Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup
Abstract
:1. Introduction
2. Material and Methods
2.1. Orthognathic-Surgery Treatment
- (a)
- In the conventional approach, surgery was performed after a period of at least seven months of complete orthodontic therapy, including the leveling and alignment of dental arches to eliminate any occlusal interference at surgery, and the removal of all dental compensations to maximize optimal surgical repositioning of the jaws.
- (b)
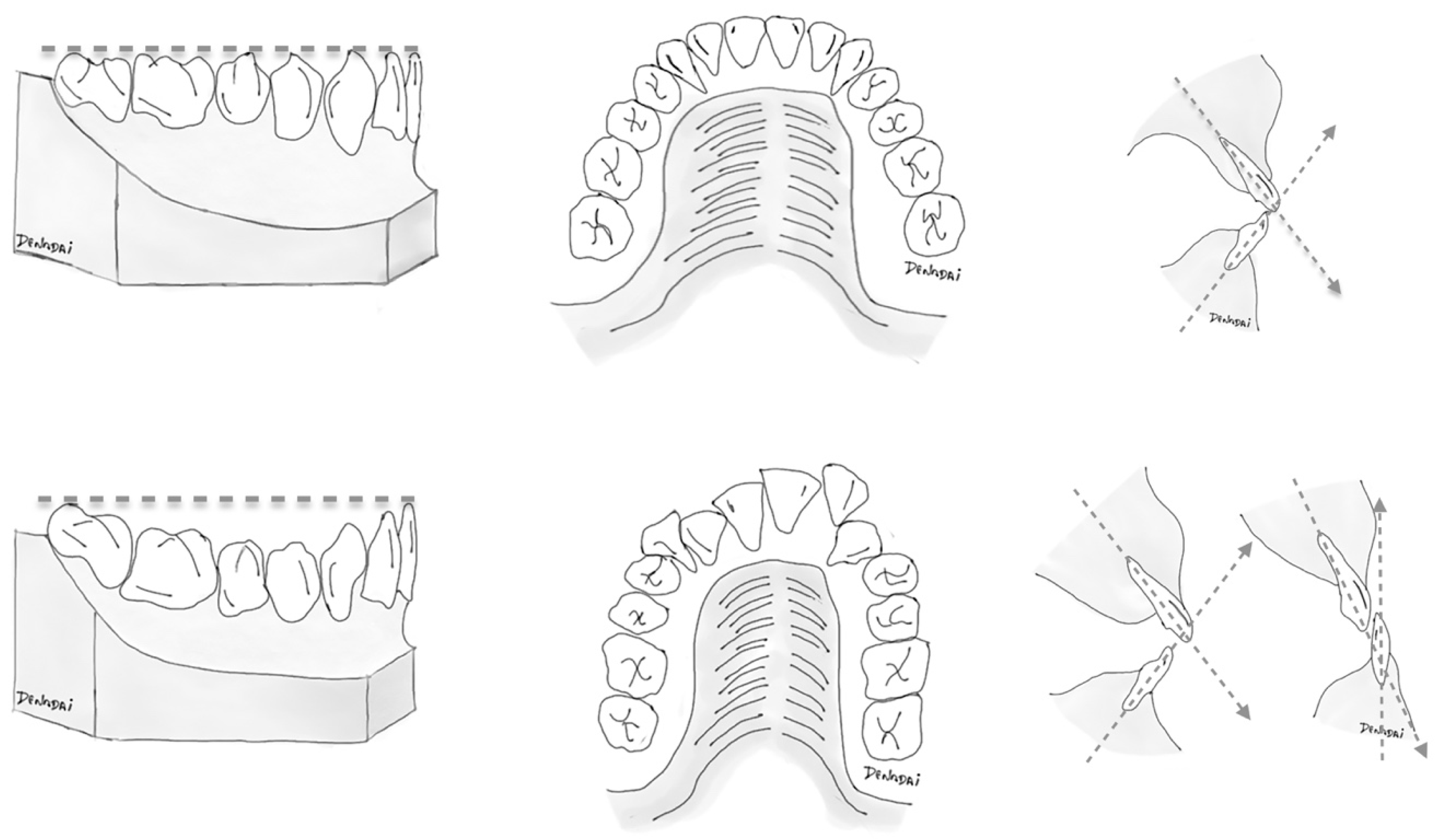
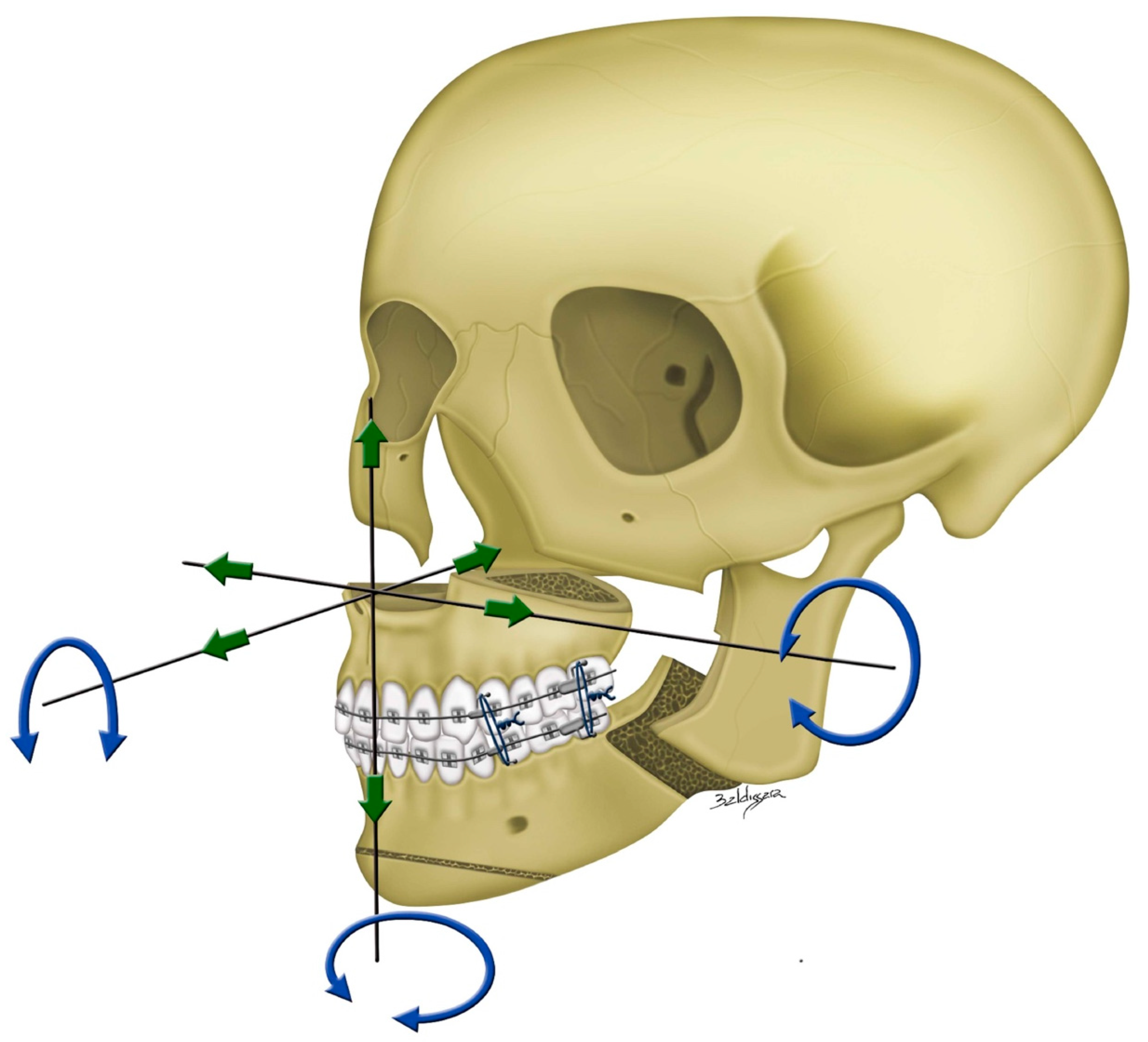
- Patients with different compositions of the dental conditions (Table 1) received the surgery-first orthognathic treatment based on a patient-specific therapeutic planning (Figure 1). Patients with more and less favorable dental conditions received the surgery-first treatment as it was based on the orthodontist’s judgment of achievement of a practicable surgical-occlusion setup as well as anticipation of a feasible postoperative orthodontic treatment. Our team stratified the surgery-first approach into two models. In the standard surgery-first model, surgery was performed with no need for presurgical orthodontic therapy. In the modified surgery-first model, a short period (≤6 months) of orthodontic therapy was performed preoperatively. This presurgical dental adjustment was exclusively implemented for the reduction of potential dental collisions and the minimal decompression of mandibular teeth.
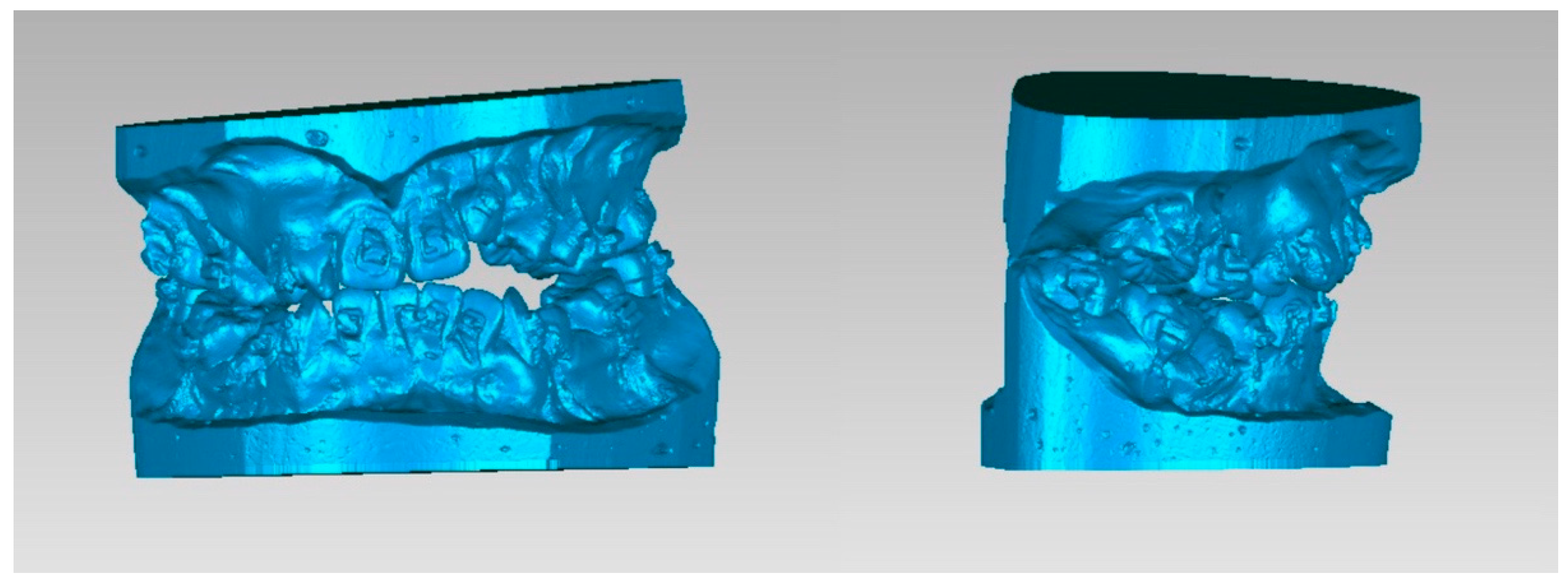
2.2. 3D-Image Acquisition
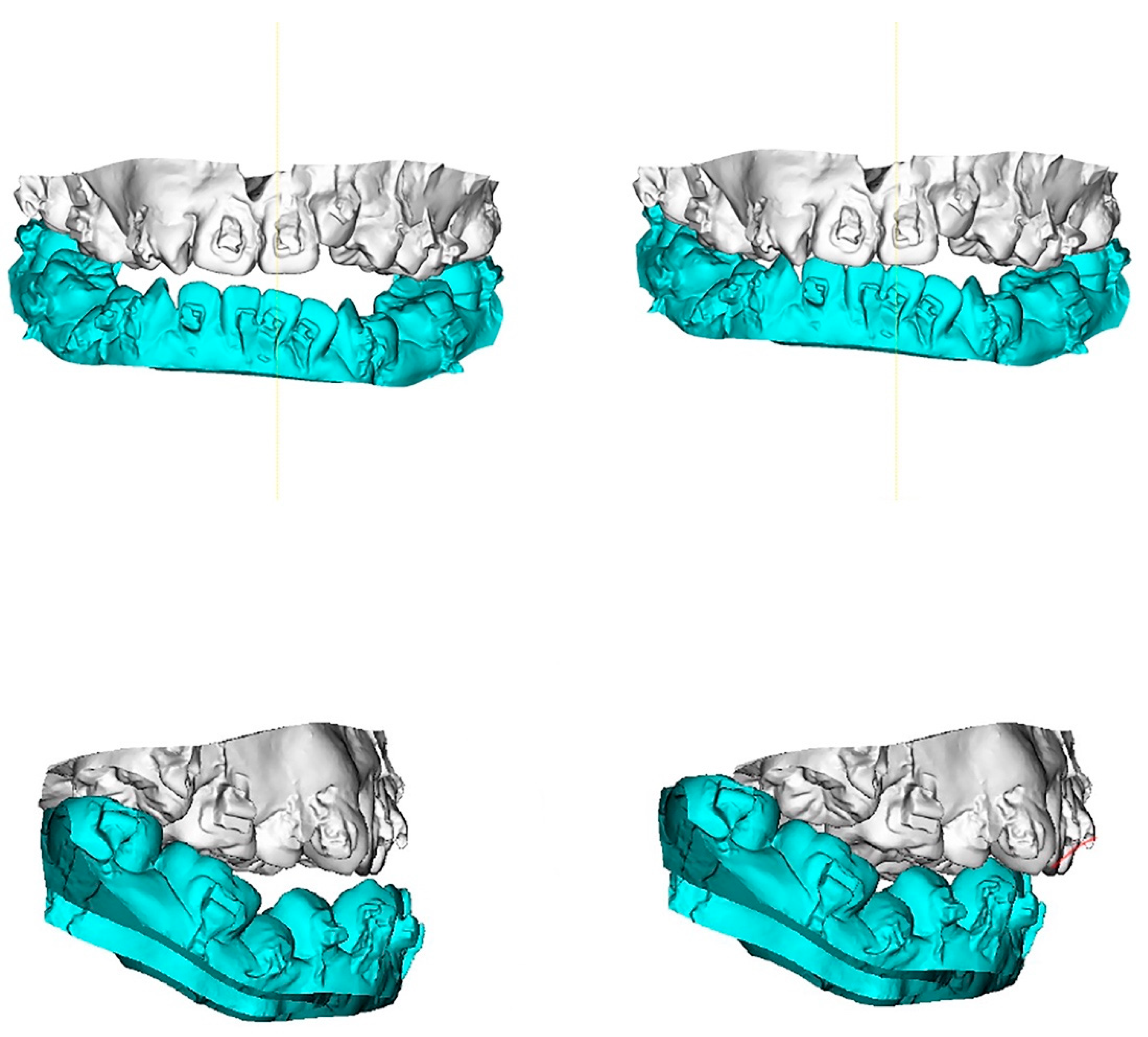
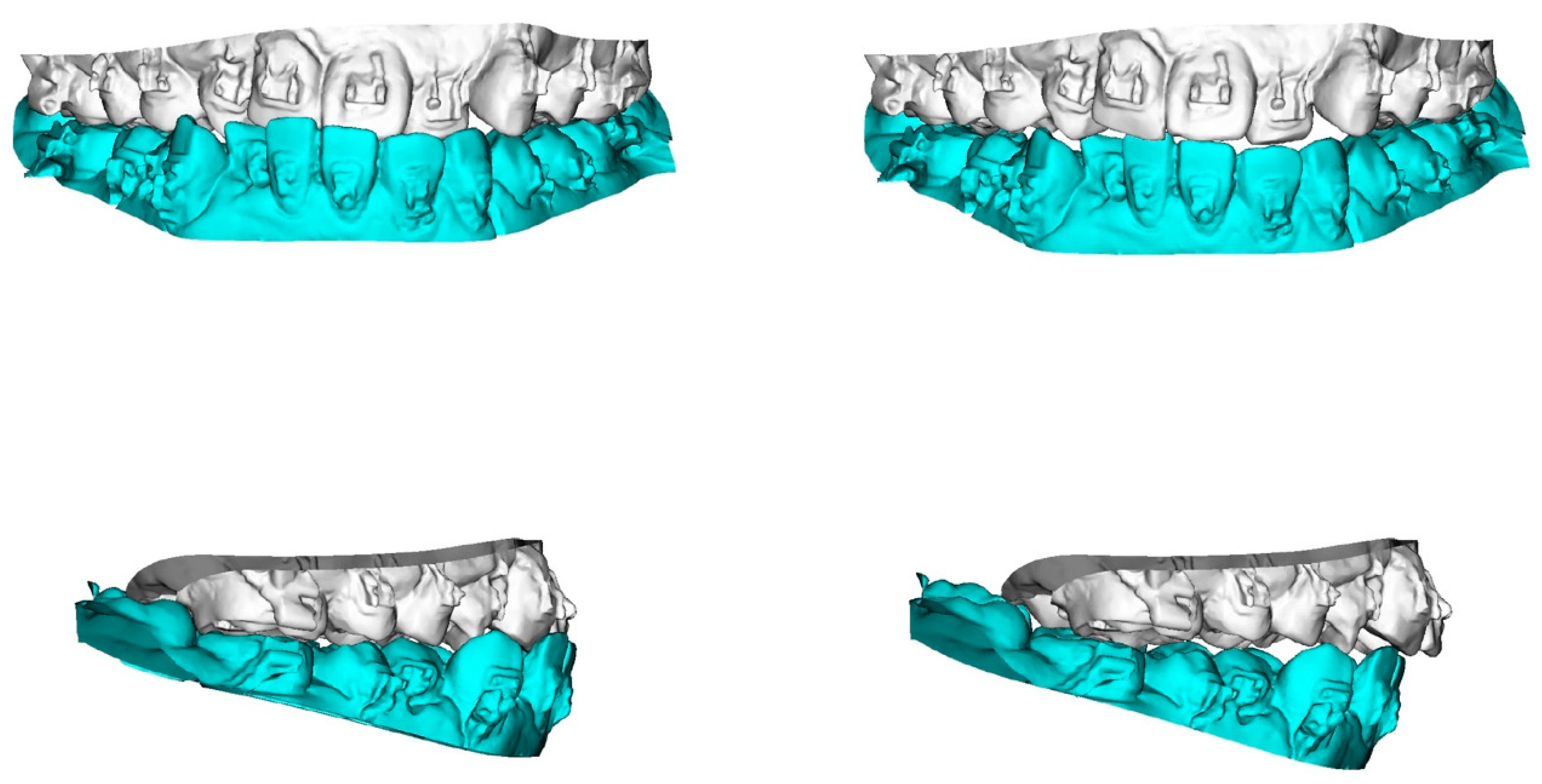
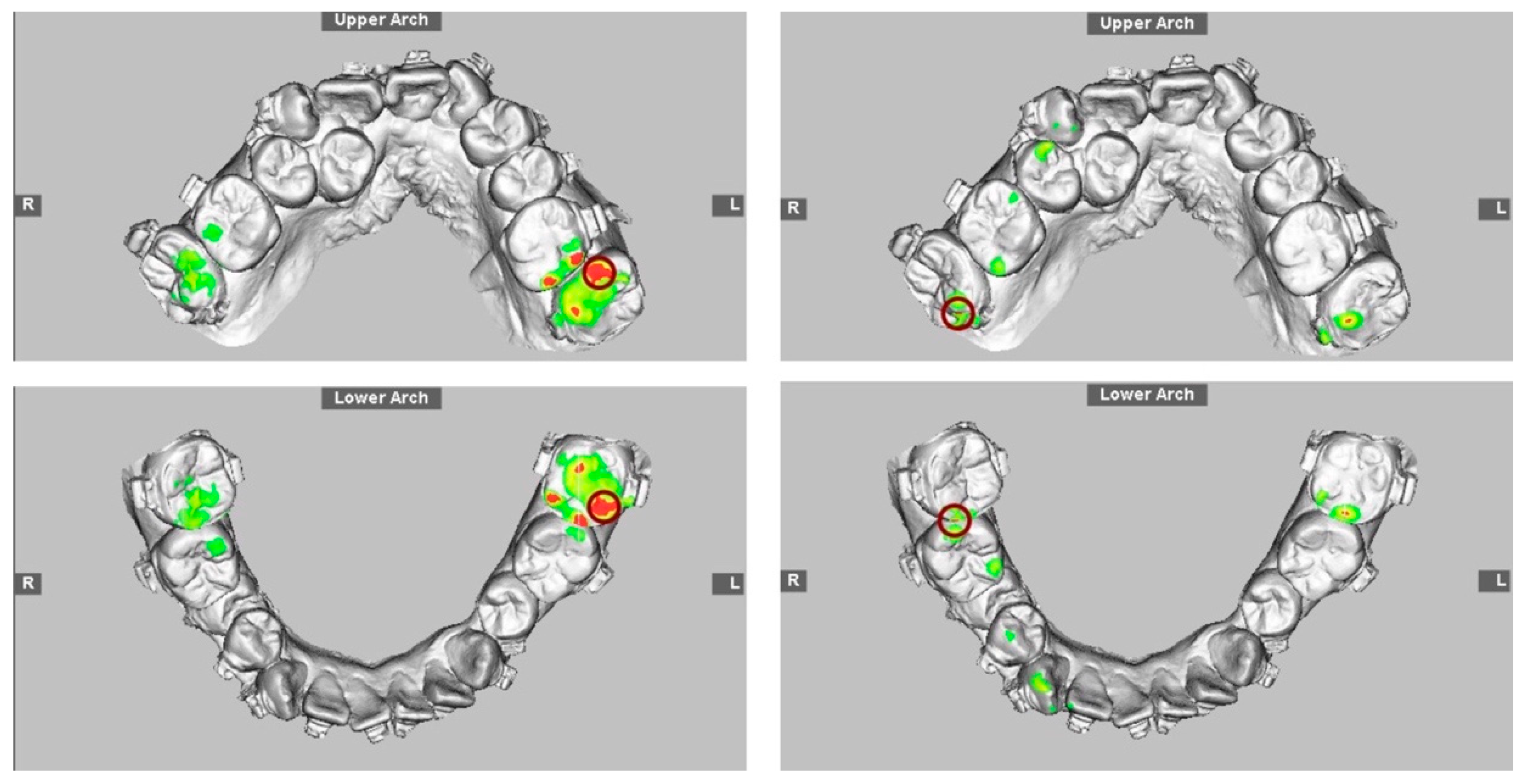
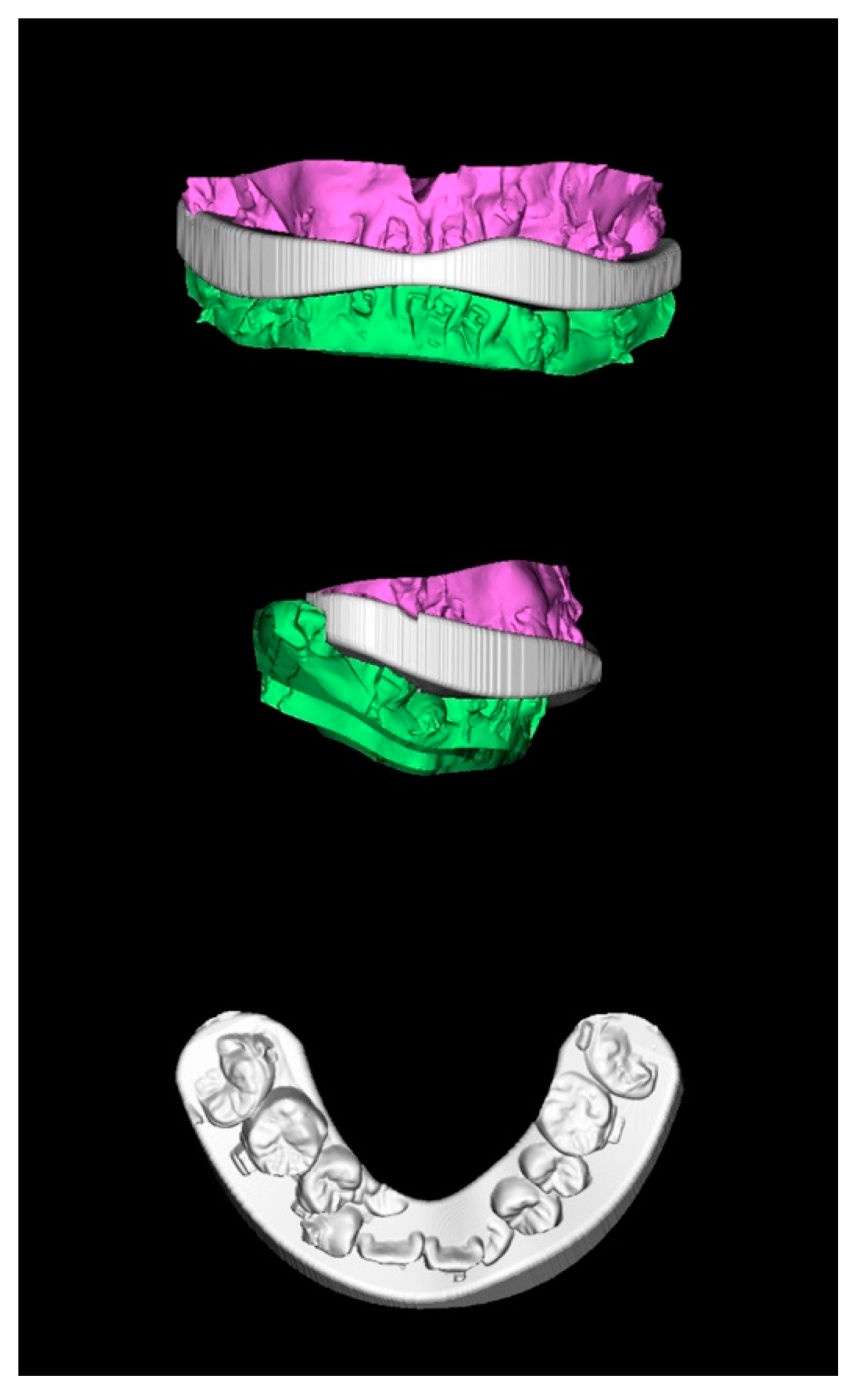
2.3. Final Surgical-Occlusion Setup
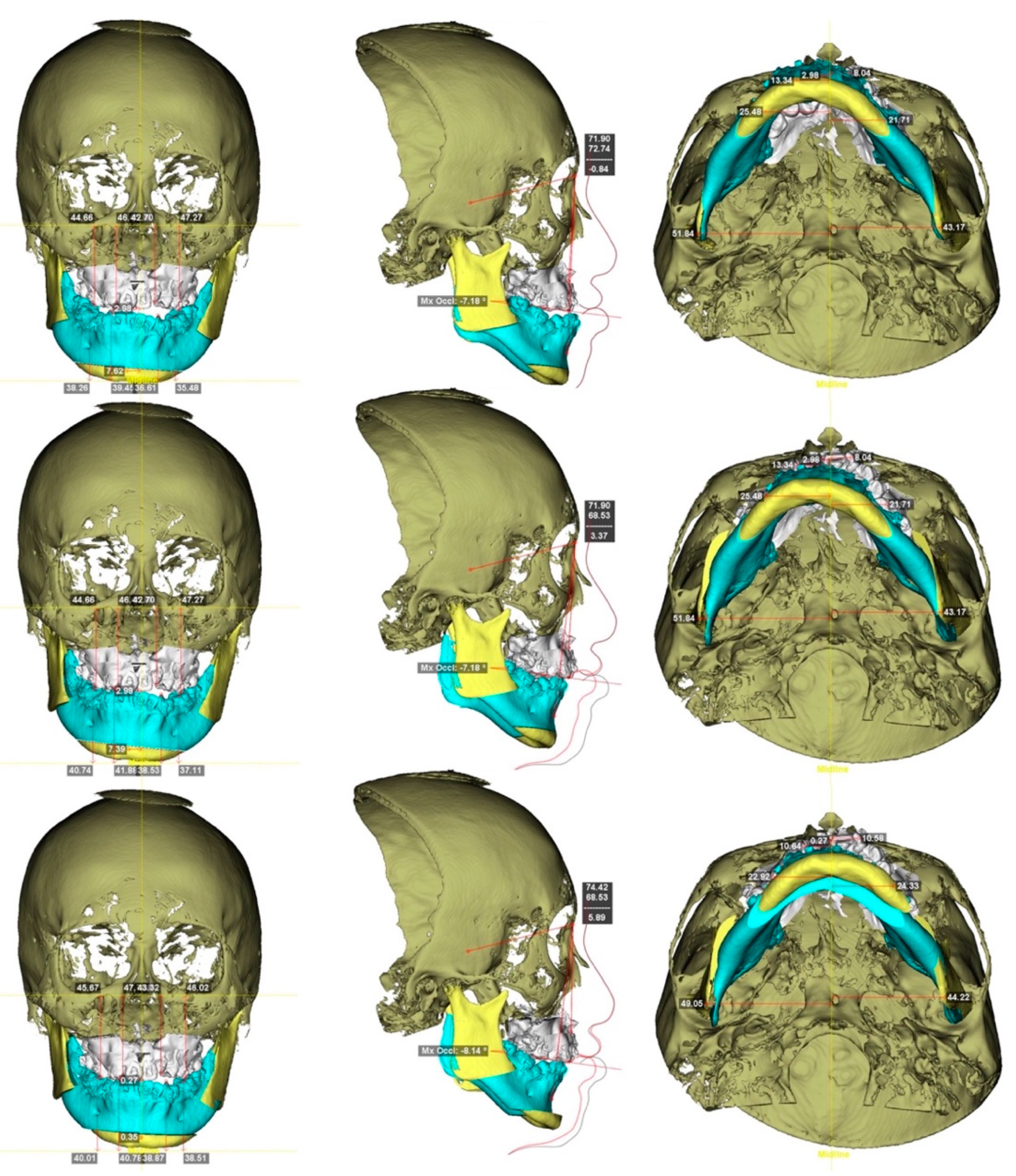
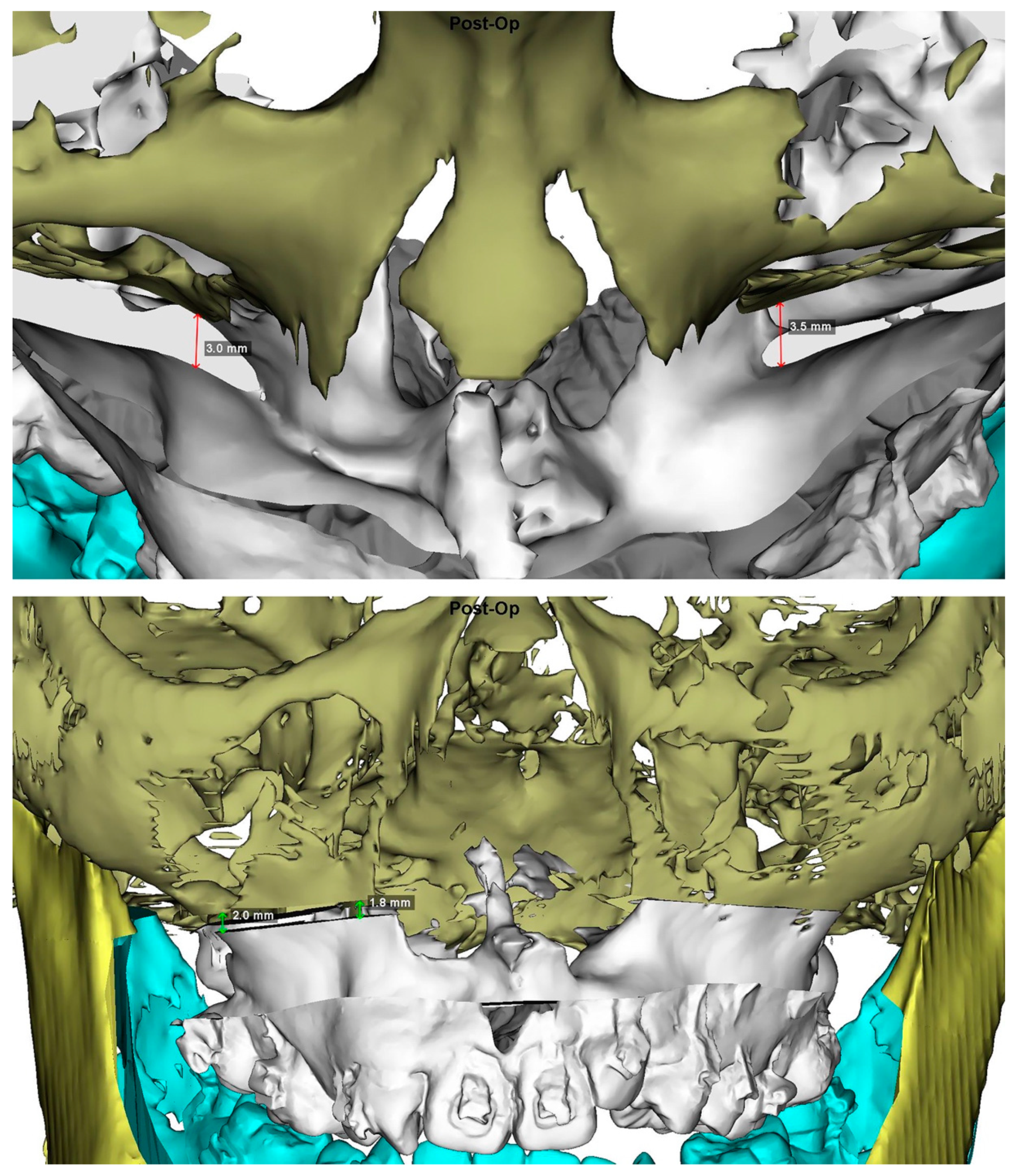
2.4. Virtual Planning
2.5. Type of Orthognathic Approach
2.6. Surgical Approach
2.7. 3D Quantitative Analysis
2.8. Statistical Analysis
3. Results
3.1. Time of Presurgical Orthodontic Therapy
3.2. Primary Endpoint
3.3. Secondary Endpoint
3.4. Reliability
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mossey, P.A.; Little, J.; Munger, R.G.; Dixon, M.J.; Shaw, W.C. Cleft lip and palate. Lancet 2009, 374, 1773–1785. [Google Scholar] [CrossRef]
- Pai, B.C.J.; Hung, Y.T.; Wang, R.S.H.; Lo, L.J. Outcome of patients with complete unilateral cleft lip and palate: 20-year follow-up of a treatment protocol. Plast. Reconstr. Surg. 2019, 143, 359e–367e. [Google Scholar] [CrossRef]
- Daskalogiannakis, J.; Mehta, M. The need for orthognathic surgery in patients with repaired complete unilateral and complete bilateral cleft lip and palate. Cleft Palate Craniofac. J. 2009, 46, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Good, P.M.; Mulliken, J.B.; Padwa, B.L. Frequency of Le Fort I osteotomy after repaired cleft lip and palate or cleft palate. Cleft Palate Craniofac. J. 2007, 44, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Klassen, A.F.; Riff, K.W.W.; Longmire, N.M.; Albert, A.; Allen, G.C.; Aydin, M.A.; Baker, S.B.; Cano, S.J.; Chan, A.J.; Courtemanche, D.J.; et al. Psychometric findings and normative values for the CLEFT-Q based on 2434 children and young adult patients with cleft lip and/or palate from 12 countries. CMAJ 2018, 190, E455–E462. [Google Scholar] [CrossRef] [PubMed]
- Raghavan, S.; Philip, K.; Batra, P.; Marcusson, A. Aesthetic perceptions and psychosocial impact of malocclusion: Comparison between cleft and non-cleft patients and their parents. Eur. J. Orthod. 2019, 41, 38–45. [Google Scholar] [CrossRef]
- Su, Y.Y.; Denadai, R.; Ho, C.T.; Lai, B.R.; Lo, L.J. Measuring patient-reported outcomes in orthognathic surgery: Linguistic and psychometric validation of the Mandarin Chinese version of FACE-Q. Biomed. J. 2019. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Su, Y.Y.; Lo, C.C.; Lin, H.H.; Ho, C.T.; Lo, L.J. Facial appearance and psychosocial features in orthognathic surgery: A FACE-Q- and 3D facial image-based comparative study of patient-, clinician-, and lay-observer-reported outcomes. J. Clin. Med. 2019, 8, 909. [Google Scholar] [CrossRef]
- Broers, D.L.M.; van der Heijden, G.J.M.G.; Rozema, F.R.; de Jongh, A. Do patients benefit from orthognathic surgery? A systematic review on the effects of elective orthognathic surgery on psychosocial functioning and patient satisfaction. Eur. J. Oral Sci. 2017, 125, 411–418. [Google Scholar] [CrossRef]
- Yim, S.; Baek, S.H. Difference in degrees of satisfaction with orthognathic surgery and orthodontic treatment between skeletal class III and cleft patients. J. Craniofac. Surg. 2019, 30, 985–991. [Google Scholar] [CrossRef]
- Baik, H.S. Presurgical and postsurgical orthodontics in patients with cleft lip and palate. J. Craniofac. Surg. 2009, 20, 1771–1775. [Google Scholar] [CrossRef] [PubMed]
- Luther, F.; Morris, D.O.; Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br. J. Oral Maxillofac. Surg. 2003, 41, 401–406. [Google Scholar] [CrossRef]
- Diaz, P.M.; Garcia, R.G.; Gias, L.N.; Aguirre-Jaime, A.; Pérez, J.S.; de la Plata, M.M.; Navarro, E.V.; Gonzalez, F.J. Time used for orthodontic surgical treatment of dentofacial deformities in white patients. J. Oral Maxillofac. Surg. 2010, 68, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Nurminen, L.; Pietila, T.; Vinkka-Puhakka, H. Motivation for and satisfaction with orthodontic-surgical treatment: A retrospective study of 28 patients. Eur. J. Orthod. 1999, 21, 79–87. [Google Scholar] [CrossRef]
- Nagasaka, H.; Sugawara, J.; Kawamura, H.; Nanda, R. “Surgery first” skeletal Class III correction using the Skeletal Anchorage System. J. Clin. Orthod. 2009, 43, 97–105. [Google Scholar]
- Villegas, C.; Uribe, F.; Sugawara, J.; Nanda, R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J. Clin. Orthod. 2010, 44, 97–103. [Google Scholar]
- Yu, C.C.; Chen, P.H.; Liou, E.J.; Huang, C.S.; Chen, Y.R. A Surgery-first approach in surgical-orthodontic treatment of mandibular prognathism-a case report. Chang. Gung Med. J. 2010, 33, 699–705. [Google Scholar]
- Huang, X.; Cen, X.; Sun, W.; Xia, K.; Yu, L.; Liu, J.; Zhao, Z. The impact of surgery-first approach on the oral health-related quality of life: A systematic review and meta-analysis. BMC. Oral Health 2019, 19, 136. [Google Scholar] [CrossRef]
- Peiró-Guijarro, M.A.; Guijarro-Martínez, R.; Hernández-Alfaro, F. Surgery first in orthognathic surgery: A systematic review of the literature. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 448–462. [Google Scholar] [CrossRef]
- Huang, C.S.; Hsu, S.S.; Chen, Y.R. Systematic review of the surgery-first approach in orthognathic surgery. Biomed. J. 2014, 37, 184–190. [Google Scholar] [CrossRef]
- Pelo, S.; Saponaro, G.; Patini, R.; Staderini, E.; Giordano, A.; Gasparini, G.; Garagiola, U.; Azzuni, C.; Cordaro, M.; Foresta, E.; et al. Risks in surgery-first orthognathic approach: Complications of segmental osteotomies of the jaws. A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4–12. [Google Scholar] [PubMed]
- Huang, C.S.; Chen, Y.R. Orthodontic principles and guidelines for the surgery-first approach to orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2015, 44, 1457–1462. [Google Scholar] [CrossRef] [PubMed]
- Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; Chen, Y.R. Surgery-first accelerated orthognathic surgery: Orthodontic guidelines and setup for model surgery. J. Oral Maxillofac. Surg. 2011, 69, 771–780. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Bradley, J.P. Surgery First Orthognathic approach without presurgical orthodontic treatment: Questions and answers. J. Craniofac. Surg. 2017, 28, 1330–1333. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.; De Luca, M.; Candida, E.; Rizzo, M.I.; Rajabtork Zadeh, O.; Bucci, D.; Zama, M.; Lajolo, C.; Cordaro, M.; Gallenzi, P. Lay people esthetic evaluation of primary surgical repair on three-dimensional images of cleft lip and palate patients. Medicina 2019, 55, 576. [Google Scholar] [CrossRef] [PubMed]
- Pelo, S.; Gasparini, G.; Garagiola, U.; Cordaro, M.; Di Nardo, F.; Staderini, E.; Patini, R.; De Angelis, P.; D’Amato, G.; Saponaro, G.; et al. Surgery-first orthognathic approach vs. traditional orthognathic approach: Oral health-related quality of life assessed with 2 questionnaires. Am. J. Orthod. Dentofaci. Orthop. 2017, 152, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Ahn, H.W.; Kwon, Y.H.; Choi, J.Y. Surgery-first approach in skeletal Class III malocclusion treated with 2-jaw surgery: Evaluation of surgical movement and postoperative orthodontic treatment. J. Craniofac. Surg. 2010, 21, 332–338. [Google Scholar] [CrossRef]
- Liao, Y.F.; Chiu, Y.T.; Huang, C.S.; Ko, E.W.; Chen, Y.R. Presurgical orthodontics versus no presurgical orthodontics: Treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast. Reconstr. Surg. 2010, 126, 2074–2083. [Google Scholar] [CrossRef]
- Park, K.R.; Kim, S.Y.; Park, H.S.; Jung, Y.S. Surgery-first approach on patients with temporomandibular joint disease by intraoral vertical ramus osteotomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 436, e429. [Google Scholar] [CrossRef]
- Kim, C.S.; Lee, S.C.; Kyung, H.M.; Park, H.S.; Kwon, T.G. Stability of mandibular setback surgery with and without presurgical orthodontics. J. Oral Maxillofac. Surg. 2014, 72, 779–787. [Google Scholar] [CrossRef]
- Yu, H.B.; Mao, L.X.; Wang, X.D.; Fang, B.; Shen, S.G. The surgery-first approach in orthognathic surgery: A retrospective study of 50 cases. Int. J. Oral Maxillofac. Surg. 2015, 4, 1463–1467. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.F.; Lo, S.H. Surgical-occlusion setup in correction of skeletal class III deformity using surgery-first approach: Guidelines, characteristics and accuracy. Sci. Rep. 2018, 8, 11673. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.F.; Chen, Y.F.; Yao, C.F.; Chen, Y.A.; Chen, Y.R. Long-term outcomes of bimaxillary surgery for treatment of asymmetric skeletal class III deformity using surgery-first approach. Clin. Oral Investig. 2019, 23, 1685–1693. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.W.; Lin, S.C.; Chen, Y.R.; Huang, C.S. Skeletal and dental variables related to the stability of orthognathic surgery in skeletal Class III malocclusion with a surgery-first approach. J. Oral Maxillofac. Surg. 2013, 71, e215–e223. [Google Scholar] [CrossRef]
- Ko, E.W.; Hsu, S.S.; Hsieh, H.Y.; Wang, Y.C.; Huang, C.S.; Chen, Y.R. Comparison of progressive cephalometric changes and postsurgical stability of skeletal Class III correction with and without presurgical orthodontic treatment. J. Oral Maxillofac. Surg. 2011, 69, 1469–1477. [Google Scholar] [CrossRef]
- Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; Chen, Y.R. Surgery-first accelerated orthognathic surgery: Postoperative rapid orthodontic tooth movement. J. Oral Maxillofac. Surg. 2011, 69, 781–785. [Google Scholar] [CrossRef]
- Wang, Y.C.; Ko, E.W.; Huang, C.S.; Chen, Y.R.; Takano-Yamamoto, T. Comparison of transverse dimensional changes in surgical skeletal Class III patients with and without presurgical orthodontics. J. Oral Maxillofac. Surg. 2010, 68, 1807–1812. [Google Scholar] [CrossRef]
- Wu, T.Y.; Denadai, R.; Lin, H.H.; Ho, C.T.; Lo, L.J. The outcome of skeletofacial reconstruction with mandibular rotation for management of asymmetric skeletal class III deformity: A three-dimensional computer-assisted investigation. Sci. Rep. 2019, 9, 13337. [Google Scholar] [CrossRef] [Green Version]
- Denadai, R.; Chou, P.Y.; Pai, B.C.J.; Chen, C.; Lin, C.C.H.; Huang, C.S.; Chen, Y.R.; Lo, L.J. Skeletofacial reconstruction for cleft-related deformities: Four decades of evolving cleft care. Ann. Plast. Surg. 2019, 8, 1706. [Google Scholar]
- Lonic, D.; Pai, B.C.J.; Yamaguchi, K.; Chortrakarnkij, P.; Lin, H.H.; Lo, L.J. Computer-assisted orthognathic surgery for patients with cleft lip/palate: From traditional planning to three-dimensional surgical simulation. PLoS ONE 2016, 11, e0152014. [Google Scholar] [CrossRef]
- Denadai, R.; Lo, L.J. Toward reducing the surgical burden of care: Modern longitudinal life-changing concept in surgical cleft care. J. Formos. Med. Assoc. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Chang, H.W.; Wang, C.H.; Kim, S.G.; Lo, L.J. Three-dimensional computer-assisted orthognathic surgery: Experience of 37 patients. Ann. Plast. Surg. 2015, 74, S118–S126. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.M.; Ho, C.T.; Lo, L.J. Automatic superimposition of palatal fiducial markers for accurate integration of digital dental model and cone beam computed tomography. J. Oral Maxillofac. Surg. 2015, 73, 1616.e1–1616.e10. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.H.; Ho, C.T.; Lin, H.H.; Lo, L.J. Three-dimensional cephalometry for orthognathic planning: Normative data and analyses. J. Formos. Med. Assoc. 2019. [Google Scholar] [CrossRef]
- Hernández-Alfaro, F.; Guijarro-Martínez, R.; Molina-Coral, A.; Badía-Escriche, C. “Surgery first” in bimaxillary orthognathic surgery. J. Oral Maxillofac. Surg. 2011, 69, e201–e207. [Google Scholar]
- Hernandez-Alfaro, F.; Guijarro-Martinez, R. On a definition of the appropriate timing for surgical intervention in orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2014, 43, 846–855. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhou, Y.; Wang, X.; Li, Z. Minimal presurgical orthodontics for a skeletal Class III patient with mandibular asymmetry. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 99–113. [Google Scholar] [CrossRef]
- Choi, T.H.; Kim, S.H.; Yun, P.Y.; Kim, Y.K.; Lee, N.K. Factors related to relapse after mandibular setback surgery with minimal presurgical orthodontics. J. Oral Maxillofac. Surg. 2019, 77, 1072.e1–1072.e9. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, Y.K.; Yun, P.Y.; Larson, B.E.; Lee, N.K. Comparison of the stability after mandibular setback with minimal orthodontics of class III patients with different facial types. J. Oral Maxillofac. Surg. 2016, 74, 1464-e1. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, Y.K.; Yun, P.Y.; Lee, N.K.; Kim, J.W.; Choi, J.H. Evaluation of stability after orthognathic surgery with minimal orthodontic preparation: Comparison according to 3 types of fixation. J. Craniofac. Surg. 2014, 25, 911–915. [Google Scholar] [CrossRef]
- Kim, J.W.; Lee, N.K.; Yun, P.Y.; Moon, S.W.; Kim, Y.K. Postsurgical stability after mandibular setback surgery with minimal orthodontic preparation following upper premolar extraction. J. Oral Maxillofac. Surg. 2013, 71, 1968-e1. [Google Scholar] [CrossRef] [PubMed]
- Uribe, F.; Farrell, B. Surgery-first approach in the orthognathic patient. Oral Maxillofac. Surg. Clin. N. Am. 2019, 32, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Kwon, T.G.; Han, M.D. Current status of surgery first approach (part II): Precautions and complications. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 23. [Google Scholar] [CrossRef] [PubMed]
- Hameed, O.; Amin, N.; Haria, P.; Patel, B.; Hay, N. Orthodontic burden of care for patients with a cleft lip and/or palate. J. Orthod. 2019, 46, 63–67. [Google Scholar] [CrossRef]
- Heliövaara, A.; Leikola, J.; Rautio, J. Anterior crossbite, dental arch dimensions, and later need for orthognathic surgery in 6-year-old children with unilateral cleft lip and palate. Cleft Palate Craniofac. J. 2014, 51, 579–584. [Google Scholar] [CrossRef]
- Wu, T.T.; Chen, P.K.; Lo, L.J.; Cheng, M.C.; Ko, E.W. The characteristics and distribution of dental anomalies in patients with cleft. Chang. Gung Med. J. 2011, 34, 306–314. [Google Scholar]
- Lo, S.H.; Chen, Y.A.; Yao, C.F.; Liao, Y.F.; Chen, Y.R. Is skeletal stability after bimaxillary surgery for skeletal class III deformity related to surgical occlusal contact? Int. J. Oral Maxillofac. Surg. 2019, 48, 1329–1336. [Google Scholar] [CrossRef]
- Chng, C.K.; Gandedkar, N.H.; Liou, E.J.W. Surgery-First Orthodontic Management: A Clinical Guide to a New Treatment Approach, 1st ed.; Springer International Publishing: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Chen, Y.R.; Huang, D.C.S. Surgery-First Approach in Orthognathic Surgery, 1st ed.; Taiwan Cleft Palate-Craniofacial Association: Taoyuan, Taiwan, 2019; ISBN 978-986-984-5304. [Google Scholar]
- Squire, D.; Best, A.M.; Lindauer, S.J.; Laskin, D.M. Determining the limits of orthodontic treatment of overbite, overjet, and transverse discrepancy: A pilot study. Am. J. Orthod. Dentofacial. Orthop. 2006, 129, 804–808. [Google Scholar] [CrossRef]
- Richardson, S.; Krishna, S.; Khandeparker, R.V. A comprehensive management protocol to treat cleft maxillary hypoplasia. J. Craniomaxillofac. Surg. 2018, 46, 356–361. [Google Scholar] [CrossRef]
- Martinez Plaza, A.; Bullejos Martínez, E.; Cariati, P.; Fernández-Valdés Gámez, R.; España López, A.; Fernández Valadés, R. Transversal maxillary distraction in patients with cleft lip and palate. J. Craniofac. Surg. 2019, 30, 1149–1153. [Google Scholar] [CrossRef]
- Carpentier, S.; van Gastel, J.; Schoenaers, J.; Carels, C.; Poorten, V.V.; Coucke, W.; Verdonck, A. Evaluation of transverse maxillary expansion after a segmental posterior subapical maxillary osteotomy in cleft lip and palate patients with severe collapse of the lateral maxillary segments. Cleft Palate Craniofac. J. 2014, 51, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.J.; Denadai, R.; Pai, B.C.J.; Lo, L.J. Digital occlusion setup is quantitatively comparable to the conventional dental model approach: Characteristics and guidelines for orthognathic surgery in patients with unilateral cleft lip and palate. Ann. Plast. Surg. 2019. [Google Scholar] [CrossRef]
- Ho, C.T.; Lin, H.H.; Lo, L.J. Intraoral scanning and setting up the digital final occlusion in three-dimensional planning of orthognathic surgery: Its comparison with the dental model approach. Plast. Reconstr. Surg. 2019, 143, 1027e–1036e. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hedo, R.; Rivera, A.; Rull, R.; Richardson, S.; Tu, X.M. Post hoc power analysis: Is it an informative and meaningful analysis? Gen. Psychiatr. 2019, 32, e100069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levine, M.; Ensom, M.H. Post hoc power analysis: An idea whose time has passed? Pharmacotherapy 2001, 21, 405–409. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Cleft Cohort (n = 21) |
|---|---|
| Maxillary dentition | |
| Missing tooth | |
| Yes/No n (%) | 12 (57.1%)/9 (42.9%) |
| Lateral incisor n (%) | 12 (57.1%) |
| Central incisor n (%) | 1 (4.8%) |
| First premolar n (%) | 1 (4.8%) |
| Spacing | |
| Yes/No n (%) | 3 (14.3%)/18 (85.7%) |
| Anterior crowding | |
| Yes/No n (%) | 21 (100%)/0 (0%) |
| Mild/Moderate/Severe n (%) | 6 (28.6%)/8 (38.1%)/7 (33.3%) |
| Posterior crowding | |
| Yes/No n (%) | 9 (42.9%)/12 (57.1%) |
| Mild/Moderate/Severe n (%) | 5 (55.6%)/2 (22.2%)/2 (22.2%) |
| Incisor relation | |
| Overjet | |
| Negative/Positive n (%) | 21 (100%)/0 (0%) |
| Negative/Positive (mm) m ± sd | −5.5 ± −3.8/– |
| Overbite | |
| Negative/Positive n (%) | 3 (14.3%)/18 (85.7%) |
| Negative/Positive (mm) m ± sd | −4.7 ± −1.5/2.6 ± 1.8 |
| Upper midline deviation | |
| Yes/No n (%) | 17 (81%)/4 (19%) |
| Yes/No (mm) m ± sd | 3.2 ± 1.8/– |
| Curve of Spee | |
| Cleft side n (%) | |
| Mild/Moderate/Severe | 10 (47.6%)/8 (38.1%)/3 (14.3%) |
| Noncleft side n (%) | |
| Mild/Moderate/Severe | 11 (52.4%)/7 (33.3%)/3 (14.3%) |
| Posterior crossbite (molar) | |
| Cleft side (Yes/No) n (%) | 9 (42.9%)/12 (57.1%) |
| Noncleft side (Yes/No) n (%) | 7 (33.3%)/14 (67.7%) |
| Parameters | Standard Surgery-First Model (n = 8) | Modified Surgery-First Model (n = 13) | p-Value |
|---|---|---|---|
| Dental-occlusion contacts | |||
| Number of segmental contacts * n (%) | |||
| Three segments | 6 (66.7%) | 11 (84.6%) | 0.425 |
| Two segments | 2 (33.3%) | 1 (7.7%) | |
| One segment | 0 (0%) | 1 (7.7%) | |
| Number of tooth contacts m ± sd | |||
| Anterior teeth | 1.88 ± 0.99 | 1.69 ± 1.03 | 0.694 |
| Premolar teeth | 2.88 ± 0.83 | 2.15 ± 2.88 | 0.139 |
| Molar teeth | 2.00 ± 1.41 | 2.92 ± 1.26 | 0.135 |
| Total | 6.75 ± 1.28 | 6.77 ± 2.05 | 0.981 |
| Incisor midpoint relation (mm) m ± sd | |||
| Overjet | 3.70 ± 2.26 | 3.07 ± 1.27 | 0.420 |
| Overbite | 1.27 ± 0.90 | 1.02 ± 0.98 | 0.574 |
| Midline deviation (mm) m ± sd | |||
| Upper midline deviation | 0.48 ± 0.53 | 1.10 ± 1.42 | 0.254 |
| Midline discrepancy | 1.36 ± 1.69 | 1.10 ± 0.93 | 0.687 |
| Pogonion deviation | 1.37 ± 1.06 | 1.61 ± 1.46 | 0.652 |
| Transverse discrepancy (mm) m ± sd | |||
| Maxillary intercanine distance | 29.70 ± 5.70 | 29.00 ± 6.45 | 0.804 |
| Maxillary intermolar distance | 49.93 ± 7.40 | 49.57 ± 4.05 | 0.888 |
| Mandibular intercanine distance | 28.85 ± 2.37 | 26.54 ± 2.60 | 0.055 |
| Mandibular intermolar distance | 47.55 ± 4.49 | 46.95 ± 2.54 | 0.700 |
| Ratio of intercanine distance | 1.03 ± 0.22 | 1.10 ± 0.23 | 0.535 |
| Ratio of intermolar distance | 1.05 ± 0.10 | 1.06 ± 0.11 | 0.791 |
| Canine lateral overjet discrepancy | 5.97 ± 3.89 | 4.30 ± 3.00 | 0.283 |
| First molar lateral overjet discrepancy | 3.10 ±1.94 | 2.24 ± 1.28 | 0.234 |
| Skeletal discrepancy m ± sd | |||
| ANB (°) | 3.00 ± 3.90 | 3.12 ± 3.29 | 0.937 |
| Advancement of A-point (mm) | 3.90 ± 1.53 | 5.68 ± 2.20 | 0.059 |
| Setback of B-point (mm) | −4.78 ± 3.59 | −5.93 ± 5.01 | 0.578 |
| Parameters | Surgery-First Approach (n = 21) | Conventional Approach (n = 23) | p-Value |
|---|---|---|---|
| Dental occlusion contacts | |||
| Number of segmental contacts * n (%) | |||
| Three segments | 17 (81.0) | 18 (78.3) | 0.873 |
| Two segments | 3 (14.3) | 3 (13.0) | |
| One segment | 1 (4.7) | 2 (8.7) | |
| Number of teeth contacts m ± sd | |||
| Anterior teeth | 1.76 ± 1.00 | 2.52 ± 1.38 | 0.044 |
| Premolar teeth | 2.42 ± 1.08 | 2.57 ± 1.04 | 0.670 |
| Molar teeth | 2.57 ± 1.36 | 2.04 ± 1.26 | 0.189 |
| Total | 6.76 ± 1.76 | 7.13 ± 2.30 | 0.557 |
| Incisor midpoint relation (mm) m ± sd | |||
| Overjet | 3.31 ± 1.69 | 2.12 ± 1.26 | 0.011 |
| Overbite | 1.11 ± 0.93 | 0.51 ± 1.25 | 0.077 |
| Midline deviation (mm) m ± sd | |||
| Upper midline deviation | 0.86 ± 1.18 | 0.83 ± 1.03 | 0.923 |
| Midline discrepancy | 1.21 ± 1.43 | 1.02 ± 1.18 | 0.634 |
| Pogonion deviation | 1.52 ± 1.30 | 1.44 ± 1.01 | 0.826 |
| Transverse discrepancy (mm) m ± sd | |||
| Maxillary intercanine distance | 29.27 ± 6.04 | 30.50 ± 5.60 | 0.485 |
| Maxillary intermolar distance | 49.70 ± 5.39 | 50.10 ± 3.69 | 0.774 |
| Mandibular intercanine distance | 27.42 ± 2.71 | 27.73 ± 1.31 | 0.625 |
| Mandibular intermolar distance | 47.18 ± 3.32 | 46.77 ± 3.39 | 0.687 |
| Ratio of intercanine distance | 1.07 ± 0.22 | 1.10 ± 0.22 | 0.646 |
| Ratio of intermolar distance | 1.06 ± 0.11 | 1.08 ± 0.09 | 0.515 |
| Canine lateral overjet discrepancy | 4.94 ± 3.37 | 3.60 ± 2.65 | 0.149 |
| First molar lateral overjet discrepancy | 2.57 ± 1.58 | 1.78 ± 1.34 | 0.080 |
| Skeletal discrepancy m ± sd | |||
| ANB (o) | 3.41 ± 3.55 | 2.54 ± 2.32 | 0.337 |
| Advancement of A-point (mm) | 5.00 ± 2.12 | 5.00 ± 1.84 | 0.997 |
| Setback of B-point (mm) | 5.49 ± 4.46 | 6.06 ± 5.06 | 0.698 |
| Cleft Side | Noncleft Side | |||||
|---|---|---|---|---|---|---|
| Parameters | Surgery-First Approach (n = 21) | Conventional Approach (n = 23) | p-Value | Surgery-First Approach (n = 21) | Conventional Approach (n = 23) | p-Value |
| Dental occlusion contact | ||||||
| Angle classification n (%) | ||||||
| Angle Class I | 2 (9.6) | 1 (4.3) | 0.496 | 1 (4.8) | 4 (17.4) | 0.257 |
| Angle Class II | 19 (90.4) | 22 (95.7) | 19 (90.4) | 19 (82.6) | ||
| Angle Class III | 0 (0) | 0 (0) | 1 (4.8) | 0 (0) | ||
| Number of tooth contact m ± sd | ||||||
| Anterior teeth | 0.76 ± 0.70 | 1.22 ± 0.67 | 0.033 | 1.00 ± 0.55 | 1.30 ± 1.11 | 0.249 |
| Premolar teeth | 1.24 ± 0.62 | 1.35 ± 0.65 | 0.571 | 1.19 ± 0.68 | 1.22 ± 0.67 | 0.896 |
| Molar teeth | 1.24 ± 0.89 | 1.00 ± 0.74 | 0.338 | 1.33 ± 0.86 | 1.04 ± 0.82 | 0.259 |
| Total | 3.24 ± 1.14 | 3.57 ± 1.34 | 0.390 | 3.52 ± 1.17 | 3.57 ± 1.41 | 0.916 |
| Dental inclination (o) m ± sd | ||||||
| U1 inclination | 98.37 ± 14.27 | 105.96 ± 9.73 | 0.044 | 101.72 ± 9.54 | 106.61 ± 8.13 | 0.074 |
| Interincisal angle | 135.20 ± 15.22 | 123.38 ± 12.64 | 0.007 | 130.64 ± 12.25 | 122.96 ± 11.36 | 0.037 |
| Anteroposterior relation (mm) m ± sd | ||||||
| U1 overjet | 3.24 ± 2.12 | 1.82 ± 1.27 | 0.009 | 3.39 ± 1.43 | 2.42 ± 1.44 | 0.030 |
| U6 overjet | 6.41 ± 3.85 | 7.16 ± 5.73 | 0.609 | 3.65 ± 4.27 | 4.29 ± 4.43 | 0.628 |
| Vertical relation of teeth | ||||||
| U1 overbite (mm) m ± sd | 0.80 ± 1.18 | 0.24 ± 1.31 | 0.144 | 1.43 ± 0.88 | 0.77 ± 1.29 | 0.057 |
| Posterior open bite (U7) n (%) | ||||||
| Yes | 11 (52.4) | 6 (26.1) | 0.041 | 13 (61.9) | 7 (30.4) | 0.035 |
| No | 10 (47.6) | 17 (73.9) | 8 (38.1) | 16 (69.6) | ||
| Transverse arch coordination m ± sd | ||||||
| Midline to U3 distance (mm) | 12.66 ± 3.41 | 14.02 ± 3.15 | 0.177 | 16.19 ± 3.57 | 16.18 ± 3.25 | 0.996 |
| Midline to L3 distance (mm) | 13.74 ± 2.89 | 14.03 ± 1.40 | 0.667 | 13.61 ± 2.62 | 13.89 ± 3.10 | 0.749 |
| Midline to canine ratio | 0.95 ± 0.29 | 1.02 ± 0.29 | 0.470 | 1.20 ± 0.24 | 1.17 ± 0.25 | 0.640 |
| Canine lateral overjet (mm) | −1.08 ± 3.79 | −0.01 ± 3.97 | 0.368 | 2.58 ± 2.94 | 2.29 ± 3.84 | 0.785 |
| Midline to U6 distance (mm) | 25.08 ± 2.97 | 24.89 ± 2.48 | 0.811 | 24.96 ± 3.73 | 25.18 ± 2.27 | 0.813 |
| Midline to L6 distance (mm) | 23.57 ± 2.88 | 23.49 ± 2.31 | 0.918 | 23.05 ± 2.27 | 23.11 ± 2.36 | 0.933 |
| Midline to first molar ratio | 1.07 ± 0.12 | 1.06 ± 0.11 | 0.838 | 1.08 ± 0.14 | 1.10 ± 0.09 | 0.749 |
| First molar lateral overjet | 1.52 ± 2.82 | 1.40 ± 2.43 | 0.883 | 1.91 ± 3.16 | 2.07±1.98 | 0.838 |
| Maxillary occlusion angle (o) m ± sd | −9.08 ± 7.27 | −11.79 ± 3.91 | 0.139 | −10.45 ± 5.51 | −10.99 ± 4.65 | 0.726 |
| Jaw movement (mm) m ± sd | ||||||
| Advancement of U3 | 4.12 ± 2.98 | 4.45 ± 2.54 | 0.698 | 3.49 ± 3.29 | 2.87 ± 2.20 | 0.467 |
| Impaction of U3 | 0.99 ± 2.40 | 0.50 ± 1.68 | 0.436 | 0.32 ± 2.02 | 0.22 ± 2.02 | 0.872 |
| Advancement of U6 | 4.43 ± 3.07 | 5.08 ± 3.08 | 0.492 | 3.34 ± 3.09 | 2.37 ± 2.73 | 0.277 |
| Impaction of U6 | −0.50 ± 1.31 | −0.49 ± 1.67 | 0.980 | −1.05 ± 1.70 | −1.12 ± 2.35 | 0.910 |
| Setback of mandible | −4.35 ± 4.73 | −4.90 ± 5.40 | 0.722 | −4.64 ± 4.18 | −6.24 ± 3.97 | 0.199 |
| Parameters | Cleft Cohort (n = 21) | Noncleft Cohort (n = 18) | p-Value |
|---|---|---|---|
| Dental-occlusion contact | |||
| Number of segmental contacts * n (%) | |||
| Three segments | 17 (81.0) | 15 (83.3) | 0.638 |
| Two segments | 3 (14.3) | 3 (16.7) | |
| One segment | 1 (4.7) | 0 (0) | |
| Number of teeth contacts m ± sd | |||
| Anterior teeth | 1.76 ± 1.00 | 2.50 ± 1.38 | 0.061 |
| Premolar teeth | 2.42 ± 1.08 | 2.22 ± 1.44 | 0.612 |
| Molar teeth | 2.57 ± 1.36 | 2.72 ± 1.18 | 0.716 |
| Total | 6.76 ± 1.76 | 7.44 ± 2.23 | 0.292 |
| Incisor midpoint relation (mm) m ± sd | |||
| Overjet | 3.31 ± 1.69 | 4.37 ± 1.27 | 0.036 |
| Overbite | 1.11 ± 0.93 | 1.46 ± 1.62 | 0.432 |
| Midline deviation (mm) m ± sd | |||
| Upper midline deviation | 0.86 ± 1.18 | 0.55 ± 0.42 | 0.287 |
| Midline discrepancy | 1.21 ± 1.43 | 0.54 ± 0.67 | 0.063 |
| Pogonion deviation | 1.52 ± 1.30 | 1.38 ± 1.46 | 0.749 |
| Transverse discrepancy (mm) m ± sd | |||
| Maxillary intercanine distance | 29.27 ± 6.04 | 36.04 ± 2.67 | <0.001 |
| Maxillary intermolar distance | 49.70 ± 5.39 | 54.61 ± 3.55 | 0.002 |
| Mandibular intercanine distance | 27.42 ± 2.71 | 27.12 ± 3.33 | 0.756 |
| Mandibular intermolar distance | 47.18 ± 3.32 | 47.31 ± 3.05 | 0.900 |
| Ratio of intercanine distance | 1.07 ± 0.22 | 1.34 ± 0.16 | <0.001 |
| Ratio of intermolar distance | 1.06 ± 0.11 | 1.16 ± 0.10 | 0.004 |
| Canine lateral overjet | 4.94 ± 3.37 | 1.37 ± 1.35 | <0.001 |
| First molar lateral overjet | 2.57 ± 1.58 | 2.30 ± 1.84 | 0.626 |
| Skeletal discrepancy m ± sd | |||
| ANB (o) | 3.41 ± 3.55 | 3.28 ±1.19 | 0.882 |
| Advancement of A-point (mm) | 5.00 ± 2.12 | 3.86 ± 1.52 | 0.066 |
| Setback of B-point (mm) | −5.49 ± 4.46 | −6.23 ± 3.34 | 0.567 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, H.J.; Denadai, R.; Pai, B.C.-J.; Lo, L.-J. Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup. J. Clin. Med. 2019, 8, 2116. https://doi.org/10.3390/jcm8122116
Seo HJ, Denadai R, Pai BC-J, Lo L-J. Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup. Journal of Clinical Medicine. 2019; 8(12):2116. https://doi.org/10.3390/jcm8122116
Chicago/Turabian StyleSeo, Hyung Joon, Rafael Denadai, Betty Chien-Jung Pai, and Lun-Jou Lo. 2019. "Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup" Journal of Clinical Medicine 8, no. 12: 2116. https://doi.org/10.3390/jcm8122116







