Reconsultation and Antimicrobial Treatment of Urinary Tract Infection in Male and Female Patients in General Practice
Abstract
:1. Introduction
2. Results
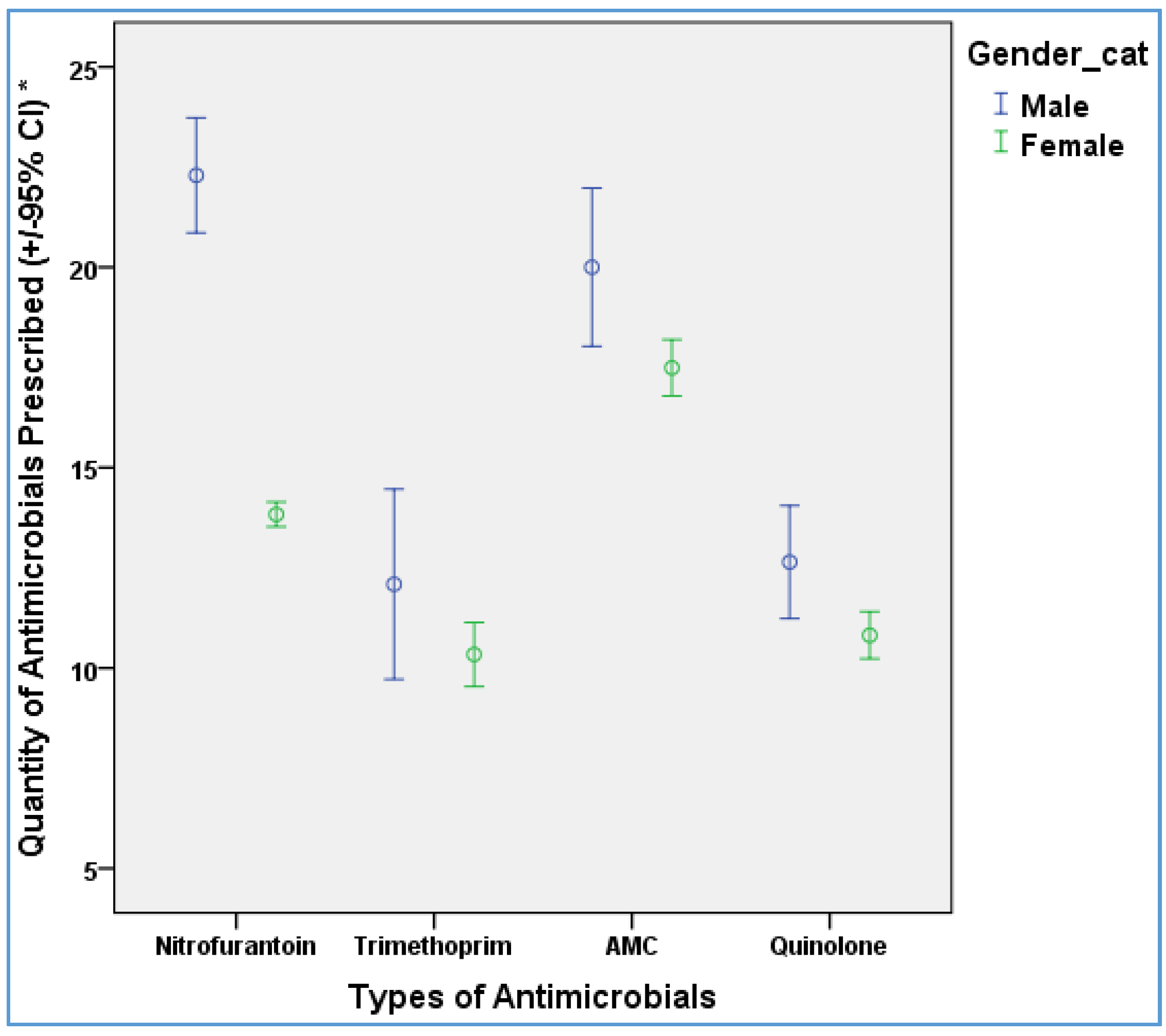
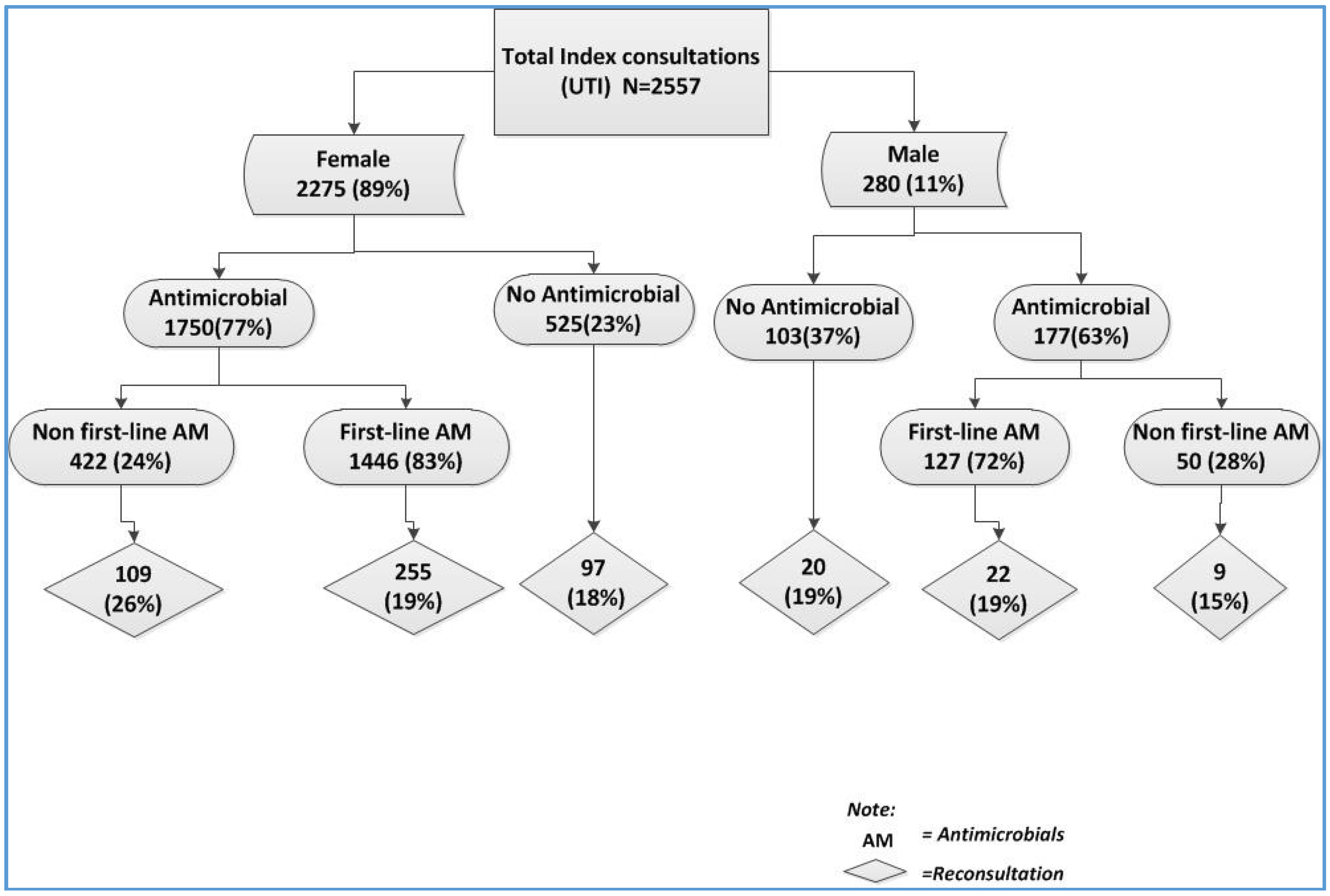
2.1. Antimicrobial Prescribing
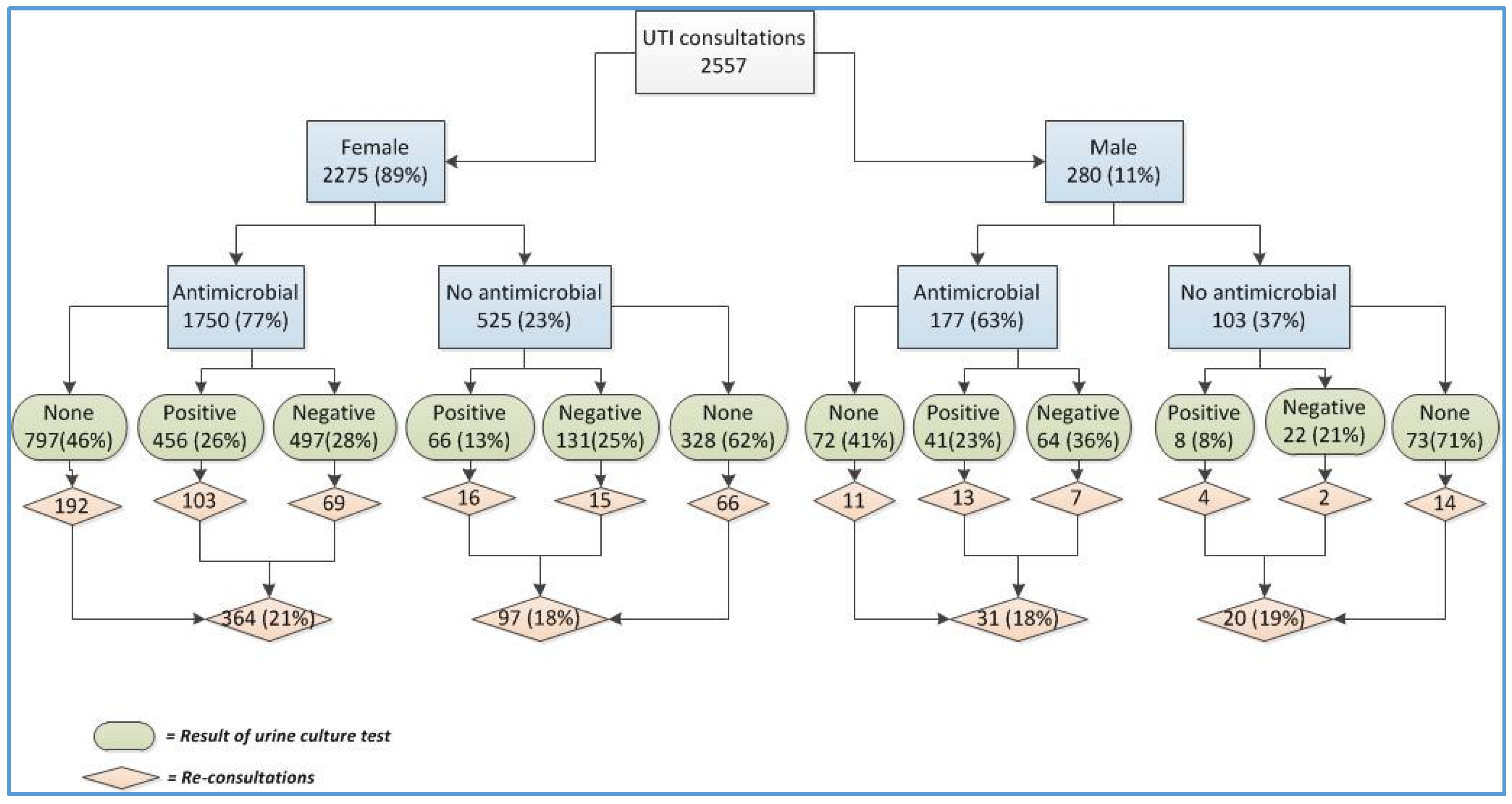
2.2. Urine Culture
2.3. Reconsultation
3. Discussion
4. Materials and Methods
4.1. UTI and Urine Culture
4.2. Reconsultation
4.3. Empirical Prescribing
4.4. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hooton, T.M.; Besser, R.; Foxman, B.; Fritsche, T.R.; Nicolle, L.E. Acute uncomplicated cystitis in an era of increasing antibiotic resistance: A proposed approach to empirical therapy. Clin. Infect. Dis. 2004, 39, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Nicolle, L.E. Epidemiology of Urinary Tract Infection. Infect. Med. 2001, 18, 153–162. [Google Scholar] [CrossRef]
- Guideline for Antimicrobial Prescribing in Primary Care in Ireland. Available online: http://www.antibioticprescribing.ie/urinary/adult-uncomplicated-uti (accessed on 21 April 2016).
- SIGN. Management of Suspected Bacterial Urinary Tract Infection in Adults: A National Clinical Guideline. Available online: http://www.sign.ac.uk/pdf/sign88.pdf (accessed on 27 July 2016).
- Drekonja, D.M.; Rector, T.S.; Cutting, A.; Johnson, J.R. Urinary tract infection in male veterans: Treatment patterns and outcomes. JAMA Intern. Med. 2013, 173, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Trautner, B.W. New perspectives on urinary tract infection in men comment on “urinary tract infection in male veterans: Treatment patterns and outcomes” and on “preoperative urine cultures at a veterans affairs medical center”. JAMA Intern. Med. 2013, 173, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Hummers-Pradier, E.; Ohse, A.M.; Koch, M.; Heizmann, W.R.; Kochen, M.M. Urinary tract infection in men. Int. J. Clin. Pharmacol. Ther. 2004, 42, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Den Heijer, C.D.; van Dongen, M.C.; Donker, G.A.; Stobberingh, E.E. Diagnostic approach to urinary tract infections in male general practice patients: A national surveillance study. Br. J. Gen. Pract. 2012, 62, e780–e786. [Google Scholar] [CrossRef] [PubMed]
- Den Heijer, C.D.J.; Penders, J.; Donker, G.A.; Bruggeman, C.A.; Stobberingh, E.E. The importance of gender-stratified antibiotic resistance surveillance of unselected uropathogens: A Dutch Nationwide Extramural Surveillance study. PLoS ONE 2013, 8, e60497. [Google Scholar] [CrossRef] [PubMed]
- Management of Suspected Lower Urinary Tract Infection in Adult Men. Available online: http://www.sign.ac.uk/pdf/sign88_algorithm_adult_men.pdf (accessed on 27 July 2016).
- Duane, S.; Callan, A.; Galvin, S.; Murphy, A.W.; Domegan, C.; O’Shea, E.; Cormican, M.; Bennett, K.; O’Donnell, M.; Vellinga, A. Supporting the improvement and management of prescribing for urinary tract infections (SIMPle): Protocol for a cluster randomized trial. Trials 2013. [Google Scholar] [CrossRef] [PubMed]
- Irish Primary Care Research Network (IPCRN). Available online: http://www.ipcrn.ie/ (accessed on 12 August 2015).
- Health Insurance Authority. Health Insurance Authority Consumers Survey; Health Insurance Authority: Dublin, Ireland, 2014. [Google Scholar]
- European Society of Clinical Microbiology and Infectious Disease (EUCAST). Available online: http://www.eucast.org/ (accessed on 12 November 2015).
- Gupta, K.; Hooton, T.M.; Naber, K.G.; Wullt, B.; Colgan, R.; Miller, L.G.; Moran, G.J.; Nicolle, L.E.; Raz, R.; Schaefferet, A.J.; et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin. Infect. Dis. 2011, 52, e103–e120. [Google Scholar] [CrossRef] [PubMed]
- Vellinga, A.; Galvin, S.; Duane, S.; Callan, A.; Bennett, K.; Cormican, M.; Domegan, C.; Murphy, A.W. Intervention to improve the quality of antimicrobial prescribing for urinary tract infection: A cluster randomized trial. CMAJ 2015. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Male | Female | p-Value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Index consultation | 280 | 11.0 | 2275 | 89.0 | |
| Reconsultation | 51 | 18.2 | 461 | 20.3 | ns |
| Age in years (mean and SD) | 63.6 | 17.8 | 52.4 | 20.9 | <0.001 |
| 17–25 | 8 | 2.9 | 275 | 12.0 | |
| 26–50 | 52 | 18.6 | 802 | 35.3 | |
| 50–75 | 134 | 47.9 | 814 | 35.8 | |
| >75 | 86 | 30.7 | 384 | 16.9 | |
| Medical card | 194 | 69.3 | 1372 | 60.3 | 0.004 |
| Arms | |||||
| Intervention arm A | 100 | 35.7 | 698 | 30.7 | ns |
| Intervention arm B | 89 | 31.8 | 827 | 36.4 | |
| Control arm | 91 | 32.5 | 750 | 33.0 | |
| Antimicrobial prescribed | 177 | 63.2 | 1750 | 76.9 | <0.001 |
| Types of antimicrobial prescribed | |||||
| Nitrofurantoin | 116 | 41.4 | 1328 | 58.4 | <0.001 |
| Trimethoprim | 11 | 3.9 | 118 | 5.2 | ns |
| Fluoroquinolone | 31 | 11.1 | 71 | 3.1 | <0.001 |
| Co-amoxiclav | 14 | 5.0 | 140 | 6.2 | ns |
| Amoxicillin | 3 | 1.1 | 43 | 1.9 | ns |
| Duration of treatment (median, min-max) where antimicrobial was prescribed | 7 | 1–14 | 3 | 1–28 | <0.001 |
| Duration of treatment (days) for types of antimicrobial prescribed (median, min-max) | |||||
| Nitrofurantoin | 7 | 1–10 | 3 | 1–28 | <0.001 |
| Trimethoprim | 5 | 1–14 | 5 | 1–14 | 0.002 |
| Fluoroquinolone | 5 | 1–10 | 5 | 1–10 | ns |
| Co-amoxiclav | 7 | 1–7 | 7 | 1–15 | ns |
| Urine sample obtained | 135 | 48.2 | 1150 | 50.5 | ns |
| Positive culture | 49 | 36.3 | 522 | 45.4 | 0.04 |
| Resistance to any tested antimicrobial | 33 | 73.3 | 268 | 56.3 | 0.02 |
| Types of bacteria (among + ve culture) | |||||
| E. coli/coliform | 40 | 14.3 | 442 | 19.4 | 0.03 |
| Proteus spp. | 2 | 3.3 | 17 | 2.4 | ns |
| Staphylococcus | 0 | 28 | |||
| Other | 7 | 35 | |||
| Characteristics | OR | 95% CI | p-Value |
|---|---|---|---|
| Gender | |||
| Male | reference | ||
| Female | 1.4 | 1.0–1.9 | 0.04 |
| Age | 1.02 | 1.0–1.02 | <0.001 |
| Medical card | |||
| No | reference | ||
| Yes | 1.7 | 1.3–2.1 | <0.001 |
| Prescribed antimicrobials | |||
| No | reference | ||
| Yes | 1.2 | 0.96–1.5 | 0.1 |
| Intervention | |||
| Control (arm C) | reference | ||
| Intervention (arm A and B) | 0.6 | 0.5–0.8 | <0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tandan, M.; Duane, S.; Cormican, M.; Murphy, A.W.; Vellinga, A. Reconsultation and Antimicrobial Treatment of Urinary Tract Infection in Male and Female Patients in General Practice. Antibiotics 2016, 5, 31. https://doi.org/10.3390/antibiotics5030031
Tandan M, Duane S, Cormican M, Murphy AW, Vellinga A. Reconsultation and Antimicrobial Treatment of Urinary Tract Infection in Male and Female Patients in General Practice. Antibiotics. 2016; 5(3):31. https://doi.org/10.3390/antibiotics5030031
Chicago/Turabian StyleTandan, Meera, Sinead Duane, Martin Cormican, Andrew W. Murphy, and Akke Vellinga. 2016. "Reconsultation and Antimicrobial Treatment of Urinary Tract Infection in Male and Female Patients in General Practice" Antibiotics 5, no. 3: 31. https://doi.org/10.3390/antibiotics5030031






