Sex-Differences in the Pattern of Comorbidities, Functional Independence, and Mortality in Elderly Inpatients: Evidence from the RePoSI Register
Abstract
:1. Introduction
2. Material and Methods
Statistical Analysis
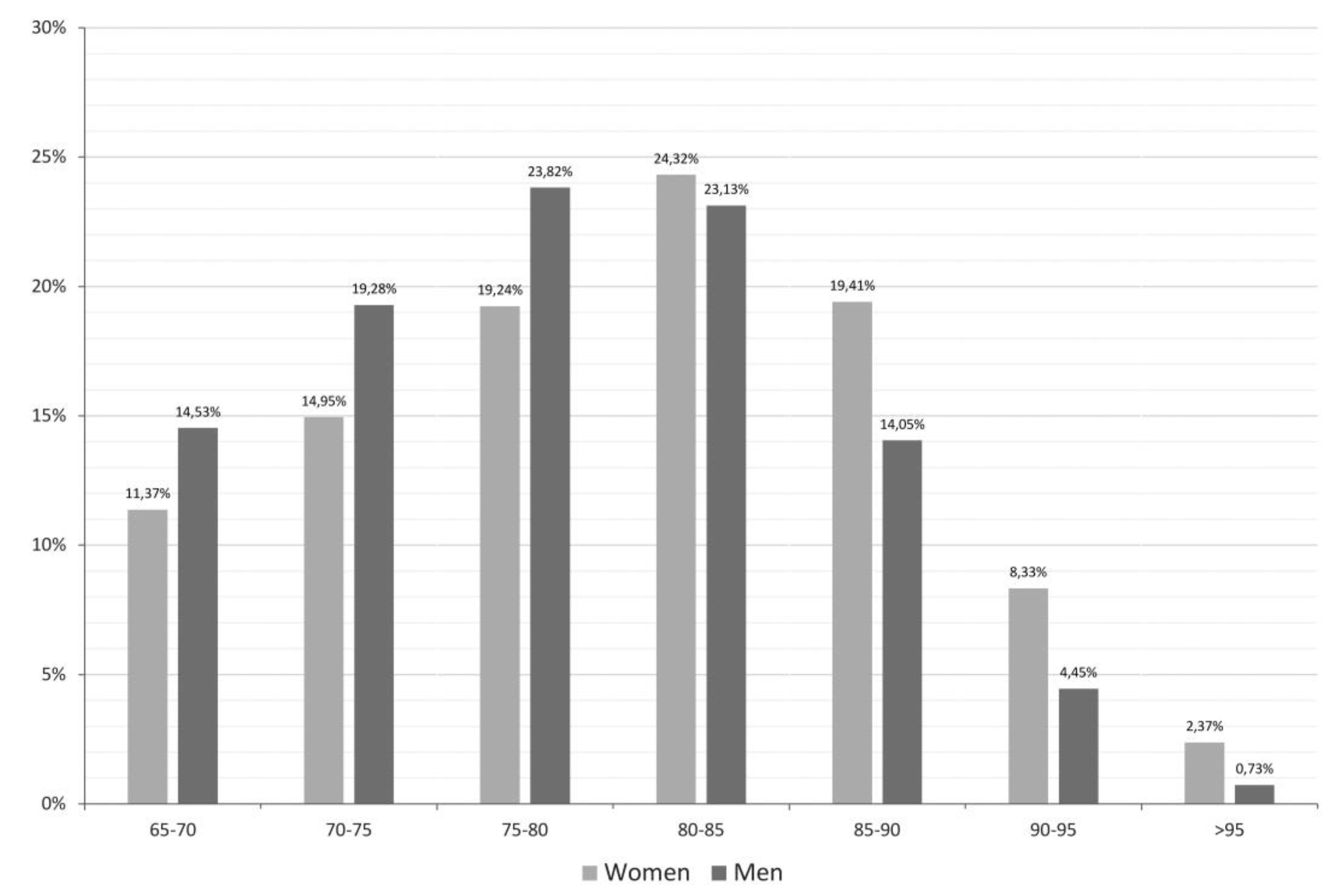
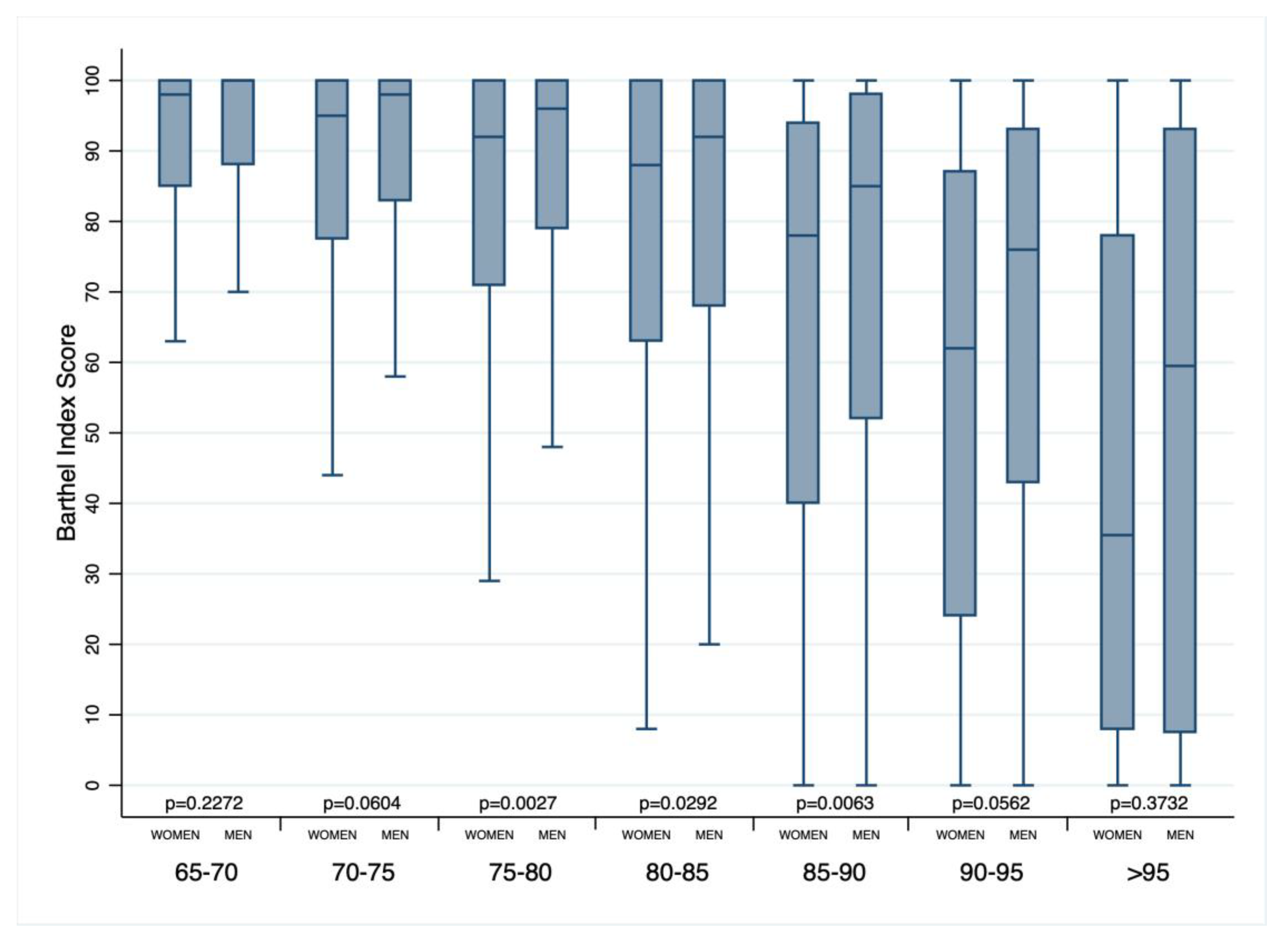
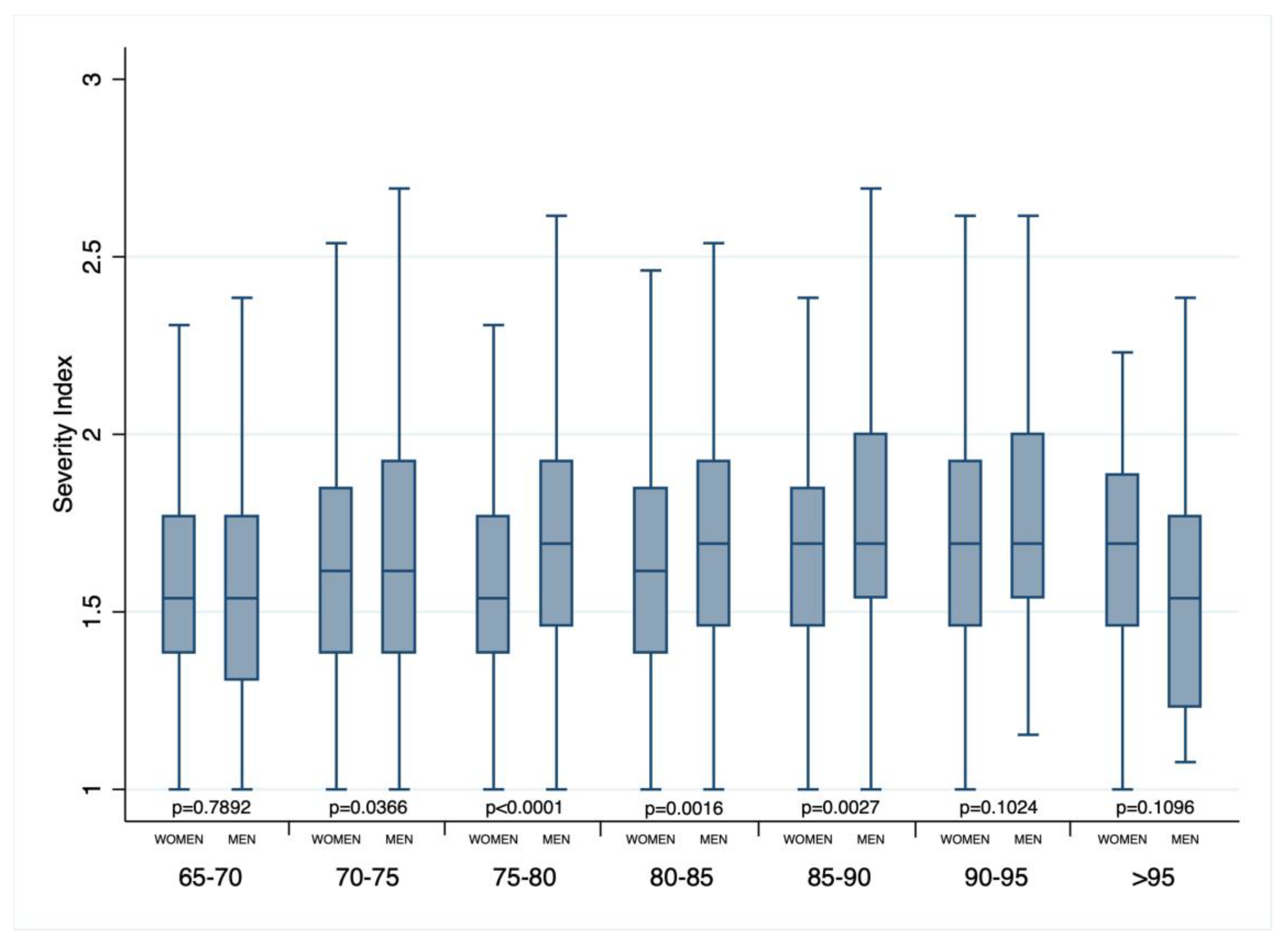
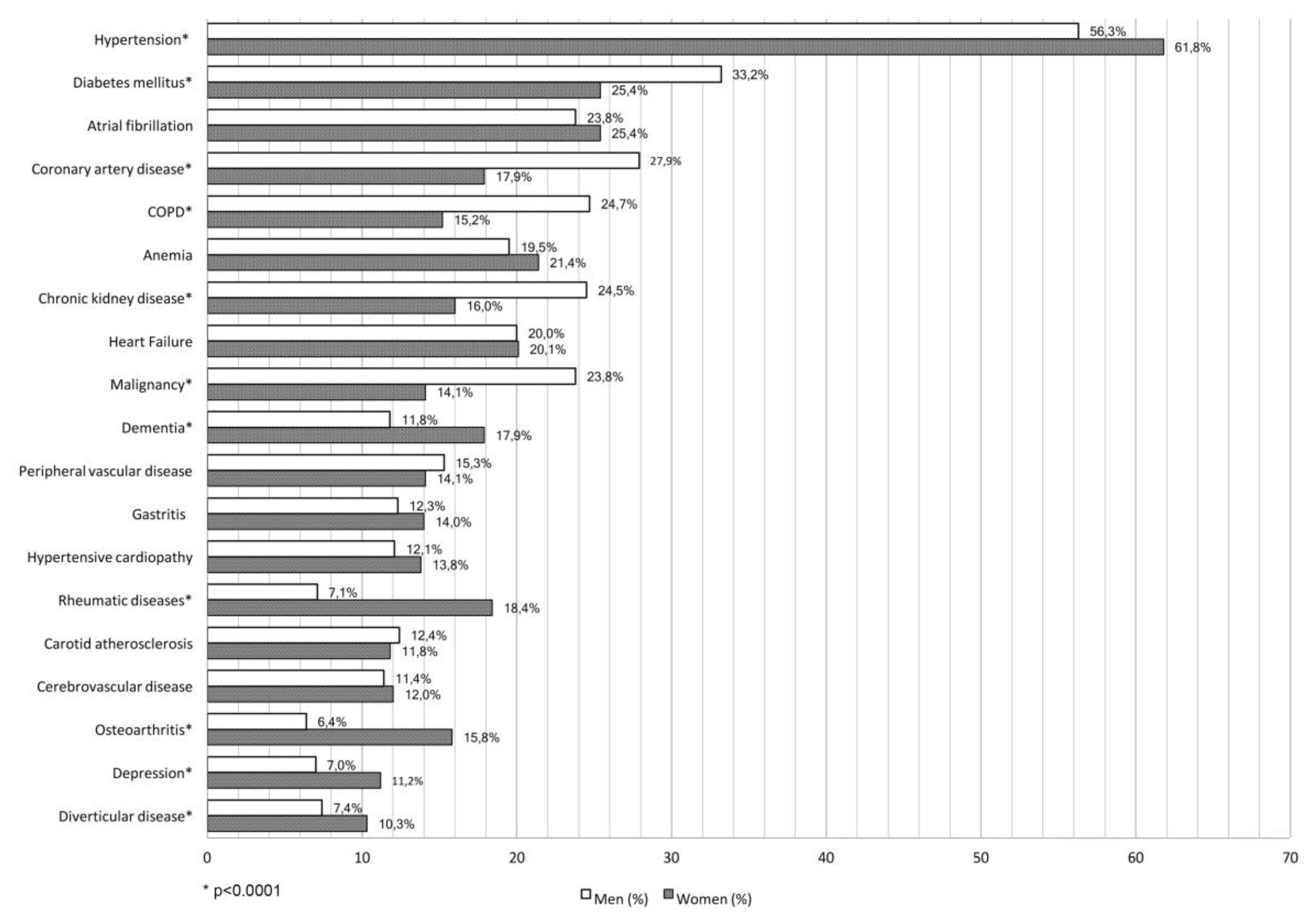
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Supplementary File 1Author Contributions
Funding
Conflicts of Interest
References
- The 2015 Aging Report European Commission. Available online: http://ec.europa.eu/economy_finance/publications/european_economy/2015/ee3_en.htm (accessed on 13 September 2018).
- Maas, A.H.; van der Schouw, Y.T.; Regitz-Zagrosek, V.; Swahn, E.; Appelman, Y.E.; Pasterkamp, G.; Ten Cate, H.; Nilsson, P.M.; Huisman, M.V.; Stam, H.C.; et al. Red alert for women’s heart: More research and knowledge on cardiovascular disease in women. Eur. Heart J. 2011, 32, 1362–1368. [Google Scholar] [CrossRef]
- Santalucia, P.; Franchi, C.; Djade, C.D.; Tettamanti, M.; Pasina, L.; Corrao, S.; Salerno, F.; Marengoni, A.; Marcucci, M.; Nobili, A.; et al. REPOSI Investigators. Gender difference in drug use in hospitalized elderly patients. Eur. J. Intern. Med. 2015, 26, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Corrao, S.; Santalucia, P.; Argano, C.; Djade, C.D.; Barone, E.; Tettamanti, M.; Pasina, L.; Franchi, C.; Kamal Eldin, T.; Marengoni, A.; et al. REPOSI Investigators. Gender-differences in disease distribution and outcome in hospitalized elderly: Data from the REPOSI study. Eur. J. Intern. Med. 2014, 25, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Nobili, A.; Licata, G.; Salerno, F.; Pasina, L.; Tettamanti, M.; Franchi, C.; De Vittorio, L.; Marengoni, A.; Corrao, S.; Iorio, A.; et al. SIMI Investigators. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur. J. Clin. Pharmacol. 2011, 67, 507–519. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Katzman, R.; Brown, T.; Fuld, P.; Peck, A.; Schechter, R.; Schimmel, H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am. J. Psychiatry 1983, 140, 734–739. [Google Scholar] [PubMed]
- Hickie, C.; Snowdon, J. Depression scales for the elderly: GDS, Gilleard, Zung. Clin. Gerontol. J. Aging Ment. Health 1987, 6, 51–53. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Linn, B.S.; Linn, M.W.; Gurel, L. Cumulative illness rating scale. J. Am. Geriatr. Soc. 1968, 16, 622–626. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression; J Wiley: New York, NY, USA, 2002. [Google Scholar]
- Global Population Ageing: Peril or Promise? World Economic Forum, 2012. Available online: http://demographic-challenge.com/files/downloads/6c59e8722eec82f7ffa0f1158d0f4e59/ageingbook_010612.pdf (accessed on 3 October 2018).
- Pan, A.; Okereke, O.I.; Sun, Q.; Logroscino, G.; Manson, J.E.; Willett, W.C.; Ascherio, A.; Hu, F.B.; Rexrode, K.M. Depression and incident stroke in women. Stroke 2011, 42, 2770–2775. [Google Scholar] [CrossRef] [PubMed]
- Whang, W.; Kubzansky, L.D.; Kawachi, I.; Rexrode, K.M.; Kroenke, C.H.; Glynn, R.J.; Garan, H.; Albert, C.M. Depression and risk of sudden cardiac death and coronary heart disease in women: Results from the Nurses’ Health Study. J. Am. Coll. Cardiol. 2009, 53, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, S.; Wolf, P.A.; Beiser, A.; Au, R.; McNulty, K.; White, R.; D’Agostino, R.B. Lifetime risk of dementia and Alzheimer’s disease. Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham Study. Neurology 1997, 49, 1498–1504. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.A.; Choudhury, K.R.; Rathakrishnan, B.G.; Marks, D.M.; Petrella, J.R.; Doraiswamy, P.M. Alzheimer’s Disease Neuroimaging Initiative. Marked gender differences in progression of mild cognitive impairment over 8 years. Alzheimers Dement. (N. Y.) 2015, 1, 103–110. [Google Scholar]
- Meyer, M.R.; Tschanz, J.T.; Norton, M.C.; Welsh-Bohmer, K.A.; Steffens, D.C.; Wyse, B.W.; Breitner, J.C. APOE genotype predicts when—Not whether—One is predisposed to develop Alzheimer disease. Nat. Genet. 1998, 19, 321–322. [Google Scholar] [CrossRef] [PubMed]
- Payami, H.; Zareparsi, S.; Montee, K.R.; Sexton, G.J.; Kaye, J.A.; Bird, T.D.; Yu, C.E.; Wijsman, E.M.; Heston, L.L.; Litt, M.; et al. Gender difference in apolipoprotein E-associated risk for familial Alzheimer disease: A possible clue to the higher incidence of Alzheimer disease in women. Am. J. Hum. Genet. 1996, 58, 803–811. [Google Scholar] [PubMed]
- Bretsky, P.M.; Buckwalter, J.G.; Seeman, T.E.; Miller, C.A.; Poirier, J.; Schellenberg, G.D.; Finch, C.E.; Henderson, V.W. Evidence for an interaction between apolipoprotein E genotype, gender, and Alzheimer disease. Alzheimer Dis. Assoc. Disord. 1999, 13, 216–221. [Google Scholar] [CrossRef]
- Fukumoto, N.; Fujii, T.; Combarros, O.; Kamboh, M.I.; Tsai, S.J.; Matsushita, S.; Nacmias, B.; Comings, D.E.; Arboleda, H.; Ingelsson, M.; et al. Sexually dimorphic effect of the Val66Met polymorphism of BDNF on susceptibility to Alzheimer’s disease: New data and meta-analysis. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2010, 153B, 235–242. [Google Scholar]
- Sohrabji, F.; Miranda, R.C.; Toran-Allerand, C.D. Identification of a putative estrogen response element in the gene encoding brain-derived neurotrophic factor. Proc. Natl. Acad. Sci. USA 1995, 92, 11110–11114. [Google Scholar] [CrossRef]
- Fried, L.P.; Bandeen-Roche, K.; Kasper, J.D. Guralnik JM for the Women’s Health and Aging Study collaborative research group. J. Clin. Epidemiol. 1999, 52, 27–37. [Google Scholar] [CrossRef]
- Camp, P.G.; Goring, S.M. Gender and the diagnosis, management, and surveillance of chronic obstructive pulmonary disease. Proc. Am. Thracic Soc. 2007, 4, 686–691. [Google Scholar] [CrossRef]
- Dransfield, M.T.; Washko, G.R.; Foreman, M.G.; Estepar, R.S.; Reilly, J. Gender differences in the severity of CT emphysema in COPD. Chest 2007, 132, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Molarius, A.; Janson, S. Self-rated health, chronic diseases, and symptoms among middle-aged and elderly men and women. J. Clin. Epidemiol. 2002, 55, 364–370. [Google Scholar] [CrossRef]
- Orshal, J.M.; Khalil, R.A. Gender, sex hormones, and vascular tone. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004, 286, R233–R249. [Google Scholar] [CrossRef] [Green Version]
- Oliver, J.E.; Silman, A.J. Why are women predisposed to autoimmune rheumatic diseases? Arthritis Res. Ther. 2009, 11, 252–260. [Google Scholar] [CrossRef]
- Cutolo, M.; Cappellino, S.; Sulli, A.; Serioli, B.; Secchi, M.E.; Villaggio, B.; Straub, R.H. Estrogens and autoimmune diseases. Ann. N. Y. Acad. Sci. 2006, 1089, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Shin, H.J.; Ding, E.L.; van Dam, R.M. Adiponectin levels and risk of type 2 diabetes: A systematic review and meta-analysis. JAMA 2009, 302, 179–188. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Karigas, G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol. Rev. 2017, 97, 1–37. [Google Scholar] [CrossRef]
- Bello, N.; Mosca, L. Epidemiology of coronary heart disease in women. Prog. Cardiovasc. Dis. 2004, 46, 287–295. [Google Scholar] [CrossRef]
- Corrao, S.; Marengoni, A.; Natoli, G.; Nobili, A.; Mannucci, P.; Perticone, F. Clinical Severity, Age, and Sex Overcome Cardiometabolic Morbidities but Not Stroke as Predictors of Mortality in Elderly Inpatients: Data From the REgistro POliterapie Società Italiana di Medicina Interna Registry. J. Am. Geriatr. Soc. 2016, 64, 1737–1739. [Google Scholar] [CrossRef]
- Corrao, S.; Argano, C.; Natoli, G.; Nobili, A.; Corazza, G.R.; Mannucci, P.M.; Perticone, F. REPOSI Investigators. Disability, and not diabetes, is a strong predictor of mortality in oldest old patients hospitalized with pneumonia. Eur. J. Intern. Med. 2018, 54, 53–59. [Google Scholar] [CrossRef]
- Satish, S.; Freeman, D.H., Jr.; Ray, L.; Goodwin, J.S. The relationship between blood pressure and mortality in the oldest old. J. Am. Geriatr. Soc. 2001, 49, 367–374. [Google Scholar] [CrossRef]
- Odden, M.C.; Peralta, C.A.; Haan, M.N.; Covinsky, K. Rethinking the association of high blood pressure with mortality in elderly adults: The impact of frailty. Arch. Intern. Med. 2012, 172, 1162–1168. [Google Scholar] [CrossRef]
| Variables | Women | Men | p |
|---|---|---|---|
| N of subjects | 2401 | 2313 | / |
| Age (years) a | 80.3 (80–80.7) | 78.4 (78.1–78.7) | <0.0001 |
| Systolic blood pressure (mm Hg) a | 132.1 (131.2–132.9) | 131.7 (130.8–132.5) | 0.5840 |
| Diastolic blood pressure (mm Hg) a | 73.5 (73.0–73.9) | 73.5 (73.1–74.0) | 0.7881 |
| eGFR (mL/min) a | 58.1 (57.1–59.0) | 60.5 (59.5–61.6) | 0.0003 |
| Hemoglobin (g/L) a | 11.6 (11.5–11.7) | 12.1 (12.0–12.2) | <0.0001 |
| Body mass index (kg/m2) a | 26.1 (25.8–26.3) | 25.8 (25.6–25.9) | 0.7880 |
| Barthel index (disability) a | 74.5 (73.3–75.8) | 80.6 (79.5–81.8) | <0.0001 |
| Barthel index ≤ 40 (disability) (%) | 17.1 | 11.8 | <0.0001 |
| Geriatric Depression Scale (GDS) a | 1.51 (1.45–1.56) | 1.27 (1.22–1.33) | <0.0001 |
| Comorbidity index (CIRS) a | 2.92 (2.84–2.99) | 3.18 (3.10–3.26) | <0.0001 |
| Severity index (CIRS) a | 1.64 (1.63–1.65) | 1.69 (1.68–1.71) | <0.0001 |
| Length of hospital stay (days) a | 11.8 (11.3–12.3) | 11.9 (11.3–12.6) | 0.2413 |
| In-hospital mortality (%) | 4.8 | 6.1 | 0.0545 |
| 3-month mortality (%) | 13.9 | 19.7 | <0.0001 |
| 1-year mortality (%) | 46.8 | 58.2 | 0.0001 |
| Fasting glucose (mmol/L) a | 125.6 (123.2–128.0) | 129.4 (126.6–132.2) | 0.2013 |
| Creatinine (μmol/L) a | 1.12 (1.09–1.16) | 1.41 (1.37–1.45) | <0.0001 |
| Cholesterol (mmol/L) a | 168.3 (166.1–170.4) | 150.6 (148.5–152.7) | <0.0001 |
| Cognitive impairment (SBT score) a | 9.74 (9.40–10.09) | 8.50 (8.17–8.84) | <0.0001 |
| Cognitive impairment (SBT score ≥ 10) (%) | 39.0 | 32.7 | <0.0001 |
| Number of drugs at hospital admission a | 5.6 (5.5–5.7) | 5.9 (5.8–6.0) | 0.0022 |
| Number of drugs at hospital discharge a | 7.6 (7.5–7.8) | 7.7 (7.5–7.9) | 0.2524 |
| Number of drugs at follow-up 3-month a | 6.5 (6.3–6.6) | 6.7 (6.5–6.9) | 0.0983 |
| Number of drugs at follow-up 1-year a | 6.4 (6.0–6.8) | 6.5 (6.1–7.0) | 0.5517 |
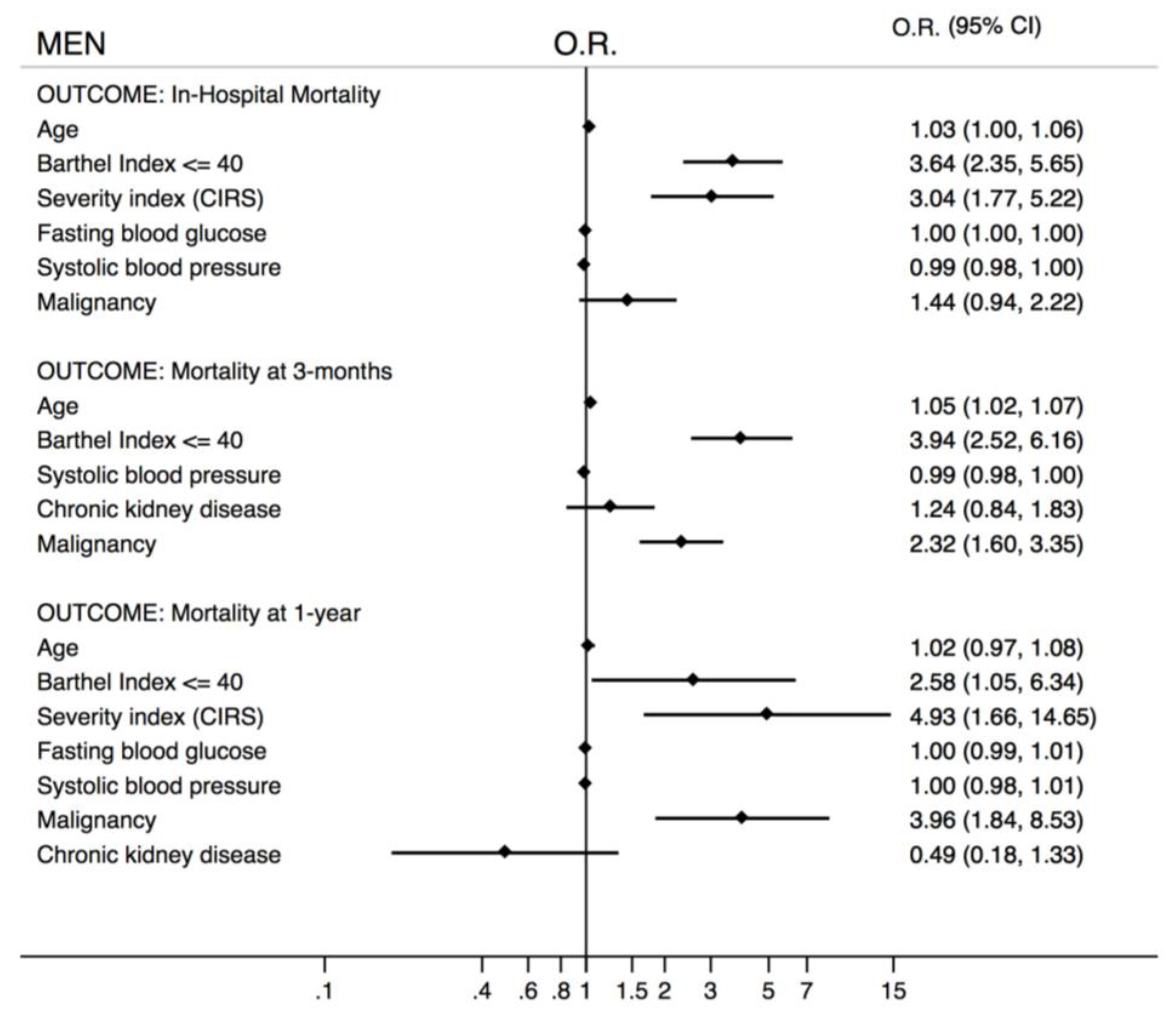
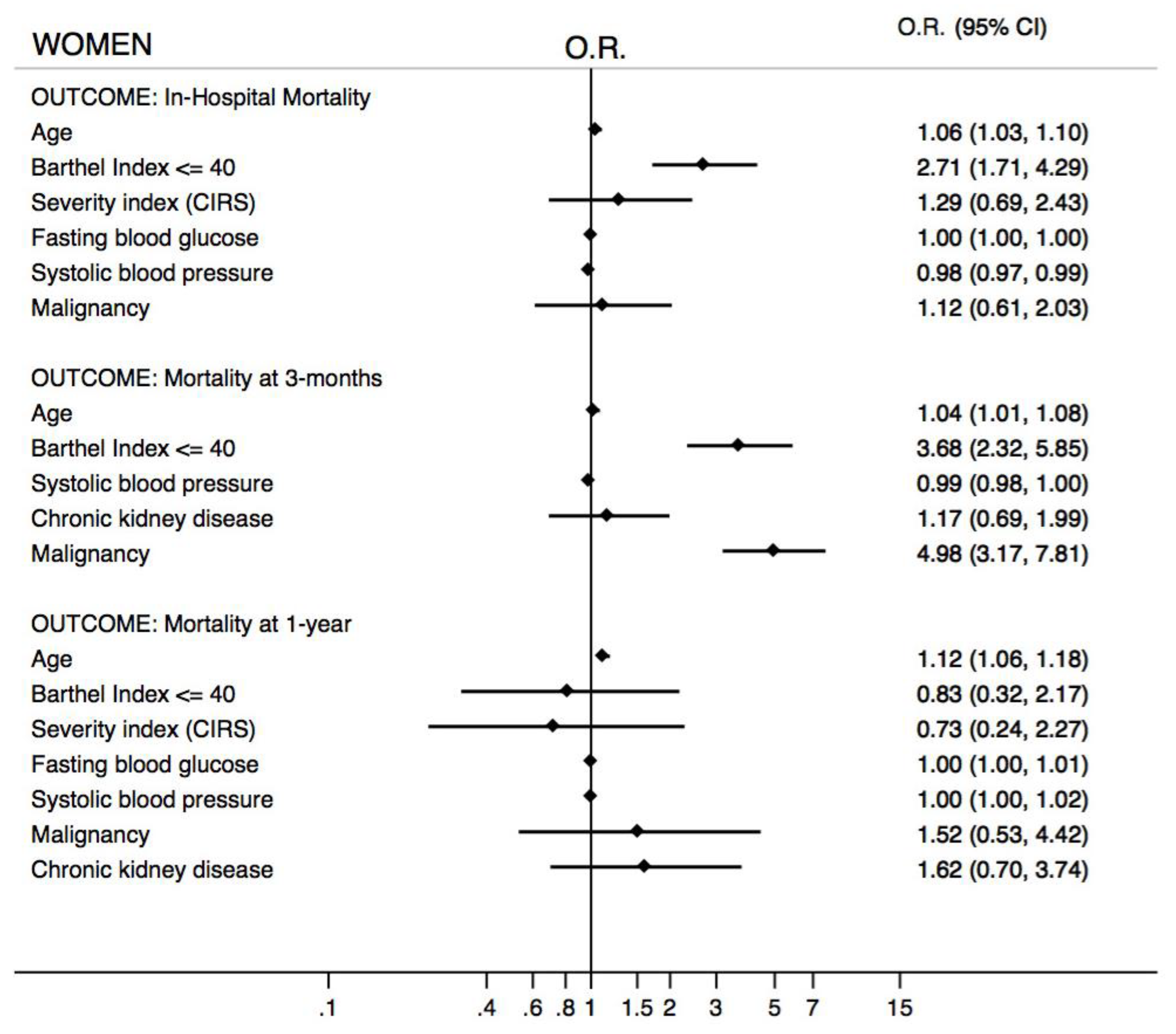
| Variables | In-Hospital Mortality | Mortality at 3-Months | Mortality at 1-Year | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% C.I.) | p = | Odds Ratio (95% C.I.) | p = | Odds Ratio (95% C.I.) | p = | |
| Age | 1.05 (1.03–1.07) | <0.0001 | 1.05 (1.04–1.07) | <0.0001 | 1.05 (1.03–1.07) | <0.0001 |
| Male sex | 1.42 (1.06–1.92) | 0.02 | 1.86 (1.49–2.32) | <0.0001 | 1.78 (1.35–2.34) | <0.0001 |
| Barthel Index ≤ 40 | 3.08 (2.24–4.24) | <0.0001 | 4.19 (3.28–5.37) | <0.0001 | 3.10 (2.17–4.42) | <0.0001 |
| Severity index (CIRS) | 2.01 (1.34–3.03) | 0.001 | - | - | 1.70 (1.12–2.59) | 0.013 |
| Fasting blood glucose | 1.16 (1.04–1.28) | 0.007 | - | - | 1.10 (0.98–1.22) | 0.106 |
| Systolic blood pressure | 0.98 (0.98–0.99) | <0.0001 | 0.99 (0.98–0.99) | <0.0001 | 0.99 (0.98–0.99) | <0.0001 |
| Chronic kidney disease | - | - | 1.15 (0.90–1.47) | 0.257 | 1.05 (0.74–1.49) | 0.767 |
| Malignancy | 1.35 (0.95–1.90) | 0.09 | 2.48 (1.96–3.14) | <0.0001 | 4.39 (3.06–6.30) | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corrao, S.; Argano, C.; Natoli, G.; Nobili, A.; Corazza, G.R.; Mannucci, P.M.; Perticone, F.; on behalf of REPOSI Investigators. Sex-Differences in the Pattern of Comorbidities, Functional Independence, and Mortality in Elderly Inpatients: Evidence from the RePoSI Register. J. Clin. Med. 2019, 8, 81. https://doi.org/10.3390/jcm8010081
Corrao S, Argano C, Natoli G, Nobili A, Corazza GR, Mannucci PM, Perticone F, on behalf of REPOSI Investigators. Sex-Differences in the Pattern of Comorbidities, Functional Independence, and Mortality in Elderly Inpatients: Evidence from the RePoSI Register. Journal of Clinical Medicine. 2019; 8(1):81. https://doi.org/10.3390/jcm8010081
Chicago/Turabian StyleCorrao, Salvatore, Christiano Argano, Giuseppe Natoli, Alessandro Nobili, Gino Roberto Corazza, Pier Mannuccio Mannucci, Francesco Perticone, and on behalf of REPOSI Investigators. 2019. "Sex-Differences in the Pattern of Comorbidities, Functional Independence, and Mortality in Elderly Inpatients: Evidence from the RePoSI Register" Journal of Clinical Medicine 8, no. 1: 81. https://doi.org/10.3390/jcm8010081





