3.1. Preparation, Characterization, and Stability of Nanoparticles
All the nanoparticles were successfully developed. HSA and MTX-HSA nanoparticles were prepared using the desolvation method, TRZ-MTX-HSA-1 nanoparticles were prepared using the adsorption method, and TRZ-MTX-HSA-2 nanoparticles were prepared using the covalent binding method. The characterization properties of nanoparticles are listed in
Table 1.
The particle size of nanostructured delivery systems plays a significant role in their accumulation in the tumor tissue, owing to the enhanced permeability and retention (EPR) effect. Nano-drug delivery systems must escape from the RES and stay in the bloodstream longer to achieve the EPR effect. It has been suggested that nanoparticles with an average size of 200–300 nm are optimal for extending the half-life in blood circulation [
47].
According to the data, HSA nanoparticles were produced with a particle size of 183.9 ± 3.08 nm and PDI of 0.05 ± 0.02. The particle size and PDI value of MTX-HSA nanoparticles prepared by adding MTX to HSA nanoparticles were 207.5 ± 2.02 nm and 0.04 ± 0.02, respectively. The particle size of TRZ-MTX-HSA nanoparticles prepared by the adsorption method was 224.1 ± 2.46 nm, and the particle size of TRZ-MTX-HSA nanoparticles prepared by the covalent bonding method was 289.0 ± 2.62 nm. The PDI value of TRZ-MTX-HSA-1 and TRZ-MTX-HSA-2 nanoparticles was 0.09 ± 0.07 and 0.29 ± 0.05, respectively. The method developed for all nanoparticle formulations was simple and repeatable.
The in vivo performance of nanoparticles can be determined by focusing on their physicochemical characteristics. A nanometer-range PDI value should be the maximum for intravenous injection in a well-designed nanoparticular system. It has been stated that nanocarriers should have 200 nm particle size to guarantee the stability of an injectable colloidal formulation [
48]. The PDI represents the degree of uniformity in the particle size distribution. The PDI scale has values between 0.0 (monodisperse) and 1.0 (polydisperse) [
49]. A PDI value ≤ 0.3 or below, which is usually optimal for drug delivery applications, represents a homogeneous dispersion of particles [
50,
51]. Therefore, our results suggest that the TRZ-MTX-HSA nanoparticles are uniform. Additionally, it was discovered that the nanoparticle particle sizes (
Table 1) were suitable for circulation for a longer period and for using the EPR effect to target the tumor preferentially.
Whether colloidal systems are stable depends critically on the ζ potential, which symbolizes the electrostatic charge on the nanoparticle surface [
52]. Also, the interaction of the drug delivery system with the biological system is affected by ζ potential value. A ζ potential of less than −50 mV or more than +50 mV can prevent particle aggregation compared to uncharged particles [
53]. In this study, the ζ potential value of all negatively charged nanoparticle formulations was below −50 mV.
In a study, MTX-HSA nanoparticles developed by Jain et al. [
54] had a particle size of 264 ± 3.5 nm, a PDI value of 0.21 ± 0.07, and a ζ potential value of −12.3 ± 2.7 mV. Similarly, in another study, biotin-functionalized MTX-HSA nanoparticles were produced with a particle size between 111 and 145 nm, PDI value between 0.10 and 0.24, and ζ potential between −12.1 and −20.45 mV [
20]. In accordance with Taheri et al. [
27], TRZ-MTX-HSA nanoparticles were developed with a particle size between 123.0 ± 12.0 and 346.0 ± 11.1 nm, PDI value between 0.18 ± 0.10 and 0.24 ± 0.09, and ζ potential between −31.30 ± 1.11 and −34.20 ± 2.41 mV. Based on the literature, we successfully synthesized all nanoparticle formulations.
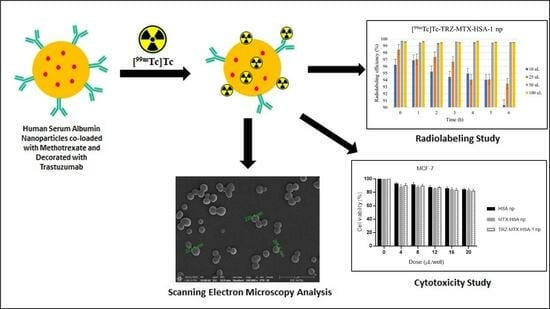
SEM images were captured to determine the surface morphology of the nanoparticles (
Figure 1).
The nanoparticles were spherical and had smooth surfaces in the obtained images (
Figure 1). The resulting nanoparticles had sizes ranging from 173.2 nm to 270.6 nm, and the measurements with the Malvern ZetaSizer were in line with the results.
UV–Vis spectrophotometric methods were successfully developed to calculate the encapsulated amounts of MTX and TRZ in nanoparticle formulations. The λ
max of MTX was 303 nm, and the λ
max of TRZ was 280 nm. While the calibration curve of MTX was linear in the concentration range of 0.5–10 μg × mL
−1 (r
2 = 0.9998) and y = 0.0546x − 0.0191, the calibration curve of TRZ was linear in the concentration range of 50–200 μg × mL
−1 (r
2 = 0.9993) and y = 0.00132x − 0.00146. The EE (%) and LC (%) of MTX in the TRZ-MTX-HSA nanoparticle formulations were 32.46 ± 1.12 and 40.62 ± 2.56, respectively. The EE (%) of TRZ in TRZ-MTX-HSA nanoparticle formulations was calculated as between 75.64 ± 2.25 and 80.26 ± 1.96%, respectively. All formulations had high EE (%) and LC (%) values, and no statistical difference was observed among the nanoparticle formulations (
p > 0.05) (
Table 2). These calculated values were compatible with the literature [
54].
The stability of the nanoparticles was evaluated under three storage conditions over three months, and the results are displayed in
Table 3,
Table 4 and
Table 5. All the nanoparticles were stable and did not significantly change the characterization parameters under any of the three conditions (
p > 0.05).
Agents such as methotrexate–human serum albumin (MTX-HSA) are commonly employed in drug delivery systems. The main goal is to enhance the therapeutic agent’s targeted delivery, stability, and efficacy while minimizing off-target effects and reducing potential toxicity. In this sense, adsorption and covalent bonding are two methods used for conjugating these agents, each with their own rationales and benefits. The adsorption involves the physical binding of molecules to the nanoparticle surface through non-covalent interactions, such as hydrogen bonding, hydrophobic interactions, and electrostatic forces. The rationales for using the adsorption method include simplicity (adsorption is a relatively straightforward method that does not require complex chemical reactions), preservation of activity (adsorption typically involves milder conditions than covalent bonding, which can help preserve the biological activity of the therapeutic agent), and flexibility (adsorption method allows for reversible interactions) [
55,
56,
57].
Otherwise, the covalent bonding method involves forming strong chemical bonds between the therapeutic agent and the nanoparticle surface, offering stability (covalent bonds are much stronger and more stable than non-covalent interactions), specificity (covalent bonding allows for precise control over the site of attachment and the number of therapeutic agents attached to each nanoparticle), longer circulation time (covalently bound conjugates often exhibit enhanced circulation time in the bloodstream due to reduced susceptibility to degradation and clearance mechanisms), and targeting (covalent attachment can be designed to enable active targeting by incorporating targeting ligands on the nanoparticle surface) [
58,
59]. In the case of conjugating TRZ with MTX-HSA nanoparticles, the method chosen (adsorption or covalent bonding) will depend on factors such as the stability of TRZ under different conditions, the desired release profile of the therapeutic agent, the level of control needed over the attachment process, and the specific goals of the drug delivery system (e.g., targeted delivery, controlled release). Both methods have their merits, and researchers often select the method that best suits their intended application while considering factors such as stability, specificity, ease of preparation, and overall performance in vitro and in vivo.
The results revealed that the adsorption and covalent bonding methods used to prepare TRZ-MTX-HSA nanoparticles considerably affected the physicochemical characterization of the particles (p < 0.05). The most suitable method for the preparation of TRZ-MTX-HSA nanoparticles was the adsorption method, and further studies were carried out using nanoparticles prepared using this method.
3.2. Radiolabeling of Nanoparticles
In this study, the [
99mTc]Tc radionuclide, reduced to a lower oxidation valency by a reductant agent, was used for radiolabeling the nanoparticles using the direct radiolabeling approach. Using this methodology, a [
99mTc=O]
3+ core was formed. The geometry of the Tc=O complex is square pyramidal, with the -yl oxygen at the apex and [
99mTc]Tc in the +4/+5-oxidation state. The square pyramid’s base comprises four ligands coordinating with this core [
60].
Figure 2 illustrates the impact of different stannous chloride concentrations on the RCP of nanoparticles. As the system’s pH (pH 7.4) remained constant, stannous chloride was added in amounts ranging from 0.01 to 0.1 mg × mL
−1 to reduce [
99mTc]Tc from +7 to +4/+5 valency. When 0.01 and 0.025 mg × mL
−1 of stannous chloride were added, the RCP of the nanoparticles was above 90%. However, when 0.050 mg × mL
−1 of stannous chloride was utilized, the RCP increased considerably to >99% (
p < 0.05). The RCP was unaffected by a subsequent increase in stannous chloride concentration (0.1 mg × mL
−1) (
p > 0.05).
[
99mTc]Tc is the most commonly used radionuclide in radiolabeled nanostructured drug delivery systems. For radiolabeling of [
99mTc]Tc, the reductant agent (type and concentration) was the most important factor. Colloids form in the radiolabeling area when the amount of reducing agent is high, which lowers RCP. In contrast, free [
99mTc]Tc was detected in the radiolabeled area when lower doses of the reducing agent were applied. The RCP of the system was considerably affected in both situations. Most stannous salts are reductant agents in radiolabeling studies [
60]. In this study, stannous chloride was used as a reductant agent for nanoparticles. The optimal concentration of stannous chloride was determined to be 0.05 mg × mL
−1 after evaluating the effects of changing the amount of the reducing agent. In addition, 90–95% of RCP was achieved using 0.01–0.025 mg × mL
−1 stannous chloride. The RCP of the system was unaffected by the successive addition of increasing quantities of reducing agents (
p > 0.05). The reason for utilizing 0.05 mg × mL
−1 of stannous chloride was based on general radiopharmacy fundamentals. Therefore, the lowest possible excipient concentration (stoichiometry) was chosen to guarantee adequate stability. The nanoparticles were incubated at 37 MBq [
99mTc]Tc for 6 h. The loaded amount of [
99mTc]Tc in nanoparticles with 0.05 mg × mL
−1 of stannous chloride was 36.12 ± 0.02 MBq. Our results suggested that 99% of [
99mTc]Tc added to the nanoparticles was loaded into the nanoparticles [
61,
62].
Quality radiopharmaceuticals can be controlled using R-UPLC, RTLC, and/or gas chromatography [
63]. A rapid and safe RTLC technique was used to test the labeling effectiveness of [
99mTc]Tc-nanoparticles. During [
99mTc]Tc labeling, three products were formed: [
99mTc]Tc-nanoparticles, [
99mTc]NaTcO
4, and radiocolloids. To ascertain the proportion of [
99mTc]NaTcO
4 that migrated to the solvent front (R
f = 1.0), while [
99mTc]Tc-nanoparticles and colloids remained at the origin (R
f = 0.0), acetone was employed as the mobile phase, and Whatman 3MM paper was used as the stationary phase. The proportion of radiocolloids that remained at the origin (R
f = 0.0) and migrated to the solvent front (R
f = 1.0) was determined using a different developing solvent that contained the PAW solution (3:5:1.5). Under these conditions, the RCP of all [
99mTc]Tc-nanoparticles was greater than 99% (
p < 0.05). This result was compatible with that of Jain et al. [
54], who developed [
99mTc]Tc-MTX-has nanoparticle formulations with 98% labeling efficiency using 0.01 mg stannous chloride.
The stability of [
99mTc]Tc-labeled nanoparticles was evaluated in saline, serum, and cell media (
Figure 3). These parameters were selected to provide information about using [
99mTc]Tc-nanoparticles in an internal environment and in vitro storage [
64]. As [
99mTc]NaTcO
4 was eluted from the [
99Mo]Mo/[
99mTc]Tc-generator using saline, [99mTc]Tc-nanoparticles must remain stable in saline. All [
99mTc]Tc-nanoparticles were stable in saline, with a high labeling efficiency (>90%) (
Figure 3).
The stability of nano-radiopharmaceuticals plays a pivotal role in determining their potential clinical application as effective diagnostic or therapeutic agents. The stability of these nanoparticles directly affects their safety, reliability, and performance in a clinical setting. Regarding pharmacokinetics and biodistribution, stability influences how nano-radiopharmaceuticals behave in the body. For instance, unstable nanoparticles can release the radioactive payload prematurely, leading to altered pharmacokinetics and biodistribution, resulting in suboptimal targeting, reduced efficacy, and potentially increased radiation exposure to healthy tissues. Also, if nanoparticles release radioactive isotopes prematurely, it could expose healthy tissues and organs to unnecessary radiation. Moreover, unstable nanoparticles might accumulate radioactive materials in unintended sites, increasing the potential for off-target effects and toxicity. Finally, stability critically influences regulatory approval since regulatory agencies worldwide require extensive characterization of nano-radiopharmaceuticals, including stability studies, to ensure their safety, efficacy, and consistent performance [
65,
66,
67].
When used as a tumor imaging agent and delivered in vivo, [
99mTc]Tc-nanoparticles must retain their stability throughout the study to accurately interpret the biodistribution and imaging results [
68]. Regarding this, it was discovered that the [
99mTc]Tc-nanoparticles were stable in serum and had high labeling effectiveness (>87%), remaining stable for 6 h (
p < 0.05) (
Figure 3).
In addition, radiolabeled nanoparticle formulations were incubated with a cell medium for 2 h. The RCP of [
99mTc]Tc nanoparticles in the medium was stable, with >96% RCP (
p < 0.05) (
Figure 3). Therefore, our radiolabeled nanoparticle formulations ([
99mTc]Tc-HSA, [
99mTc]Tc-MTX-HSA, and [
99mTc]Tc-TRZ-MTX-HSA-1 nanoparticles) were suitable for cell incorporation studies.
3.3. Cell Culture Studies: Cytotoxicity and Cell Binding
The cytotoxicity of HSA, MTX-HSA, and TRZ-MTX-HSA-1 nanoparticle formulations in MCF-7, 4T1, and MCF-10A cells was determined by evaluating cell viability using an MTT assay. The cell viability was higher than 80% for all nanoparticle formulations (
Figure 4).
The choice of cell lines for cytotoxicity studies in cancer research is critical to assessing a therapeutic agent’s potential effectiveness and selectivity against specific cancer types while considering its impact on healthy cells. In our case, the cell lines MCF-7, 4T1, and MCF-10A have been selected, and each has its rationales based on their characteristics and relevance to the study.
The MCF-7 is a well-established breast cancer cell line from the human mammary gland adenocarcinoma. It is often used in research related to breast cancer therapeutics due to the expression of estrogen and progesterone receptors, making them a model for hormone receptor-positive breast cancer. Also, these cells have low levels of HER2 expression, making them a suitable model for HER2-negative breast cancer [
69,
70].
The 4T1 is a murine mammary carcinoma cell line used in breast cancer research involving animal models. Its selection is based on the aggressive and metastatic behavior of these cells in mice, closely resembling the invasive characteristics of human breast cancer, making 4T1 an appropriate model for evaluating therapies targeting metastatic breast cancer [
71,
72,
73].
Finally, the MCF-10A is an immortalized, non-transformed, human mammary epithelial cell line. It serves as a model for healthy breast tissue and is selected for control and safety assessment purposes [
74,
75].
In summary, the choice of MCF-7, 4T1, and MCF-10A cell lines for cytotoxicity studies is driven by the desire to evaluate the therapy’s efficacy against breast cancer, especially in hormone receptor-positive and metastatic contexts while also assessing its safety and potential impact on healthy cells. These cell lines provide valuable insights into the therapy’s potential clinical applications and limitations.
Owing to the MTX and TRZ contents, MTX-HSA and TRZ-MTX-HSA-1 nanoparticle formulations had a slightly higher cytotoxic effect than HSA nanoparticles, but this difference was not statistically significant (
p > 0.05). This outcome indicates that the biocompatibility of protein- and HSA-based nanoparticle formulations prevents their toxic effects on healthy cells. In the literature, it was reported that TRZ-MTX-HSA nanoparticles did not show any cytotoxic effect on the human ovarian cancer cell line (SKOV-3), human breast cancer cell line (T-47D), or human adenocarcinoma cell line (HeLa), which is in agreement with our results [
22]. Therefore, for future in vivo studies, TRZ-MTX-HSA-based nanoparticles can be regarded as effective and safe drug delivery vehicles because of their high biocompatibility and non-toxic characteristics.
To shed light on in vivo research, cell culture studies have recently become more important for assessing the tumor-targeting affinities of radioactive molecules or systems [
76,
77]. In this study, the capacity of radiolabeled nanoparticles ([
99mTc]Tc-HSA, [
99mTc]Tc-MTX-HSA, and [
99mTc]Tc-TRZ-MTX-HSA-1) to bind to MCF-7, 4T1, and MCF-10A cells was investigated. The cell-binding test was performed for 2 h, owing to the available half-life of [
99mTc]Tc. The cell binding (%) to MCF-7, 4T1, and MCF-10A cell lines of [
99mTc]Tc-labeled nanoparticles and R/H-[
99mTc]NaTcO
4 (as a control group) are shown in
Table 6.
The radiolabeled complex’s high target/non-target ratio enables the acquisition of high-quality images and prevents radiation damage to non-target tissues. Low target/non-target ratios can harm tissues in non-targeting organs and degrade target organ imaging by localization [
78]. As shown in
Table 6, [
99mTc]Tc-TRZ-MTX-HSA-1 nanoparticles had greater cell binding activity in MCF-7 cells than [
99mTc]Tc-HSA, [
99mTc]Tc-MTX-HSA nanoparticles, and R/H-[
99mTc]NaTcO
4 during the experimental period. The cell binding percentage of [
99mTc]Tc-TRZ-MTX-HSA-1 nanoparticles in MCF-7 cells ranged from 95.21 ± 3.25% at 30 min to 97.54 ± 2.16% at 120 min. At the same time, the cell binding percentages of [
99mTc]Tc-HSA and [
99mTc]Tc-MTX-HSA nanoparticles in MCF-7 cells were found to be 60.78 ± 2.34–73.24 ± 3.49% and 81.56 ± 2.64–85.12 ± 2.46%, respectively. These findings suggest that the [
99mTc]Tc-TRZ-MTX-HSA-1 nanoparticle formulations increased cellular uptake compared with [
99mTc]Tc-HSA and [
99mTc]Tc-MTX-HSA nanoparticles because of the TRZ content. In addition, the cell binding (%) of [
99mTc]Tc-TRZ-MTX-HSA-1 nanoparticles was found to be significantly higher than that of the other formulations owing to the targeting ability of TRZ in MCF-7 and 4T1 cell lines (
p < 0.05) and was found to have a 3-fold higher uptake in cancer cells than in healthy cells. Cell binding (%) in MCF-10A cells did not differ significantly between the formulations (
p > 0.05).
Also, the cell binding (%) of R/H-[
99mTc]NaTcO
4 ranged from 20.36 ± 2.56% at 30 min to 24.68 ± 1.56% at 120 min in MCF-7 cells. This finding proves that our labeled nanoparticle formulations behaved differently in cell medium than R/H-[
99mTc]NaTcO
4 and supported the high labeling efficiency and in vitro stability (
Table 6).