Body Mass Index and Waist Circumference as Predictors of Above-Average Increased Cardiovascular Risk Assessed by the SCORE2 and SCORE2-OP Calculators and the Proposition of New Optimal Cut-Off Values: Cross-Sectional Single-Center Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. Circulation 2014, 129, S102–S138. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ambrosi, J.; Silva, C.; Galofré, J.C.; Escalada, J.; Santos, S.; Millán, D.; Vila, N.; Ibañez, P.; Gil, M.J.; Valentí, V.; et al. Body Mass Index Classification Misses Subjects with Increased Cardiometabolic Risk Factors Related to Elevated Adiposity. Int. J. Obes. 2012, 36, 286–294. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA J. Am. Med. Assoc. 2001, 285, 2486–2497. [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic Syndrome-a New World-Wide Definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Dobrowolski, P.; Prejbisz, A.; Kuryłowicz, A.; Baska, A.; Burchardt, P.; Chlebus, K.; Dzida, G.; Jankowski, P.; Jaroszewicz, J.; Jaworski, P.; et al. Metabolic Syndrome—A New Definition and Management Guidelines. A Joint Position Paper by the Polish Society of Hypertension, Polish Society for the Treatment of Obesity, Polish Lipid Association, Polish Association for Study of Liver, Polish Society of Family Medicine, Polish Society of Lifestyle Medicine, Division of Prevention and Epidemiology Polish Cardiac Society, “Club 30” Polish Cardiac Society, and Division of Metabolic and Bariatric Surgery Society of Polish Surgeons. Arch. Med. Sci. 2022, 18, 1133–1156. [Google Scholar] [CrossRef] [PubMed]
- Conroy, R. Estimation of Ten-Year Risk of Fatal Cardiovascular Disease in Europe: The SCORE Project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef] [PubMed]
- Hageman, S.; Pennells, L.; Ojeda, F.; Kaptoge, S.; Kuulasmaa, K.; de Vries, T.; Xu, Z.; Kee, F.; Chung, R.; Wood, A.; et al. SCORE2 Risk Prediction Algorithms: New Models to Estimate 10-Year Risk of Cardiovascular Disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- de Vries, T.I.; Cooney, M.T.; Selmer, R.M.; Hageman, S.H.J.; Pennells, L.A.; Wood, A.; Kaptoge, S.; Xu, Z.; Westerink, J.; Rabanal, K.S.; et al. SCORE2-OP Risk Prediction Algorithms: Estimating Incident Cardiovascular Event Risk in Older Persons in Four Geographical Risk Regions. Eur. Heart J. 2021, 42, 2455–2467. [Google Scholar] [CrossRef]
- North, B.J.; Sinclair, D.A. The Intersection between Aging and Cardiovascular Disease. Circ. Res. 2012, 110, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Pennells, L.; Kaptoge, S.; Østergaard, H.B.; Read, S.H.; Carinci, F.; Franch-Nadal, J.; Petitjean, C.; Taylor, O.; Hageman, S.H.J.; Xu, Z.; et al. SCORE2-Diabetes: 10-Year Cardiovascular Risk Estimation in Type 2 Diabetes in Europe. Eur. Heart J. 2023, 44, 2544–2556. [Google Scholar] [CrossRef]
- Yin, J.; Tian, L. Joint Confidence Region Estimation for Area under ROC Curve and Youden Index. Stat. Med. 2014, 33, 985–1000. [Google Scholar] [CrossRef]
- Mascha, E.J. Identifying the Best Cut-Point for a Biomarker, or Not. Anesth. Analg. 2018, 127, 820–822. [Google Scholar] [CrossRef] [PubMed]
- Macek, P.; Biskup, M.; Terek-Derszniak, M.; Krol, H.; Smok-Kalwat, J.; Gozdz, S.; Zak, M. Optimal Cut-off Values for Anthropometric Measures of Obesity in Screening for Cardiometabolic Disorders in Adults. Sci. Rep. 2020, 10, 11253. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, B.R.; Magalhães, E.I.d.S.; Bragança, M.L.B.M.; Coelho, C.C.N.d.S.; Lima, N.P.; Bettiol, H.; Barbieri, M.A.; Cardoso, V.C.; Santos, A.M.d.; Horta, B.L.; et al. Performance of Body Fat Percentage, Fat Mass Index and Body Mass Index for Detecting Cardiometabolic Outcomes in Brazilian Adults. Nutrients 2023, 15, 2974. [Google Scholar] [CrossRef] [PubMed]
- Głuszek, S.; Ciesla, E.; Głuszek-Osuch, M.; Kozieł, D.; Kiebzak, W.; Wypchło, Ł.; Suliga, E. Anthropometric Indices and Cut-off Points in the Diagnosis of Metabolic Disorders. PLoS ONE 2020, 15, e0235121. [Google Scholar] [CrossRef] [PubMed]
- Cardinal, T.R.; Vigo, A.; Duncan, B.B.; Matos, S.M.A.; da Fonseca, M.d.J.M.; Barreto, S.M.; Schmidt, M.I. Optimal Cut-off Points for Waist Circumference in the Definition of Metabolic Syndrome in Brazilian Adults: Baseline Analyses of the Longitudinal Study of Adult Health (ELSA-Brasil). Diabetol. Metab. Syndr. 2018, 10, 49. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Martínez-Sanguinetti, M.A.; Ho, F.K.; Celis-Morales, C.; Pizarro, A. Optimal Cut-off Points for Waist Circumference in the Definition of Metabolic Syndrome in Chile. Public Health Nutr. 2020, 23, 2898–2903. [Google Scholar] [CrossRef]
- Prasad, D.; Kabir, Z.; Suganthy, J.; Dash, A.; Das, B. Appropriate Anthropometric Indices to Identify Cardiometabolic Risk in South Asians. WHO South East Asia J. Public Health 2013, 2, 142. [Google Scholar] [CrossRef]
- Wang, H.; Liu, A.; Zhao, T.; Gong, X.; Pang, T.; Zhou, Y.; Xiao, Y.; Yan, Y.; Fan, C.; Teng, W.; et al. Comparison of Anthropometric Indices for Predicting the Risk of Metabolic Syndrome and Its Components in Chinese Adults: A Prospective, Longitudinal Study. BMJ Open 2017, 7, e016062. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Kim, N.H.; Kwon, T.Y.; Kim, S.G. A Novel Adiposity Index as an Integrated Predictor of Cardiometabolic Disease Morbidity and Mortality. Sci. Rep. 2018, 8, 16753. [Google Scholar] [CrossRef] [PubMed]
- Wen, S.-H.; Tang, X.; Tang, T.; Ye, Z.-R. Association between Weight-Adjusted-Waist Index and Gallstones: An Analysis of the National Health and Nutrition Examination Survey. BMC Gastroenterol. 2024, 24, 40. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.-T.; Wang, X.-M.; Zhong, Y.-S.; Zhong, W.-F.; Song, W.-Q.; Wu, X.-B. Association of Changes in Waist Circumference, Waist-to-Height Ratio and Weight-Adjusted-Waist Index with Multimorbidity among Older Chinese Adults: Results from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). BMC Public Health 2024, 24, 318. [Google Scholar] [CrossRef]
- Hu, Q.; Han, K.; Shen, J.; Sun, W.; Gao, L.; Gao, Y. Association of Weight-Adjusted-Waist Index with Non-Alcoholic Fatty Liver Disease and Liver Fibrosis: A Cross-Sectional Study Based on NHANES. Eur. J. Med. Res. 2023, 28, 263. [Google Scholar] [CrossRef] [PubMed]
- Suwała, S.; Białczyk, A.; Koperska, K.; Rajewska, A.; Krintus, M.; Junik, R. Prevalence and Crucial Parameters in Diabesity-Related Liver Fibrosis: A Preliminary Study. J. Clin. Med. 2023, 12, 7760. [Google Scholar] [CrossRef] [PubMed]
- Stefanska, A.; Bergmann, K.; Suwała, S.; Mankowska-Cyl, A.; Kozinski, M.; Junik, R.; Krintus, M.; Panteghini, M. Performance Evaluation of a Novel Non-Invasive Test for the Detection of Advanced Liver Fibrosis in Metabolic Dysfunction-Associated Fatty Liver Disease. Metabolites 2024, 14, 52. [Google Scholar] [CrossRef] [PubMed]
- Schorr, M.; Dichtel, L.E.; Gerweck, A.V.; Valera, R.D.; Torriani, M.; Miller, K.K.; Bredella, M.A. Sex Differences in Body Composition and Association with Cardiometabolic Risk. Biol. Sex Differ. 2018, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Gruzdeva, O.; Borodkina, D.; Uchasova, E.; Dyleva, Y.; Barbarash, O. Localization of Fat Depots and Cardiovascular Risk. Lipids Health Dis. 2018, 17, 218. [Google Scholar] [CrossRef] [PubMed]
- Van Trier, T.; Snaterse, M.; Boekholdt, S.M.; Scholte Op Reimer, W.J.M.; Visseren, F.L.J.; Hageman, S.H.J.; Dorresteijn, J.A.N.; Wareham, N.J.; Peters, R.J.G.; Jorstad, H.T. External Validation of Systematic COronary Risk Evaluation 2—Older Persons (SCORE2-OP) in the EPIC-Norfolk Prospective Population Study. Eur. J. Prev. Cardiol. 2023, 30, i433. [Google Scholar] [CrossRef]
- van Trier, T.J.; Snaterse, M.; Boekholdt, S.M.; Scholte op Reimer, W.J.M.; Hageman, S.H.J.; Visseren, F.L.J.; Dorresteijn, J.A.N.; Peters, R.J.G.; Jørstad, H.T. Validation of Systematic Coronary Risk Evaluation 2 (SCORE2) and SCORE2-Older Persons in the EPIC-Norfolk Prospective Population Cohort. Eur. J. Prev. Cardiol. 2024, 31, 182–189. [Google Scholar] [CrossRef]
- Kasim, S.S.; Ibrahim, N.; Malek, S.; Ibrahim, K.S.; Aziz, M.F.; Song, C.; Chia, Y.C.; Ramli, A.S.; Negishi, K.; Mat Nasir, N. Validation of the General Framingham Risk Score (FRS), SCORE2, Revised PCE and WHO CVD Risk Scores in an Asian Population. Lancet Reg. Health West. Pac. 2023, 35, 100742. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Manent, J.I.; Jover, A.M.; Martinez, C.S.; Tomás-Gil, P.; Martí-Lliteras, P.; López-González, Á.A. Waist Circumference Is an Essential Factor in Predicting Insulin Resistance and Early Detection of Metabolic Syndrome in Adults. Nutrients 2023, 15, 257. [Google Scholar] [CrossRef] [PubMed]
- Nkwana, M.R.; Monyeki, K.D.; Lebelo, S.L. Body Roundness Index, A Body Shape Index, Conicity Index, and Their Association with Nutritional Status and Cardiovascular Risk Factors in South African Rural Young Adults. Int. J. Environ. Res. Public Health 2021, 18, 281. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Lee, M.; Sung, K. Prediction of Mortality with A Body Shape Index in Young Asians: Comparison with Body Mass Index and Waist Circumference. Obesity 2018, 26, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
- Venkatrao, M.; Nagarathna, R.; Patil, S.S.; Singh, A.; Rajesh, S.K.; Nagendra, H. A Composite of BMI and Waist Circumference May Be a Better Obesity Metric in Indians with High Risk for Type 2 Diabetes: An Analysis of NMB-2017, a Nationwide Cross-Sectional Study. Diabetes Res. Clin. Pract. 2020, 161, 108037. [Google Scholar] [CrossRef]

| Group | Cut-Off to Define ICVR in Specific Group |
|---|---|
| Females, 40–44 years old, non-smokers | >1% |
| Females, 40–44 years old, smokers | >4% |
| Males, 40–44 years old, non-smokers | >2% |
| Males, 40–44 years old, smokers | >5% |
| Females, 45–49 years old, non-smokers | >2% |
| Females, 45–49 years old, smokers | >4% |
| Males, 45–49 years old, non-smokers | >3% |
| Males, 45–49 years old, smokers | >6% |
| Females, 50–54 years old, non-smokers | >3% |
| Females, 50–54 years old, smokers | >9% |
| Males, 50–54 years old, non-smokers | >4% |
| Males, 50–54 years old, smokers | >10% |
| Females, 55–59 years old, non-smokers | >9% |
| Females, 55–59 years old, smokers | >10% |
| Males, 55–59 years old, non-smokers | >11% |
| Males, 55–59 years old, smokers | >12% |
| Females, 60–64 years old, non-smokers | >7% |
| Females, 60–64 years old, smokers | >13% |
| Males, 60–64 years old, non-smokers | >8% |
| Males, 60–64 years old, smokers | >13% |
| Females, 65–44 years old, non-smokers | >10% |
| Females, 65–69 years old, smokers | >16% |
| Males, 65–69 years old, non-smokers | >11% |
| Males, 65–69 years old, smokers | >17% |
| Females, 70–74 years old, non-smokers | >14% |
| Females, 70–74 years old, smokers | >27% |
| Males, 70–74 years old, non-smokers | >15% |
| Males, 70–74 years old, smokers | >29% |
| Females, 75–79 years old, non-smokers | >22% |
| Females, 75–79 years old, smokers | >28% |
| Males, 75–79 years old, non-smokers | >23% |
| Males, 75–79 years old, smokers | >33% |
| Females, 80–84 years old, non-smokers | >31% |
| Females, 80–84 years old, smokers | >40% |
| Males, 80–84 years old, non-smokers | >29% |
| Males, 80–84 years old, smokers | >42% |
| Females, 85–89 years old, non-smokers | >47% |
| Females, 85–89 years old, smokers | >52% |
| Males, 85–89 years old, non-smokers | >43% |
| Males, 80–89 years old, smokers | >50% |
| Cut-Off Point | Group (Males/Female) | Se [%] | Sp [%] | NPV [%] | PPV [%] | DA [%] | YI |
|---|---|---|---|---|---|---|---|
| Body mass index | |||||||
| 25.0 kg/m2 | Males | 95.8 | 60.2 | 95.7 | 40.0 | 56.3 | 0.355 |
| Females | 89.7 | 38.5 | 89.4 | 39.5 | 54.3 | 0.283 | |
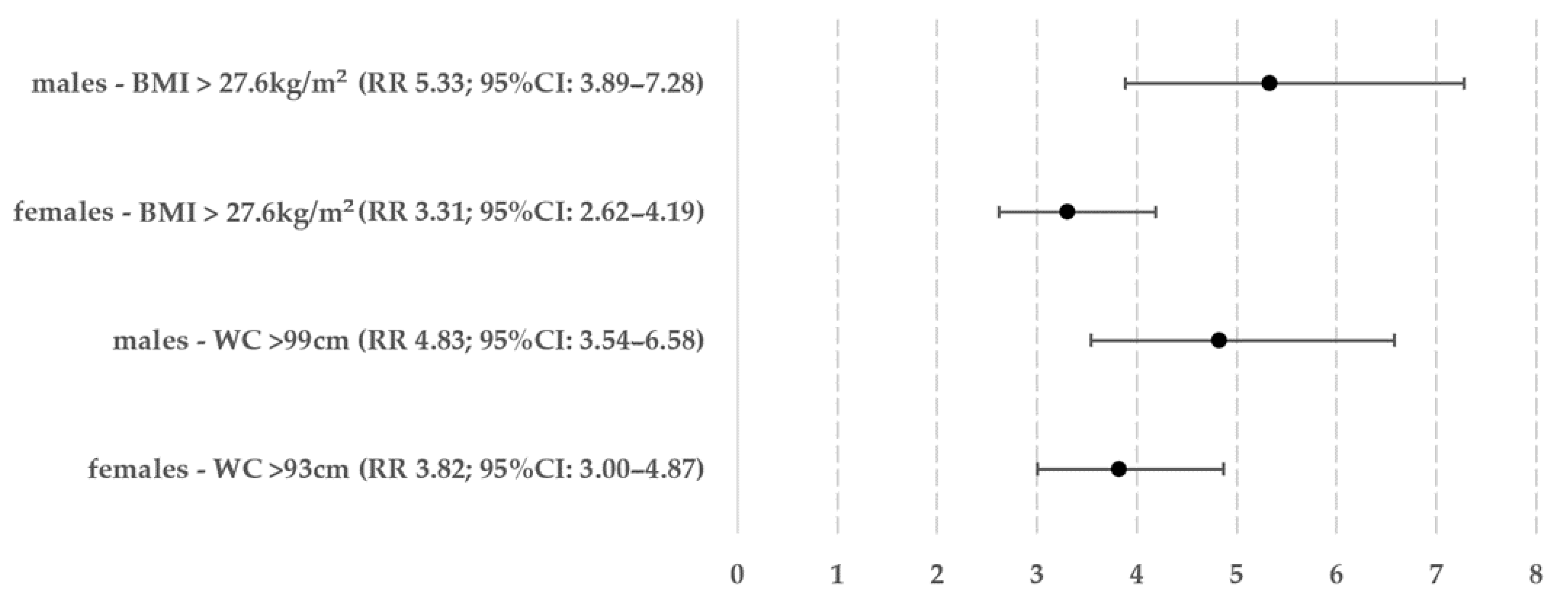
| 27.6 kg/m2 | Males | 86.2 | 60.1 | 91.2 | 47.6 | 67.8 | 0.463 |
| Females | 75.4 | 36.6 | 85.2 | 47.9 | 67.1 | 0.388 | |
| 30.0 kg/m2 | Males | 58.0 | 83.5 | 82.6 | 59.6 | 76.0 | 0.415 |
| Females | 47.8 | 82.3 | 77.9 | 54.7 | 71.6 | 0.301 | |
| Waist circumference | |||||||
| 80 cm | Females | 99.7 | 7.5 | 98.3 | 32.5 | 36.0 | 0.072 |
| 88 cm | Females | 89.7 | 39.1 | 89.5 | 39.7 | 54.7 | 0.288 |
| 93 cm | Females | 80.9 | 60.0 | 87.6 | 47.5 | 66.5 | 0.410 |
| 94 cm | Males | 95.1 | 39.8 | 95.0 | 39.9 | 56.1 | 0.348 |
| 99 cm | Males | 85.9 | 57.0 | 90.6 | 45.6 | 65.5 | 0.428 |
| 102 cm | Males | 70.3 | 70.8 | 85.6 | 50.3 | 70.6 | 0.411 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suwała, S.; Junik, R. Body Mass Index and Waist Circumference as Predictors of Above-Average Increased Cardiovascular Risk Assessed by the SCORE2 and SCORE2-OP Calculators and the Proposition of New Optimal Cut-Off Values: Cross-Sectional Single-Center Study. J. Clin. Med. 2024, 13, 1931. https://doi.org/10.3390/jcm13071931
Suwała S, Junik R. Body Mass Index and Waist Circumference as Predictors of Above-Average Increased Cardiovascular Risk Assessed by the SCORE2 and SCORE2-OP Calculators and the Proposition of New Optimal Cut-Off Values: Cross-Sectional Single-Center Study. Journal of Clinical Medicine. 2024; 13(7):1931. https://doi.org/10.3390/jcm13071931
Chicago/Turabian StyleSuwała, Szymon, and Roman Junik. 2024. "Body Mass Index and Waist Circumference as Predictors of Above-Average Increased Cardiovascular Risk Assessed by the SCORE2 and SCORE2-OP Calculators and the Proposition of New Optimal Cut-Off Values: Cross-Sectional Single-Center Study" Journal of Clinical Medicine 13, no. 7: 1931. https://doi.org/10.3390/jcm13071931




