Does Nasal Surgery Affect Right Ventricular Myocardial Functions at the Tissue Level in Patients with Nasal Septum Deviation?
Abstract
:1. Introduction
2. Subjects and Methods
3. Surgical Procedure
4. Echocardiography
5. Speckle Tracking Echocardiography
6. Statistical Analysis
7. Results
8. Discussion
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sahin, M.S.; Ozmen, O.A.; Yalcin, M.U. Does Septoplasty Improve Heart Functions of Patients With Septum Deviation in Terms of Echocardiography Findings? J. Craniofac. Surg. 2017, 28, 1803–1805. [Google Scholar] [CrossRef] [PubMed]
- Ozkececi, G.; Akci, O.; Bucak, A.; Ulu, S.; Yalım, Z.; Aycicek, A.; Onrat, E.; Avsar, A. The effect of septoplasty on pulmonary artery pressure and right ventricular function in nasal septum deviation. Eur. Arch. Otorhinolaryngol. 2016, 273, 3747–3752. [Google Scholar] [CrossRef] [PubMed]
- Uluyol, S.; Kilicaslan, S.; Gur, M.H.; Karakaya, N.E.; Buber, I.; Ural, S.G. Effects of Nasal SeptumDeviation and Septoplasty on Cardiac ArrhythmiaRisk. Otolaryngol. Head Neck Surg. 2016, 155, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Haack, J.; Papel, I.D. Caudal septal deviation. Otolaryngol. Clin. N. Am. 2009, 423, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Proctor, D.F. The upper airways: I. Nasal physiology and defence of the lungs. Am. Rev. Respir. Dis. 1977, 115, 97–129. [Google Scholar] [PubMed]
- Blum, R.H.; Mcgowan, F.X., Jr. Chronic upper airway obstruction and cardiac dysfunction: Anatomy, pathophysiology and anesthetic implications. Paediatr. Anaesth. 2004, 14, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Duman, D.; Naiboglu, B.; Esen, H.S.; Toros, S.Z.; Demirtunc, R. Impaired right ventricular function in adenotonsillar hypertrophy. Int. J. Cardiovasc. Imaging 2008, 24, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Fidan, V.; Aksakal, E. Impact of septoplasty on pulmonary artery pressure in patients with markedly deviated septum. J. Craniofac. Surg. 2011, 22, 1591–1593. [Google Scholar] [CrossRef] [PubMed]
- Koc, S.; Aytekin, M.; Kalay, N.; Ozcetin, M.; Burucu, T.; Ozbek, K.; Celik, A.; Kadi, H.; Gulturk, S.; Koc, F. The effect of adenotonsillectomy on right ventricle function and pulmonary artery pressure in children with adenotonsillar hypertrophy. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Moneım, E.S.; Badawy, B.S.; Atya, M. The effect of adenoidectomy on right ventricular performance in children. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1584–1588. [Google Scholar] [CrossRef] [PubMed]
- Attia, G.; Ahmad, M.A.; Saleh, A.B.; Elsharkawy, A. Impact of obstructive sleep apneaon global myocardial performance in children assessed by tissue Doppler imaging. Pediatr. Cardiol. 2010, 31, 1025–1036. [Google Scholar] [CrossRef] [PubMed]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H.; Leano, R.L.; Brown, J.; Sun, J.P.; Hoffmann, R.; Lysyansky, P.; Becker, M.; Thomas, J.D. Myocardial strain measurement with 2-imensional speckle-tracking echocardiography: Definition of normal range. JACC Cardiovasc. Imaging 2009, 2, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Biswas, M.; Sudhakar, S.; Nanda, N.C.; Buckberg, G.; Pradhan, M.; Roomi, A.U.; Gorissen, W.; Houle, H. Two- and three-dimensional speckle tracking echocardiography: Clinical applications and future directions. Echocardiography 2013, 30, 88–105. [Google Scholar] [CrossRef] [PubMed]
- Sadeghpour, A.; Kyavar, M.; Madadi, S.; Ebrahimi, L.; Khajali, Z.; Sani, Z.A. Doppler-derived strain and strain rate imaging assessment of right ventricular systolic function in adults late after tetralogy of Fallot repair: An observational study. Anadolu Kardiyol. Derg. 2013, 13, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.G.; Witsell, D.L.; Smith, T.L.; Weaver, E.M.; Yueh, B.; Hannley, M.T. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol. Head Neck Surg. 2004, 130, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Kahveci, O.K.; Miman, M.C.; Yucel, A.; Yucedag, F.; Okur, E.; Altuntas, A. The efficiency of Nose Obstruction Symptom Evaluation (NOSE) scale on patients with nasal septal deviation. Auris Nasus Larynx 2012, 39, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Getz, A.E.; Hwang, P.H. Endoscopic septoplasty. Curr. Opin. Otolaryngol. Head Neck Surg. 2008, 16, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.S.; et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 2005, 18, 1440–1463. [Google Scholar] [PubMed]
- Calleja, A.M.; Jiamsripong, P.; Alharthi, M.S.; Cha, S.; Cho, E.J.; McMahon, E.M.; Mookadam, F.; Khandheria, B.K.; Belohlavek, M. Correlation of automated function imaging (AFI) to conventional strain analyses of regional and global right ventricular function. J. Am. Soc. Echocardiogr. 2009, 22, 1031–1039. [Google Scholar] [CrossRef] [PubMed]
- Mor-Avi, V.; Lang, R.M.; Badano, L.P.; Belohlavek, M.; Cardim, N.M.; Derumeaux, G.; Galderisi, M.; Marwick, T.; Nagueh, S.F.; Sengupta, P.P.; et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J. Am. Soc. Echocardiogr. 2011, 24, 277–313. [Google Scholar] [CrossRef] [PubMed]
- Wauthy, P.; Pagnamenta, A.; Vassallı, F.; Naeıje, R.; Brımıoulle, S. Right ventricular adaptation to pulmonary hypertension: An interspecies comparison. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, 1441–1447. [Google Scholar] [CrossRef] [PubMed]
- Mcgowan, F.X., Jr. Cardiovascular and airway interactions. Int. Anesthesiol. Clin. 1992, 30, 21–44. [Google Scholar] [PubMed]
- Fuster, V.; Steele, P.M.; Edwards, W.D.; Gersh, B.J.; Mcgoon, M.D.; Frye, R.L. Primary pulmoner hypertension: Natural history and the importance of thrombosis. Circulation 1984, 70, 580–587. [Google Scholar] [CrossRef] [PubMed]
- West, J.B. Gas Exchange. In Pulmonary Pathophysiology; West, J.B., Ed.; Williams & Wilkins Company: Baltimore, MD, USA, 1977; pp. 20–41. [Google Scholar]
- Kossaify, A. Echocardiographic Assessment of the Right Ventricle, from the Conventional Approach to Speckle Tracking and Three-Dimensional Imaging, and Insights into the “Right Way” to Explore the Forgotten Chamber. Clin. Med. Insights Cardiol. 2015, 9, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Gatzoulis, M.A.; Adatia, I.; Celermajer, D.; Denton, C.; Ghofrani, A.; Sanchez, M.A.; Kumar, R.K.; Landzberg, M.; Machado, R.F.; et al. Updated clinical classification of pulmonary hypertension. J. Am. Coll. Cardiol. 2013, 24, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Teske, A.J.; De Boeck, B.W.; Olımulder, M.; Prakken, N.H.; Doevendans, P.A.; Cramer, M.J. Echocardiographic assessment of regional right ventricular function: A head-to-head comparison between 2-dimensional and tissue Doppler-derived strain analysis. J. Am. Soc. Echocardiogr. 2008, 21, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, S.G.; Rudski, L.G. Echocardiographic evaluation of the right ventricle: A 2014 perspective. Curr. Cardiol. Rep. 2015, 17, 21. [Google Scholar] [CrossRef] [PubMed]
- Fine, N.M.; Chen, L.; Bastiansen, P.M.; Frantz, R.P.; Pellikka, P.; Oh, J.K.; Kane, G.C. Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ. Cardiovasc. Imaging 2013, 6, 711–721. [Google Scholar] [CrossRef] [PubMed]

| n | 58 |
| Age, years | 36 ± 7 |
| Male, n (%) | 38 (65) |
| Female, n (%) | 20 (35) |
| BMI, kg/m2 | 22.8 ± 2.1 |
| Heart rate, beats/min | 74.2 ± 6.6 |
| Systolic blood pressure, mmHg | 118 ± 14 |
| Diastolic blood pressure, mmHg | 69 ± 8 |
| Preoperative | Postoperative Third Month | p * | |
|---|---|---|---|
| LVED, mm | 48.21 ± 1.96 | 49.20 ± 2.12 | 0.88 |
| LVES, mm | 29.92 ± 1.56 | 30.85 ± 1.82 | 0.72 |
| LA, mm | 32.22 ± 1.19 | 32.56 ± 1.25 | 0.94 |
| IVSd, mm | 8.93 ± 1.18 | 8.84 ± 1.15 | 0.78 |
| LVEF, Simpson % | 65.9 ± 2,31 | 66.1 ± 2.44 | 0.96 |
| RVED, mm | 33.1 ± 2.21 | 32.8 ± 2.1 | 0.80 |
| RAED, mm | 32.8 ± 2.16 | 32.1 ± 2.34 | 0.78 |
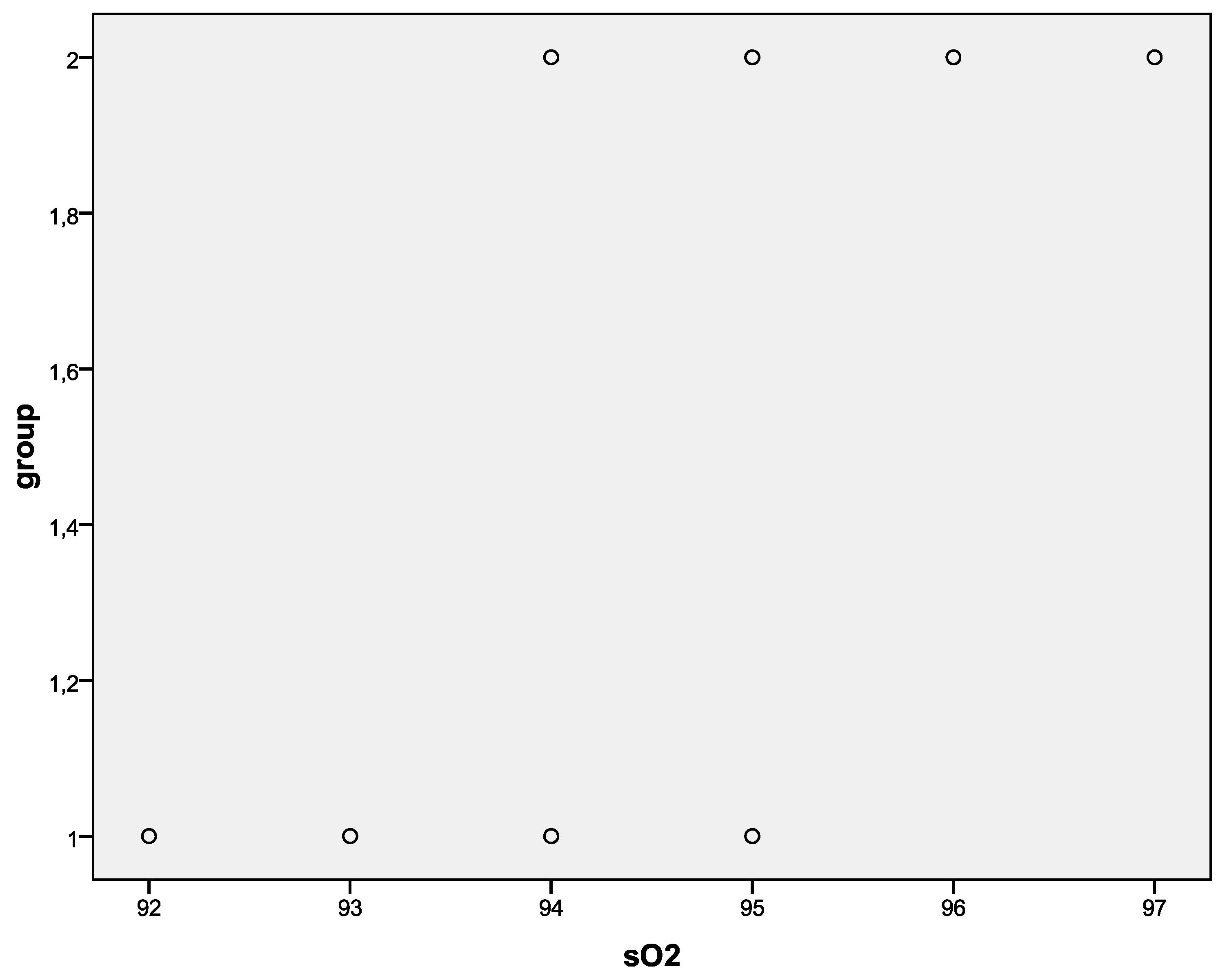
| SpO2, % | 93.5 ± 0.82 | 95.6 ± 0.79 | 0.001 |
| PASP, mmHg | 32.54 ± 5.24 | 24.22 ± 4.55 | 0.001 |
| Preoperative | Postoperative Third Month | p * | |
|---|---|---|---|
| Tricuspid lateral annulus Sm, cm/s | 13.11 ± 1.34 | 13.79 ± 1.12 | 0.51 |
| Tricuspid lateral annulus Em, cm/s | 14.6 ± 2.1 | 15.1 ± 2.7 | 0.48 |
| Tricuspid lateral annulus Am, cm/s | 11.3 ± 3.49 | 11.3 ± 3.43 | 0.96 |
| RV GLS, % | 21.12 ± 2.07 | 22.49 ± 1.89 | 0.013 |
| RV GLSRs, 1/sec | 1.30 ± 0.12 | 1.38 ± 0.13 | 0.015 |
| RV GLSRe, 1/sec | 1.56 ± 0.21 | 1.55 ± 0.26 | 0.86 |
| RV GLSRa, 1/sec | 0.88 ± 0.19 | 0.89 ± 0.18 | 0.76 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simsek, Z.; Simsek, E. Does Nasal Surgery Affect Right Ventricular Myocardial Functions at the Tissue Level in Patients with Nasal Septum Deviation? J. Clin. Med. 2018, 7, 186. https://doi.org/10.3390/jcm7080186
Simsek Z, Simsek E. Does Nasal Surgery Affect Right Ventricular Myocardial Functions at the Tissue Level in Patients with Nasal Septum Deviation? Journal of Clinical Medicine. 2018; 7(8):186. https://doi.org/10.3390/jcm7080186
Chicago/Turabian StyleSimsek, Ziya, and Eda Simsek. 2018. "Does Nasal Surgery Affect Right Ventricular Myocardial Functions at the Tissue Level in Patients with Nasal Septum Deviation?" Journal of Clinical Medicine 7, no. 8: 186. https://doi.org/10.3390/jcm7080186
APA StyleSimsek, Z., & Simsek, E. (2018). Does Nasal Surgery Affect Right Ventricular Myocardial Functions at the Tissue Level in Patients with Nasal Septum Deviation? Journal of Clinical Medicine, 7(8), 186. https://doi.org/10.3390/jcm7080186





