Artificial Intelligence vs. Natural Stupidity: Evaluating AI Readiness for the Vietnamese Medical Information System
Abstract
:1. Introduction
“My colleagues, they study artificial intelligence; me, I study natural stupidity.”—Amos Tversky (1937–1996)
2. Literature Review
2.1. Advances in AIM Since 1950s
2.2. Research and Applications of AIM in Non-Western Countries
3. Framework
4. Evaluating AI Readiness in Vietnam
4.1. Evaluating the Overall AI Readiness
4.2. Evaluating the AI Readiness in Vietnam’s Healthcare Sector
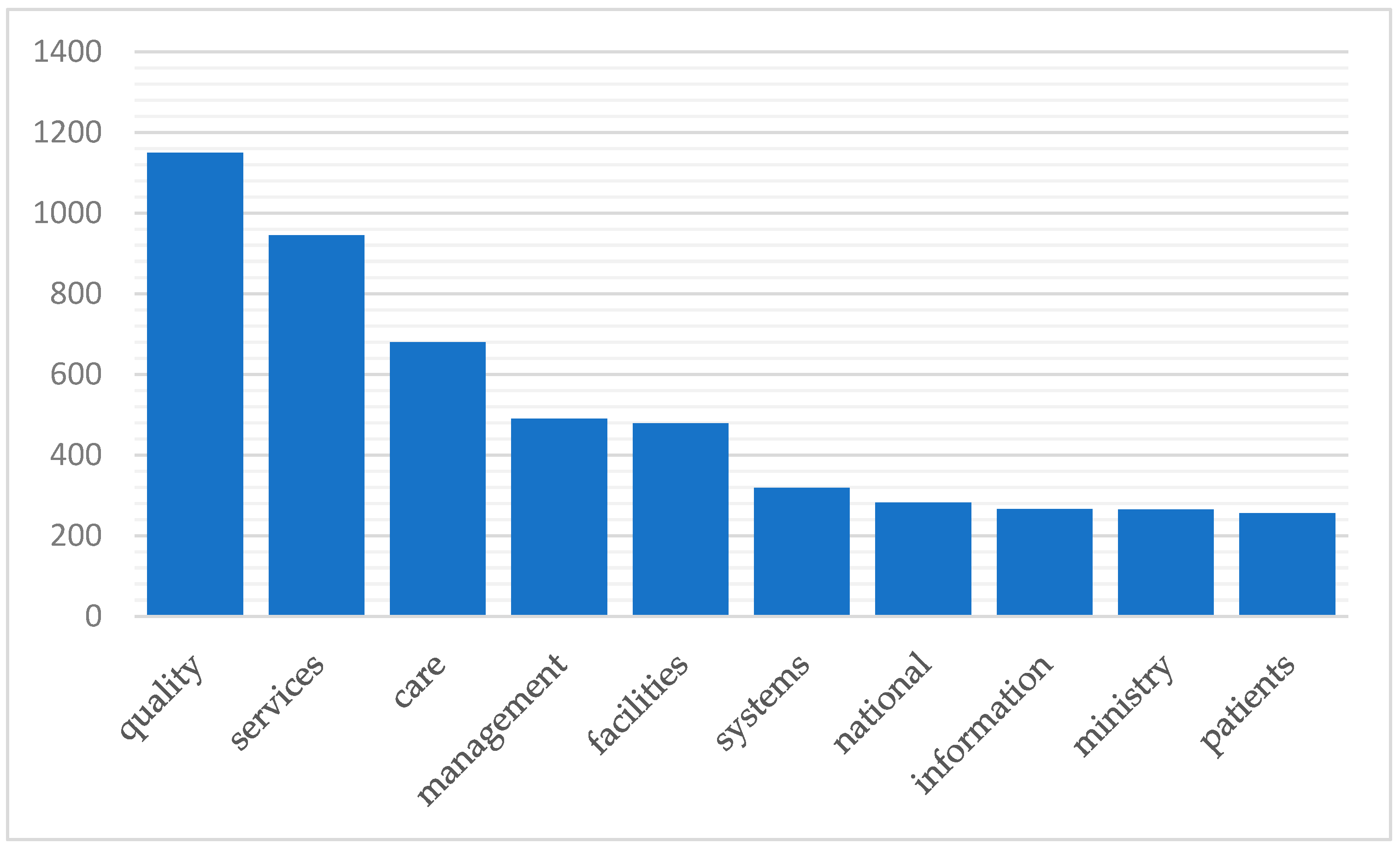
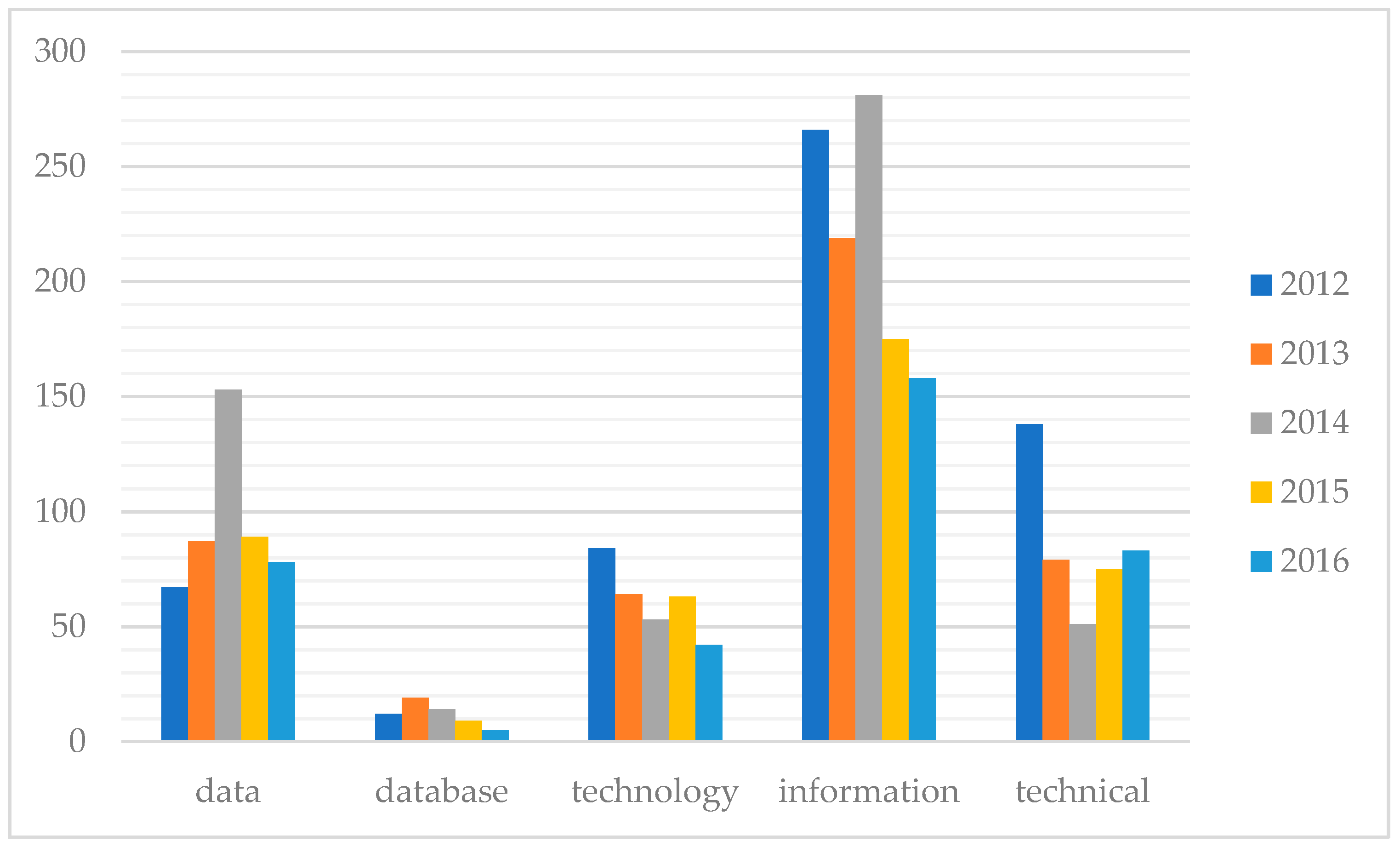
4.2.1. Research on AI in Medicine and Health in Vietnam
4.2.2. Applications of AI-Related Technology in Vietnam’s Healthcare
5. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Frankish, K.; Ramsey, W.M. Introduction. In The Cambridge Handbook of Artificial Intelligence; Frankish, K., Ramsey, W.M., Eds.; Cambridge University Press: Cambridge, UK, 2014; pp. 1–14. [Google Scholar]
- McAfee, A.; Brynjolfsson, E. Machine, Platform, Crowd: Harnessing Our Digital Future; WW Norton & Company: New York, NY, USA, 2017. [Google Scholar]
- Mayer-Schönberger, V.; Cukier, K. Big Data: A Revolution That Transforms How We Work, Live, and Think; Houghton Mifflin: Harcourt Boston, MA, USA, 2012. [Google Scholar]
- Long, E.; Lin, H.; Liu, Z.; Wu, X.; Wang, L.; Jiang, J.; An, Y.; Lin, Z.; Li, X.; Chen, J.; et al. An artificial intelligence platform for the multihospital collaborative management of congenital cataracts. Nat. Biomed. Eng. 2017, 1, 24. [Google Scholar] [CrossRef]
- Yu, K.-H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Faust, K.; Van Ommeren, R.; Sheikh, A.; Djuric, U.; Diamandis, P. Deep learning for image analysis: Personalizing medicine closer to the point of care AU—Xie, Quin. Crit. Rev. Clin. Lab. Sci. 2019, 1–13. [Google Scholar] [CrossRef]
- Begovic, M.; Oprunenco, A.; Sadiku, L. Let’s Talk about Artificial Intelligence; UNDP: New York, NY, USA, 2018; Volume 2019. [Google Scholar]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Baxter, S.L.; Xu, J.; Xu, J.; Zhou, X.; Zhang, K. The practical implementation of artificial intelligence technologies in medicine. Nat. Med. 2019, 25, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Shaban-Nejad, A.; Michalowski, M.; Buckeridge, D.L. Health intelligence: How artificial intelligence transforms population and personalized health. NPJ Dig. Med. 2018, 1, 53. [Google Scholar] [CrossRef]
- Hamet, P.; Tremblay, J. Artificial intelligence in medicine. Metabolism 2017, 69, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Mudaly, T.; Moodley, D.; Pillay, A.; Seebregts, C.J. Architectural frameworks for developing national health information systems in low and middle income countries. In Proceedings of the First International Conference on Enterprise Systems, Cape Town, South Africa, 7–8 November 2013; pp. 1–9. [Google Scholar]
- Mead, L. Global Summit Focuses on the Role of Artificial Intelligence in Advancing SDGs. Available online: http://sdg.iisd.org/news/global-summit-focuses-on-the-role-of-artificial-intelligence-in-advancing-sdgs/ (accessed on 20 November 2018).
- Wahl, B.; Cossy-Gantner, A.; Germann, S.; Schwalbe, N.R. Artificial intelligence (AI) and global health: How can AI contribute to health in resource-poor settings? BMJ Glob. Health 2018, 3, e000798. [Google Scholar] [CrossRef]
- Vuong, Q.H.; Nguyen, H.; Vuong, T.-T. Health insurance thresholds and policy implications: A Vietnamese medical survey in 2015. Biomed. Res. 2017, 26, 2432–2438. [Google Scholar]
- Vuong, Q.H.; Nguyen, T.K. Vietnamese patients’ choice of healthcare provider: In search of quality information. Int. J. Behav. Healthc. Res. 2015, 5, 184–212. [Google Scholar] [CrossRef]
- McKinsey Global Institute Study. Artificial Intelligence, the Next Digital Frontier; McKinsey Global Institute Study: New York, NY, USA, 2017. [Google Scholar]
- Allied Market Research. Artificial Intelligence in Medicine Market by Product Type (Hardware, Software, and Services), Technology (Deep Learning, Querying Method, Natural Language Processing, and Context Aware Processing), and Application (Drug Discovery & Repurposing, Clinical Research Trial, Personalized Medicine, and Others)—Global Opportunity Analysis and Industry Forecast, 2018–2025; Allied Market Research: Portland, OR, USA, 2017. [Google Scholar]
- IDC. Worldwide Spending on Cognitive and Artificial Intelligence Systems Forecast to Reach $77.6 Billion in 2022, According to New IDC Spending Guide. Available online: https://www.idc.com/getdoc.jsp?containerId=prUS44291818 (accessed on 11 December 2018).
- ReportLinker. Global AI in Healthcare Market Report for 2016–2027; ReportLinker: New York, NY, USA, 2017. [Google Scholar]
- Turing, A.M. Computing machinery and intelligence. In Parsing the Turing Test; Epstein, R., Roberts, G., Beber, G., Eds.; Springer: Dordrecht, The Netherlands, 2009; pp. 23–65. [Google Scholar]
- High, R. The Era of Cognitive Systems: An Inside Look at IBM Watson and How It Works; IBM Corporation: Armonk, NY, USA, 2012. [Google Scholar]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, A.N.; Kambhampati, C.; Monson, J.R.T.; Drew, P.J. Artificial intelligence in medicine. Ann. R. Coll. Surg. Engl. 2004, 86, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, W.B.; Patil, R.S.; Szolovits, P. Artificial intelligence in medicine. N. Engl. J. Med. 1987, 316, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.L.; Shortliffe, E.H.; Stefanelli, M.; Szolovits, P.; Berthold, M.R.; Bellazzi, R.; Abu-Hanna, A. The coming of age of artificial intelligence in medicine. Artif. Intell. Med. 2009, 46, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Shortliffe, E.H. The adolescence of AI in medicine: Will the field come of age in the ’90s? Artif. Intell. Med. 1993, 5, 93–106. [Google Scholar] [CrossRef]
- Patel, J.L.; Goyal, R.K. Applications of artificial neural networks in medical science. Curr. Clin. Pharmacol. 2007, 2, 217–226. [Google Scholar] [CrossRef]
- Schipor, O.; Geman, O.; Chiuchisan, I.; Covasa, M. From fuzzy expert system to artificial neural network: Application to assisted speech therapy. In Artificial Neural Networks: Models and Applications; Rosa, J.L.G., Ed.; IntechOpen: London, UK, 2016. [Google Scholar]
- Rumsfeld, J.S.; Joynt, K.E.; Maddox, T.M. Big data analytics to improve cardiovascular care: Promise and challenges. Nat. Rev. Cardiol. 2016, 13, 350. [Google Scholar] [CrossRef]
- Chute, C.G.; Ullman-Cullere, M.; Wood, G.M.; Lin, S.M.; He, M.; Pathak, J. Some experiences and opportunities for big data in translational research. Genet. Med. 2013, 15, 802. [Google Scholar] [CrossRef]
- Onnela, J.-P.; Rauch, S.L. Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology 2016, 41, 1691. [Google Scholar] [CrossRef]
- Frey, L.J.; Lenert, L.; Lopez-Campos, G. Ehr big data deep phenotyping. Contribution of the imia genomic medicine working group. Yearb. Med. Inform. 2014, 9, 206–211. [Google Scholar] [CrossRef]
- Denaxas, S.C.; Morley, K.I. Big biomedical data and cardiovascular disease research: Opportunities and challenges. Eur. Heart J. Qual. Care Clin. Outcomes 2015, 1, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.H. Translational bioinformatics embraces big data. Yearb. Med. Inform. 2012, 7, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Byers, S.W.; Dakshanamurthy, S. Big data: The next frontier for innovation in therapeutics and healthcare AU—Issa, Naiem T. Expert Rev. Clin. Pharmacol. 2014, 7, 293–298. [Google Scholar] [CrossRef]
- Marx, V. Human phenotyping on a population scale. Nat. Methods 2015, 12, 711. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.D.; Brown, E.W. Artificial Intelligence in Medical Practice: The Question to the Answer? Am. J. Med. 2018, 131, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Elsevier. Artificial Intelligence: How Knowledge Is Created, Transferred, and Used; Elsevier Artificial Intelligence Program: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Lee, Y.; Lee, H.-J.; Lee, H.-S.; Jang, Y.-A.; Kim, C.-I. Analytical dietary fiber database for the national health and nutrition survey in Korea. J. Food Compos. Anal. 2008, 21, S35–S42. [Google Scholar] [CrossRef]
- Valerie, T.; Choy, K.L.; Siu, P.K.Y.; Lam, H.Y.; Ho, G.T.S.; Cheng, S.W.Y. An intelligent performance assessment system for enhancing the service quality of home care nursing staff in the healthcare industry. In Proceedings of the 2016 Portland International Conference on Management of Engineering and Technology (PICMET), Honolulu, HI, USA, 4–8 September 2016; pp. 576–584. [Google Scholar]
- Woo, H.; Cho, Y.; Shim, E.; Lee, J.-K.; Lee, C.-G.; Kim, S.H. Estimating influenza outbreaks using both search engine query data and social media data in south korea. J. Med. Internet Res. 2016, 18, e177. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, H.; Xie, J.; Ally, M.S.; Hou, Z.; Xu, Y.; Zhang, Y. A novel method for evaluating the cardiotoxicity of traditional chinese medicine compatibility by using support vector machine model combined with metabonomics. Evid.-Based Complement. Altern. Med. 2016, 2016. [Google Scholar] [CrossRef]
- Lukman, S.; He, Y.; Hui, S.-C. Computational methods for traditional Chinese medicine: A survey. Comput. Methods Programs Biomed. 2007, 88, 283–294. [Google Scholar] [CrossRef]
- Meicun, Y.; Yuemei, Y.; Lu, A. Data mining and its application in the modernization of traditional chinese medicine and traditional Chinese pharmacy. J.-Beijing Univ. Tradit. Chin. Med. 2002, 25, 20–23. [Google Scholar]
- Yang, H.; Chen, J.; Tang, S.; Li, Z.; Zhen, Y.; Huang, L.; Yi, J. New drug R&D of traditional Chinese medicine: Role of data mining approaches. J. Biol. Syst. 2009, 17, 329–347. [Google Scholar]
- Zhu, J.; Ju, S.; Xin, Y. Data mining based approach to preprocessing TCM data set. Comput. Eng. 2006, 15, 098. [Google Scholar]
- Nakamura, H.; Suda, T.; Ikeda, N.; Okada, M.; Date, H.; Oda, M.; Iwasaki, A. Initial results of robot-assisted thoracoscopic surgery in Japan. Gen. Thoracic Cardiovasc. Surg. 2014, 62, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Wada, K.; Shibata, T.; Saito, T.; Sakamoto, K.; Tanie, K. Psychological and social effects of one year robot assisted activity on elderly people at a health service facility for the aged. In Proceedings of the 2005 IEEE International Conference on Robotics and Automation, Barcelona, Spain, 18–22 April 2005; pp. 2785–2790. [Google Scholar]
- Wada, K.; Shibata, T.; Saito, T.; Tanie, K. Effects of three months robot assisted activity to depression of elderly people who stay at a health service facility for the aged. In Proceedings of the SICE 2004 Annual Conference, Sapporo, Japan, 4–6 August 2004; Volume 2703, pp. 2709–2714. [Google Scholar]
- Matsusaka, Y.; Fujii, H.; Okano, T.; Hara, I. Health exercise demonstration robot TAIZO and effects of using voice command in robot-human collaborative demonstration. In Proceedings of the RO-MAN 2009—The 18th IEEE International Symposium on Robot and Human Interactive Communication, Toyama, Japan, 27 September–2 October 2009; pp. 472–477. [Google Scholar]
- Poo, M.-M.; Du, J.-L.; Ip, N.Y.; Xiong, Z.-Q.; Xu, B.; Tan, T. China Brain Project: Basic neuroscience, brain diseases, and brain-inspired computing. Neuron 2016, 92, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Jing, M.; Dai, S. China Recruits Baidu, Alibaba and Tencent to AI ‘National Team’. Available online: https://www.scmp.com/tech/china-tech/article/2120913/china-recruits-baidu-alibaba-and-tencent-ai-national-team (accessed on 11 December 2018).
- Jee, K.; Kim, G.-H. Potentiality of big data in the medical sector: Focus on how to reshape the healthcare system. Healthc. Inform. Res. 2013, 19, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Vuong, Q.-H. Health communication, information technology and the public’s attitude toward periodic general health examinations. F1000Research 2016, 5, 2935. [Google Scholar] [CrossRef]
- Piette, J.D.; Lun, K.; Moura Jr, L.A.; Fraser, H.S.; Mechael, P.N.; Powell, J.; Khoja, S.R. Impacts of e-health on the outcomes of care in low-and middle-income countries: Where do we go from here? Bull. World Health Organ. 2012, 90, 365–372. [Google Scholar] [CrossRef] [PubMed]
- DeRenzi, B.; Borriello, G.; Jackson, J.; Kumar, V.S.; Parikh, T.S.; Virk, P.; Lesh, N. Mobile phone tools for field-based health care workers in low-income countries. Mount Sinai J. Med. A J. Transl. Person. Med. 2011, 78, 406–418. [Google Scholar] [CrossRef]
- Kahn, J.G.; Yang, J.S.; Kahn, J.S. ‘Mobile’ Health Needs And Opportunities In Developing Countries. Health Aff. 2010, 29, 252–258. [Google Scholar] [CrossRef] [PubMed]
- DeRenzi, B.; Lesh, N.; Parikh, T.; Sims, C.; Maokla, W.; Chemba, M.; Hamisi, Y.; Hellenberg, D.S.; Mitchell, M.; Borriello, G. E-IMCI: Improving pediatric health care in low-income countries. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Florence, Italy, 5–10 April 2008; pp. 753–762. [Google Scholar]
- Piette, J.D.; Datwani, H.; Gaudioso, S.; Foster, S.M.; Westphal, J.; Perry, W.; Rodríguez-Saldaña, J.; Mendoza-Avelares, M.O.; Marinec, N. Hypertension management using mobile technology and home blood pressure monitoring: Results of a randomized trial in two low/middle-income countries. Telemed. e-Health 2012, 18, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Chretien, J.-P.; Burkom, H.S.; Sedyaningsih, E.R.; Larasati, R.P.; Lescano, A.G.; Mundaca, C.C.; Blazes, D.L.; Munayco, C.V.; Coberly, J.S.; Ashar, R.J.; et al. Syndromic surveillance: Adapting innovations to developing settings. PLoS Med. 2008, 5, e72. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Chen, S.; Liu, B.; Zhang, R.; Wang, Y.; Li, P.; Guo, Y.; Zhang, H.; Gao, Z.; Yan, X. Development of traditional Chinese medicine clinical data warehouse for medical knowledge discovery and decision support. Artif. Intell. Med. 2010, 48, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Zhou, X.; Wang, Y.; Hu, J.; He, L.; Zhang, R.; Chen, S.; Guo, Y. Data processing and analysis in real-world traditional Chinese medicine clinical data: Challenges and approaches. Stat. Med. 2012, 31, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Tien Bui, D.; Pradhan, B.; Lofman, O.; Revhaug, I. Landslide susceptibility assessment in Vietnam using support vector machines, decision tree, and Naive Bayes Models. Math. Probl. Eng. 2012, 2012. [Google Scholar] [CrossRef]
- Tien Bui, D.; Pradhan, B.; Lofman, O.; Revhaug, I.; Dick, O.B. Landslide susceptibility mapping at Hoa Binh province (Vietnam) using an adaptive neuro-fuzzy inference system and GIS. Comput. Geosci. 2012, 45, 199–211. [Google Scholar] [CrossRef]
- Tien Bui, D.; Pradhan, B.; Lofman, O.; Revhaug, I.; Dick, O.B. Landslide susceptibility assessment in the Hoa Binh province of Vietnam: A comparison of the Levenberg–Marquardt and Bayesian regularized neural networks. Geomorphology 2012, 171–172, 12–29. [Google Scholar] [CrossRef]
- Tien Bui, D.; Pradhan, B.; Nampak, H.; Bui, Q.-T.; Tran, Q.-A.; Nguyen, Q.-P. Hybrid artificial intelligence approach based on neural fuzzy inference model and metaheuristic optimization for flood susceptibilitgy modeling in a high-frequency tropical cyclone area using GIS. J. Hydrol. 2016, 540, 317–330. [Google Scholar] [CrossRef]
- Tien Bui, D.; Bui, Q.-T.; Nguyen, Q.-P.; Pradhan, B.; Nampak, H.; Trinh, P.T. A hybrid artificial intelligence approach using GIS-based neural-fuzzy inference system and particle swarm optimization for forest fire susceptibility modeling at a tropical area. Agric. Forest Meteorol. 2017, 233, 32–44. [Google Scholar] [CrossRef]
- Truong, X.; Mitamura, M.; Kono, Y.; Raghavan, V.; Yonezawa, G.; Truong, X.; Do, T.; Tien Bui, D.; Lee, S. Enhancing prediction performance of landslide susceptibility model using hybrid machine learning approach of bagging ensemble and logistic model tree. Appl. Sci. 2018, 8, 1046. [Google Scholar] [CrossRef]
- Tien Bui, D.; Tuan, T.A.; Hoang, N.-D.; Thanh, N.Q.; Nguyen, D.B.; Van Liem, N.; Pradhan, B. Spatial prediction of rainfall-induced landslides for the Lao Cai area (Vietnam) using a hybrid intelligent approach of least squares support vector machines inference model and artificial bee colony optimization. Landslides 2017, 14, 447–458. [Google Scholar] [CrossRef]
- Tien Bui, D.; Pradhan, B.; Revhaug, I.; Trung Tran, C. A comparative assessment between the application of fuzzy unordered rules induction algorithm and J48 decision tree models in spatial prediction of shallow landslidaes at Lang Son city, Vietnam. In Remote Sensing Applications in Environmental Research; Srivastava, P.K., Mukherjee, S., Gupta, M., Islam, T., Eds.; Springer International Publishing: Cham, Switzerland, 2014; pp. 87–111. [Google Scholar]
- Nguyen, Q.B.; Vu, T.T.; Luong, C.M. Improving acoustic model for vietnamese large vocabulary continuous speech recognition system using deep bottleneck features. In Knowledge and Systems Engineering. Advances in Intelligent Systems and Computing; Nguyen, V.H., Le, A.C., Huynh, V.N., Eds.; Springer International Publishing: Cham, Switzerland, 2015; Volume 326, pp. 49–60. [Google Scholar]
- Sakti, S.; Kimura, N.; Paul, M.; Hori, C.; Sumita, E.; Nakamura, S.; Park, J.; Wutiwiwatchai, C.; Xu, B.; Riza, H.; et al. The Asian network-based speech-to-speech translation system. In Proceedings of the 2009 IEEE Workshop on Automatic Speech Recognition & Understanding, Merano, Italy, 13 November–17 December 2009; pp. 507–512. [Google Scholar]
- Nguyen, D.; Nguyen, C.; Thuan, D.-B.; Nguyen, H.; Nguyen, A.; Tran, T. Joint network coding and machine learning for error-prone wireless broadcast. In Proceedings of the 2017 IEEE 7th Annual Computing and Communication Workshop and Conference (CCWC), Las Vegas, NV, USA, 9–11 January 2017; pp. 1–7. [Google Scholar]
- Hoang, N.-D.; Pham, A.-D. Hybrid artificial intelligence approach based on metaheuristic and machine learning for slope stability assessment: A multinational data analysis. Expert Syst. Appl. 2016, 46, 60–68. [Google Scholar] [CrossRef]
- Le, D.-H.; Nguyen, M.-H. Towards more realistic machine learning techniques for prediction of disease-associated genes. In Proceedings of the Sixth International Symposium on Information and Communication Technology, Hue City, Vietnam, 3–4 December 2015; pp. 116–120. [Google Scholar]
- Nguyen, T.-P.; Ho, T.-B. Detecting disease genes based on semi-supervised learning and protein–protein interaction networks. Artif. Intell. Med. 2012, 54, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Bui, Q.-T.; Nguyen, Q.-H.; Pham, V.M.; Pham, M.H.; Tran, A.T. Understanding spatial variations of malaria in Vietnam using remotely sensed data integrated into GIS and machine learning classifiers. Geocarto Int. 2018, 1–15. [Google Scholar] [CrossRef]
- Bui, T.Q.; Pham, H.M. Web-based GIS for spatial pattern detection: Application to malaria incidence in Vietnam. SpringerPlus 2016, 5, 1014. [Google Scholar] [CrossRef] [PubMed]
- Pham, V.H.; Pham, V.H.; Pham, X.C. Application of remote sensing and GIS for prevention-risk warning of malaria in Gia Lai areas. In Proceedings of the 35th Asian Conference on Remote Sensing 2014 (ACRS 2014), Nay Pyi Taw, Myanmar, 27–31 October 2014. [Google Scholar]
- Doan, S.; Kawazoe, A.; Collier, N. Global health monitor-a web-based system for detecting and mapping infectious diseases. In Proceedings of the Third International Joint Conference on Natural Language Processing (IJCNLP), Hyderabad, India, 7–12 January 2008; Volume II, pp. 951–956. [Google Scholar]
- Hai, T.S.; Thuy, N.T. Image classification using support vector machine and artificial neural network. Int. J. Inf. Technol. Comput. Sci. 2012, 4, 32–38. [Google Scholar] [CrossRef]
- Hoang, T.H.; Lock, K.; Mouton, A.; Goethals, P.L.M. Application of classification trees and support vector machines to model the presence of macroinvertebrates in rivers in Vietnam. Ecol. Inform. 2010, 5, 140–146. [Google Scholar] [CrossRef]
- Nguyen Tan Tran Minh, K.; Nguyen Ba, P.; Tran Thi Hue, N. The bees algorithm for a practical university timetabling problem in Vietnam. In Proceedings of the 2011 IEEE International Conference on Computer Science and Automation Engineering, Shanghai, China, 10–12 June 2011; pp. 42–47. [Google Scholar]
- Boissau, S.; Castella, J.-C. Constructing a common representation of local institutions and land use systems through simulation-gaming and multiagent modeling in rural areas of northern Vietnam: The samba-week methodology. Simul. Gaming 2003, 34, 342–357. [Google Scholar] [CrossRef]
- Castella, J.-C.; Boissau, S.; Trung, T.N.; Quang, D.D. Agrarian transition and lowland–upland interactions in mountain areas in northern Vietnam: Application of a multi-agent simulation model. Agric. Syst. 2005, 86, 312–332. [Google Scholar] [CrossRef]
- Polo, J.; Bernardos, A.; Navarro, A.A.; Fernandez-Peruchena, C.M.; Ramírez, L.; Guisado, M.V.; Martínez, S. Solar resources and power potential mapping in Vietnam using satellite-derived and GIS-based information. Energy Convers. Manag. 2015, 98, 348–358. [Google Scholar] [CrossRef]
- Nguyen, X.P. PM Phuc’s Remarks at Opening Session of WEF on ASEAN 2018. Available online: http://news.chinhphu.vn/Home/PM-Phucs-remarks-at-opening-session-of-WEF-on-ASEAN-2018/20189/34676.vgp (accessed on 18 December 2018).
- Vuong, Q.H. The rise of computational entrepreneurship. In Working Draft #AISDL 18-02; Phenikaa University: Hanoi, Vietnam, 2018. [Google Scholar]
- Dan Tri. Trí tuệ nhân tạo—ngành học “nóng” trong tương lai [Artificial Intelligence—A “hot” subject in the future]. Available online: https://dantri.com.vn/giao-duc-khuyen-hoc/dai-hoc-viet-nam-tang-cuong-dao-tao-chuong-trinh-lien-quan-den-tri-tue-nhan-tao-20180512155935665.htm (accessed on 16 December 2018).
- Khanh, H.T.K.; Hung, T.C.; Dang, V.-H.; Thang, N.D. Human Organ Classifications from Computed Tomography Images Using Deep-Convolutional Neural Network. In 6th International Conference on the Development of Biomedical Engineering in Vietnam (BME6); Springer: Singapore, 2018; pp. 917–923. [Google Scholar]
- Le, H.; Can, D.; Dang, T.H.; Tran, M.; Ha, Q.; Collier, N. Improving chemical-induced disease relation extraction with learned features based on convolutional neural network. In Proceedings of the 2017 9th International Conference on Knowledge and Systems Engineering (KSE), Hue, Vietnam, 19–21 October 2017; pp. 292–297. [Google Scholar]
- Thompson, C.N.; Zelner, J.L.; Nhu, T.D.H.; Phan, M.V.T.; Hoang Le, P.; Nguyen Thanh, H.; Vu Thuy, D.; Minh Nguyen, N.; Ha Manh, T.; Van Hoang Minh, T.; et al. The impact of environmental and climatic variation on the spatiotemporal trends of hospitalized pediatric diarrhea in Ho Chi Minh City, Vietnam. Health Place 2015, 35, 147–154. [Google Scholar] [CrossRef]
- Nguyen, P.A.; Syed-Abdul, S.; Minamareddy, P.; Lee, P.; Ngo, T.D.; Iqbal, U.; Nguyen, P.H.; Jian, W.-S.; Li, Y.-C. A method to manage and share anti-retroviral (ARV) therapy information of human immunodeficiency virus (HIV) patients in Vietnam. Comput. Methods Programs Biomed. 2013, 111, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.T.; Nguyen, G.T.; Lam, V.T.N. An Approach to Data Mining in Healthcare: Improved K-means Algorithm. J. Ind. Intell. Inf. 2013, 1. [Google Scholar] [CrossRef]
- Chan, C.L.; Ang, P.S.; Li, S.C. A survey on pharmacovigilance activities in Asean and selected non-Asean countries, and the use of quantitative signal detection algorithms. Drug Saf. 2017, 40, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Hayton, B. Vietnam: Rising Dragon; Yale University Press: New Haven, CT, USA, 2010. [Google Scholar]
- Vuong, Q.H. Vietnam’s political economy: A discussion on the 1986–2016 period. In Working Papers CEB 14-010, ULB; Universite Libre de Bruxelles: Bruxelles, Belgium, 2014. [Google Scholar]
- Vietnam Ministry of Health; Health Partnership Group. Joint Annual Health Review 2012: Strengthening Prevention and Control of Non-Communicable Disease; Vietnam Ministry of Health: Hanoi, Vietnam, 2012. Available online: http://www.jahr.org.vn/ (accessed on 31 January 2019).
- Vietnam Ministry of Health; Health Partnership Group. Joint Annual Health Review 2013: Towards Universal Health Coverage; Vietnam Ministry of Health: Hanoi, Vietnam, 2013. Available online: http://www.jahr.org.vn/ (accessed on 31 January 2019).
- Vietnam Ministry of Health. Joint Annual Health Review 2014: Strengthening Prevention and Control of Non-Communicable Disease; Vietnam Ministry of Health: Hanoi, Vietnam, 2014. Available online: http://www.jahr.org.vn/ (accessed on 31 January 2019).
- Vietnam Ministry of Health; Health Partnership Group. Joint Annual Health Review 2015: Strengthening Primary Health Care at the Grassroots towards Universal Health Coverage; Medical Publishing House: Hanoi, Vietnam, 2016. Available online: http://www.jahr.org.vn/ (accessed on 31 January 2019).
- Vietnam Ministry of Health; Health Partnership Group. Joint Annual Health Review 2016: Towards Healthy Aging in Vietnam; Medical Publishing House: Hanoi, Vietnam, 2018. Available online: http://www.jahr.org.vn/ (accessed on 31 January 2019).
- Nguyen, Q.; Naguib, R.; Tawfik, H.; Phuong, N. Strategic challenges facing user-and patient-centred e-health in Vietnam. Int. J. Healthcare Technol. Manag. 2012, 13, 378–394. [Google Scholar] [CrossRef]
- Hecht, J. Managing expectations of artificial intelligence. Nature 2018, 563, S141–S143. [Google Scholar] [CrossRef] [PubMed]
- Ngoc, N.T. Institutional perspectives on implementing health information systems in developing countries: The case of electronic medical records (EMR) for children health in Vietnam. In Proceedings of the AMCIS 2010, Lima, Peru, 12–15 August 2010. [Google Scholar]
- Hoang, V.M.; Nasca, P. Public Health in Transitional Vietnam: Achievements and Challenges. J. Public Health Manag. Pract. 2018, 24, S1–S2. [Google Scholar] [CrossRef]
- Kitaki, H. Managing Technical Efficiency of Public and Private Hospitals in Vietnam: Do Market-Oriented Policies Matter? In JICA-RI Working Paper; JICA Research Institute: Tokyo, Japan, 2018. [Google Scholar]
- Vuong, Q.-H.; Ho, T.-M.; Nguyen, H.-K.; Vuong, T.-T. Healthcare consumers’ sensitivity to costs: A reflection on behavioural economics from an emerging market. Palgrave Commun. 2018, 4, 70. [Google Scholar] [CrossRef]
- Vuong, Q.-H.; Bui, Q.-K.; La, V.-P.; Vuong, T.-T.; Nguyen, V.-H.T.; Ho, M.-T.; Nguyen, H.-K.T.; Ho, M.-T. Cultural additivity: Behavioural insights from the interaction of Confucianism, Buddhism and Taoism in folktales. Palgrave Commun. 2018, 4, 143. [Google Scholar] [CrossRef]
- Khuat, H.T.; Do, T.T.; Nguyen, A.V.; Vu, T.X.; Nguyen, T.P.; Tran, K.; Ho, T.M.; Nguyen, T.H.K.; Vuong, T.T.; La, P.V.; et al. The Dark Side of Female HIV Patient Care: Sexual and Reproductive Health Risks in Pre- and Post-Clinical Treatments. J. Clin. Med. 2018, 7, 402. [Google Scholar] [CrossRef] [PubMed]
- Vuong, Q.-H. The (ir)rational consideration of the cost of science in transition economies. Nat. Hum. Behav. 2018, 2, 5. [Google Scholar] [CrossRef]
- Ousmane, D. Industry 4.0—Harnessing Disruption for Vietnam’s Development. Available online: https://www.worldbank.org/en/news/speech/2018/07/13/industry-4-harnessing-disruption-for-vietnams-development (accessed on 18 December 2018).
- Sunstein, C.; Thaler, R. The Two Friends Who Changed How We Think About How We Think. Available online: http://www.newyorker.com/books/page-turner/the-two-friends-who-changed-how-we-think-about-how-we-think (accessed on 18 December 2018).

| Artificial Neural Networks | Fuzzy Expert Systems | Evolutionary Computations | Hybrid Intelligent Systems | |
|---|---|---|---|---|
| Inception date | 1943: first artificial neuron; | 1965: popularized by Lofti Zadeh; | 1975: John Holland’s “Genetic Algorithms”; | |
| Description | Computational analytical tools; | Data handling methodology that permits ambiguity; | Computational techniques based on natural evolution process; | A combination of two or three of the above systems; |
| Algorithms | Multilayer feedforward; backpropagation algorithm; gradient descent; | Fuzzy control language; Continuous set membership from 0 to 1; “If-then” modeling: - Rule-based - Knowledge-based; | Stochastic search and optimization algorithms; Suitable for functions that are: non-linear, non-convex, non-differentiable, discontinuous; | Fuzzy logic; Genetic algorithms; Case-based reasoning; Neural networks; |
| Notable Applications | Clinical diagnosis; Image analysis in radiology & histopathology; Data interpretation in intensive care setting; Waveform analysis; Prognosis; | Diagnosis of certain types of cancer; Health/Clinical decision support systems; Reference consultation; | Outcome prediction in critically ill patients, lung cancer, melanoma, response to warfarin; Computerized analysis of certain carcinogenic diseases; Prediction of protein complexes; | Medical decision support tool; Breast cancer diagnosis; Diagnosis of coronary artery stenosis; Control of the depth of anesthesia; |
| 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|
| 0.32–0.38 | lacking | information | analyzing | ||
| standardization | inefficient | software | |||
| 0.43–0.55 | online | computers | |||
| warehouse | digital | ||||
| Above 0.56 | inaccurate | ||||
| standardizing | |||||
| incomplete | |||||
| inefficient |
| Administrative | Progress | Clinical | Progress | National | Progress |
|---|---|---|---|---|---|
| Hospital management | 54% of hospitals are using some software for internal management. | Diagnosis and treatment database | Under construction but remains not unified; hospitals use different software. | National standardized database | Not yet built. |
| Human resources management | Hospital software is said to be HR-focused. | Medical devices database | Under construction but not unified. | Departmental or provincial health databases | Under construction but not unified. |
| Database to track stakeholders in health management | Not yet built. | Drugs database/Prescription monitoring system | Under construction but largely mismatched. | Database about national target programs, preventive health, the private sector | Under construction but severely lacking. |
| Medical data collection | Manual collection, sporadic, lack of integration across establishments, which created duplication. | Electronic medical record (EMR) database | Under construction but needs to be standardized and integrated into the national system. | Health information system 2015–2020 | Under construction but needs to be standardized. |
| Medical costs database | Not yet built. | Mortality and infection reports | Requested to be formulated a long time ago but lacking accurate data. | System to monitor implement of legal health documents | Not yet built. |
| Medical information reporting | There is no requirement for replacing paper reports with digital reports. | Database for diseases control | Not yet built. | Databases linking private and public health resources, and tracking patient responses | Not yet built. |
| Picture archiving and communication system (PACS) | Some medical establishments have used PACS but there is no official guideline for this yet. | Database to monitor adverse drug reaction (ADR) | Most hospitals have been collecting this information, but no official reports have been made. | Database about all licensed doctors | Not yet built. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; La, V.-P.; Ho, M.-T.; Nghiem, K.-C.P.; Tran, B.X.; Giang, H.-H.; Giang, T.-V.; Latkin, C.; et al. Artificial Intelligence vs. Natural Stupidity: Evaluating AI Readiness for the Vietnamese Medical Information System. J. Clin. Med. 2019, 8, 168. https://doi.org/10.3390/jcm8020168
Vuong Q-H, Ho M-T, Vuong T-T, La V-P, Ho M-T, Nghiem K-CP, Tran BX, Giang H-H, Giang T-V, Latkin C, et al. Artificial Intelligence vs. Natural Stupidity: Evaluating AI Readiness for the Vietnamese Medical Information System. Journal of Clinical Medicine. 2019; 8(2):168. https://doi.org/10.3390/jcm8020168
Chicago/Turabian StyleVuong, Quan-Hoang, Manh-Tung Ho, Thu-Trang Vuong, Viet-Phuong La, Manh-Toan Ho, Kien-Cuong P. Nghiem, Bach Xuan Tran, Hai-Ha Giang, Thu-Vu Giang, Carl Latkin, and et al. 2019. "Artificial Intelligence vs. Natural Stupidity: Evaluating AI Readiness for the Vietnamese Medical Information System" Journal of Clinical Medicine 8, no. 2: 168. https://doi.org/10.3390/jcm8020168









