Fatigue is Highly Prevalent in Patients with Asthma and Contributes to the Burden of Disease
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Health Status and Disease-Specific Characteristics
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Prevalence of Fatigue
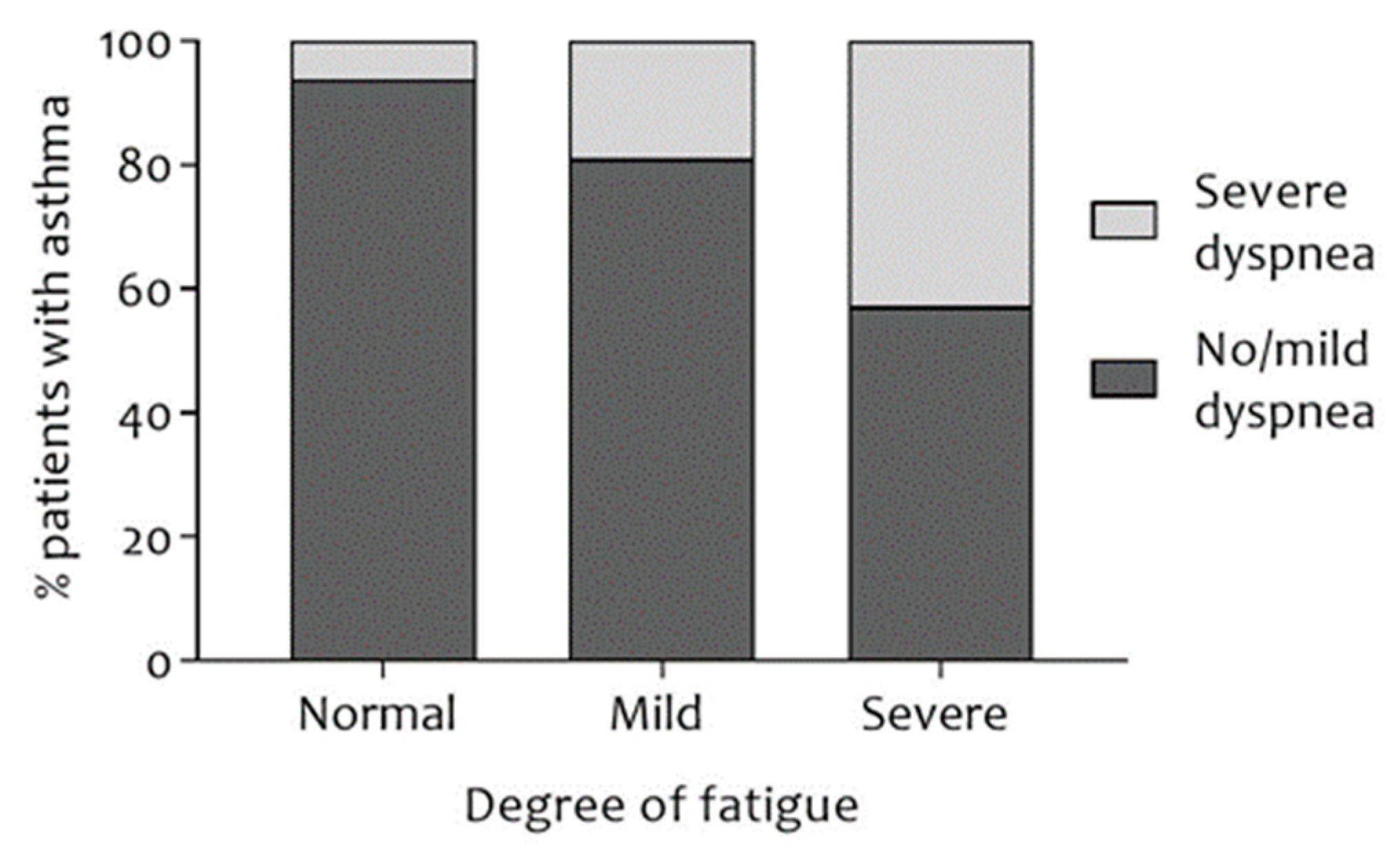
3.3. Differences between Asthmatic Patients with Normal, Mild, and Severe Fatigue
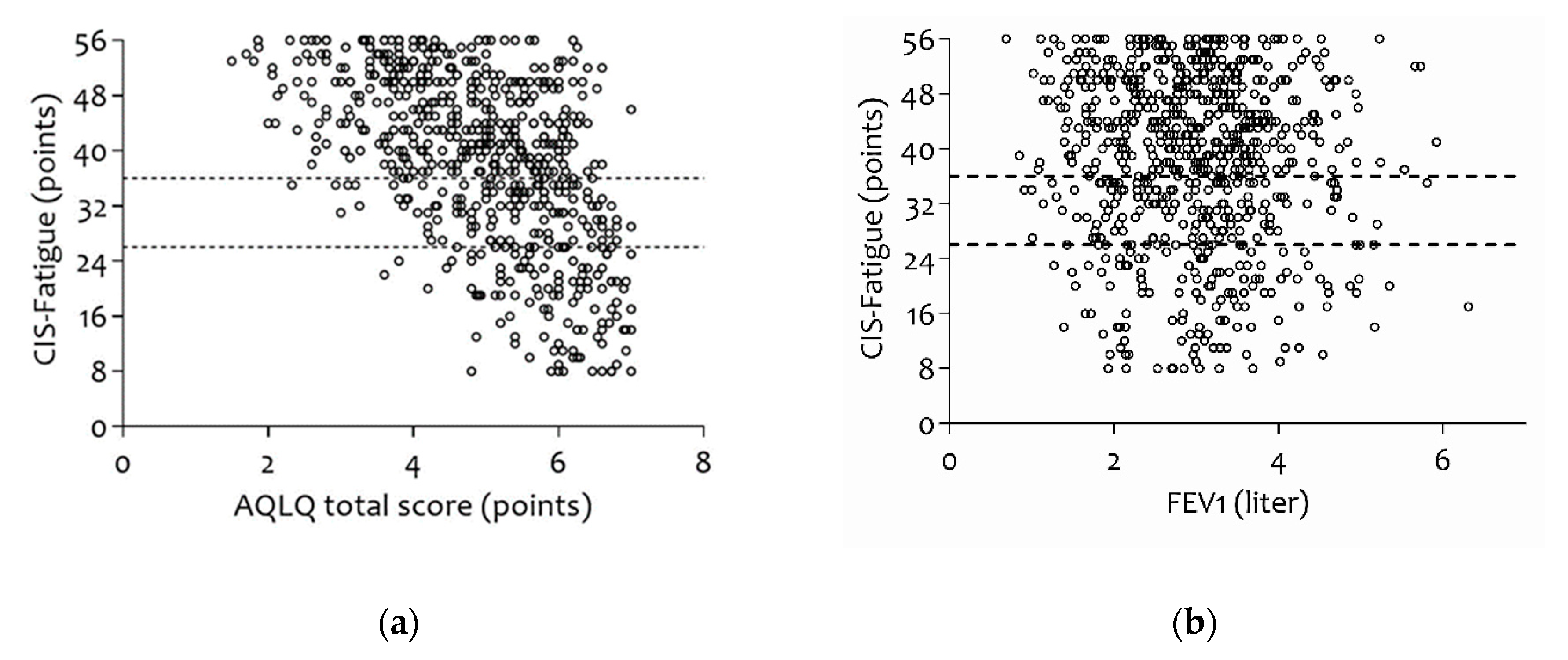
3.4. Correlations and Determinants of Fatigue
3.5. Correlations and Determinants of Disease-Specific QoL
4. Discussion
4.1. Methodological Considerations
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2018. Available online: www.ginasthma.org (accessed on 7 July 2018).
- Rudell, K.; Hareendran, A.; Bonner, N.; Arbuckle, R.; Burbridge, C.; Abetz, L. Patients’ experience of asthma control and clinical guidelines: Perspectives from a qualitative study. Respir. Med. 2012, 106, 909–911. [Google Scholar] [CrossRef] [PubMed]
- Svedsater, H.; Roberts, J.; Patel, C.; Macey, J.; Hilton, E.; Bradshaw, L. Life Impact and Treatment Preferences of Individuals with Asthma and Chronic Obstructive Pulmonary Disease: Results from Qualitative Interviews and Focus Groups. Adv. Ther. 2017, 34, 1466–1481. [Google Scholar] [CrossRef] [PubMed]
- Teodorescu, M.; Consens, F.B.; Bria, W.F.; Coffey, M.J.; McMorris, M.S.; Weatherwax, K.J.; Durance, A.; Palmisano, J.; Senger, C.M.; Chervin, R.D. Correlates of daytime sleepiness in patients with asthma. Sleep Med. 2006, 7, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Landmark-Hoyvik, H.; Reinertsen, K.V.; Loge, J.H.; Kristensen, V.N.; Dumeaux, V.; Fossa, S.D.; Borresen-Dale, A.L.; Edvardsen, H. The genetics and epigenetics of fatigue. PM R J. Inj. Funct. Rehabil. 2010, 2, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Peters, J.B.; Rijssenbeek-Nouwens, L.H.; Bron, A.O.; Fieten, K.B.; Weersink, E.J.; Bel, E.H.; Vercoulen, J.H. Health status measurement in patients with severe asthma. Respir. Med. 2014, 108, 278–286. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Vercoulen, J.H.; Swanink, C.M.; Fennis, J.F.; Galama, J.M.; van der Meer, J.W.; Bleijenberg, G. Dimensional assessment of chronic fatigue syndrome. J. Psychosom. Res. 1994, 38, 383–392. [Google Scholar] [CrossRef] [Green Version]
- Beurskens, A.J.; Bultmann, U.; Kant, I.; Vercoulen, J.H.; Bleijenberg, G.; Swaen, G.M. Fatigue among working people: Validity of a questionnaire measure. Occup. Environ. Med. 2000, 57, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Bultmann, U.; de Vries, M.; Beurskens, A.J.; Bleijenberg, G.; Vercoulen, J.H.; Kant, I. Measurement of prolonged fatigue in the working population: Determination of a cutoff point for the checklist individual strength. J. Occup. Health Psychol. 2000, 5, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Worm-Smeitink, M.; Gielissen, M.; Bloot, L.; van Laarhoven, H.W.M.; van Engelen, B.G.M.; van Riel, P.; Bleijenberg, G.; Nikolaus, S.; Knoop, H. The assessment of fatigue: Psychometric qualities and norms for the Checklist individual strength. J. Psychosom. Res. 2017, 98, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Juniper, E.F.; Guyatt, G.H.; Epstein, R.S.; Ferrie, P.J.; Jaeschke, R.; Hiller, T.K. Evaluation of impairment of health related quality of life in asthma: Development of a questionnaire for use in clinical trials. Thorax 1992, 47, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Juniper, E.F.; Bousquet, J.; Abetz, L.; Bateman, E.D. Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the Asthma Control Questionnaire. Respir. Med. 2006, 100, 616–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.; Zheng, J.; et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef] [PubMed]
- Roffman, C.E.; Buchanan, J.; Allison, G.T. Charlson Comorbidities Index. J. Physiother. 2016, 62, 171. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- Troosters, T.; Gosselink, R.; Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 1999, 14, 270–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akinwande, M.O.; Dikko, H.G.; Samson, A. Variance Inflation Factor: As a Condition for the Inclusion of Suppressor Variable(s) in Regression Analysis. Open J. Stat. 2015, 5, 754–767. [Google Scholar] [CrossRef]
- Dormann, C.F.; Elith, J.; Bacher, S.; Buchmann, C.; Carl, G.; Carre, G.; Marquez, J.R.G.; Gruber, B.; Lafourcade, B.; Leitao, P.J.; et al. Collinearity: A review of methods to deal with it and a simulation study evaluating their performance. Ecography 2013, 36, 27–46. [Google Scholar] [CrossRef]
- Engberg, I.; Segerstedt, J.; Waller, G.; Wennberg, P.; Eliasson, M. Fatigue in the general population—Associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: The northern Sweden MONICA study 2014. BMC Public Health 2017, 17, 654. [Google Scholar] [CrossRef] [PubMed]
- Goërtz, Y.M.J.; Spruit, M.A.; Van’t Hul, A.J.; Vercoulen, J.H.; Van Herck, M., Nakken; Nakken, N.; Djamin, R.S.; Burtin, C.; Thong, M.S.Y.; Coors, A.; et al. Fatigue is highly prevalent in patients with COPD and correlates poorly with the degree of airflow limitation. Manuscript under review.
- Artom, M.; Moss-Morris, R.; Caskey, F.; Chilcot, J. Fatigue in advanced kidney disease. Kidney Int. 2014, 86, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A. The clinical epidemiology of fatigue in newly diagnosed heart failure. BMC Cardiovasc. Disord. 2017, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Boter, H.; Manty, M.; Hansen, A.M.; Hortobagyi, T.; Avlund, K. Self-reported fatigue and physical function in late mid-life. J. Rehabil. Med. 2014, 46, 684–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vercoulen, J.H.; Swanink, C.M.; Galama, J.M.; Fennis, J.F.; Jongen, P.J.; Hommes, O.R.; van der Meer, J.W.; Bleijenberg, G. The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: Development of a model. J. Psychosom. Res. 1998, 45, 507–517. [Google Scholar] [CrossRef]
- Ellingson, L.D.; Kuffel, A.E.; Vack, N.J.; Cook, D.B. Active and sedentary behaviors influence feelings of energy and fatigue in women. Med. Sci. Sports Exerc. 2014, 46, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Rank, M.A.; Bertram, S.L.; Wollan, P.C. Obesity, low levels of physical activity and smoking present opportunities for primary care asthma interventions: An analysis of baseline data from The Asthma Tools Study. NPJ Prim. Care Respir. Med. 2015, 25, 15058. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Vercoulen, J.H.; Sprangers, M.A.G.; Wouters, E.F.M. Fatigue in COPD: An important yet ignored symptom. Lancet Respir. Med. 2017, 5, 542–544. [Google Scholar] [CrossRef]
- Laforest, L.; Van Ganse, E.; Devouassoux, G.; Osman, L.M.; Bauguil, G.; Chamba, G. Patient-reported adverse events under asthma therapy: A community pharmacy-based survey. Clin. Pharmacol. Ther. 2007, 82, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Lacasse, Y.; Wong, E.; Guyatt, G.H.; King, D.; Cook, D.J.; Goldstein, R.S. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet 1996, 348, 1115–1119. [Google Scholar] [CrossRef]
- Carson, K.V.; Chandratilleke, M.G.; Picot, J.; Brinn, M.P.; Esterman, A.J.; Smith, B.J. Physical training for asthma. Cochrane Database Syst. Rev. 2013, CD001116. [Google Scholar] [CrossRef] [PubMed]
- Franca-Pinto, A.; Mendes, F.A.; de Carvalho-Pinto, R.M.; Agondi, R.C.; Cukier, A.; Stelmach, R.; Saraiva-Romanholo, B.M.; Kalil, J.; Martins, M.A.; Giavina-Bianchi, P.; et al. Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: A randomised controlled trial. Thorax 2015, 70, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Joosen, M.; Sluiter, J.; Joling, C.; Frings-Dresen, M. Evaluation of the effects of a training programme for patients with prolonged fatigue on physiological parameters and fatigue complaints. Int. J. Occup. Med. Environ. Health 2008, 21, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Kinsman, R.A.; Luparello, T.; O’Banion, K.; Spector, S. Multidimensional analysis of the subjective symptomatology of asthma. Psychosom. Med. 1973, 35, 250–267. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.; Price, D.; Brown, R. The impact of asthma exacerbations on health-related quality of life in moderate to severe asthma patients in the UK. Prim. Care Respir. J. 2007, 16, 22–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baghai-Ravary, R.; Quint, J.K.; Goldring, J.J.; Hurst, J.R.; Donaldson, G.C.; Wedzicha, J.A. Determinants and impact of fatigue in patients with chronic obstructive pulmonary disease. Respir. Med. 2009, 103, 216–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lukasiewicz, M.; Fareng, M.; Benyamina, A.; Blecha, L.; Reynaud, M.; Falissard, B. Ecological momentary assessment in addiction. Expert Rev. Neurother. 2007, 7, 939–950. [Google Scholar] [CrossRef] [PubMed]


| Variables | Patients with Asthma (n = 733) | Fatigue Severity in Asthmatic Patients | p-Value | ||
|---|---|---|---|---|---|
| Normal Fatigue (n = 138) | Mild Fatigue (n = 136) | Severe Fatigue (n = 459) | |||
| CIS-Fatigue | 38.4 ± 12.4 | 18.5 ± 5.6 | 31.6 ± 2.6 * | 46.4 ± 6.1 *† | <0.001 |
| General Characteristics | |||||
| Gender (male, %) | 302 (41.2) | 78 (56.5) | 55 (40.4) | 169 (36.8) | <0.001 |
| Age (years) | 47.4 ± 16.3 | 50.4 ± 16.4 | 48.5 ± 17.0 | 46.1 ± 15.9 | 0.009 |
| Weight (kg) | 80.7 ± 17.7 | 81.6 ± 20.1 | 78.7 ± 16.8 | 81.1 ± 17.2 | 0.418 |
| BMI (kg/m2) | 27.5 ± 5.5 | 26.5 ± 4.9 | 26.8 ± 4.9 | 28.0 ± 5.8 | 0.019 |
| Underweight (n, %) | 11 (1.5) | 1 (0.7) | 4 (2.9) | 6 (1.3) | 0.005 |
| Normal (n, %) | 242 (33.0) | 55 (39.9) | 42 (30.9) | 145 (31.6) | |
| Overweight (n, %) | 286 (39.8) | 57 (41.3) | 64 (47.1) | 165 (35.9) | |
| Obese (n, %) | 194 (26.5) | 25 (18.1) | 26 (19.1) | 143 (31.2) | |
| Waist circumference a (cm) | 97.5 ± 14.9 | 96.3 ± 13.7 | 96.7 ± 14.4 | 98.2 ± 15.4 | 0.474 |
| Exacerbations last 12 months b (n) | 0 (0–2) | 0 (0–1) | 0 (0–1) | 0 (0–2) * | <0.001 |
| Patients with ≥1 exacerbations last 12 months (n, %) | 281 (44.5) | 33 (28.0) | 50 (45.5) | 198 (49.1) | <0.001 |
| Hospitalization last 12 months c (n) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.344 |
| Patients with ≥1 hospitalization last 12 months (n, %) | 18 (3.0) | 1 (0.9) | 4 (3.8) | 13 (3.4) | 0.326 |
| Smoking status d Current smoker (n,%) | 164 (24.0) | 24 (19.5) | 25 (19.7) | 115 (26.5) | 0.126 |
| Level of education e Secondary general education or higher (n,%) | 295 (43.0) | 68 (51.5) | 62 (51.2) | 165 (38.1) | 0.003 |
| Employment status f Paid work (n, %) | 413 (61.1) | 76 (61.3) | 70 (56.9) | 267 (62.2) | 0.566 |
| Exercise Capacity | |||||
| 6MWT g (m) | 519.1 ± 109.2 | 565.2 ± 93.8 | 525.8 ± 89.0 | 503.5 ± 114.6 * | <0.001 |
| 6MWT g (% predicted) | 71.9 ± 13.8 | 79.4 ± 12.4 | 74.0 ± 11.1 * | 69.1 ± 14.1 *† | <0.001 |
| Patients with <80% predicted g (n, %) | 481 (73.8) | 62 (50.4) | 82 (70.7) | 337 (81.6) | <0.001 |
| Spirometry | |||||
| FEV1 (% predicted) | 87.7 ± 17.4 | 88.3 ± 15.7 | 88.1 ± 19.3 | 87.3 ± 17.4 | 0.867 |
| FEV1 (liter) | 3.0 ± 0.9 | 3.1 ± 1.0 | 2.9 ± 0.9 | 2.9 ± 0.9 | 0.203 |
| FVC (% predicted) | 98.7 ± 14.2 | 102.2 ± 14.2 | 100.4 ± 14.2 | 97.1 ± 14.0 * | 0.001 |
| FVC (liter) | 4.2 ± 1.2 | 4.5 ± 1.3 | 4.2 ± 1.1 | 4.0 ± 1.1 * | <0.001 |
| FEV1/VC * 100 (%) | 71.6 ± 11.9 | 69.1 ± 11.0 | 70.3 ± 11.9 | 72.8 ± 12.0 * | <0.001 |
| Comorbidities | |||||
| CCI h (p) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.200 |
| Persons with ≥1 comorbidities h (n, %) | 70 (17.6) | 8 (11.0) | 14 (18.4) | 48 (19.4) | 0.249 |
| Dyspnea | |||||
| MRC-Dyspnea i (p) | 2 (1–3) | 1 (1–2) | 2 (1–2) * | 2 (2–3) *† | <0.001 |
| MRC grade ≥ 3 (severe dyspnea) i (n, %) | 168 (31.6) | 6 (6.1) | 19 (19.0) | 143 (42.8) | <0.001 |
| Disease-Specific QoL | |||||
| AQLQ j (p) | 4.9 ± 1.3 | 5.9 ± 0.7 | 5.3 ± 1.0 * | 4.5 ± 1.1 *† | <0.001 |
| Symptoms j (p) | 4.7 ± 1.3 | 5.7 ± 0.9 | 5.1 ± 1.2 * | 4.4 ± 1.2 *† | <0.001 |
| Activity limitation j (p) | 4.7 ± 1.5 | 6.1 ± 1.0 | 5.2 ± 1.2 * | 4.1 ± 1.4 *† | <0.001 |
| Emotional function j (p) | 5.3 ± 1.4 | 6.2 ± 0.8 | 5.6 ± 1.2 | 5.0 ± 1.5 *† | <0.001 |
| Environmental exposure j (p) | 5.2 ± 1.5 | 5.9 ± 1.1 | 5.6 ± 1.3 | 4.9 ± 1.5 *† | <0.001 |
| Asthma Control | |||||
| ACQ k (p) | 1.8 ± 1.0 | 1.2 ± 0.7 | 1.6 ± 0.8 * | 2.1 ± 1.0 *† | <0.001 |
| Partially controlled asthmatic patients (n, %) | 170 (25.6) | 53 (43.4) | 39 (31.2) | 78 (18.7) | <0.001 |
| Uncontrolled asthmatic patients (n, %) | 395 (59.5) | 32 (26.2) | 61 (48.8) | 302 (72.4) | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Herck, M.; Spruit, M.A.; Burtin, C.; Djamin, R.; Antons, J.; Goërtz, Y.M.J.; Ebadi, Z.; Janssen, D.J.A.; Vercoulen, J.H.; Peters, J.B.; et al. Fatigue is Highly Prevalent in Patients with Asthma and Contributes to the Burden of Disease. J. Clin. Med. 2018, 7, 471. https://doi.org/10.3390/jcm7120471
Van Herck M, Spruit MA, Burtin C, Djamin R, Antons J, Goërtz YMJ, Ebadi Z, Janssen DJA, Vercoulen JH, Peters JB, et al. Fatigue is Highly Prevalent in Patients with Asthma and Contributes to the Burden of Disease. Journal of Clinical Medicine. 2018; 7(12):471. https://doi.org/10.3390/jcm7120471
Chicago/Turabian StyleVan Herck, Maarten, Martijn A. Spruit, Chris Burtin, Remco Djamin, Jeanine Antons, Yvonne M. J. Goërtz, Zjala Ebadi, Daisy J. A. Janssen, Jan H. Vercoulen, Jeannette B. Peters, and et al. 2018. "Fatigue is Highly Prevalent in Patients with Asthma and Contributes to the Burden of Disease" Journal of Clinical Medicine 7, no. 12: 471. https://doi.org/10.3390/jcm7120471





