Irreversible Electroporation in Liver Cancers and Whole Organ Engineering
Abstract
:1. Introduction
Electroporation: Technical Description, Procedure, and Role in Medicine
2. Irreversible Electroporation in Hepatic Malignancies
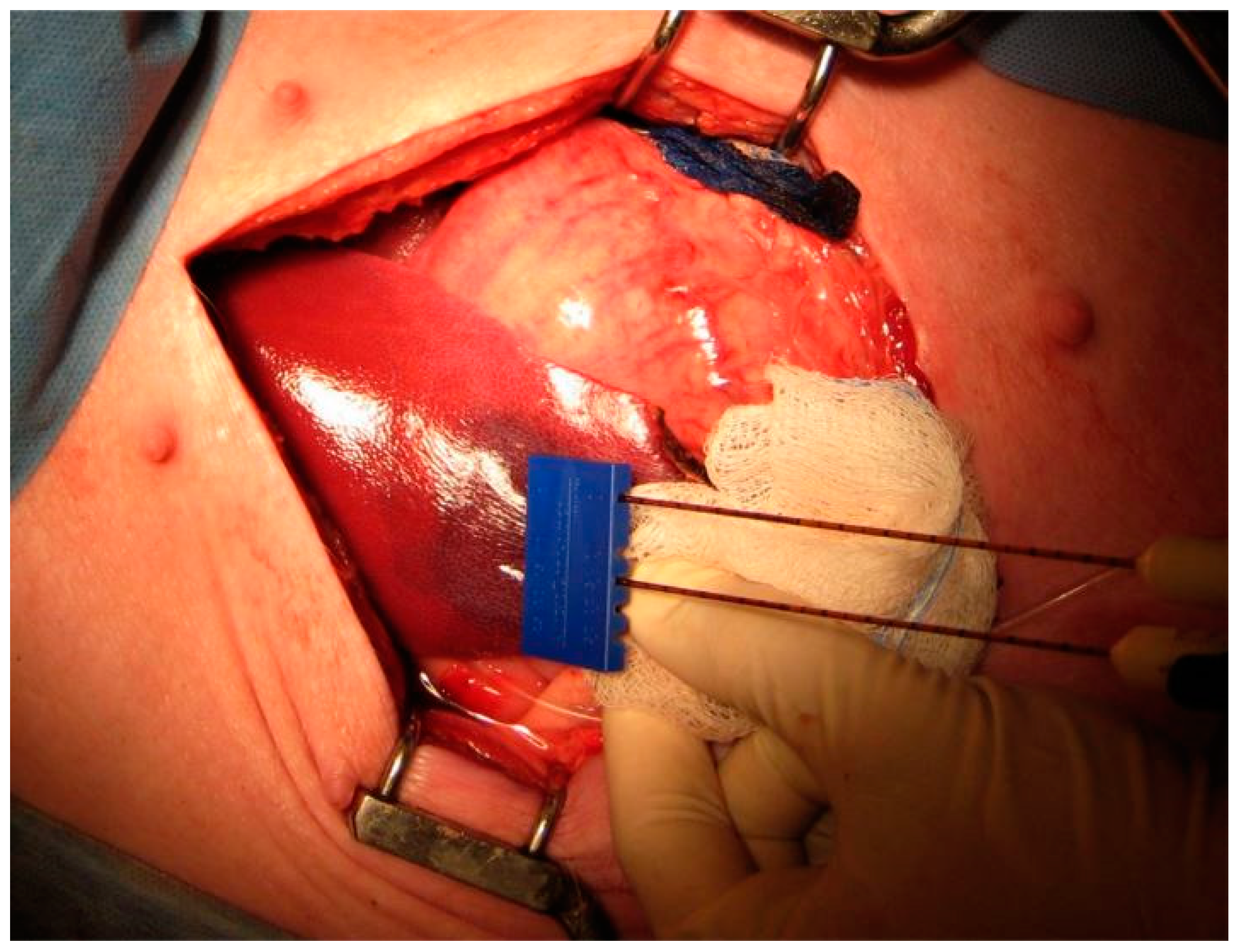
2.1. Safety and Early Efficacy
2.2. Recurrence and Survival Outcomes for IRE-Ablated Liver Tumors
3. Irreversible Electroporation in Whole-Organ Engineering
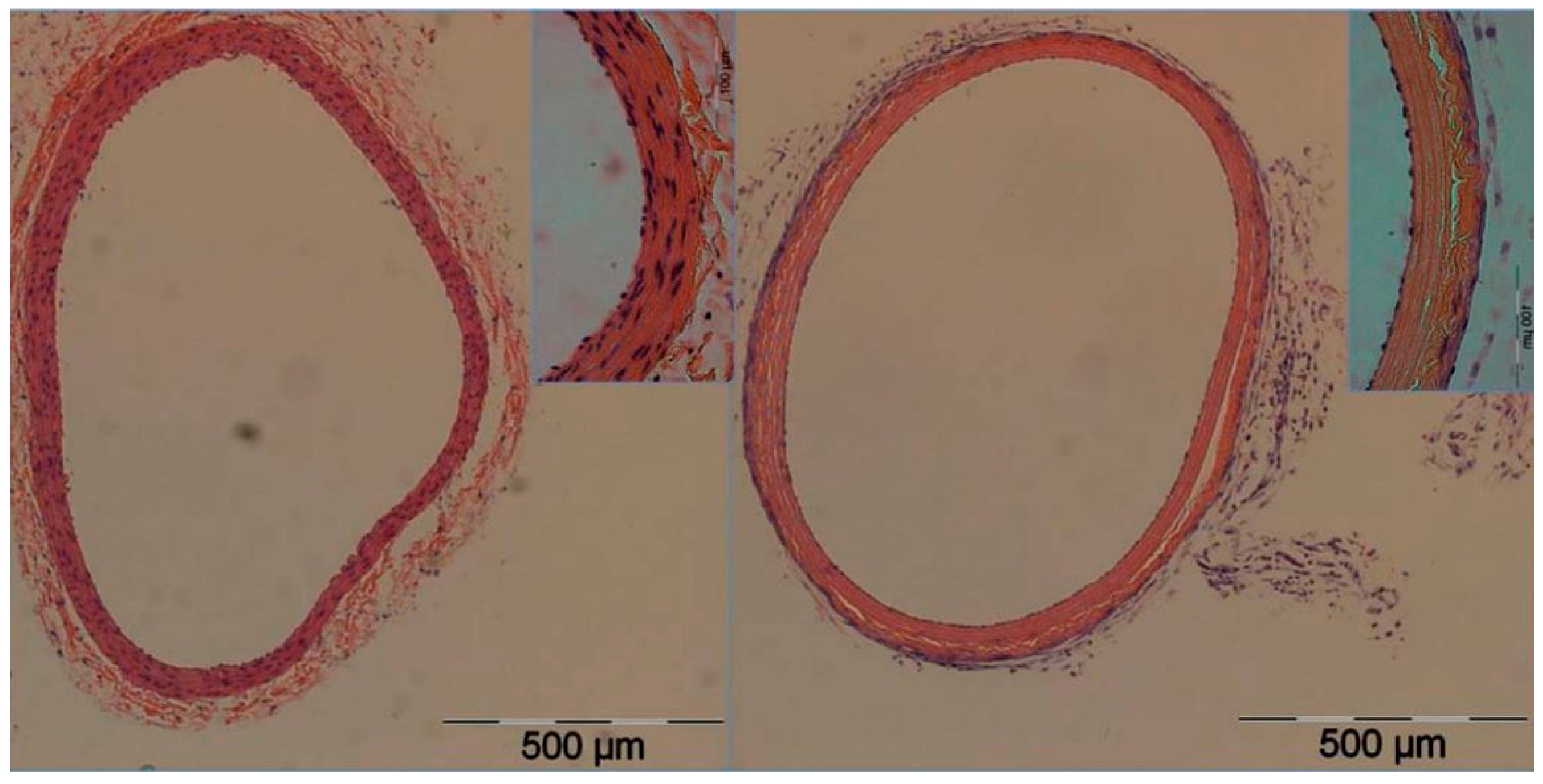
3.1. Decellularization
3.2. Recellularization
Sources of Cells
4. Methods of Recellularization
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Ahmedin, J. Cáncer Statistics. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef]
- Xu, J.Q. Trends in Liver Cancer Mortality among Adults Aged 25 and Over in the United States, 2000–2016. In NCHS Data Brief, No 314; National Center for Health Statistics, Ed.; National Center for Health Statistics: Hyattsville, MD, USA, 2018. [Google Scholar]
- Sheth, R.A.; Hesketh, R.; Kong, D.S.; Wicky, S.; Oklu, R. Barriers to Drug Delivery in Interventional Oncology. J. Vasc. Interv. Radiol. 2013, 24, 1201–1207. [Google Scholar] [CrossRef]
- Oklu, R.; Sheth, R.; Albadawi, H.; Bhan, I.; Sarioglu, A.F.; Choz, M.; Zeinali, M.; Deshpande, V.; Maheswaran, S.; Haber, D.A.; et al. Relationship between Hepatocellular Carcinoma Circulating Tumor Cells and Tumor Volume. Cancer Converg. 2018, 2, 2. [Google Scholar] [CrossRef]
- Sheth, R.A.; Patel, M.S.; Koottappillil, B.; Shah, J.A.; Oklu, R.; Mueller, P.; Vagefi, P.A.; Ganguli, S. Role of Locoregional Therapy and Predictors for Dropout in Patients with Hepatocellular Carcinoma Listed for Liver Transplantation. J. Vasc. Interv. Radiol. 2015, 26, 1761–1768. [Google Scholar] [CrossRef]
- Deipolyi, A.R.; Golberg, A.; Yarmush, M.L.; Arellano, R.S.; Oklu, R. Irreversible Electroporation: Evolution of a Laboratory Technique in Interventional Oncology. Diagn. Interv. Radiol. 2014, 20, 147–154. [Google Scholar] [CrossRef]
- Hesketh, R.L.; Zhu, A.X.; Oklu, R. Hepatocellular Carcinoma: Can Circulating Tumor Cells and Radiogenomics Deliver Personalized Care? Am. J. Clin. Oncol. 2015, 38, 431–436. [Google Scholar] [CrossRef]
- Hesketh, R.L.; Zhu, A.X.; Oklu, R. Radiomics and Circulating Tumor Cells: Personalized Care in Hepatocellular Carcinoma? Diagn. Interv. Radiol. 2015, 21, 78–84. [Google Scholar] [CrossRef]
- Mehta, A.; Oklu, R.; Sheth, R.A. Thermal Ablative Therapies and Immune Checkpoint Modulation: Can Locoregional Approaches Effect a Systemic Response? Gastroenterol. Res. Pract. 2016, 2016. [Google Scholar] [CrossRef]
- Gehl, J. Electroporation: Theory and Methods, Perspectives for Drug Delivery, Gene Therapy and Research. Acta Physiol. Scand. 2003, 177, 437–447. [Google Scholar] [CrossRef]
- Thomson, K.R.; Cheung, W.; Ellis, S.J.; Federman, D.; Kavnoudias, H.; Loader-Oliver, D.; Roberts, S.; Evans, P.; Ball, C.; Haydon, A. Investigation of the Safety of Irreversible Electroporation in Humans. J. Vasc. Interv. Radiol. 2011, 22, 611–621. [Google Scholar] [CrossRef]
- Philips, P.; Hays, D.; Martin, R.C.G. Irreversible Electroporation Ablation (IRE) of Unresectable Soft Tissue Tumors: Learning Curve Evaluation in the First 150 Patients Treated. PLoS ONE 2013, 8, e76260. [Google Scholar] [CrossRef]
- Siddiqui, I.A.; Kirks, R.C.; Latouche, E.L.; DeWitt, M.R.; Swet, J.H.; Baker, E.H.; Vrochides, D.; Iannitti, D.A.; Davalos, R.V.; McKillop, I.H. High-Frequency Irreversible Electroporation: Safety and Efficacy of Next-Generation Irreversible Electroporation Adjacent to Critical Hepatic Structures. Surg. Innov. 2017, 24, 276–283. [Google Scholar] [CrossRef]
- Scheffer, H.J.; Nielsen, K.; van Tilborg, A.A.J.M.; Vieveen, J.M.; Bouwman, R.A.; Kazemier, G.; Niessen, H.W.M.; Meijer, S.; van Kuijk, C.; van den Tol, M.P.; et al. Ablation of Colorectal Liver Metastases by Irreversible Electroporation: Results of the COLDFIRE-I Ablate-and-Resect Study. Eur. Radiol. 2014, 24, 2467–2475. [Google Scholar] [CrossRef]
- Beebe, S.; Sain, N.; Ren, W. Induction of Cell Death Mechanisms and Apoptosis by Nanosecond Pulsed Electric Fields (NsPEFs). Cells 2013, 2, 136–162. [Google Scholar] [CrossRef]
- Zhang, Y.; Lyu, C.; Liu, Y.; Lv, Y.; Chang, T.T.; Rubinsky, B. Molecular and Histological Study on the Effects of Non-Thermal Irreversible Electroporation on the Liver. Biochem. Biophys. Res. Commun. 2018, 500, 665–670. [Google Scholar] [CrossRef]
- Long, G.; Bakos, G.; Shires, P.K.; Gritter, L.; Crissman, J.W.; Harris, J.L.; Clymer, J.W. Histological and Finite Element Analysis of Cell Death Due to Irreversible Electroporation. Technol. Cancer Res. Treat. 2014, 13. [Google Scholar] [CrossRef]
- Narayanan, G.; Hosein, P.J.; Arora, G.; Barbery, K.J.; Froud, T.; Livingstone, A.S.; Franceschi, D.; Rocha Lima, C.M.; Yrizarry, J. Percutaneous Irreversible Electroporation for Downstaging and Control of Unresectable Pancreatic Adenocarcinoma. J. Vasc. Interv. Radiol. 2012, 23, 1613–1621. [Google Scholar] [CrossRef]
- Martin, R.C.G.; McFarland, K.; Ellis, S.; Velanovich, V. Irreversible Electroporation Therapy in the Management of Locally Advanced Pancreatic Adenocarcinoma. J. Am. Coll. Surg. 2012, 215, 361–369. [Google Scholar] [CrossRef]
- Kingham, T.P.; Karkar, A.M.; D’Angelica, M.I.; Allen, P.J.; Dematteo, R.P.; Getrajdman, G.I.; Sofocleous, C.T.; Solomon, S.B.; Jarnagin, W.R.; Fong, Y. Ablation of Perivascular Hepatic Malignant Tumors with Irreversible Electroporation. J. Am. Coll. Surg. 2012, 215, 379–387. [Google Scholar] [CrossRef]
- Deodhar, A.; Monette, S.; Single, G.W.; Hamilton, W.C.; Thornton, R.H.; Sofocleous, C.T.; Maybody, M.; Solomon, S.B. Percutaneous Irreversible Electroporation Lung Ablation: Preliminary Results in a Porcine Model. Cardiovasc. Intervent. Radiol. 2011, 34, 1278–1287. [Google Scholar] [CrossRef]
- Au, J.T.; Mittra, A.; Song, T.J.; Cavnar, M.; Jun, K.; Carson, J.; Gholami, S.; Haddad, D.; Gaujoux, S.; Monette, S.; et al. Irreversible Electroporation Facilitates Gene Transfer of a GM-CSF Plasmid with a Local and Systemic Response. Surgery 2013, 154, 496–503. [Google Scholar] [CrossRef]
- Cannon, R.; Ellis, S.; Hayes, D.; Narayanan, G.; Martin, R.C.G. Safety and Early Efficacy of Irreversible Electroporation for Hepatic Tumors in Proximity to Vital Structures. J. Surg. Oncol. 2013, 107, 544–549. [Google Scholar] [CrossRef]
- Cheung, W.; Kavnoudias, H.; Roberts, S.; Szkandera, B.; Kemp, W.; Thomson, K.R. Irreversible Electroporation for Unresectable Hepatocellular Carcinoma: Initial Experience and Review of Safety and Outcomes. Technol. Cancer Res. Treat. 2013, 12, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Scheffer, H.J.; Nielsen, K.; De Jong, M.C.; Van Tilborg, A.A.J.M.; Vieveen, J.M.; Bouwman, A.; Meijer, S.; Van Kuijk, C.; Van Den Tol, P.; Meijerink, M.R. Irreversible Electroporation for Nonthermal Tumor Ablation in the Clinical Setting: A Systematic Review of Safety and Efficacy. J. Vasc. Interv. Radiol. 2014, 25, 997–1011. [Google Scholar] [CrossRef]
- Dollinger, M.; Beyer, L.P.; Haimerl, M.; Niessen, C.; Jung, E.M.; Zeman, F.; Stroszczynski, C.; Wiggermann, P. Adverse Effects of Irreversible Electroporation of Malignant Liver Tumors under CT Fluoroscopic Guidance: A Single-Center Experience. Diagn. Interv. Radiol. 2015, 21, 471–475. [Google Scholar] [CrossRef]
- Frühling, P.; Nilsson, A.; Duraj, F.; Haglund, U.; Norén, A. Single-Center Nonrandomized Clinical Trial to Assess the Safety and Efficacy of Irreversible Electroporation (IRE) Ablation of Liver Tumors in Humans: Short to Mid-Term Results. Eur. J. Surg. Oncol. 2017, 43, 751–757. [Google Scholar] [CrossRef]
- Niessen, C.; Thumann, S.; Beyer, L.; Pregler, B.; Kramer, J.; Lang, S.; Teufel, A.; Jung, E.M.; Stroszczynski, C.; Wiggermann, P. Percutaneous Irreversible Electroporation: Long-Term Survival Analysis of 71 Patients with Inoperable Malignant Hepatic Tumors. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Langan, R.C.; Ms, D.A.G.; Angelica, M.I.D.; Ronald, P.; Allen, P.J.; Balachandran, V.P.; Jarnagin, W.R. Recurrence Patterns Following Irreversible Electroporation for Hepatic Malignancies. J. Surg. Oncol. 2018, 115, 704–710. [Google Scholar] [CrossRef]
- Soto-Gutiérrez, A.; Kobayashi, N.; Rivas-Carrillo, J.D.; Navarro-Alvarez, N.; Zhao, D.; Zhao, D.; Okitsu, T.; Noguchi, H.; Basma, H.; Tabata, Y.; et al. Reversal of Mouse Hepatic Failure Using an Implanted Liver-Assist Device Containing ES Cell-Derived Hepatocytes. Nat. Biotechnol. 2006, 24, 1412–1419. [Google Scholar] [CrossRef]
- Khan, A.A.; Vishwakarma, S.K.; Bardia, A.; Venkateshwarulu, J. Repopulation of Decellularized Whole Organ Scaffold Using Stem Cells: An Emerging Technology for the Development of Neo-Organ. J. Artif. Organs 2014, 17, 291–300. [Google Scholar] [CrossRef]
- Crapo, P.M.; Gilbert, T.W.; Badylak, S.F. An Overview of Tissue and Whole Organ Decellularization Processes. Biomaterials 2011, 32, 3233–3243. [Google Scholar] [CrossRef] [PubMed]
- Maor, E.; Ivorra, A.; Rubinsky, B. Non Thermal Irreversible Electroporation: Novel Technology for Vascular Smooth Muscle Cells Ablation. PLoS ONE 2009, 4, e4757. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.; Maor, E.; Rubinsky, B. Nonthermal Irreversible Electroporation for Tissue Decellularization. J. Biomech. Eng. 2010, 132, 091003. [Google Scholar] [CrossRef] [PubMed]
- Sano, M.B.; Neal, R.E.; Garcia, P.A.; Gerber, D.; Robertson, J.; Davalos, R.V. Towards the Creation of Decellularized Organ Constructs Using Irreversible Electroporation and Active Mechanical Perfusion. Biomed. Eng. Online 2010, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.T.; Zhou, V.X.; Rubinsky, B. Using Non-Thermal Irreversible Electroporation to Create an in Vivo Niche for Exogenous Cell Engraftment. Biotechniques 2017, 62, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Badylak, S.F.; Taylor, D.; Uygun, K. Whole-Organ Tissue Engineering: Decellularization and Recellularization of Three-Dimensional Matrix Scaffolds. Annu. Rev. Biomed. Eng. 2011, 13, 27–53. [Google Scholar] [CrossRef] [PubMed]
- Halloran, P.F. Immunosuppressive Drugs for Kidney Transplantation. N. Engl. J. Med. 2004, 351, 2715–2729. [Google Scholar] [CrossRef]
- Antonucci, I.; Pantalone, A.; De Amicis, D.; D’Onofrio, S.; Stuppia, L.; Palka, G.; Salini, V. Human Amniotic Fluid Stem Cells Culture onto Titanium Screws: A New Perspective for Bone Engineering. J. Biol. Regul. Homeost. Agents 2009, 23, 277–279. [Google Scholar]
- Peister, A.; Deutsch, E.R.; Kolambkar, Y.; Hutmacher, D.W.; Guldberg, R.E. Amniotic Fluid Stem Cells Produce Robust Mineral Deposits on Biodegradable Scaffolds. Tissue Eng. Part A 2009, 15, 3129–3138. [Google Scholar] [CrossRef] [Green Version]
- Maherali, N.; Sridharan, R.; Xie, W.; Utikal, J.; Eminli, S.; Arnold, K.; Stadtfeld, M.; Yachechko, R.; Tchieu, J.; Jaenisch, R.; et al. Directly Reprogrammed Fibroblasts Show Global Epigenetic Remodeling and Widespread Tissue Contribution. Cell Stem Cell 2007, 1, 55–70. [Google Scholar] [CrossRef] [Green Version]
- Sussman, N.L.; Kelly, J.H. Artificial Liver: A Forthcoming Attraction. Hepatology 1993, 17, 1163–1164. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saini, A.; Breen, I.; Alzubaidi, S.; Pershad, Y.; Sheth, R.; Naidu, S.; Knuttinen, M.G.; Albadawi, H.; Oklu, R. Irreversible Electroporation in Liver Cancers and Whole Organ Engineering. J. Clin. Med. 2019, 8, 22. https://doi.org/10.3390/jcm8010022
Saini A, Breen I, Alzubaidi S, Pershad Y, Sheth R, Naidu S, Knuttinen MG, Albadawi H, Oklu R. Irreversible Electroporation in Liver Cancers and Whole Organ Engineering. Journal of Clinical Medicine. 2019; 8(1):22. https://doi.org/10.3390/jcm8010022
Chicago/Turabian StyleSaini, Aman, Ilana Breen, Sadeer Alzubaidi, Yash Pershad, Rahul Sheth, Sailendra Naidu, M. Grace Knuttinen, Hassan Albadawi, and Rahmi Oklu. 2019. "Irreversible Electroporation in Liver Cancers and Whole Organ Engineering" Journal of Clinical Medicine 8, no. 1: 22. https://doi.org/10.3390/jcm8010022




