Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice
Abstract
:1. Introduction
2. Experimental Section
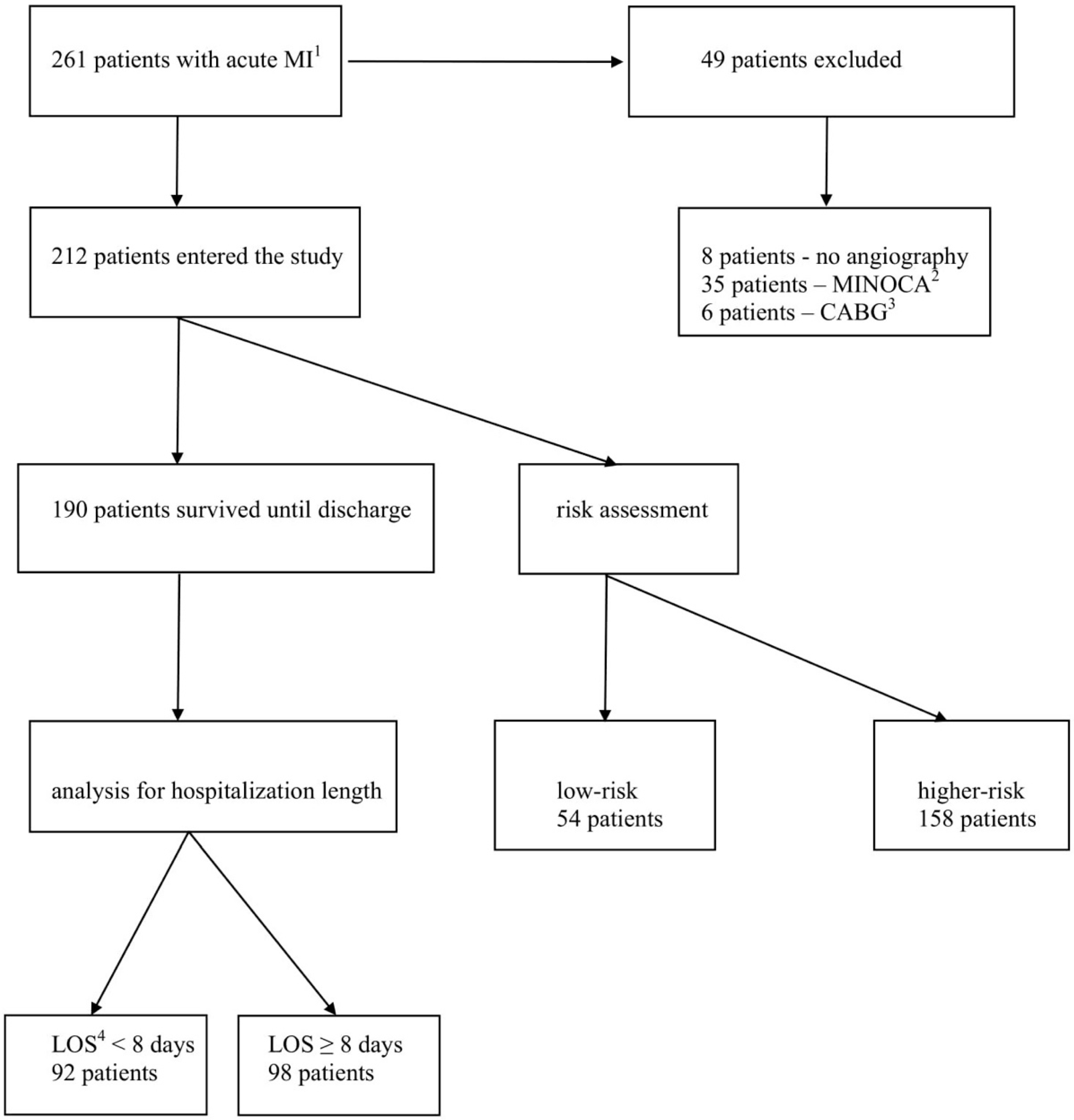
2.1. Study Population
2.2. Statistical Analysis
3. Results
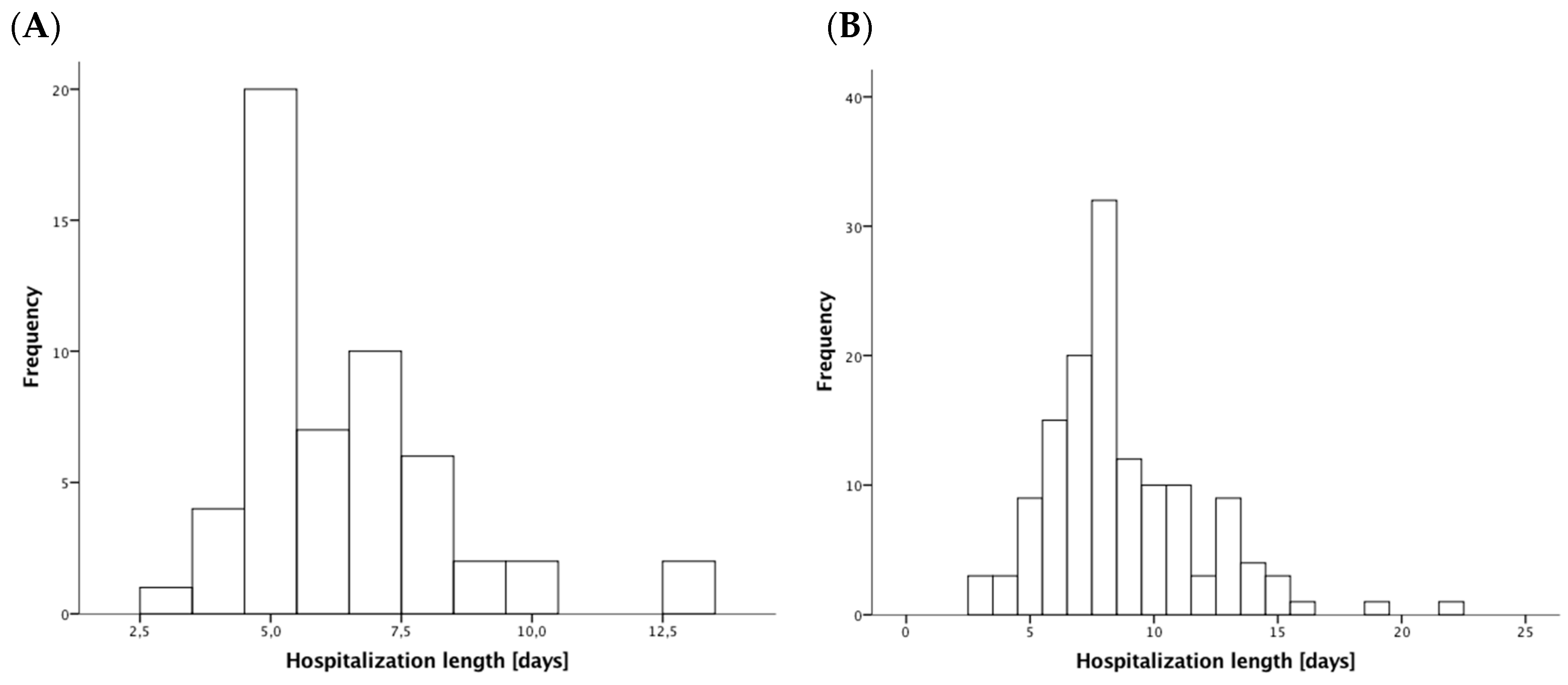
3.1. Patients’ Characteristics
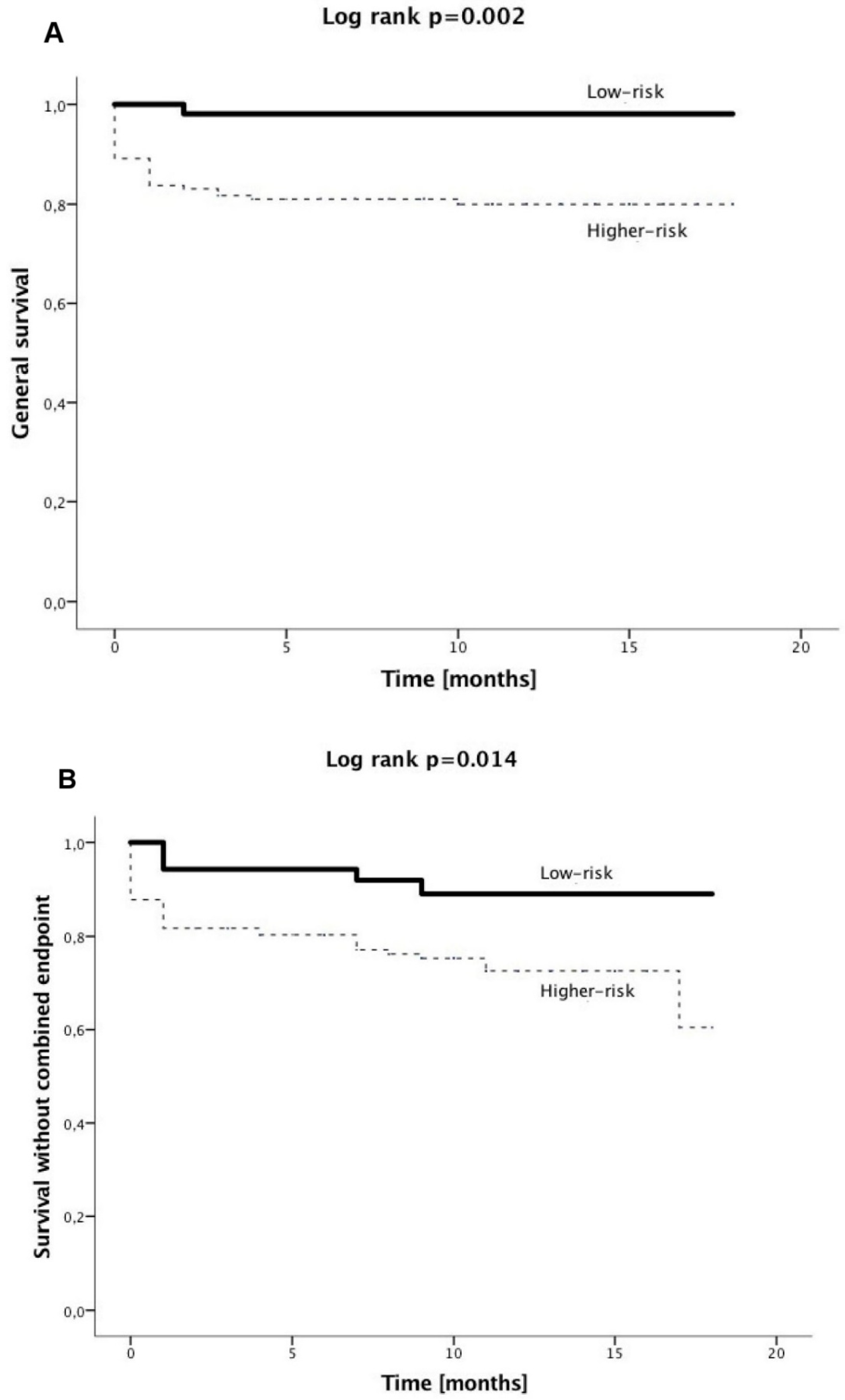
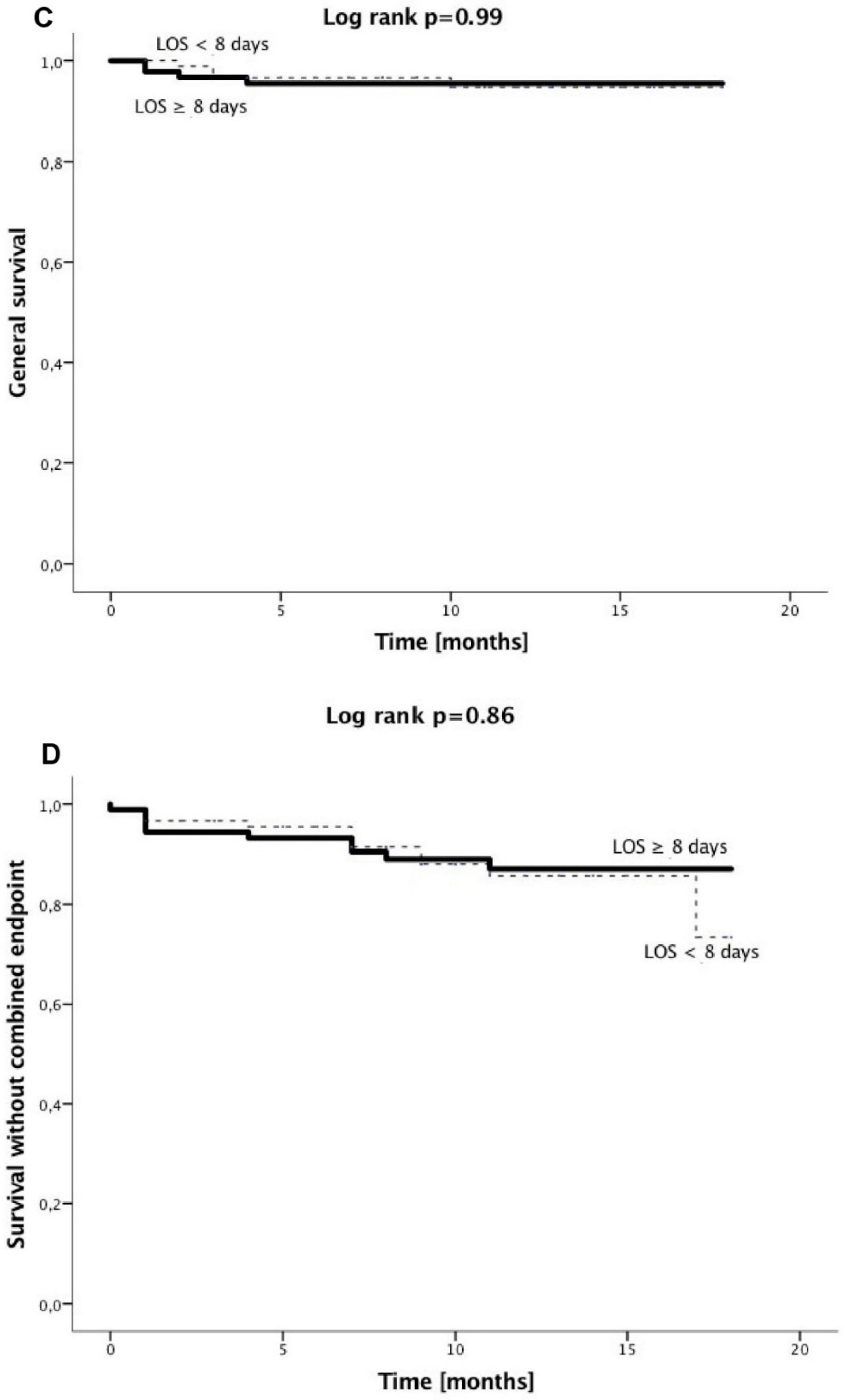
3.2. Clinical Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Azzalini, L.; Solé, E.; Sans, J.; Vila, M.; Durán, A.; Gil-Alonso, D.; Santaló, M.; Garcia-Moll, X.; Sionis, A. Feasibility and safety of an early discharge strategy after low-risk acute myocardial infarction treated with primary percutaneous coronary intervention: The EDAMI pilot trial. Cardiology 2015, 130, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Melberg, T.; Jørgensen, M.; Ørn, S.; Solli, T.; Edland, U.; Dickstein, K. Safety and health status following early discharge in patients with acute myocardial infarction treated with primary PCI: A randomized trial. Eur. J. Prev. Cardiol. 2015, 22, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Noman, A.; Zaman, A.G.; Schechter, C.; Balasubramaniam, K.; Das, R. Early discharge after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 262–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, D.A.; Rathod, K.S.; Howard, J.P.; Gallagher, S.; Antoniou, S.; De Palma, R.; Guttmann, O.; Cliffe, S.; Colley, J.; Butler, J.; et al. Safety and feasibility of hospital discharge 2 days following primary percutaneous intervention for ST-segment elevation myocardial infarction. Heart 2012, 98, 1722–1727. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J.; Burek, K.; O’Neill, W.W.; Kewman, D.G.; Kander, N.H.; Shea, M.J.; Schork, M.A.; Kirscht, J.; Juni, J.E.; Pitt, B. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N. Engl. J. Med. 1988, 318, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Bogaty, P.; Dumont, S.; O’Hara, G.E.; Boyer, L.; Auclair, L.; Jobin, J.; Boudreault, J.R. Randomized trial of a noninvasive strategy to reduce hospital stay for patients with low-risk myocardial infarction. J. Am. Coll. Cardiol. 2001, 37, 1289–1296. [Google Scholar] [CrossRef]
- Chen, E.; Naylor, C.D. Variation in hospital length of stay for acute myocardial infarction in Ontario, Canada. Med. Care 1994, 32, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Every, N.R.; Spertus, J.; Fihn, S.D.; Hlatky, M.; Martin, J.S.; Weaver, W.D. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J. Am. Coll. Cardiol. 1996, 28, 287–293. [Google Scholar] [CrossRef]
- Kinjo, K.; Sato, H.; Nakatani, D.; Mizuno, H.; Shimizu, M.; Hishida, E.; Ezumi, A.; Hoshida, S.; Koretsune, Y.; Hori, M.; et al. Predictors of length of hospital stay after acute myocardial infarction in Japan. Circ. J. 2004, 68, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Grines, C.L.; Marsalese, D.L.; Brodie, B.; Griffin, J.; Donohue, B.; Costantini, C.R.; Balestrini, C.; Stone, G.; Wharton, T.; Esente, P.; et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. J. Am. Coll. Cardiol. 1998, 31, 967–972. [Google Scholar] [CrossRef]
- Hutter, A.M., Jr.; Sidel, V.W.; Shine, K.I.; De Sanctis, R.W. Early hospital discharge after myocardial infarction. N. Engl. J. Med. 1973, 288, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Wenger, N.K.; Hellerstein, H.K.; Blackburn, H.; Castranova, S.J. Uncomplicated myocardial infarction. Current physician practice in patient management. JAMA 1973, 224, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Ahlmark, G.; Ahlberg, G.; Saetre, H.; Haglund, I.; Korsgren, M. A controlled study of early discharge after uncomplicated myocardial infarction. Acta Med. Scand. 1979, 206, 87–91. [Google Scholar] [CrossRef] [PubMed]
- McNeer, J.F.; Wagner, G.S.; Ginsburg, P.B.; Wallace, A.G.; McCants, C.B.; Conley, M.J.; Rosati, R.A. Hospital discharge one week after acute myocardial infarction. N. Engl. J. Med. 1978, 298, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Morrow, D.A.; Antman, E.M.; Charlesworth, A.; Cairns, R.; Murphy, S.A.; de Lemos, J.A.; Giugliano, R.P.; McCabe, C.H.; Braunwald, E. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000, 102, 2031–2037. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.A.; Anderson, F.A., Jr.; Dabbous, O.H.; Steg, P.G.; López-Sendón, J.; Van de Werf, F.; Gurfinkel, E.P.; Goodman, S.G.; Brieger, D. Intervention in acute coronary syndromes: Do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE). Heart 2007, 93, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.L.; Woodlief, L.H.; Topol, E.J.; Weaver, W.D.; Betriu, A.; Col, J.; Simoons, M.; Aylward, P.; Van de Werf, F.; Califf, R.M. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. Circulation 1995, 91, 1659–1668. [Google Scholar] [CrossRef] [PubMed]
- De Luca, G.; Suryapranata, H.; van’t Hof, A.W.; de Boer, M.J.; Hoorntje, J.C.; Dambrink, J.H.; Gosselink, A.T.; Ottervanger, J.P.; Zijlstra, F. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: Implications for early discharge. Circulation 2004, 109, 2737–2743. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Spencer, F.A.; Lessard, D.; Gore, J.M.; Yarzebski, J.; Goldberg, R.J. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: A community-wide perspective. Arch. Int. Med. 2004, 164, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.K.; Duval, S.; Jacobs, D.R., Jr.; Barber, C.; Vazquez, G.; Lee, S.; Luepker, R.V. Relation of length of hospital stay in acute myocardial infarction to postdischarge mortality. Am. J. Cardiol. 2008, 101, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Rogers, W.J.; Canto, J.G.; Lambrew, C.T.; Tiefenbrunn, A.J.; Kinkaid, B.; Shoultz, D.A.; Frederick, P.D.; Every, N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: The National Registry of Myocardial Infarction 1, 2 and 3. J. Am. Coll. Cardiol. 2000, 36, 2056–2063. [Google Scholar] [CrossRef]
- Alonso Salinas, G.L.; Sanmartin, M.; Pascual Izco, M.; Rincon, L.M.; Martin-Acuna, A.; Pastor Pueyo, P.; Del Val Martín, D.; Marco Del Castillo, Á.; Recio-Mayoral, A.; Martin-Asenjo, R.; et al. The role of frailty in acute coronary syndromes in the elderly. Gerontology 2018, 64, 422–429. [Google Scholar] [CrossRef] [PubMed]
| Patients Surviving until Hospital Discharge (n = 190) | All Patients (n = 212) | |||||
|---|---|---|---|---|---|---|
| LOS 8 <8 Days (92 Patients) | LOS ≥8 Days (98 Patients) | p-Value | Higher-Risk (158 Patients) | Low-Risk (54 Patients) | p-Value | |
| Baseline presentation | ||||||
| ST-elevation MI 1 (%) | 22 | 37 | 0.03 | 33 | 24 | 0.24 |
| Age (years) | 64 ± 11 | 69 ± 12 | 0.003 | 71±11 | 57 ± 8 | <0.001 |
| Male gender (%) | 71 | 64 | 0.36 | 63 | 76 | 0.097 |
| Hypertension history (%) | 82 | 82 | 1.0 | 79 | 78 | 0.85 |
| Diabetes history (%) | 29 | 41 | 0.13 | 41 | 24 | 0.03 |
| COPD history 2 (%) | 9 | 14 | 0.26 | 13 | 7 | 0.45 |
| Smoking (%) | 48 | 45 | 0.77 | 38 | 65 | 0.001 |
| Stroke history (%) | 8 | 11 | 0.46 | 11 | 2 | 0.048 |
| MI history (%) | 29 | 23 | 0.41 | 27 | 22 | 0.59 |
| In-hospital characteristics | ||||||
| LVEF 3 (%) | 55 (Q1: 45; Q3: 60) | 45 (Q1: 38; Q3: 55) | <0.001 | 45 (Q1: 37 Q3: 52) | 56 (Q1: 50 Q3: 60) | <0.001 |
| LAD 4 culprit (%) | 29 | 40 | 0.17 | 39 | 30 | 0.25 |
| Multi-vessel disease (%) | 23 | 48 | <0.001 | 48 | 0 | <0.001 |
| Staged revascularization (%) | 14 | 33 | 0.003 | 28 | 4 | <0.001 |
| Ventricular arrhythmia (%) | 9 | 16 | 0.13 | 11 | 0 | 0.008 |
| GFR 5 (mL/min/1.73 m2) | 85 ± 28 | 77 ± 34 | 0.08 | 72 ± 33 | 92 ± 23 | <0.001 |
| RBC 6 transfusion (%) | 2 | 4 | 0.68 | 4 | 2 | 0.68 |
| Respiratory infections (%) | 6 | 20 | 0.006 | 19 | 6 | 0.017 |
| ACEI/ARB 7 (%) | 88 | 88 | 1.0 | 78 | 91 | 0.04 |
| B-blocker (%) | 88 | 90 | 0.82 | 80 | 89 | 0.21 |
| Loop diuretics (%) | 24 | 42 | 0.009 | 47 | 9 | <0.001 |
| Aldosterone antagonists (%) | 13 | 33 | 0.002 | 28 | 6 | <0.001 |
| ST-Elevation MI 1 (65 Patients) | Non-ST-Elevation MI (147 Patients) | p-Value | |
|---|---|---|---|
| Baseline presentation | |||
| Age (years) | 67 ± 13 | 67 ± 11 | 0.93 |
| Male gender (%) | 60 | 69 | 0.21 |
| Hypertension history (%) | 71 | 82 | 0.07 |
| Diabetes history (%) | 35 | 37 | 0.88 |
| COPD history 2 (%) | 11 | 12 | 1.0 |
| Smoking (%) | 48 | 43 | 0.65 |
| Stroke history (%) | 6 | 9 | 0.59 |
| MI history (%) | 12 | 31 | 0.003 |
| Low-risk (%) | 20 | 28 | 0.24 |
| In-hospital characteristics | |||
| Length of hospital stay (d) | 8 (Q1: 7; Q3: 9) | 7 (Q1: 6; Q3: 10) | 0.19 |
| LVEF 3 (%) | 45 (Q1: 38; Q3: 55) | 50 (Q1: 40; Q3: 55) | 0.14 |
| LAD 4 culprit (%) | 45 | 33 | 0.12 |
| Multi-vessel disease (%) | 31 | 38 | 0.35 |
| Staged revascularization (%) | 20 | 22 | 0.86 |
| Ventricular arrhythmia (%) | 11 | 7 | 0.41 |
| GFR 5 (mL/min/1.73 m2) | 87 ± 35 | 73 ± 30 | 0.006 |
| RBC 6 transfusion (%) | 5 | 3 | 0.7 |
| Respiratory infections (%) | 15 | 16 | 1.0 |
| ACEI/ARB 7 (%) | 78 | 83 | 0.44 |
| B-blocker (%) | 80 | 84 | 0.56 |
| Loop diuretics (%) | 36 | 38 | 0.76 |
| Aldosterone antagonists (%) | 31 | 18 | 0.04 |
| Multi-Vessel Disease (76 Patients) | No Multi-Vessel Disease (136 Patients) | p-Value | |
|---|---|---|---|
| Baseline presentation | |||
| ST-elevation MI 1 (%) | 26 | 33 | 0.35 |
| Age (years) | 67 ± 10 | 67 ± 12 | 0.72 |
| Male gender (%) | 71 | 64 | 0.36 |
| Hypertension history (%) | 72 | 82 | 0.11 |
| Diabetes history (%) | 41 | 34 | 0.37 |
| COPD history 2 (%) | 8 | 13 | 0.27 |
| Smoking (%) | 46 | 44 | 0.89 |
| Stroke history (%) | 7 | 10 | 0.61 |
| MI history (%) | 24 | 26 | 0.74 |
| Low-risk (%) | 0 | 40 | <0.001 |
| In-hospital characteristics | |||
| Length of hospital stay (d) | 8 (Q1: 7; Q3: 10) | 7 (Q1: 5; Q3: 9) | <0.001 |
| LVEF 3 (%) | 45 (Q1: 39; Q3: 55) | 50 (Q1: 40; Q3: 58) | 0.14 |
| LAD 4 culprit (%) | 34 | 38 | 0.66 |
| Staged revascularization (%) | 54 | 4 | <0.001 |
| Ventricular arrhythmia (%) | 9 | 7 | 0.61 |
| GFR 5 (mL/min/1.73 m2) | 81 ± 35 | 76 ± 30 | 0.31 |
| RBC 6 transfusion (%) | 3 | 4 | 0.71 |
| Respiratory infections (%) | 16 | 15 | 1.0 |
| ACEI/ARB 7 (%) | 77 | 84 | 0.27 |
| B-blocker (%) | 83 | 82 | 1.0 |
| Loop diuretics (%) | 33 | 40 | 0.37 |
| Aldosterone antagonists (%) | 17 | 24 | 0.29 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| OR 7 | 95% CI 8 | p-Value | OR | 95% CI | p-Value | |
| Baseline characteristics | ||||||
| Age (per one year increase) | 1.04 | 1.01–1.07 | 0.004 | 1.04 | 1.01–1.07 | 0.016 |
| Female gender | 1.3 | 0.7–2.4 | 0.35 | |||
| Arterial hypertension | 1.0 | 0.48–2.1 | 0.98 | |||
| Diabetes mellitus | 1.7 | 0.91–3.0 | 0.1 | |||
| History of MI 1 | 0.74 | 0.4–1.4 | 0.36 | |||
| History of CABG 2 | 0.69 | 0.15–3.2 | 0.64 | |||
| History of stroke | 1.5 | 0.57–4.1 | 0.4 | |||
| Smoking | 0.89 | 0.5–1.6 | 0.69 | |||
| Hyperlipidemia | 0.87 | 0.47–1.6 | 0.64 | |||
| COPD 3 | 1.75 | 0.7–4.4 | 0.23 | |||
| Atrial fibrillation | 2.1 | 0.97–4.7 | 0.06 | |||
| Hemodialysis | 1.9 | 0.34–10.7 | 0.46 | |||
| In hospital characteristics | ||||||
| ST-elevation MI | 2.09 | 1.1–4.0 | 0.025 | 2.3 | 1.1–4.7 | 0.02 |
| LVEF 4 (per 1% increase) | 0.95 | 0.93–0.98 | 0.001 | 0.97 | 0.94–0.99 | 0.016 |
| Multi-vessel disease | 3.1 | 1.7–5.8 | <0.001 | 3.4 | 1.7–6.6 | <0.001 |
| Ventricular arrhythmia | 2.2 | 0.7–7.5 | 0.2 | |||
| RBC 5 transfusion | 1.9 | 0.3–10.7 | 0.46 | |||
| Pneumonia | 3.7 | 1.4– 9.6 | 0.008 | |||
| GFR 6 (per 1 mL/min/1.73 m2 increase) | 0.9 | 0.98–1.0 | 0.09 | |||
| Patients Surviving until Hospital Discharge (n = 190) | All Patients (n = 212) | |||||
|---|---|---|---|---|---|---|
| LOS 2 <8 Days (92 Patients) | LOS ≥8 Days (98 Patients) | p-Value | Higher-Risk (158 Patients) | Low-Risk (54 Patients) | p-Value | |
| In hospital outcomes | ||||||
| All-cause mortality (%) | - | - | - | 14 | 0 | 0.001 |
| Cardiovascular mortality (%) | - | - | - | 14 | 0 | 0.001 |
| All recurrent MI 1 (%) | 0 | 0 | - | 0 | 0 | - |
| Non-fatal recurrent MI (%) | 0 | 0 | - | 0 | 0 | - |
| All stroke (%) | 1 | 1 | 1.0 | 2 | 0 | 0.57 |
| Non-fatal stroke (%) | 1 | 1 | 1.0 | 1 | 0 | 1.0 |
| Combined endpoint (%) | 1 | 1 | 1.0 | 15 | 0 | 0.001 |
| Long-term outcomes | ||||||
| All-cause mortality (%) | 4 | 4 | 1.0 | 18 | 2 | 0.001 |
| Cardiovascular mortality (%) | 0 | 2 | 0.5 | 15 | 0 | 0.001 |
| All recurrent MI (%) | 11 | 7 | 0.45 | 8 | 9 | 0.77 |
| Non-fatal recurrent MI (%) | 11 | 6 | 0.3 | 7 | 9 | 0.56 |
| All stroke (%) | 2 | 2 | 1.0 | 4 | 0 | 0.34 |
| Non-fatal stroke (%) | 2 | 2 | 1.0 | 2 | 0 | 0.57 |
| Combined endpoint (%) | 12 | 10 | 0.82 | 24 | 9 | 0.02 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Węgiel, M.; Dziewierz, A.; Wojtasik-Bakalarz, J.; Sorysz, D.; Surdacki, A.; Bartuś, S.; Dudek, D.; Rakowski, T. Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice. J. Clin. Med. 2018, 7, 564. https://doi.org/10.3390/jcm7120564
Węgiel M, Dziewierz A, Wojtasik-Bakalarz J, Sorysz D, Surdacki A, Bartuś S, Dudek D, Rakowski T. Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice. Journal of Clinical Medicine. 2018; 7(12):564. https://doi.org/10.3390/jcm7120564
Chicago/Turabian StyleWęgiel, Michał, Artur Dziewierz, Joanna Wojtasik-Bakalarz, Danuta Sorysz, Andrzej Surdacki, Stanisław Bartuś, Dariusz Dudek, and Tomasz Rakowski. 2018. "Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice" Journal of Clinical Medicine 7, no. 12: 564. https://doi.org/10.3390/jcm7120564






