Comprehensive Evaluation of the Biological Properties of Surface-Modified Titanium Alloy Implants
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Modification of the Ti6Al4V Implant Surface and the Characterization of Titania Coatings
2.2. Wettability and Surface Free Energy of Biomaterials
2.3. Immunological Assessment
2.3.1. Cell Culture
2.3.2. Cell Proliferation Assays
2.3.3. MG-63 Osteoblasts Morphology Observed by SEM
2.3.4. Alkaline Phosphatase Activity Assay
2.3.5. ELISA Quantification of Cytokines and Nitric Oxide
2.4. Genotoxicity Assessment
2.5. Microbiological Assessment
2.5.1. Microbial Strains and Growth Conditions
2.5.2. Anti-Adhesive and Anti-Biofilm Properties of Titanium Surfaces Tested
2.5.3. Antimicrobial Activity of the Titanium Sample-Derived Supernatants
2.6. AFM Topography and Mechanical Properties Studies
2.7. Statistical Analysis in the Biological Assays
3. Results
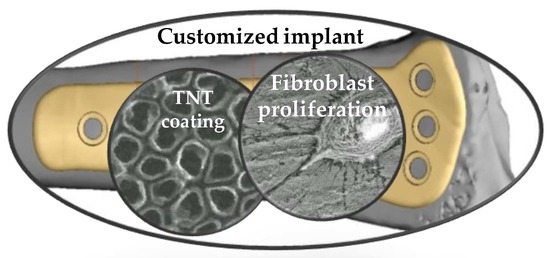
3.1. Ti6Al4V Implants Modified by Titania Nanotube Coatings
3.2. Wettability and Surface Free Energy of Biomaterials
3.3. Immunological Assessment
3.3.1. Cell Proliferation Detected by the MTT Assay
3.3.2. Morphology and Proliferation Rate of MG-63 Osteoblasts Observed by Scanning Electron Microscopy
3.3.3. Alkaline Phosphatase Activity of MG-63 Cells
3.3.4. Secretion of Cytokines and Nitric Oxide by RAW 264.7 Macrophages
3.4. Genotoxicity Assessment
3.5. Microbiological Assessment
3.6. AFM Topography and Nanomechanical Properties Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000 2017, 73, 7–21. [Google Scholar] [CrossRef]
- Scholz, M.-S.; Blanchfield, J.P.; Bloom, L.D.; Coburn, B.H.; Elkington, M.; Fuller, J.D.; Gilbert, M.E.; Muflahi, S.A.; Pernice, M.F.; Rae, S.I.; et al. The use of composite materials in modern orthopaedic medicine and prosthetic devices: A review. Compos. Sci. Technol. 2011, 71, 1791–1803. [Google Scholar] [CrossRef]
- Cronskär, M.; Lars-Erik Rännar, L.-E.; Bäckström, M. Implementation of Digital Design and Solid Free-Form Fabrication for Customization of Implants in Trauma Orthopaedics. J. Med. Biol. Eng. 2010, 32, 91–96. [Google Scholar] [CrossRef]
- Lim, K.M.; Park, J.W.; Park, S.J.; Kang, H.K. 3D-Printed Personalized Titanium Implant Design,Manufacturing and Verification for Bone Tumor Surgery of Forearm. Biomed. J. Sci. Tech. 2018, 10. [Google Scholar] [CrossRef] [Green Version]
- Manić, M.; Stamenković, Z.; Mitković, M.; Stojković, M.; Shepherd, D.E.T. Design of 3D Model of Customized Anatomically Adjusted Implants. Facta Univ. Ser. Mech. Eng. 2015, 13, 269–282. [Google Scholar]
- Pilliar, R.M. Metallic Biomaterials. In Biomedical Materials; Narayan, R.C., Ed.; Springer Science+Business Media, LLC: Berlin/Heidelberg, Germany, 2009; Volume 2, pp. 41–81. [Google Scholar] [CrossRef]
- Wang, D.; Wang, Y.; Wu, S.; Lin, H.; Yang, Y.; Fan, S.; Gu, C.; Wang, J.; Song, C. Customized a Ti6Al4V Bone Plate for Complex Pelvic Fracture by Selective Laser Melting. Materials 2017, 10, 35. [Google Scholar] [CrossRef]
- Moiduddin, K.; Mian, S.H.; Umer, U.; Alkhalefah, H. Fabrication and Analysis of a Ti6Al4V Implant for Cranial Restoration. Appl. Sci. 2019, 9, 2513. [Google Scholar] [CrossRef] [Green Version]
- Xue, W.; Krishna, B.V.; Bandyopadhyay, A.; Bose, S. Processing and biocompatibility evaluation of laser proceeded porous titanium. Acta Biomater. 2007, 3, 1007–1018. [Google Scholar] [CrossRef]
- Sarker, A.; Tran, N.; Rifai, A.; Brandt, M.; Tran, P.A.; Leary, M.; Fox, K.; Williams, R. Rational design of additively manufactured Ti6Al4V implants to control Staphylococcus aureus biofilm formation. Materialia 2019, 5, 100250. [Google Scholar] [CrossRef]
- Chu, T.G.; Khouja, N.; Chahine, G.; Kovacevic, R.; Koike, M.; Okabe, T. In vivo Evaluation of a Novel Custom-Made press-Fit Dental Implant Through Electron Beam Melting® (EBM®). Int. J. Dent. Oral Sci. 2016, 3, 358–365. [Google Scholar]
- Minagar, S.; Wang, J.; Bernt, C.C.; Ivanova, E.P.; Wen, C. Cell response of anodized nanotubes on titanium and titanium alloys. J. Biomed. Mater. Res. A 2013, 101A, 2726–2739. [Google Scholar] [CrossRef]
- Radtke, A. Photocatalytic Activity of Titania Nanotube Coatings Enriched With Nanohydroxyapatite. Biomed. J. Sci. Tech. Res. 2019, 15. [Google Scholar] [CrossRef]
- Li, X.; Gao, P.; Wan, P.; Pei, Y.; Shi, L.; Fan, B.; Shen, C.; Xiao, X.; Yang, K.; Guo, Z. Novel Bio-functional Magnesium Coating on Porous Ti6Al4V Orthopaedic Implants: In vitro and In vivo Study. Sci. Rep. 2017, 7, 40755. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godoy-Gallardo, M.; Rodríguez-Hernández, A.G.; Delgado, L.M.; Manero, J.M.; Gil, F.J.; Rodríguez, D. Silver deposition on titanium surface by electrochemical anodizing process reduces bacterial adhesion of Streptococcus sanguinis and Lactabacillus salivarius. Clin. Oral Impl. Res. 2015, 26, 1170–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piszczek, P.; Radtke, A. Silver Nanoparticles Fabricated Using Chemical Vapor Deposition and Atomic Layer Deposition Techniques: Properties, Applications and Perspectives: Review. In Noble and Precious Metals; Seehra, M.S., Bristow, A.D., Eds.; IntechOpen: London, UK, 2018; pp. 187–213. [Google Scholar]
- Kasemo, B.; Lausmaa, J. Biomaterial and implant surfaces: A surface science approach. Int. J. Oral Maxillofac. Implant. 1988, 3, 247–259. [Google Scholar]
- Takebe, J.; Itoh, S.; Okada, J.; Ishibashi, K. Anodic oxidation and hydrothermal treatment of titanium results in a surface that causes increased attachment and altered cytoskeletal morphology of rat bone marrow stromal cells in vitro. J. Biomed. Mater. Res. 2000, 51, 398–407. [Google Scholar] [CrossRef]
- Dzhurinskiy, D. Bioactive antimicrobial coatings for implantable medical devices formed by plasma electrolytic oxidation. Met. Form. 2018, 29, 65–76. [Google Scholar]
- Radtke, A.; Topolski, A.; Jedrzejewski, T.; Kozak, W.; Sadowska, B.; Wieckowska-Szakiel, M.; Piszczek, P. Bioactivity Studies on Titania Coatings and the Estimation of Their Usefulness in the Modification of Implant Surfaces. Nanomaterials 2017, 4, 90. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A.; Bal, M.; Jędrzejewski, T. Novel titania nanocoatings produced by the anodic anodization with the use of the cyclically changing potential; their photocatalytic activity and biocompability. Nanomaterials 2018, 8, 712. [Google Scholar] [CrossRef] [Green Version]
- Gong, D.; Grimes, C.A.; Varghese, O.K.; Hu, W.; Singh, R.S.; Chen, Z.; Dickey, E.C. Titanium oxide nanotube arrays prepared by anodic oxidation. J. Mater. Res. 2001, 16, 3331–3334. [Google Scholar] [CrossRef] [Green Version]
- Macak, J.M.; Tsuchiya, H.; Ghicov, A.; Yasuda, K.; Hahn, R.; Bauer, S.; Schmuki, P. TiO2 nanotubes: Self-organized electrochemical formation, properties and applications. Curr. Opin. Solid State Mater. Sci. 2007, 11, 3–18. [Google Scholar] [CrossRef]
- Lewandowska, Ż.; Piszczek, P.; Radtke, A.; Jędrzejewski, T.; Kozak, W.; Sadowska, B. The Evaluation of the Impact of Titania Nanotube Covers Morphology and Crystal Phase on Their Biological Properties. J. Mater. Sci. Mater. Med. 2015, 26, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radtke, A.; Topolski, A.; Jędrzejewski, T.; Sadowska, B.; Więckowska-Szakiel, M.; Szubka, M.; Talik, E.; Nielsen, L.P.; Piszczek, P. Studies on the bioactivity and photocatalytic properties of titania nanotube coatings produced with the use of the low potential anodization of Ti6Al4V alloy surface. Nanomaterials 2017, 7, 197. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A.; Ehlert, M.; Bartmański, M.; Jędrzejewski, T. The morphology, structure, mechanical properties and biocompatibility of nanotubular titania coatings before and after autoclaving process. J. Clin. Med. 2019, 8, 272. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A.; Jędrzejewski, T.; Kozak, W.; Sadowska, B.; Więckowska-Szakiel, M.; Talik, E.; Mäkelä, M.; Leskelä, M.; Piszczek, P. Optimization of the silver clusters PEALD process on the surface of 1-D titania coatings. Nanomaterials 2017, 7, 193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piszczek, P.; Lewandowska, Ż.; Radtke, A.; Jędrzejewski, T.; Kozak, W.; Sadowska, B.; Szubka, M.; Talik, E.; Fiori, F. Biocompatibility of Titania Nanotube Coatings Enriched with Silver Nanograins by Chemical Vapor Depositiom. Nanomaterials 2017, 7, 274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radtke, A.; Grodzicka, M.; Ehlert, M.; Muzioł, T.; Szkodo, M.; Bartmański, M.; Piszczek, P. Studies on silver ions releasing processes and mechanical properties of surface-modificated titanium alloy implants, International Journal of Molecular Science. Int. J. Mol. Sci. 2018, 19, 3962. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A.; Grodzicka, M.; Ehlert, M.; Ję, *!!! REPLACE !!!*; drzejewski, T.; Wypij, M.; Goliń, *!!! REPLACE !!!*; ska, P. “To Be Microbiocidal and Not to be Cytotoxic at the Same Time.”-Silver Nanoparticles in Their Main Role on the Surface of the Titania Alloy Implant. J. Clin. Med. 2019, 8, 334. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A. 1D Titania Nanoarchitecture as Bioactive and Photoactive Coatingas for Modern Implants: A Review. In Application of Titanium Dioxide; Janus, M., Ed.; InTech: Croatia, 2017; pp. 73–102. [Google Scholar]
- Sonntag, R.; Reinders, J.; Gibmeier, J.; Kretzer, J.P. Fatigue Performance of Medical Ti6Al4V Alloy after Mechanical Surface Treatments. PLoS ONE 2015, 10, e0121963. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Y.; Lee, T.R. Chapter 1 Contact Angle and Wetting Properties. In Surface Science Techniques, Springer Series in Surface Sciences; Bracco, G., Holst, B., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 3–34. [Google Scholar] [CrossRef]
- Flückiger-Isler, S.; Kamber, M. Direct comparison of the Ames microplate format (MPF) test in liquid medium with the standard Ames pre-incubation assay on agar plates by use of equivocal to weakly positive test compounds. Mutat. Res. Toxicol. Environ. Mutagen 2012, 747, 36–45. [Google Scholar] [CrossRef]
- Leyland, A.; Matthews, A. Design criteria for wear-resistant nanostructured and glassy-metal coatings. Surf. Coat. Technol. 2004, 177–178, 317–324. [Google Scholar] [CrossRef]
- Oliver, W.C.; Pharr, G.M. An improved technique for determining hardness and elastic modulus using load and displacement sensing indentation experiments. J. Mater. Res. 1992, 7, 1564–1583. [Google Scholar] [CrossRef]
- Atuchin, V.V.; Kesler, V.G.; Pervukhina, N.V.; Zhang, Z. Ti 2p and O 1s core levels and chemical bonding in titanium-bearing oxides. J. Electron Spectrosc. Relat. Phenom. 2006, 152, 18–24. [Google Scholar] [CrossRef]
- Chinh, V.D.; Broggi, A.; Di Palma, L.; Scarsella, M.; Sperenza, G.; Vilardi, G.; Thang, P.N. XPS Spectra Analysis of Ti2+, Ti3+ Ions and Dye Photodegradation Evaluation of Titania-Silica Mixed Oxide Nanoparticles. J. Phys. D Appl. Phys. 2017, 10. [Google Scholar] [CrossRef]
- Wen, H.; Dan, M.; Yang, Y.; Lyu, J.; Shao, A.; Cheng, X.; Chen, L.; Xu, L. Acute toxicity and genotoxicity of silver nanoparticle in rats. PLoS ONE 2017, 12, e0185554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Qin, T.; Ingle, T.; Yan, J.; He, W.; Yin, J.J.; Chen, T. Differential genotoxicity mechanisms of silver nanoparticles and silver ions. Arch Toxicol. 2017, 91, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Jemat, A.; Ghazali, M.J.; Razali, M.; Otsuka, Y.; Rajabi, A. Effects of TiO2 on microstructural, mechanical properties and in-vitro bioactivity of plasma sprayed yttria stabilised zirconia coatings for dental application. Ceram. Int. 2017, 44, 4271–4281. [Google Scholar] [CrossRef]
- Rayón, E.; Bonache, V.; Salvador, M.D.; Bannier, E.; Sánchez, E.; Denoirjean, A.; Ageorges, H. Nanoindentation study of the mechanical and damage behaviour of suspension plasma sprayed TiO2 coatings. Surf. Coat. Technol. 2012, 206, 2655–2660. [Google Scholar] [CrossRef]
- Wysocki, B.; Maj, P.; Sitek, R.; Buhagiar, J.; Kurzydłowski, K.J.; Święszkowski, W. Laser and Electron Beam Additive Manufacturing Methods of Fabricating Titanium Bone Implants. Appl. Sci. 2017, 7, 657. [Google Scholar] [CrossRef]
- Hiromoto, S.; Hanawa, T.; Asami, K. Composition of surface oxide film of titanium with culturing Marine fibroblast L929. Biomaterials 2004, 25, 979–986. [Google Scholar] [CrossRef]
- Brammer, K.S.; Oh, S.; Cobb, C.J.; Bjursten, L.M.; van der Heyde, H.; Jin, S. Improved bone-forming functionality on diameter-controlled TiO2 nanotube surface. Acta Biomater. 2009, 5, 3215–3223. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Bauer, S.; von der Mark, K.; Schmuki, P. Nanosize and vitality: TiO2 nanotube diameter directs cell fate. Nano Lett. 2007, 7, 1686–1691. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Bauer, S.; Schlegel, K.A.; Neukam, F.W.; von der Mark, K.; Schmuki, P. TiO2 nanotube surfaces: 15 nm--an optimal length scale of surface topography for cell adhesion and differentiation. Small 2009, 5, 666–671. [Google Scholar] [CrossRef]
- Albers, C.E.; Hofstetter, W.; Siebenrock, K.A.; Landmann, R.; Klenke, F.M. In vitro cytotoxicity of silver nanoparticles on osteoblasts and osteoclasts at antibacterial concentrations. Nanotoxicology 2013, 7, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Castiglioni, S.; Cazzania, A.; Locatelli, L.; Maier, J.A.M. Silver Nanoparticles in Orthopedic Applications: New Insights on Their Effects on Osteogenic Cells. Nanomaterials (Basel) 2017, 7, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shivaram, A.; Bose, S.; Bandyopadhyay, A. Mechanical degradation of TiO2 nanotubes with and without nanoparticulate silver coating. J. Mech. Behav. Biomed. Mater. 2016, 59, 508–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, L.; Wang, H.; Huo, K.; Cui, L.; Zhang, W.; Ni, H.; Zhang, Y.; Wu, Z.; Chu, P.K. Antibacterial nano-structured titania coating incorporated with silver nanoparticles. Biomaterials 2011, 32, 5706–5716. [Google Scholar] [CrossRef]
- Esfandiari, N.; Simchi, A.; Bagheri, R. Size tuning of Ag-decorated TiO2 nanotube arrays for improved bactericidal capacity of orthopedic implants. J. Biomed. Mater. Res. A. 2014, 102, 2625–2635. [Google Scholar] [CrossRef]
- Fenton, M.J.; Golenbock, D.T. LPS-binding proteins and receptors. J. Leuk. Biol. 1998, 64, 25–32. [Google Scholar] [CrossRef]
- Netea, M.G.; Kullberg, B.J.; van der Meer, J.W. Circulating cytokines as mediators of fever. Clin. Infect. Dis. 2000, 31, S178–S184:. [Google Scholar] [CrossRef]
- Neacsu, P.; Mazare, A.; Cimpean, A.; Park, J.; Costache, M.; Schmuki, P.; Demetrescu, I. Reduced inflammatory activity of RAW 264.7 macrophages on titania nanotube modified Ti surface. Int. J. Biochem. Cell. Biol. 2014, 55, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Furuhashi, A.; Ayukawa, Y.; Atsuta, I.; Okawachi, H.; Koyano, K. The difference of fibroblast behavior on titanium substrata with different surface characteristics. Odontology 2012, 100, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.S.; Qian, L.; Rosado, R.; Flood, P.M.; Cooper, L.F. The role of titanium surface topography on J774A.1 macrophage inflammatory cytokines and nitric oxide production. Biomaterials 2006, 27, 5170–5177. [Google Scholar] [CrossRef] [PubMed]
- Dinarello, C.A. Proinflammatory cytokines. Chest 2000, 118, 503–508. [Google Scholar] [CrossRef]
- Radi, R. Nitric oxide, oxidants, and protein tyrosine nitration. Proc. Natl. Acad. Sci. USA 2004, 101, 4003–4008. [Google Scholar] [CrossRef] [Green Version]
- Mosser, D.M.; Zhang, X. Interleukin-10: new perspectives on an old cytokine. Immunol. Rev. 2008, 226, 205–218. [Google Scholar] [CrossRef]
- Ullah Khan, S.; Saleh, T.A.; Wahab, A.; Khan, M.H.U.; Khan, D.; Ullah Khan, W.; Rahim, A.; Kamal, S.; Fahad, S. Nanosilver: new ageless and versatile biomedical therapeutic scaffold. Int. J. Nanomedicine. 2018, 13, 733–762. [Google Scholar] [CrossRef] [Green Version]
- Goodman, S.B.; Ma, T. Cellular chemotaxis induced by wear particles from joint replacements. Biomaterials 2010, 31, 5045–5050. [Google Scholar] [CrossRef] [Green Version]
- Swift, L.H.; Golsteyn, R.M. Genotoxic anti-cancer agents and their relationship to DNA damage, mitosis, and checkpoint adaptation in proliferating cancer cells. Int. J. Mol. Sci. 2014, 15, 3403–3431. [Google Scholar] [CrossRef] [Green Version]
- Velasco-Ortega, E.; Jos, A.; Cameán, A.M.; Pato-Mourelo, J.; Segura-Egea, J.J. In vitro evaluation of cytotoxicity and genotoxicity of a commercial titanium alloy for dental implantology. Mutation Res. Genetic Toxicol. Environ. Mutag. 2010, 702, 17–22. [Google Scholar] [CrossRef]
- Ghosh, M.J.M.; Sinha, S.; Chakraborty, A.; Mallick, S.K.; Bandyopadhyay, M.; Mukherjee, A. In vitro and in vivo genotoxicity of silver nanoparticles. Mut. Res./Genet. Toxicol. Environ. Mutagen. 2012, 749, 60–69. [Google Scholar] [CrossRef]
- Li, Y.; Bhalli, J.A.; Ding, W.; Yan, J.; Pearce, M.G.; Sadiq, R.; Cunningham, C.K.; Jones, M.Y.; Monroe, W.A.; Howard, P.C.; et al. Cytotoxicity and genotoxicity assessment of silver nanoparticles in mouse. Nanotoxicology 2014, 8, 36–45. [Google Scholar] [CrossRef]
- Lebedová, J.; Hedberg, Y.S.; Odnevall Wallinder, I.; Karlsson, H.L. Size-dependent genotoxicity of silver, gold and platinum nanoparticles studied using the mini-gel comet assay and micronucleus scoring with flow cytometry. Mutagenesis 2018, 33, 77–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burmølle, M.; Thomsen, T.R.; Fazli, M.; Dige, I.; Christensen, L.; Homøe, P.; Tvede, M.; Nyvad, B.; Tolker-Nielsen, T.; Givskov, M.; et al. Biofilms in chronic infections - a matter of opportunity - monospecies biofilms in multispecies infections. FEMS Immunol. Med. Microbiol. 2010, 59, 324–336. [Google Scholar] [CrossRef] [Green Version]
- Høiby, N.; Bjarnsholt, T.; Givskov, M.; Molin, S.; Ciofu, O. Antibiotic resistance of bacterial biofilms. Intern. J. Antim. Agents 2010, 35, 322–332. [Google Scholar] [CrossRef] [Green Version]
- Leid, J.G.; Cope, E. Population level virulence in polymicrobial communities associated with chronic disease. Front. Biol. 2011, 6, 435–445. [Google Scholar] [CrossRef]
- Mottola, C.; Matias, C.S.; Mendes, J.J.; Melo-Cristino, J.; Tavares, L.; Cavaco-Silva, P.; Oliveira, M. Susceptibility patterns of Staphylococcus aureus biofilms in diabetic foot infections. BMC Microbiol. 2016, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Jin, J.; Zhang, L.; Shi, M.; Zhang, Y.; Wang, Q. Ti-GO-Ag nanocomposite: the effect of content level on the antimicrobial activity and cytotoxicity. Int. J. Nanomed. 2017, 12, 4209–4224. [Google Scholar] [CrossRef] [Green Version]
- Lan, M.-Y.; Liu, C.-P.; Huang, H.-H.; Lee, S.-W. Both enhanced biocompatibility and antibacterial activity in Ag-decorated TiO2 nanotubes. PLoS ONE 2013, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Liu, R.; Memarzadeh, K.; Chang, B.; Zhang, Y.; Ma, Z.; Allaker, R.P.; Ren, L.; Yang, K. Antibacterial effect of copper-bearing titanium alloy (Ti-Cu) against. Strept. Mutans Porphyrom. Gingival. Scientific Rep. 2016, 6, 29985. [Google Scholar] [CrossRef] [Green Version]
- Besinis, A.; Hadi, S.D.; Le, H.R.; Tredwin, C.; Handy, R.D. Antibacterial activity and biofilm inhibition by surface modified titanium alloy medical implants following application of silver, titanium dioxide and hydroxyapatite nanocoatings. Nanotoxicology 2017, 11, 327–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dudek, K.; Dulski, M.; Goryczka, T.; Gerle, A. Structural changes of hydroxyapatite coating electrophoretically deposited on NiTi shape memory alloy. Ceram. Int. 2018, 44, 11292–11300. [Google Scholar] [CrossRef]
- He, J.; Zhou, W.; Zhou, X.; Zhong, X.; Zhang, X.; Wan, P.; Zhu, B.; Chen, W. The anatase phase of nanotopography titania plays an important role on osteoblast cell morphology and proliferation. J. Mater. Sci. Mater. Med. 2008, 19, 3465–3472. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Soares, P.B.; Moura, C.C.G.; Claudino, M.; Carvalho, V.F.; Rocha, F.S.; Zanetta-Barbosa, D. Influence of implant surfaces on osseointegration: A histomorphometric and implant stability study in rabbits. Braz. Dent. J. 2015, 26, 451–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Wang, G.; Liang, J.; Cheng, J.; Ma, W.; Zhao, Y. Staphylococcus aureus adhesion to different implant surface coatings: An in vitro study. Surf. Coatings Technol. 2009, 203, 3454–3458. [Google Scholar] [CrossRef]
- Bahadur, J.; Agrawal, S.; Panwar, V.; Parveen, A.; Pal, K. Antibacterial properties of silver doped TiO2 nanoparticles synthesized via sol-gel technique. Macromol. Res. 2016, 24, 488–493. [Google Scholar] [CrossRef]
- Godoy-Gallardo, M.; Manzanares-Céspedes, M.C.; Sevilla, P.; Nart, J.; Manzanares, N.; Manero, J.M.; Gil, F.J.; Boyd, S.K.; Rodríguez, D. Evaluation of bone loss in antibacterial coated dental implants: An experimental study in dogs. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 1, 538–545. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.K.; Wen, H.C.; Cheng, C.H.; Hung, C.H.; Chou, W.C.; Yau, W.H.; Yang, P.F.; Lai, Y.S. Nanotribological properties of ALD-processed bilayer TiO2/ZnO films. Microelectron. Reliab. 2014, 54, 2754–2759. [Google Scholar] [CrossRef]
- Bartmanski, M.; Zielinski, A.; Majkowska-Marzec, B.; Strugala, G. Effects of solution composition and electrophoretic deposition voltage on various properties of nanohydroxyapatite coatings on the Ti13Zr13Nb alloy. Ceram. Int. 2018, 19236–19246. [Google Scholar] [CrossRef]
- Sumner, D.R.; Galante, J.O. Determinants of stress shielding: Design versus materials versus interface. Clin. Orthop. Relat. Res. 1992, 274, 202–212. [Google Scholar] [CrossRef]
- Ridzwan, M.I.Z.; Shuib, S.; Hassan, A.Y.; Shokri, A.A.; Mohammad Ibrahim, M.N. Problem of stress shielding and improvement to the hip implant designs: A review. J. Med. Sci. 2007, 7, 460–467. [Google Scholar] [CrossRef] [Green Version]
- Huiskes, R.; Weinans, H.; Van Rietbergen, B. The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin. Orthop. Relat. Res. 1992, 124–134. [Google Scholar] [CrossRef] [Green Version]
- Asgharzadeh Shirazi, H.; Ayatollahi, M.R.; Asnafi, A. To reduce the maximum stress and the stress shielding effect around a dental implant–bone interface using radial functionally graded biomaterials. Comput. Methods Biomech. Biomed. Engin. 2017, 20, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Noyama, Y.; Miura, T.; Ishimoto, T.; Itaya, T.; Niinomi, M.; Nakano, T. Bone loss and reduced bone quality of the human femur after total hip arthroplasty under stress-shielding effects by titanium-based implant. Mater. Trans. 2012, 53, 565–570. [Google Scholar] [CrossRef] [Green Version]
- Drevet, R.; Ben Jaber, N.; Fauré, J.; Tara, A.; Ben Cheikh Larbi, A.; Benhayoune, H. Electrophoretic deposition (EPD) of nano-hydroxyapatite coatings with improved mechanical properties on prosthetic Ti6Al4V substrates. Surf. Coatings Technol. 2015, 301, 94–99. [Google Scholar] [CrossRef]
- Charles, A.H. Handbook of Ceramics, Glasses, and Diamonds, Charles, A.H., Ed.; The McGraw-Hill Companies Inc.: New York, NY, USA, 2001. [CrossRef]
- Manoj Kumar, R.; Kuntal, K.K.; Singh, S.; Gupta, P.; Bhushan, B.; Gopinath, P.; Lahiri, D. Electrophoretic deposition of hydroxyapatite coating on Mg-3Zn alloy for orthopaedic application. Surf. Coatings Technol. 2016, 287, 82–92. [Google Scholar] [CrossRef]
- Bartmański, M.; Cieślik, B.; Głodowska, J.; Kalka, P. Electrophoretic deposition (EPD) of nanohydroxyapatite - nanosilver coatings on Ti13Zr13Nb alloy. Ceram. Int. 2017, 43, 11820–11829. [Google Scholar] [CrossRef]
- Chernozem, R.V.; Surmeneva, M.A.; Krause, B.; Baumbach, T.; Ignatov, V.P.; Tyurin, A.I.; Loza, K.; Epple, M.; Surmenev, R.A. Hybrid biocomposites based on titania nanotubes and a hydroxyapatite coating deposited by RF-magnetron sputtering: Surface topography, structure, and mechanical properties. Appl. Surf. Sci. 2017, 426, 229–237. [Google Scholar] [CrossRef]











| TNT5 | ||||||||
| O2− | Ti4+ | Ti3+ | Ti2+ | Ti0 | ||||
| O1s BE (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | |
| Non-sputtered | 530.2 | 458.9 | 71.3 | -- | -- | -- | -- | -- |
| First Sputter | 530.5 | 458.8 | 71.7 | 457.1 | 73.4 | 455.2 | 75.3 | -- |
| Second Sputter | 530.6 | -- | -- | -- | -- | 455.2, 454.0 | 75.4, 76.6 | 453.5 |
| Third Sputter | 530.7 | -- | -- | -- | -- | 453.9 | 76.8 | 453.4 |
| TNT15 | ||||||||
| O2− | Ti4+ | Ti3+ | Ti2+ | Ti0 | ||||
| O1s BE (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | Δ(O–Ti) (eV) | 2p3/2 BE (eV) | |
| Non-sputtered | 530.2 | 459.0 | 71.2 | 457.8 | 72.4 | -- | -- | -- |
| First Sputter | 530.4 | 458.9 | 71.5 | 457.3 | 73.1 | 455.0 | 75.4 | -- |
| Second Sputter | 530.5 | 458.9 | 71.6 | 457.1 | 73.4 | 454.8 | 75.7 | -- |
| Third Sputter | 530.5 | 458.6 | 71.9 | 456.8 | 73.7 | 454.8 | 75.7 | 453.5 |
| TNT5 | TNT15 | |||||||
|---|---|---|---|---|---|---|---|---|
| Ti4+ | Ti3+ | Ti2+ | Ti0 | Ti4+ | Ti+3 | Ti2+ | Ti0 | |
| % | ||||||||
| Non-sputtered | 100 | -- | -- | -- | 86 | 14 | -- | -- |
| First Sputter | 58 | 24 | 18 | -- | 37 | 45 | 18 | -- |
| Second Sputter | -- | -- | 12, 55 | 33 | 35 | 34 | 31 | -- |
| Third Sputter | -- | -- | 35 | 65 | 30 | 23 | 37 | 10 |
| Average Contact Angle [°] ± Standard Deviation | SFE [mJ/m2] | ||
|---|---|---|---|
| Measuring Liquid | |||
| Water | Diodomethane | ||
| Ti6Al4V | 108.3 ± 0.1 | 37.0 ± 0.2 | 45.4 ± 0.1 |
| TNT5 | 76.4 ± 1.3 | 43.2 ± 2.2 | 39.1 ± 0.7 |
| TNT15 | 62.4 ± 0.8 | 46.1 ± 0.7 | 44.08± 0.4 |
| TNT5/AgNPs | 131.9 ±0.1 | 44.8 ± 1.6 | 52.8 ± 0.6 |
| TNT15/AgNPs | 124.2 ± 0.1 | 67.3 ± 1.0 | 29.1 ± 0.2 |
| Position of Indentation | Hardness H (GPa) | Young’s Modulus E (GPa) | H/E (-) | |
|---|---|---|---|---|
| TNT5 | Area I | 0.048 ± 0.079 | 22.49 ± 64.95 | 0.0044 ± 0.0024 |
| Area II | 0.058 ± 0.105 | 8.12 ± 9.66 | 0.0063 ± 0.0049 | |
| Area I+II | 0.053 ± 0.092 | 17.00 ± 61.02 | 0.0054 ± 0.0039 | |
| TNT5/AgNPs | Area I | 0.751 ± 1.145 | 37.99 ± 48.74 | 0.0114 ± 0.0077 |
| Area II | 5.835 ± 5.720 | 168.57 ± 121.25 | 0.0266 ± 0.0135 | |
| Area I + II | 3.293 ± 4.862 | 103.28 ± 112.75 | 0.0190 ± 0.0133 |
| Nanoscratch Test Properties | ||
|---|---|---|
| Critical Force (mN) | Critical Friction Force (mN) | |
| TNT5 | 79.70 ± 33.73 | 130.77 ± 31.09 |
| TNT5/AgNPs | 173.40 ± 41.97 | 212.34 ± 66.84 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piszczek, P.; Radtke, A.; Ehlert, M.; Jędrzejewski, T.; Sznarkowska, A.; Sadowska, B.; Bartmański, M.; Erdoğan, Y.K.; Ercan, B.; Jedrzejczyk, W. Comprehensive Evaluation of the Biological Properties of Surface-Modified Titanium Alloy Implants. J. Clin. Med. 2020, 9, 342. https://doi.org/10.3390/jcm9020342
Piszczek P, Radtke A, Ehlert M, Jędrzejewski T, Sznarkowska A, Sadowska B, Bartmański M, Erdoğan YK, Ercan B, Jedrzejczyk W. Comprehensive Evaluation of the Biological Properties of Surface-Modified Titanium Alloy Implants. Journal of Clinical Medicine. 2020; 9(2):342. https://doi.org/10.3390/jcm9020342
Chicago/Turabian StylePiszczek, Piotr, Aleksandra Radtke, Michalina Ehlert, Tomasz Jędrzejewski, Alicja Sznarkowska, Beata Sadowska, Michał Bartmański, Yaşar Kemal Erdoğan, Batur Ercan, and Waldemar Jedrzejczyk. 2020. "Comprehensive Evaluation of the Biological Properties of Surface-Modified Titanium Alloy Implants" Journal of Clinical Medicine 9, no. 2: 342. https://doi.org/10.3390/jcm9020342