91.67) | 1.24 (1.09–1.40) | 0.003 * |
| Income | |||||||
| Up to a minimum wage | 115 (50.44) | 98 (85.22) | 1.02 (0.90–1.12) | 0.448 | 90 (78.26) | 0.99 (0.86–1.14) | 0.472 |
| 2–5 minimum wages | 102 (44.74) | 85 (83.33) | 1.00 (ref.) | 78 (76.47) | 1.00 (ref.) | ||
| Above 6 minimum wages | 11 (4.82) | 11 (100.00) | 11 (100.00) | ||||
| Level of schooling | |||||||
| Illiterate ** | 36 (15.79) | 25 (69.44) | 0.79 (0.60–0.94) | 0.004 * | 22 (61.11) | 0.75 (0.55–0.93) | 0.005 * |
| Literate *** | 53 (23.25) | 42 (79.25) | 0.91 (0.76–1.04) | 0.127 | 36 (67.92) | 0.83 (0.66–0.99) | 0.026 * |
| Complete middle school | 57 (25.00) | 52 (91.23) | 1.10 (0.96–1.21) | 0.099 | 49 (85.96) | 1.13 (0.97–1.28) | 0.081 |
| Complete high school | 49 (21.49) | 45 (91.84) | 1.10 (0.96–1.22) | 0.102 | 43 (87.76) | 1.16 (0.98–1.31) | 0.057 |
| Undergraduate | 23 (10.09) | 21 (91.30) | 1.00 (ref.) | 21 (91.30) | 1.00 (ref.) |
| Hematological Disease/Transfusion | N (%) | EBV IgG Positive (%) | EBV PR (95% CI) | p-Value a | Coinfection Positives (%) | Coinfection PR (95% CI) | p-Value a |
|---|---|---|---|---|---|---|---|
| Hematological disease | |||||||
| Anemia | 72 (31.58) | 61 (84.72) | 0.99 (0.87–1.11) | 0.462 | 56 (77.78) | 0.99 (0.84–1.13) | 0.496 |
| ITP | 20 (8.77) | 18 (90.00) | 1.06 (0.82–1.19) | 0.376 | 16 (80.00) | 1.02 (0.74–1.21) | 0.454 |
| Leukemia | 117 (51.32) | 98 (83.76) | 0.97 (0.86–1.08) | 0.348 | 92 (78.63) | 1.00 (0.87–1.16) | 0.454 |
| ALL | 83 (70.94) | 68 (81.93) | 0.93 (0.80–1.14) | 0.286 | 65 (78.31) | 0.99 (0.82–1.26) | 0.454 |
| AML | 22 (18.80) | 19 (86.36) | 1.00 (ref.) | 17 (77.27) | 1.00 (ref.) | ||
| CLL | 1 (0.86) | 1 (100.00) | 1 (100.00) | ||||
| CML | 11 (9.40) | 10 (90.91) | 1.10 (0.75–1.26) | 0.403 | 9 (81.82) | 1.05 (0.66–1.28) | 0.454 |
| Lymphoma | 19 (8.33) | 17 (89.47) | 1.00 (ref.) | 15 (78.95) | 1.00 (ref.) | ||
| Type of transfusion | 143 (62.72) | 119 (83.22) | 0.94 (0.85–1.06) | 0.202 | 111 (77.62) | 0.97 (0.85–1.13) | 0.399 |
| Complete | 101 (70.63) | 82 (57.34) | 0.92 (0.80–1.10) | 0.223 | 76 (75.25) | 0.90 (0.76–1.11) | 0.202 |
| Erythrocytes | 30 (20.98) | 28 (19.58) | 1.16 (0.96–1.31) | 0.082 | 26 (86.67) | 1.15 (0.92–1.35) | 0.138 |
| Erythrocytes/Platelets | 2 (1.40) | 2 (1.40) | 2 (100.00) | ||||
| Plasma | 1 (0.70) | 0 (0.00) | |||||
| Platelets | 9 (6.29) | 7 (4.90) | 0.93 (0.54–1.15) | 0.496 | 7 (77.78) | 1.00 (0.58–1.25) | 0.344 |
| No transfusion | 85 (37.28) | 75 (88.24) | 1.00 (ref.) | 68 (80.00) | 1.00 (ref.) | 0.399 |
| Liver Biomarkers | N (%) | EBV IgG Positive (%) | EBV PR (95% CI) | p-Value a | Coinfection EBV/CMV Positive (%) | Coinfection PR (95% CI) | p-Value a |
|---|---|---|---|---|---|---|---|
| Ferritin | |||||||
| Altered | 28 (38.89) | 27 (96.43) | 1.25 (1.03–1.54) | 0.031 * | 25 (89.29) | 1.31 (1.02–1.70) | 0.038 * |
| Normal | 44 (61.11) | 34 (77.27) | 1.00 (ref.) | 30 (68.18) | 1.00 (ref.) | ||
| SGPT | |||||||
| Altered | 7 (20.59) | 6 (85.71) | 1.16 (0.64–1.63) | 0.442 | 5 (71.43) | 1.02 (0.49–1.56) | 0.341 |
| Normal | 27 (79.41) | 20 (74.07) | 1.00 (ref.) | 19 (70.37) | 1.00 (ref.) | ||
| SGOT | |||||||
| Altered | 13 (34.21) | 10 (76.92) | 1.07 (0.66–1.56) | 0.476 | 10 (76.92) | 1.20 (0.73–1.84) | 0.328 |
| Normal | 25 (65.79) | 18 (72.00) | 1.00 (ref.) | 16 (64.00) | 1.00 (ref.) | ||
| LDH | |||||||
| Altered | 20 (55.56) | 18 (90.00) | 12.00 (0.88–1.81) | 0.227 | 17 (85.00) | 1.24 (0.86–1.96) | 0.223 |
| Normal | 16 (44.44) | 12 (75.00) | 1.00 (ref.) | 11 (68.75) | 1.00 (ref.) | ||
| Creatinine | |||||||
| Altered | 24 (64.86) | 18 (75.00) | 17 (70.83) | ||||
| Normal | 13 (35.14) | 13 (100.00) | 13 (100.00) | ||||
| Liver function | |||||||
| Altered | 40 (69.00) | 34 (85.00) | 1.16 (0.93–1.41) | 0.126 | 32 (80.00) | 1.18 (0.93–1.49) | 0.123 |
| Normal | 68 (31.00) | 50 (73.53) | 1.00 (ref.) | 46 (67.65) | 1.00 (ref.) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrari de Freitas, L.; de Melo Silva, J.; Nogueira Barbosa, A.; Miranda Santos, E.; Pinheiro-Silva, R.; Soares Pontes, G. Epidemiological and Liver Biomarkers Profile of Epstein-Barr Virus Infection and Its Coinfection with Cytomegalovirus in Patients with Hematological Diseases. Biomolecules 2021, 11, 1151. https://doi.org/10.3390/biom11081151
Ferrari de Freitas L, de Melo Silva J, Nogueira Barbosa A, Miranda Santos E, Pinheiro-Silva R, Soares Pontes G. Epidemiological and Liver Biomarkers Profile of Epstein-Barr Virus Infection and Its Coinfection with Cytomegalovirus in Patients with Hematological Diseases. Biomolecules. 2021; 11(8):1151. https://doi.org/10.3390/biom11081151
Chicago/Turabian StyleFerrari de Freitas, Lilian, Jean de Melo Silva, Anderson Nogueira Barbosa, Enzo Miranda Santos, Renato Pinheiro-Silva, and Gemilson Soares Pontes. 2021. "Epidemiological and Liver Biomarkers Profile of Epstein-Barr Virus Infection and Its Coinfection with Cytomegalovirus in Patients with Hematological Diseases" Biomolecules 11, no. 8: 1151. https://doi.org/10.3390/biom11081151







