Quadrilateral Space Syndrome: Diagnosis and Clinical Management
Abstract
1. Introduction
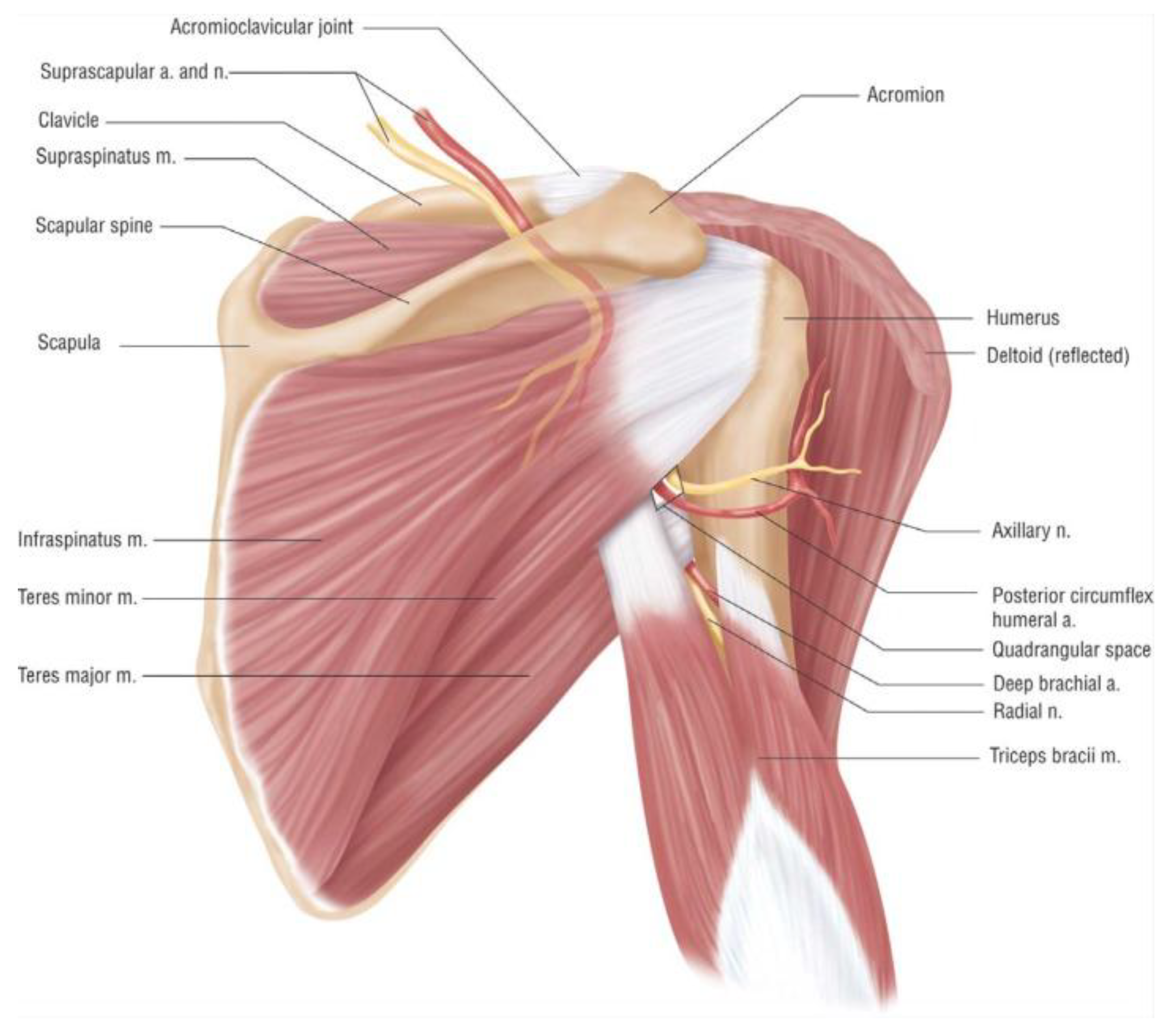
2. Anatomy
3. Etiology
4. Presentation, Differential Diagnoses, Imaging, and Other Workup
4.1. Presentation
4.2. Differential Diagnoses
4.3. Imaging and Other Workup
5. Treatment
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Chen, D.; Cai, P.; Lao, G.; Gu, Y. Quadrilateral space syndrome. Chin. Med. J. 1995, 108, 109–112. [Google Scholar] [PubMed]
- Chautems, R.C.; Glauser, T.; Waeber-Fey, M.C.; Rostan, O.; Barraud, G.E. Quadrilateral space syndrome: Case report and review of the literature. Ann. Vasc. Surg. 2000, 14, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Hoskins, W.T.; Pollard, H.P.; McDonald, A.J. Quadrilateral space syndrome: A case study and review of the literature. Br. J. Sports Med. 2005, 39, e9. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.A.; Doolittle, D.A.; Bohanon, C.J.; Jayaraj, A.; Naidu, S.G.; Huettl, E.A.; Renfree, K.J.; Oderich, G.S.; Bjarnason, H.; Gloviczki, P.; et al. Quadrilateral space syndrome: The mayo clinic experience with a new classification system and case series. Mayo Clin. Proc. 2015, 90, 382–394. [Google Scholar] [CrossRef] [PubMed]
- Cahill, B.R.; Palmer, R.E. Quadrilateral space syndrome. J. Hand Surg. Am. 1983, 8, 65–69. [Google Scholar] [CrossRef]
- Flynn, L.S.; Wright, T.W.; King, J.J. Quadrilateral space syndrome: A review. J. Shoulder Elbow Surg. 2018, 27, 650–956. [Google Scholar] [CrossRef] [PubMed]
- Cothran, R.L.; Helms, C. Quadrilateral space syndrome: Incidence of imaging findings in a population referred for MRI of the shoulder. Am. J. Roentgenol. 2005, 184, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Liveson, J.A. Nerve lesions associated with shoulder dislocation; an electrodiagnostic study of 11 cases. J. Neurol. Neurosurg. Psychiatry 1984, 47, 742–744. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Tsai, T.L.; Altamimi, A.; Tsai, T.M. Quadrilateral space syndrome: A case report. J. Hand Surg. Asian Pac. Vol. 2017, 22, 125–127. [Google Scholar] [CrossRef] [PubMed]
- McClelland, D.; Paxinos, A. The anatomy of the quadrilateral space with reference to quadrilateral space syndrome. J. Shoulder Elbow Surg. 2008, 17, 162–164. [Google Scholar] [CrossRef] [PubMed]
- Aszmann, O.C.; Dellon, A.L.; Birely, B.T.; McFarland, E.G. Innervation of the human shoulder joint and its implications for surgery. Clin. Orthop. Relat. Res. 1996, 202–207. [Google Scholar] [CrossRef]
- Durham, J.R.; Yao, J.S.; Pearce, W.H.; Nuber, G.M.; McCarthy, W.J., 3rd. Arterial injuries in the thoracic outlet syndrome. J. Vasc. Surg. 1995, 21, 57–69, discussion 70. [Google Scholar] [CrossRef]
- Vlychou, M.; Spanomichos, G.; Chatziioannou, A.; Georganas, M.; Zavras, G.M. Embolisation of a traumatic aneurysm of the posterior circumflex humeral artery in a volleyball player. Br. J. Sports Med. 2001, 35, 136–137. [Google Scholar] [CrossRef] [PubMed]
- Seroyer, S.T.; Nho, S.J.; Bach, B.R., Jr.; Bush-Joseph, C.A.; Nicholson, G.P.; Romeo, A.A. Shoulder pain in the overhead throwing athlete. Sports Health 2009, 1, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Cirpar, M.; Gudemez, E.; Cetik, O.; Uslu, M.; Eksioglu, F. Quadrilateral space syndrome caused by a humeral osteochondroma: A case report and review of literature. HSS J. 2006, 2, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.G.; Tirman, P.F. Paralabral cyst: An unusual cause of quadrilateral space syndrome. Arthroscopy 1999, 15, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; White, L.M.; Lax, M.; Salonen, D.; Bell, R.S. Quadrilateral space syndrome caused by glenoid labral cyst. AJR Am. J. Roentgenol. 2000, 175, 1103–1105. [Google Scholar] [CrossRef] [PubMed]
- Mohandas Rao, K.G.; Somayaji, S.N.; Ashwini, L.S.; Ravindra, S.; Abhinitha, P.; Rao, A.; Sapna, M.; Jyothsna, P. Variant course of posterior circumflex humeral artery associated with the abnormal origin of radial collateral artery: Could it mimic the quadrangular space syndrome? Acta Med. Iran. 2012, 50, 572–576. [Google Scholar] [PubMed]
- Pires, L.A.S.; Souza, C.F.C.; Teixeira, A.R.; Leite, T.F.O.; Babinski, M.A.; Chagas, C.A.A. Accessory subscapularis muscle—A forgotten variation? Morphologie 2017, 101, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Kobayashi, M.; Hamagashira, K.; Noumi, S.; Ito, K.; Kato, D.; Shimada, J. Quadrilateral space syndrome: A rare complication of thoracic surgery. Ann. Thorac. Surg. 2008, 86, 1350–1351. [Google Scholar] [CrossRef] [PubMed]
- Koga, R.; Furushima, K.; Kusano, H.; Hamada, J.; Itoh, Y. Quadrilateral space syndrome with involvement of the tendon of the latissimus dorsi. Orthopedics 2017, 40, e714–e716. [Google Scholar] [CrossRef] [PubMed]
- Van de Pol, D.; Kuijer, P.P.; Langenhorst, T.; Maas, M. High prevalence of self-reported symptoms of digital ischemia in elite male volleyball players in the Netherlands: A cross-sectional national survey. Am. J. Sports Med. 2012, 40, 2296–2302. [Google Scholar] [CrossRef] [PubMed]
- McClelland, D.; Hoy, G. A case of quadrilateral space syndrome with involvement of the long head of the triceps. Am. J. Sports Med. 2008, 36, 1615–1617. [Google Scholar] [CrossRef] [PubMed]
- Cummins, C.A.; Schneider, D.S. Peripheral nerve injuries in baseball players. Neurol. Clin. 2008, 26, 195–215. [Google Scholar] [CrossRef] [PubMed]
- Aval, S.M.; Durand, P., Jr.; Shankwiler, J.A. Neurovascular injuries to the athlete’s shoulder: Part II. J. Am. Acad. Orthop. Surg. 2007, 15, 281–289. [Google Scholar] [CrossRef] [PubMed]
- De Mooij, T.; Duncan, A.A.; Kakar, S. Vascular injuries in the upper extremity in athletes. Hand Clin. 2015, 31, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, G.; Gismant, M.; Stevanato, G.; Tiloca, A. Silent deltoid atrophy in beach volleyball players: A report of two cases and literature review. Int. J. Sports Phys. Ther. 2015, 10, 347–353. [Google Scholar] [PubMed]
- Rollo, J.; Rigberg, D.; Gelabert, H. Vascular quadrilateral space syndrome in 3 overhead throwing athletes: An underdiagnosed cause of digital ischemia. Ann. Vasc. Surg. 2017, 42, 63e1–63e6. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.L.; Chung, K.C. Quadrangular space syndrome associated with superficial radial sensory neuropathy. Ann. Plast. Surg. 1999, 43, 207–210. [Google Scholar] [PubMed]
- Jackson, M.R. Upper extremity arterial injuries in athletes. Semin. Vasc. Surg. 2003, 16, 232–239. [Google Scholar] [CrossRef]
- Mochizuki, T.; Isoda, H.; Masui, T.; Ohkawa, Y.; Takahashi, M.; Takehara, Y.; Ichijo, K.; Kodaira, N.; Kitanaka, H. Occlusion of the posterior humeral circumflex artery: Detection with MR angiography in healthy volunteers and in a patient with quadrilateral space syndrome. AJR Am. J. Roentgenol. 1994, 163, 625–627. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Narvaez, V.R. Ultrasound-guided quadrilateral space block for the diagnosis of quadrilateral syndrome. Case Rep. Orthop. 2015, 2015, 378627. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.-H.; Hsiao, M.-Y.; Wu, C.-H.; Özçakar, L. Ultrasound-guided diagnosis and management for quadrilateral space syndrome. Pain Med. 2017, 18, 184–186. [Google Scholar] [CrossRef] [PubMed]
- Wilson, L.; Sundaram, M.; Piraino, D.W.; Ilaslan, H.; Recht, M.P. Isolated teres minor atrophy: Manifestation of quadrilateral space syndrome or traction injury to the axillary nerve? Orthopedics 2006, 29, 447–450. [Google Scholar] [PubMed]
- Lopez Ovenza, J.M.; Ranalletta, M.; Alonso Hidalgo, I.; Tanoira, I.; Bongiovanni, S.; Maignon, G. Quadrilateral space syndrome with compromise of the teres minor muscle. Medicina 2011, 71, 49. [Google Scholar] [PubMed]
- Molina Granados, J.F.; Dominguez Franjo, E. Quadrilateral space syndrome with complete denervation of the deltoid and teres minor muscles. Radiologia 2010, 52, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Brestas, P.S.; Tsouroulas, M.; Nikolakopoulou, Z.; Malagari, K.; Drossos, C. Ultrasound findings of teres minor denervation in suspected quadrilateral space syndrome. J. Clin. Ultrasound 2006, 34, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.Y.; Chang, K.V.; Chen, P.T.; Ho, Y.T.; Han, D.S.; Chen, W.S.; Wang, T.G. Sonoelastography for the evaluation of an axillary schwannoma in a case of quadrilateral space syndrome. Clin. Imaging 2014, 38, 360–363. [Google Scholar] [CrossRef] [PubMed]
- McAdams, T.R.; Dillingham, M.F. Surgical decompression of the quadrilateral space in overhead athletes. Am. J. Sports Med. 2008, 36, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Manske, R.C.; Sumler, A.; Runge, J. Quadrilateral space syndrome. Hum. Kinet. 2009, 14, 45–47. [Google Scholar] [CrossRef][Green Version]
- Reeser, J.C. Diagnosis and management of vascular injuries in the shoulder girdle of the overhead athlete. Curr. Sports Med. Rep. 2007, 6, 322–327. [Google Scholar] [PubMed]
- Hangge, P.; Rotellini-Coltvet, L.; Deipolyi, A.R.; Albadawi, H.; Oklu, R. Paget-schroetter syndrome: Treatment of venous thrombosis and outcomes. Cardiovasc. Diagn. Ther. 2017, 7, S285–S290. [Google Scholar] [CrossRef] [PubMed]
- Francel, T.J.; Dellon, A.L.; Campbell, J.N. Quadrilateral space syndrome: Diagnosis and operative decompression technique. Plast. Reconstr. Surg. 1991, 87, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Reekers, J.A.; den Hartog, B.M.; Kuyper, C.F.; Kromhout, J.G.; Peeters, F.L. Traumatic aneurysm of the posterior circumflex humeral artery: A volleyball player’s disease? J. Vasc. Interv. Radiol. 1993, 4, 405–408. [Google Scholar] [CrossRef]
- Duwayri, Y.M.; Emery, V.B.; Driskill, M.R.; Earley, J.A.; Wright, R.W.; Paletta, G.A., Jr.; Thompson, R.W. Positional compression of the axillary artery causing upper extremity thrombosis and embolism in the elite overhead throwing athlete. J. Vasc. Surg. 2011, 53, 1329–1340. [Google Scholar] [CrossRef] [PubMed]
- Arko, F.R.; Harris, E.J.; Zarins, C.K.; Olcott, C.T. Vascular complications in high-performance athletes. J. Vasc. Surg. 2001, 33, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Reekers, J.A.; Koedam, N. Volleyball-related ischemia of the hand. Cardiovasc. Interv. Radiol. 1998, 21, 261. [Google Scholar] [CrossRef]
- Gregory, T.; Sangha, H.; Bleakney, R. Spontaneous resolution of quadrilateral space syndrome: A case report. Am. J. Phys. Med. Rehabil. 2015, 94, e1–e5. [Google Scholar] [CrossRef] [PubMed]


© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hangge, P.T.; Breen, I.; Albadawi, H.; Knuttinen, M.G.; Naidu, S.G.; Oklu, R. Quadrilateral Space Syndrome: Diagnosis and Clinical Management. J. Clin. Med. 2018, 7, 86. https://doi.org/10.3390/jcm7040086
Hangge PT, Breen I, Albadawi H, Knuttinen MG, Naidu SG, Oklu R. Quadrilateral Space Syndrome: Diagnosis and Clinical Management. Journal of Clinical Medicine. 2018; 7(4):86. https://doi.org/10.3390/jcm7040086
Chicago/Turabian StyleHangge, Patrick T., Ilana Breen, Hassan Albadawi, M. Grace Knuttinen, Sailendra G. Naidu, and Rahmi Oklu. 2018. "Quadrilateral Space Syndrome: Diagnosis and Clinical Management" Journal of Clinical Medicine 7, no. 4: 86. https://doi.org/10.3390/jcm7040086
APA StyleHangge, P. T., Breen, I., Albadawi, H., Knuttinen, M. G., Naidu, S. G., & Oklu, R. (2018). Quadrilateral Space Syndrome: Diagnosis and Clinical Management. Journal of Clinical Medicine, 7(4), 86. https://doi.org/10.3390/jcm7040086




