Long-Term Pancreatic Functional Impairment after Surgery for Neuroendocrine Neoplasms
Abstract
:1. Introduction
2. Experimental Section
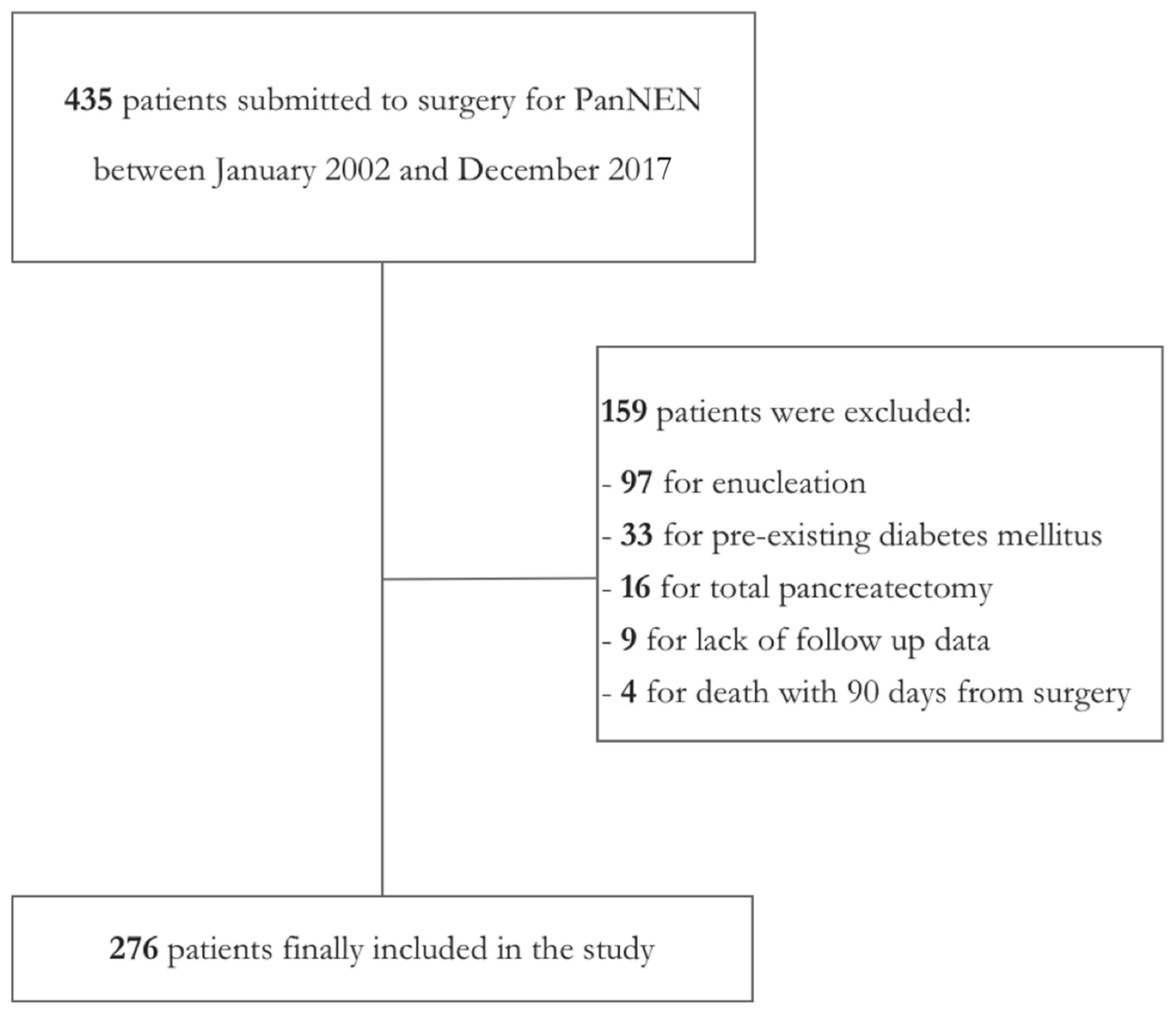
2.1. Study Design
2.2. Definition of Outcomes
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Postoperative DM
3.3. Postoperative PEI
3.4. Long-Term Oncological Outcomes
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Kuo, E.J.; Salem, R.R. Population-level analysis of pancreatic neuroendocrine tumors 2 cm or less in size. Ann. Surg. Oncol. 2013, 20, 2815–2821. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.V.; Osamura, R.Y.; Kloppel, G.; Rosai, J. WHO Classification of Tumours of Endocrine Organs, 4th ed.; Lloyd, R.V., Osamura, R.Y., Kloppel, G., Rosai, J., Eds.; IARC Press: Lyon, France, 2017. [Google Scholar]
- Partelli, S.; Javed, A.A.; Andreasi, V.; He, J.; Muffatti, F.; Weiss, M.J.; Sessa, F.; La Rosa, S.; Doglioni, C.; Zamboni, G.; et al. The number of positive nodes accurately predicts recurrence after pancreaticoduodenectomy for nonfunctioning neuroendocrine neoplasms. Eur. J. Surg. Oncol. 2018, 44, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Genc, C.G.; Jilesen, A.P.; Partelli, S.; Falconi, M.; Muffatti, F.; van Kemenade, F.J.; van Eeden, S.; Verheij, J.; van Dieren, S.; van Eijck, C.H.J.; et al. A New Scoring System to Predict Recurrent Disease in Grade 1 and 2 Nonfunctional Pancreatic Neuroendocrine Tumors. Ann. Surg. 2018, 267, 1148–1154. [Google Scholar] [CrossRef]
- Falconi, M.; Eriksson, B.; Kaltsas, G.; Bartsch, D.K.; Capdevila, J.; Caplin, M.; Kos-Kudla, B.; Kwekkeboom, D.; Rindi, G.; Kloppel, G.; et al. ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology 2016, 103, 153–171. [Google Scholar] [CrossRef]
- Phillips, M.E. Pancreatic exocrine insufficiency following pancreatic resection. Pancreatology 2015, 15, 449–455. [Google Scholar] [CrossRef]
- Halloran, C.M.; Cox, T.F.; Chauhan, S.; Raraty, M.G.T.; Sutton, R.; Neoptolemos, J.P.; Ghaneh, P. Partial pancreatic resection for pancreatic malignancy is associated with sustained pancreatic exocrine failure and reduced quality of life: A prospective study. Pancreatology 2011, 11, 535–545. [Google Scholar] [CrossRef]
- Armstrong, T.; Strommer, L.; Ruiz-Jasbon, F.; Shek, F.W.; Harris, S.F.; Permert, J.; Johnson, C.D. Pancreaticoduodenectomy for peri-ampullary neoplasia leads to specific micronutrient deficiencies. Pancreatology 2007, 7, 37–44. [Google Scholar] [CrossRef]
- Winny, M.; Paroglou, V.; Bektas, H.; Kaltenborn, A.; Reichert, B.; Zachau, L.; Kleine, M.; Klempnauer, J.; Schrem, H. Insulin dependence and pancreatic enzyme replacement therapy are independent prognostic factors for long-term survival after operation for chronic pancreatitis. Surg. (U. S.) 2014, 155, 271–279. [Google Scholar] [CrossRef]
- Iacono, C.; Verlato, G.; Ruzzenente, A.; Campagnaro, T.; Bacchelli, C.; Valdegamberi, A.; Bortolasi, L.; Guglielmi, A. Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br. J. Surg. 2013, 100, 873–885. [Google Scholar] [CrossRef]
- Santangelo, M.; Esposito, A.; Tammaro, V.; Calogero, A.; Criscitiello, C.; Roberti, G.; Candida, M.; Rupealta, N.; Pisani, A.; Carlomagno, N. What indication, morbidity and mortality for central pancreatectomy in oncological surgery? A systematic review. Int. J. Surg. 2016, 28, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Beger, H.G.; Siech, M.; Poch, B.; Mayer, B.; Schoenberg, M.H. Limited surgery for benign tumours of the pancreas: A systematic review. World J. Surg. 2015, 39, 1557–1566. [Google Scholar] [CrossRef] [PubMed]
- Gharios, J.; Hain, E.; Dohan, A.; Prat, F.; Terris, B.; Bertherat, J.; Coriat, R.; Dousset, B.; Gaujoux, S. Pre- and intraoperative diagnostic requirements, benefits and risks of minimally invasive and robotic surgery for neuroendocrine tumors of the pancreas. Best Pract. Res. Clin. Endocrinol. Metab. 2019. [Google Scholar] [CrossRef] [PubMed]
- Crippa, S.; Bassi, C.; Salvia, R.; Falconi, M.; Butturini, G.; Pederzoli, P. Enucleation of pancreatic neoplasms. Br. J. Surg. 2007, 94, 1254–1259. [Google Scholar] [CrossRef] [PubMed]
- Cauley, C.E.; Pitt, H.A.; Ziegler, K.M.; Nakeeb, A.; Schmidt, C.M.; Zyromski, N.J.; House, M.G.; Lillemoe, K.D. Pancreatic Enucleation: Improved Outcomes Compared to Resection. J. Gastrointest. Surg. 2012, 16, 1347–1353. [Google Scholar] [CrossRef]
- Paiella, S.; De Pastena, M.; Faustini, F.; Landoni, L.; Pollini, T.; Bonamini, D.; Giuliani, T.; Bassi, C.; Esposito, A.; Tuveri, M.; et al. Central pancreatectomy for benign or low-grade malignant pancreatic lesions—A single-center retrospective analysis of 116 cases. Eur. J. Surg. Oncol. 2019, 45, 788–792. [Google Scholar] [CrossRef]
- Falconi, M.; Zerbi, A.; Crippa, S.; Balzano, G.; Boninsegna, L.; Capitanio, V.; Bassi, C.; Di Carlo, V.; Pederzoli, P. Parenchyma-Preserving resections for small nonfunctioning pancreatic endocrine tumors. Ann. Surg. Oncol. 2010, 17, 1621–1627. [Google Scholar] [CrossRef]
- Falconi, M.; Mantovani, W.; Crippa, S.; Mascetta, G.; Salvia, R.; Pederzoli, P. Pancreatic insufficiency after different resections for benign tumours. Br. J. Surg. 2008, 95, 85–91. [Google Scholar] [CrossRef]
- Kwon, J.H.; Kim, S.C.; Shim, I.K.; Song, K.B.; Lee, J.H.; Hwang, D.W.; Park, K.M.; Lee, Y.J. Factors affecting the development of diabetes mellitus after pancreatic resection. Pancreas 2015, 44, 1296–1303. [Google Scholar] [CrossRef]
- Malka, D.; Hammel, P.; Sauvanet, A.; Rufat, P. Risk factors for diabetes mellitus in chronic pancreatitis. Gastroenterology 2000, 119, 1324–1332. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Partelli, S.; Boninsegna, L.; Salvia, R.; Bassi, C.; Pederzoli, P.; Falconi, M. Middle-preserving pancreatectomy for multicentric body-sparing lesions of the pancreas. Am. J. Surg. 2009, 198, 49–53. [Google Scholar] [CrossRef]
- Balzano, G.; Maffi, P.; Nano, R.; Mercalli, A.; Melzi, R.; Aleotti, F.; Zerbi, A.; De Cobelli, F.; Gavazzi, F.; Magistretti, P.; et al. Autologous Islet Transplantation in Patients Requiring Pancreatectomy: A Broader Spectrum of Indications Beyond Chronic Pancreatitis. Am. J. Transplant. 2016, 16, 1812–1826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Bassi, C.; Marchegiani, G.; Dervenis, C.; Sarr, M.; Abu Hilal, M.; Adham, M.; Allen, P.; Andersson, R.; Asbun, H.J.; Besselink, M.G.; et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 2017, 161, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Rindi, G.; Kloppel, G.; Couvelard, A.; Komminoth, P.; Korner, M.; Lopes, J.M.; McNicol, A.-M.; Nilsson, O.; Perren, A.; Scarpa, A.; et al. TNM staging of midgut and hindgut (neuro) endocrine tumors: A consensus proposal including a grading system. Virchows Arch. 2007, 451, 757–762. [Google Scholar] [CrossRef]
- Kusakabe, J.; Anderson, B.; Liu, J.; Williams, G.A.; Chapman, W.C.; Doyle, M.M.B.; Khan, A.S.; Sanford, D.E.; Hammill, C.W.; Strasberg, S.M.; et al. Long-Term Endocrine and Exocrine Insufficiency After Pancreatectomy. J. Gastrointest. Surg. 2019, 23, 1604–1613. [Google Scholar] [CrossRef]
- Shirakawa, S.; Matsumoto, I.; Toyama, H.; Shinzeki, M.; Ajiki, T.; Fukumoto, T.; Ku, Y. Pancreatic Volumetric Assessment as a Predictor of New-Onset Diabetes Following Distal Pancreatectomy. J. Gastrointest. Surg. 2012, 16, 2212–2219. [Google Scholar] [CrossRef] [Green Version]
- You, D.D.; Choi, S.H.; Choi, D.W.; Heo, J.S.; Ho, C.Y.; Kim, W.S. Long-term effects of pancreaticoduodenectomy on glucose metabolism. ANZ J. Surg. 2012, 82, 447–451. [Google Scholar] [CrossRef]
- Neophytou, H.; Wangermez, M.; Gand, E.; Carretier, M.; Danion, J.; Richer, J.-P. Predictive factors of endocrine and exocrine insufficiency after resection of a benign tumour of the pancreas. Ann. Endocrinol. (Paris) 2018, 79, 53–61. [Google Scholar] [CrossRef] [PubMed]
- King, J.; Kazanjian, K.; Matsumoto, J.; Reber, H.A.; Yeh, M.W.; Hines, O.J.; Eibl, G. Distal pancreatectomy: Incidence of postoperative diabetes. J. Gastrointest. Surg. 2008, 12, 1548–1553. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Jang, J.Y.; Hwang, D.W.; Lee, K.U.; Kim, S.W. Clinical efficacy of organ-preserving pancreatectomy for benign or low-grade malignant potential lesion. J. Korean Med. Sci. 2010, 25, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Shoup, M.; Brennan, M.F.; McWhite, K.; Leung, D.H.Y.; Klimstra, D.; Conlon, K.C. The value of splenic preservation with distal pancreatectomy. Arch. Surg. 2002, 137, 164–168. [Google Scholar] [CrossRef]
- Hirata, K.; Nakata, B.; Amano, R.; Yamazoe, S.; Kimura, K.; Hirakawa, K. Predictive Factors for Change of Diabetes Mellitus Status After Pancreatectomy in Preoperative Diabetic and Nondiabetic Patients. J. Gastrointest. Surg. 2014, 18, 1597–1603. [Google Scholar] [CrossRef]
- Nguyen, N.T.; Nguyen, X.M.T.; Lane, J.; Wang, P. Relationship between obesity and diabetes in a US adult population: Findings from the national health and nutrition examination survey, 1999–2006. Obes. Surg. 2011, 21, 351–355. [Google Scholar] [CrossRef]
- Mann, S.T.W.; Stracke, H.; Lange, U.; Klör, H.U.; Teichmann, J. Vitamin D3 in patients with various grades of chronic pancreatitis, according to morphological and functional criteria of the pancreas. Dig. Dis. Sci. 2003, 48, 533–538. [Google Scholar] [CrossRef]
- Lim, P.W.; Dinh, K.H.; Sullivan, M.; Wassef, W.Y.; Zivny, J.; Whalen, G.F.; LaFemina, J. Thirty-day outcomes underestimate endocrine and exocrine insufficiency after pancreatic resection. HPB 2016, 18, 360–366. [Google Scholar] [CrossRef] [Green Version]
- Matsumoto, J.; Traverso, L.W. Exocrine Function Following the Whipple Operation as Assessed by Stool Elastase. J. Gastrointest. Surg. 2006, 10, 1225–1229. [Google Scholar] [CrossRef]
- Capurso, G.; Traini, M.; Piciucchi, M.; Signoretti, M.; Arcidiacono, P.G. Exocrine pancreatic insufficiency: Prevalence, diagnosis, and management. Clin. Exp. Gastroenterol. 2019, 12, 129–139. [Google Scholar] [CrossRef]
- Kachare, S.D.; Fitzgerald, T.L.; Schuth, O.; Vohra, N.A.; Zervos, E.E. The impact of pancreatic resection on exocrine homeostasis. Am. Surg. 2014, 80, 704–709. [Google Scholar] [PubMed]
- Benini, L.; Gabbrielli, A.; Cristofori, C.; Amodio, A.; Butturini, G.; Cardobi, N.; Sozzi, C.; Frulloni, L.; Mucelli, R.P.; Crinò, S.; et al. Residual pancreatic function after pancreaticoduodenectomy is better preserved with pancreaticojejunostomy than pancreaticogastrostomy: A long-term analysis. Pancreatology 2019, 9, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.C.K.; Van Lanschot, J.J.B.; Bruno, M.J.; Van Eijck, C.H.J. Functional changes after pancreatoduodenectomy: Diagnosis and treatment. Pancreatology 2009, 9, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Bettini, R.; Partelli, S.; Boninsegna, L.; Capelli, P.; Crippa, S.; Pederzoli, P.; Scarpa, A.; Falconi, M. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery 2011, 150, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Gaujoux, S.; Partelli, S.; Maire, F.; D’Onofrio, M.; Larroque, B.; Tamburrino, D.; Sauvanet, A.; Falconi, M.; Ruszniewski, P. Observational study of natural history of small sporadic nonfunctioning pancreatic neuroendocrine tumors. J. Clin. Endocrinol. Metab. 2013, 98, 4784–4789. [Google Scholar] [CrossRef] [PubMed]
- Benini, L.; Amodio, A.; Campagnola, P.; Agugiaro, F.; Cristofori, C.; Micciolo, R.; Magro, A.; Gabbrielli, A.; Cabrini, G.; Moser, L.; et al. Fecal elastase-1 is useful in the detection of steatorrhea in patients with pancreatic diseases but not after pancreatic resection. Pancreatology 2013, 13, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Morifuji, M.; Murakami, Y.; Uemura, K.; Ohge, H.; Hayashidani, Y.; Sudo, T.; Sueda, T. Usefulness of a 13C-labeled mixed triglyceride breath test for assessing pancreatic exocrine function after pancreatic surgery. Surgery 2009, 145, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, S.; Agnes, A.; Rosa, F.; Di Miceli, D.; Grieco, D.L.; Scaldaferri, F.; Gasbarrini, A.; Doglietto, G.B.; Quero, G. Long-term pancreatic exocrine and endometabolic functionality after pancreaticoduodenectomy. Comparison between pancreaticojejunostomy and pancreatic duct occlusion with fibrin glue. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 4310–4318. [Google Scholar]
- Lamarca, A.; McCallum, L.; Nuttall, C.; Barriuso, J.; Backen, A.; Frizziero, M.; Leon, R.; Mansoor, W.; McNamara, M.G.; Hubner, R.A.; et al. Somatostatin analogue-induced pancreatic exocrine insufficiency in patients with neuroendocrine tumors: Results of a prospective observational study. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 723–731. [Google Scholar] [CrossRef]
| Variable | n (%) |
|---|---|
| Operative time, min 1 | 240 (180;300) |
| Length of stay, days 1 | 9 (7;11) |
| Readmission | |
| No | 242 (88) |
| Yes | 34 (12) |
| Blood transfusion | |
| No | 229 (83) |
| Yes | 47 (17) |
| Islet autotransplatation | |
| No | 267 (97) |
| Yes | 9 (3) |
| Complications [26] | |
| No complications | 94 (34) |
| I | 56 (20) |
| II | 89 (32) |
| III | 36 (13) |
| IV | 1 (1) |
| POPF [27] | |
| No | 147 (53) |
| Yes | 129 (47) |
| Abdominal Collection | |
| No | 223 (81) |
| Yes | 53 (19) |
| Postoperative Hemorrhage | |
| No | 262 (95) |
| Yes | 14 (5) |
| Variable | Total Population | No Postoperative DM | Postoperative DM | p Value |
|---|---|---|---|---|
| n = 276 | n = 210 | n = 68 | ||
| Age, years | 58 (49;67) | 56 (46;67) | 60 (56;67) | 0.002 |
| Gender | ||||
| Male | 138 (50) | 95 (46) | 43 (63) | |
| Female | 138 (50) | 113 (54) | 25 (37) | 0.017 |
| Preoperative BMI, Kg/m2 | 25 (22;27) | 24 (22;27) | 27 (25;30) | <0.0001 |
| PanNEN functionality | ||||
| Nonfunctioning | 225 (82) | 163 (78) | 62 (91) | |
| Functioning | 51 (18) | 45 (22) | 6 (9) | 0.019 |
| Inherited Syndrome | ||||
| No | 261 (95) | 194 (93) | 67 (99) | |
| Yes | 15 (5) | 14 (7) | 1 (1) | 0.127 |
| Type of Surgery | ||||
| Pancreaticoduodenectomy | 76 (27) | 61 (29) | 15 (22) | |
| Distal Pancreatectomy | 192 (70) | 141 (68) | 51 (75) | |
| Atypical Resection | 8 (3) | 6 (3) | 2 (3) | 0.476 |
| T stage [28] | ||||
| T1–T2 | 180 (65) | 136 (65) | 44 (65) | |
| T3–T4 | 96 (35) | 72 (35) | 24 (35) | 0.919 |
| Tumor grade [3] | ||||
| G1 | 153 (55) | 110 (53) | 43 (63) | |
| G2 | 110 (40) | 85 (41) | 25 (37) | |
| G3 | 13 (5) | 13 (6) | 0 (0) | 0.065 |
| Complications [26] | ||||
| No-I-II | 239 (87) | 179 (85) | 60 (88) | |
| III-IV | 37 (13) | 29 (15) | 8 (12) | 0.647 |
| Variable | OR | 95% C.I. | p |
|---|---|---|---|
| Gender | |||
| Male | 1 | - | |
| Female | 0.481 | 0.178–1.305 | 0.151 |
| Age | |||
| ≤60 years | 1 | - | |
| >60 years | 0.972 | 0.366–2.579 | 0.954 |
| Preoperative BMI | |||
| ≤25 Kg/m2 | 1 | - | |
| >25 Kg/m2 | 4.945 | 1.889–12.943 | 0.001 |
| Type of PanNEN | |||
| Nonfunctioning | 1 | - | |
| Functioning | 0.269 | 0.071–1.022 | 0.054 |
| Variable | Total Population | No Postoperative PEI | Postoperative PEI | p Value |
|---|---|---|---|---|
| n = 276 | n = 158 | n = 118 | ||
| Age, years | 58 (49;67) | 58 (49;65) | 60 (47;68) | 0.556 |
| Gender | ||||
| Male | 138 (50) | 76 (48) | 62 (53) | |
| Female | 138 (50) | 82 (52) | 56 (47) | 0.543 |
| BMI, Kg/m2 | 24.5 (22.5;27) | 25 (23;28) | 24 (22;25) | 0.005 |
| Type of PanNEN | ||||
| Non-functioning | 225 (82) | 123 (78) | 102 (86) | |
| Functioning | 51 (18) | 35 (22) | 16 (14) | 0.085 |
| Inherited Syndrome | ||||
| No | 261 (95) | 150 (95) | 111 (94) | |
| Yes | 15 (5) | 8 (5) | 7 (6) | 0.793 |
| Type of Surgery | ||||
| Pancreaticoduodenectomy | 76 (27) | 8 (5) | 68 (58) | |
| Distal Pancreatectomy | 192 (70) | 144 (91) | 48 (41) | |
| Atypical Resection | 8 (3) | 6 (4) | 2 (1) | <0.0001 |
| T stage [28] | ||||
| T1–T2 | 180 (65) | 116 (73) | 64 (54) | |
| T3–T4 | 96 (35) | 42 (27) | 54 (46) | 0.001 |
| Tumor grade [3] | ||||
| G1 | 153 (55) | 96 (61) | 57 (48) | |
| G2 | 110 (40) | 55 (35) | 55 (47) | |
| G3 | 13 (5) | 7 (4) | 6 (5) | 0.108 |
| Complications [26] | ||||
| No-I-II | 239 (87) | 143 (91) | 96 (81) | |
| III-IV | 37 (13) | 15 (9) | 22 (19) | 0.027 |
| Variable | OR | 95% C.I. | p |
|---|---|---|---|
| BMI | |||
| ≤25 Kg/m2 | 1 | - | |
| >25 Kg/m2 | 0.746 | 0.280–1.989 | 0.558 |
| Type of Surgery | |||
| Distal Pancreatectomy | 1 | - | |
| Pancreaticoduodenectomy | 31.68 | 10.622–94.487 | <0.0001 |
| Atypical resection | 4.8 | 0.626–36.818 | 0.131 |
| T stage [28] | |||
| T1–T2 | 1 | - | |
| T3–T4 | 1.245 | 0.461–3.365 | 0.665 |
| Complications [26] | |||
| No-I–II | 1 | - | |
| III–IV | 1.464 | 0.330–6.486 | 0.616 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreasi, V.; Partelli, S.; Capurso, G.; Muffatti, F.; Balzano, G.; Crippa, S.; Falconi, M. Long-Term Pancreatic Functional Impairment after Surgery for Neuroendocrine Neoplasms. J. Clin. Med. 2019, 8, 1611. https://doi.org/10.3390/jcm8101611
Andreasi V, Partelli S, Capurso G, Muffatti F, Balzano G, Crippa S, Falconi M. Long-Term Pancreatic Functional Impairment after Surgery for Neuroendocrine Neoplasms. Journal of Clinical Medicine. 2019; 8(10):1611. https://doi.org/10.3390/jcm8101611
Chicago/Turabian StyleAndreasi, Valentina, Stefano Partelli, Gabriele Capurso, Francesca Muffatti, Gianpaolo Balzano, Stefano Crippa, and Massimo Falconi. 2019. "Long-Term Pancreatic Functional Impairment after Surgery for Neuroendocrine Neoplasms" Journal of Clinical Medicine 8, no. 10: 1611. https://doi.org/10.3390/jcm8101611




