1. Introduction
Malignant melanoma is an aggressive tumor that mostly arises on the skin. The incidence of this disease is increasing worldwide [
1,
2]. Clinical application of targeted therapy (BRAF inhibitors with or without MEK inhibitors) and immunotherapy (PD-1 inhibitors and CTLA-4 inhibitors) improve the survival of patients with unresectable melanoma, but the principal therapy for localized melanoma is surgical eradication [
3,
4]. To achieve complete excision of primary melanoma, wide-margin excision (e.g., 5 cm around the tumor) has historically been performed [
5,
6,
7]. However, extensive excision inevitably involves unnecessary removal of normal tissue, causing large skin defects. In such cases, skin grafting or skin flaps, rather than simple suturing, may be needed to close the defects. Many randomized controlled studies have been conducted to explore appropriate surgical margins for melanoma [
5,
8,
9,
10,
11,
12]. A large randomized controlled study (
n = 936) found no significant differences in either overall survival or recurrence-free survival between patients with thick melanoma (>4 mm) who underwent resections with 2-cm or 4-cm margins [
12]. Another large randomized controlled study compared the overall survival between patients undergoing 1-cm and 3-cm resections. Although the 1-cm excision group had a higher risk of locoregional recurrence, overall survival was similar to the 3-cm excision group [
11]. The latest National Comprehensive Cancer Network (NCCN) guidelines recommend surgical margins according to Breslow thickness of the primary melanoma: 5 mm for in situ melanoma, 10 mm for T1 melanoma, 10–20 mm for T2 melanoma, and 20 mm for T3 and T4 melanoma [
3].
Acral melanoma is a type of cutaneous melanoma that occurs on the glabrous skin of the palms, soles, and nail beds. It has a unique genetic background compared to other types of melanoma [
13,
14]. Histopathologically, most acral melanomas are of the acral lentiginous subtype, characterized by the lentiginous spread of melanoma cells in the basal layer of the epidermis [
15,
16]. Acral melanoma may show a relatively small nodule surrounded by a wide spreading in-situ macule (
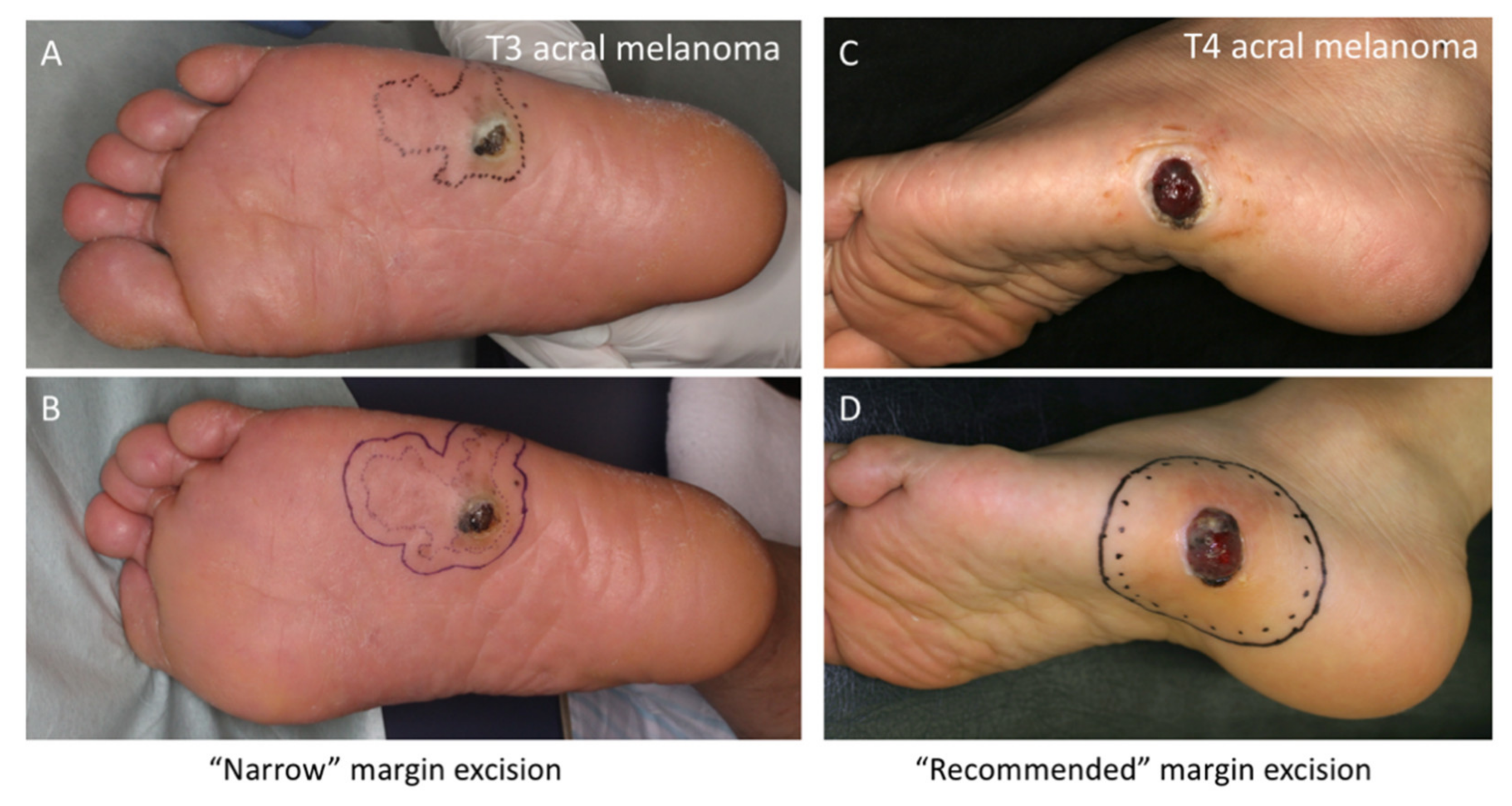
Figure 1).
Sufficient surgical margins for acral melanomas may not always be feasible due to anatomical constraints. Extensive excision for melanoma in the nail beds causes amputation at more proximal sites. For melanoma of the soles or palms, reconstruction requires wider skin grafting in weight-bearing areas, leading to long-lasting pain. When designing the surgical resection line for acral melanoma, the question is: How far away from the surrounding (seemingly) in situ macule should the resection line be? Theoretically, melanoma cells in situ are restricted within the epidermis and do not metastasize.
Figure 2A shows a typical case of T3 acral melanoma with a wide spreading in situ area. Although the ideal resection line is 2 cm away from the in-situ area, such wide excision could be an overtreatment. In this case, we excised with a final margin of 1 cm around the surrounding macule (0.5 cm at the time of excision biopsy, as shown in
Figure 2B, and an additional 0.5 cm at the time of reconstruction). Although the final margin was 1 cm away from the macule, it was 2 cm away from the nodule. This resection appears to be appropriate, and we have sometimes chosen this kind of narrow-margin excision for acral melanoma after in-depth discussion with patients. However, another question arises: Are narrow-margin excisions warranted? For comparison,
Figure 2C,D shows a case in which the acral melanoma was excised with recommended surgical margins from the macule. In this article, we summarize our 18 years of experience treating acral melanomas and analyze the outcomes of narrow-margin excisions. One hundred patients with invasive acral melanoma and long-term follow-up are included.
4. Discussion
This retrospective study aimed to investigate whether the acral melanoma excisions we performed using narrow resection margins yielded results comparable to those we performed using recommended resection margins in terms of local recurrence and patient survival. Our findings were unexpected.
We observed considerably good primary disease control. Only three of 100 patients (3.0%) had tumor-positive margins regardless of resection with narrow (one patient) or recommended (two patients) margins. One patient underwent re-excision, but the other two did not due to advanced age; none experienced any local recurrence or distant metastasis. During the follow-up period, local recurrence occurred in only two patients (2.0%), who were both in the N-group. These results imply no remarkable impact on primary disease control between narrow and recommended margin excision.
In contrast to the good primary disease control, 19 patients (20.0%) died of melanoma among the 95 patients with stage I–III diseases. In the Kaplan–Meier survival curves for these patients, N-group patients had a significantly shorter MSS and DFS than R-group patients. This result should be interpreted with caution, however, because patients in the N-group had significantly thicker acral melanomas. Most death events occurred among T4 acral melanoma patients (78.9% of melanoma deaths, 15/19), and patients with T1–3 melanoma had relatively good prognoses. For patients with T1–3 melanoma, the mortality rate of the N-group was 1.36 per 100 person-years, and that of the R-group was 1.28 per 100 person-years, showing similar rates in the two group. For patients with T4 melanoma, the mortality rate of the N-group was 11.44 per 100 person-years, and that of the R-group was 5.03 per 100 person-years, suggesting a higher risk in the N-group. Interestingly, when adjusted by Breslow thickness in multivariate analyses, narrow-margin excision was not a significant prognostic factor either for MSS or DFS (p = 0.3836 and p = 0.3092, respectively).
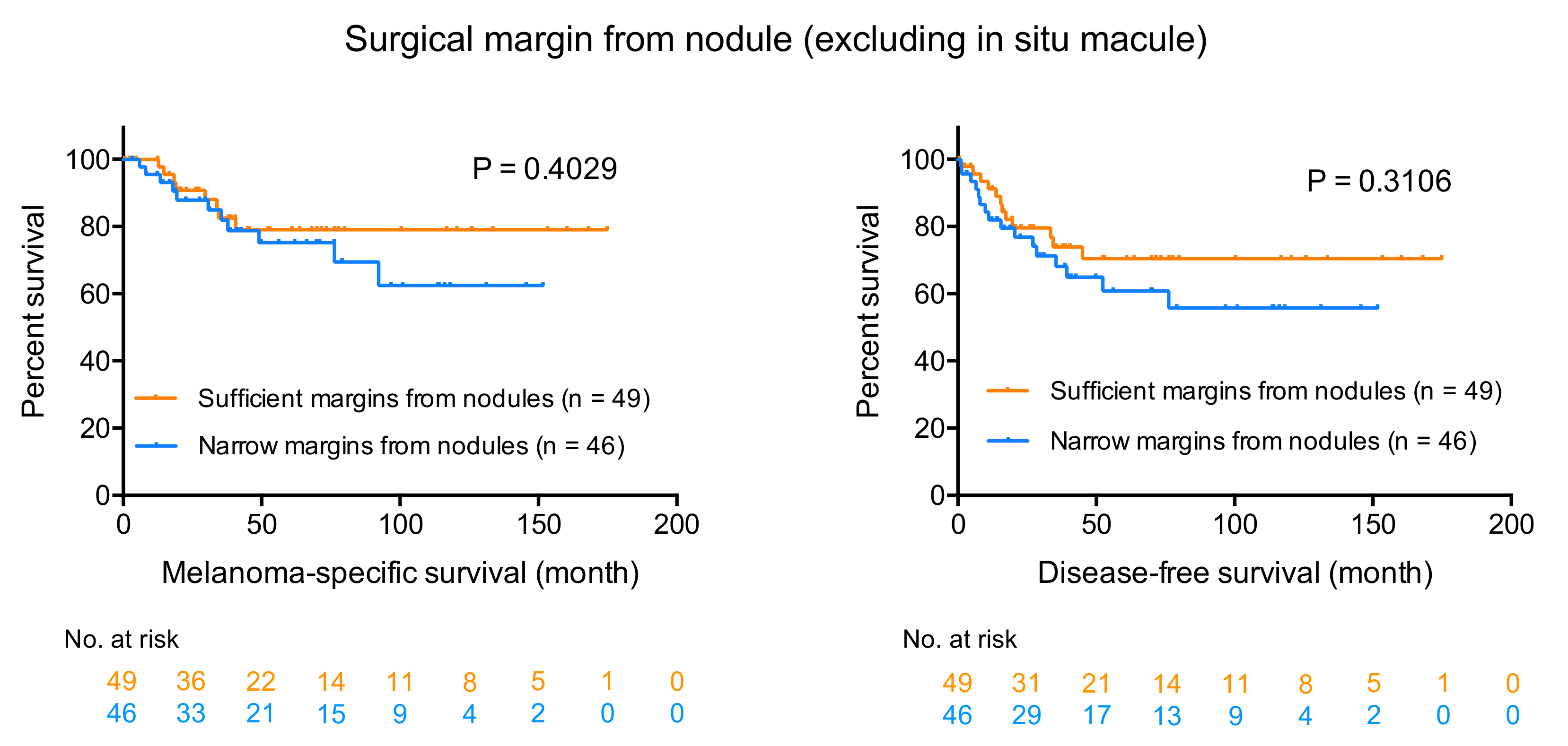
The results of the analyses on the surgical margins from nodules are also interesting and unexpected. Amazingly, the narrow-margin excision from nodules did not statistically impair MSS or DFS compared to the sufficient-margin excision from nodules. Multivariate analyses also revealed no statistical significance between the narrow and sufficient excision from nodules on MSS or DFS (p = 0.5962 and p = 0.6087, respectively).
These findings may suggest that treatments to control primary disease could be considered separately from those to prevent distant metastases and subsequent fatal events. In the current study, positive surgical margins were observed only in three patients and local recurrence only in two patients. Interpretation of the results on the survival is, however, more complicated and challenging. For thinner acral melanomas (T1–3), the mortality rates of the N- and R-groups were similar. The possibility still remains that narrow-margin excision does not affect patient survival, but there is no evidence at this time that narrow-margin excision is safe. For T4 acral melanoma, prognosis of the patients is generally worse. The fact that sufficient surgical margins from nodules did not improve patient survival might imply the limitation of the surgical treatment alone for T4 acral melanoma. Meanwhile, five patients whose melanomas were resected with sufficient margins both from nodules and macules showed relatively good survival. A meta-analysis in 2016 [
21] that integrated six randomized controlled trials [
5,
8,
9,
10,
11,
12] warns about the potential risk of narrow margin excision for melanoma, providing evidence that 1–2-cm margins may lead to poorer outcomes than 3–5-cm margins. We cannot currently judge whether removal of all local micrometastases in the vicinity of the primary tumor achieved by wide resection led to the better survival outcomes of the five patients because the number of patients is too small. After all, we still do not have enough evidence that warrants narrow-margin excision, and margins following current guidelines would be preferred for curative purpose. In cases with wide in situ macules, optimal surgical margins from nodules and macules may be decided for individual patient. A clinical trial comparing narrow margins (1 cm vs. 2 cm) is ongoing (NCT01457157) and the results of this trial will provide further insights into appropriate surgical margins.
Besides the bias inherent in a retrospective study and the relatively small sample size, one limitation of this study is that dermatologic surgeons determined the surgical margins according to anatomical constraints or patients’ general conditions and wishes. Thus, the rules of the choice of resection margins were inconsistent. Furthermore, in some cases of the narrow-margin excision, surgeons could be less concerned about margins because they considered that a prognosis was going to be poor. All of these factors may have caused uncontrolled bias.
In conclusion, although we could not find a difference between the narrow-margin excision and recommended-margin excision in this study, we suggest following the current recommendations of guidelines. Our study warrants the prospective collection of data on acral melanoma to better define the prognosis of this infrequent type of melanoma.