Odontoid Fracture with Accompanying Severe Atlantoaxial Instability in Elderly Patients—Analysis of Treatment, Adverse Events, and Outcome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Patients’ Data
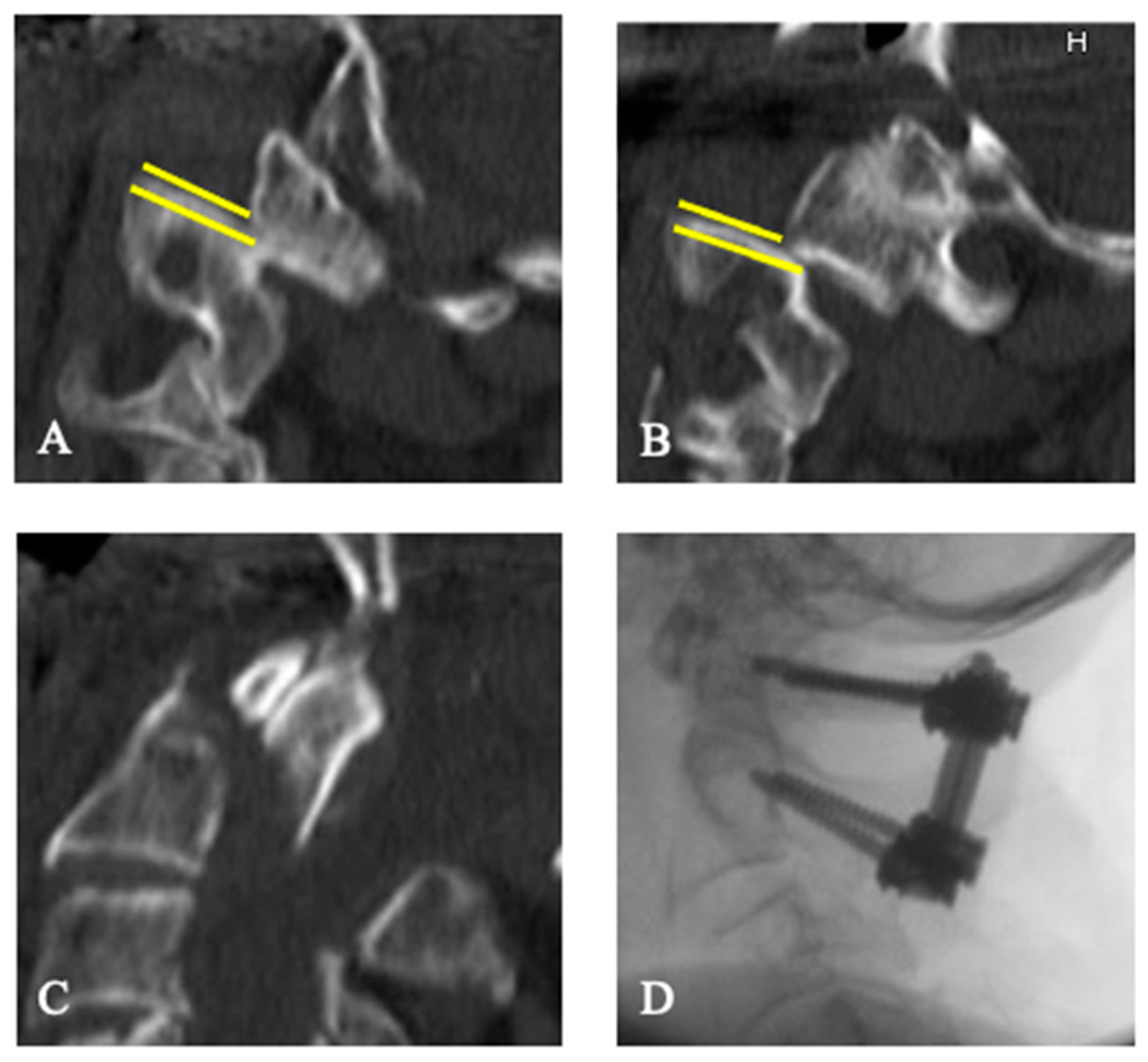
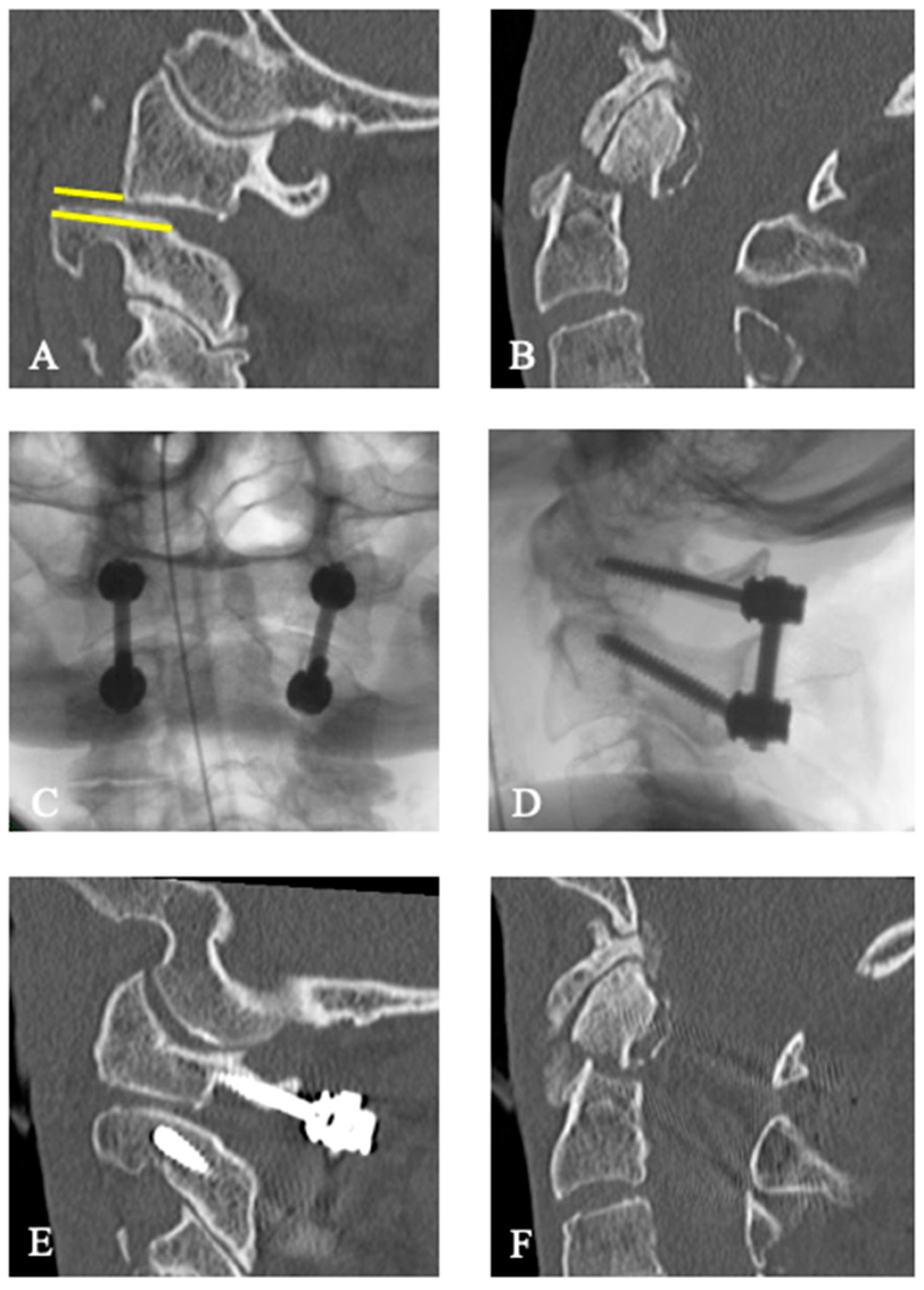
2.3. Treatment of the Patients
2.4. Evaluation of Adverse Events
2.5. Clinical Evaluation
2.6. Radiological Evaluation
2.7. Endpoints
2.8. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Treatment
3.3. Adverse Events
3.4. Outcome
3.4.1. Functional Outcome
3.4.2. Secondary Dislocations
4. Discussion
4.1. Evidence in Treatment of Type II Odontoid Fractures
4.2. Evidence in Treatment of Odontoid Fractures with AAI
4.3. Adverse Events and Mortality
4.4. Functional Outcome
4.5. Radiological Outcome
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hasler, R.M.; Exadaktylos, A.K.; Bouamra, O.; Benneker, L.M.; Clancy, M.; Sieber, R.; Zimmermann, H.; Lecky, F. Epidemiology and Predictors of Cervical Spine Injury in Adult Major Trauma Patients: A Multicenter Cohort Study. J. Trauma Acute Care Surg. 2012, 72, 975–981. [Google Scholar] [CrossRef]
- Smith, H.E.; Kerr, S.M.; Fehlings, M.G.; Chapman, J.; Maltenfort, M.; Zavlasky, J.; Harris, E.; Albert, T.J.; Harrop, J.; Hilibrand, A.S.; et al. Trends in Epidemiology and Management of Type II Odontoid Fractures: 20-Year Experience at a Model System Spine Injury Tertiary Referral Center. J. Spinal Disord. Tech. 2010, 23, 501–505. [Google Scholar] [CrossRef]
- Robinson, A.-L.; Olerud, C.; Robinson, Y. Epidemiology of C2 Fractures in the 21st Century: A National Registry Cohort Study of 6,370 Patients from 1997 to 2014. Adv. Orthop. 2017, 2017, 6516893. [Google Scholar] [CrossRef]
- Chapman, J.; Smith, J.S.; Kopjar, B.; Vaccaro, A.R.; Arnold, P.; Shaffrey, C.I.; Fehlings, M.G. The AOSpine North America Geriatric Odontoid Fracture Mortality Study: A Retrospective Review of Mortality Outcomes for Operative versus Nonoperative Treatment of 322 Patients with Long-Term Follow-Up. Spine 2013, 38, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Kepler, C.K.; Kopjar, B.; Chapman, J.; Shaffrey, C.; Arnold, P.; Gokaslan, Z.; Brodke, D.; France, J.; Dekutoski, M.; et al. Functional and Quality-of-Life Outcomes in Geriatric Patients with Type-II Dens Fracture. J. Bone Jt. Surg. Am. 2013, 95, 729–735. [Google Scholar] [CrossRef]
- Venkatesan, M.; Northover, J.R.; Wild, J.B.; Johnson, N.; Lee, K.; Uzoigwe, C.E.; Braybrooke, J.R. Survival Analysis of Elderly Patients with a Fracture of the Odontoid Peg. Bone Jt. J. 2014, 96-B, 88–93. [Google Scholar] [CrossRef]
- Schroeder, G.D.; Kepler, C.K.; Kurd, M.F.; Paul, J.T.; Rubenstein, R.N.; Harrop, J.S.; Brodke, D.S.; Chapman, J.R.; Vaccaro, A.R. A Systematic Review of the Treatment of Geriatric Type II Odontoid Fractures. Neurosurgery 2015, 77 (Suppl. S4), S6–S14. [Google Scholar] [CrossRef]
- Sarode, D.P.; Demetriades, A.K. Surgical versus Nonsurgical Management for Type II Odontoid Fractures in the Elderly Population: A Systematic Review. Spine J. 2018, 18, 1921–1933. [Google Scholar] [CrossRef]
- Yang, Z.; Yuan, Z.-Z.; Ma, J.-X.; Ma, X.-L. Conservative versus Surgical Treatment for Type II Odontoid Fractures in the Elderly: Grading the Evidence through a Meta-Analysis. Orthop. Traumatol. Surg. Res. 2015, 101, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Warburton, R.N.; Parke, B.; Church, W.; McCusker, J. Identification of Seniors at Risk: Process Evaluation of a Screening and Referral Program for Patients Aged > or =75 in a Community Hospital Emergency Department. Int. J. Health Care Qual. Assur. Inc. Leadersh. Health Serv. 2004, 17, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Barlow, D.R.; Higgins, B.T.; Ozanne, E.M.; Tosteson, A.N.A.; Pearson, A.M. Cost Effectiveness of Operative Versus Non-Operative Treatment of Geriatric Type-II Odontoid Fracture. Spine 2016, 41, 610–617. [Google Scholar] [CrossRef]
- Evaniew, N.; Yarascavitch, B.; Madden, K.; Ghert, M.; Drew, B.; Bhandari, M.; Kwok, D. Atlantoaxial Instability in Acute Odontoid Fractures Is Associated with Nonunion and Mortality. Spine J. 2015, 15, 910–917. [Google Scholar] [CrossRef]
- Wang, L.; Liu, C.; Zhao, Q.-H.; Tian, J.-W. Outcomes of Surgery for Unstable Odontoid Fractures Combined with Instability of Adjacent Segments. J. Orthop. Surg. Res. 2014, 9, 64. [Google Scholar] [CrossRef]
- Minyu, Z.; Shiyang, W.; Suraj, C.; Kelun, H.; Chaowei, L.; Honglin, T. Traumatic Posterolateral C1-C2 Dislocation Complicated with Locked Lateral Mass and Type II Odontoid Fracture-5-Year Follow-Up. World Neurosurg. 2018, 114, 330–334. [Google Scholar] [CrossRef]
- Moreau, P.E.; Nguyen, V.; Atallah, A.; Kassab, G.; Thiong’o, M.W.; Laporte, C. Traumatic Atlantoaxial Dislocation with Odontoid Fracture: A Case Report. Orthop. Traumatol. Surg. Res. 2012, 98, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Riouallon, G.; Pascal-Moussellard, H. Atlanto-Axial Dislocation Complicating a Type II Odontoid Fracture. Reduction and Final Fixation. Orthop. Traumatol. Surg. Res. 2014, 100, 341–345. [Google Scholar] [CrossRef]
- He, D.-W.; Huang, W.-J.; Sheng, X.-Y.; Wu, L.-J.; Fan, S.-W. Atlantoaxial Joint Interlocking Following Type II Odontoid Fracture Associated with Posterolateral Atlantoaxial Dislocation: A Case Report and Review of Published Reports. Orthop. Surg. 2016, 8, 405–410. [Google Scholar] [CrossRef] [PubMed]
- McCabe, C.M.J.; McLachlin, S.D.; Bailey, S.I.; Gurr, K.R.; Bailey, C.S.; Dunning, C.E. The Effect of Soft-Tissue Restraints after Type II Odontoid Fractures in the Elderly: A Biomechanical Study. Spine 2012, 37, 1030–1035. [Google Scholar] [CrossRef] [PubMed]
- Agha, R.A.; Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; O’Neill, N. PROCESS Group The PROCESS 2020 Guideline: Updating Consensus Preferred Reporting Of CasESeries in Surgery (PROCESS) Guidelines. Int. J. Surg. 2020, 84, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.D.; D’Alonzo, R.T. Fractures of the Odontoid Process of the Axis. J. Bone Jt. Surg. Am. 1974, 56, 1663–1674. [Google Scholar] [CrossRef] [PubMed]
- Grauer, J.N.; Shafi, B.; Hilibrand, A.S.; Harrop, J.S.; Kwon, B.K.; Beiner, J.M.; Albert, T.J.; Fehlings, M.G.; Vaccaro, A.R. Proposal of a Modified, Treatment-Oriented Classification of Odontoid Fractures. Spine J. 2005, 5, 123–129. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Koerner, J.D.; Radcliff, K.E.; Oner, F.C.; Reinhold, M.; Schnake, K.J.; Kandziora, F.; Fehlings, M.G.; Dvorak, M.F.; Aarabi, B.; et al. AOSpine Subaxial Cervical Spine Injury Classification System. Eur. Spine J. 2016, 25, 2173–2184. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Hilibrand, A.S. Rheumatoid Arthritis in the Cervical Spine. J. Am. Acad. Orthop. Surg. 2005, 13, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Molina, C.A.; Gokaslan, Z.L.; Sciubba, D.M. Diagnosis and Management of Metastatic Cervical Spine Tumors. Orthop. Clin. N. Am. 2012, 43, 75–87, viii–ix. [Google Scholar] [CrossRef] [PubMed]
- Cauchoix, J.; Binet, J.P. Anterior Surgical Approaches to the Spine. Ann. R. Coll. Surg. Engl. 1957, 21, 237–243. [Google Scholar] [PubMed]
- Harms, J.; Melcher, R.P. Posterior C1-C2 Fusion with Polyaxial Screw and Rod Fixation. Spine 2001, 26, 2467–2471. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, A.J.; Bono, C.M.; Reichmann, W.M.; Warholic, N.; Wood, K.B.; Losina, E.; Katz, J.N.; Harris, M.B. Type II Odontoid Fractures of the Cervical Spine: Do Treatment Type and Medical Comorbidities Affect Mortality in Elderly Patients? Spine 2011, 36, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Robinson, Y.; Robinson, A.-L.; Olerud, C. Systematic Review on Surgical and Nonsurgical Treatment of Type II Odontoid Fractures in the Elderly. Biomed. Res. Int. 2014, 2014, 231948. [Google Scholar] [CrossRef]
- Chibbaro, S.; Mallereau, C.-H.; Ganau, M.; Zaed, I.; Teresa Bozzi, M.; Scibilia, A.; Cebula, H.; Ollivier, I.; Loit, M.-P.; Chaussemy, D.; et al. Odontoid Type II Fractures in Elderly: What Are the Real Management Goals and How to Best Achieve Them? A Multicenter European Study on Functional Outcome. Neurosurg. Rev. 2022, 45, 709–718. [Google Scholar] [CrossRef]
- White, A.P.; Hashimoto, R.; Norvell, D.C.; Vaccaro, A.R. Morbidity and Mortality Related to Odontoid Fracture Surgery in the Elderly Population. Spine 2010, 35, S146–S157. [Google Scholar] [CrossRef] [PubMed]
- Harrop, J.S.; Sharan, A.D.; Przybylski, G.J. Epidemiology of Spinal Cord Injury after Acute Odontoid Fractures. Neurosurg. Focus. 2000, 8, e4. [Google Scholar] [CrossRef] [PubMed]
- Surkan, M.J.; Gibson, W. Interventions to Mobilize Elderly Patients and Reduce Length of Hospital Stay. Can. J. Cardiol. 2018, 34, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.T.; Theologis, A.A.; Sing, D.; Tay, B. Anterior Versus Posterior Approaches for Odontoid Fracture Stabilization in Patients Older Than 65 Years: 30-Day Morbidity and Mortality in a National Database. Clin. Spine Surg. 2017, 30, E1033–E1038. [Google Scholar] [CrossRef]
- Platzer, P.; Thalhammer, G.; Oberleitner, G.; Schuster, R.; Vécsei, V.; Gaebler, C. Surgical Treatment of Dens Fractures in Elderly Patients. J. Bone Jt. Surg. Am. 2007, 89, 1716–1722. [Google Scholar] [CrossRef]
- Smith, J.S.; Kepler, C.K.; Kopjar, B.; Harrop, J.S.; Arnold, P.; Chapman, J.R.; Fehlings, M.G.; Vaccaro, A.R.; Shaffrey, C.I. Effect of Type II Odontoid Fracture Nonunion on Outcome among Elderly Patients Treated without Surgery: Based on the AOSpine North America Geriatric Odontoid Fracture Study. Spine 2013, 38, 2240–2246. [Google Scholar] [CrossRef]

| Conservative Treatment n = 11 | Ventral Surgery n = 8 | Dorsal Surgery n = 20 | p | |
|---|---|---|---|---|
| Mean age, years (range) | 82.6 (66–93) | 79.9 (67–90) | 78.8 (65–92) | 0.5049 |
| Classification according to Grauer, n (%) | 0.0998 | |||
| Grauer 2 A | 2 (18.2) | 0 (0.0) | 0 (0.0) | |
| Grauer 2 B | 8 (72.7) | 5 (62.5) | 17 (85.0) | |
| Grauer 2 C | 1 (9.1) | 3 (37.5) | 3 (15.0) | |
| Sex, n (%) | 0.5788 | |||
| Female | 5 (45.5) | 5 (62.5) | 8 (40) | |
| Male | 6 (54.5) | 3 (37.5) | 12 (60) | |
| Median GCS (CI) | 15 (14–15) | 15 (14–15) | 15 (15–15) | 0.1448 |
| Medical comorbidities, n (%) | ||||
| Cardiological | 7 (63.6) | 5 (62.5) | 14 (70.0) | |
| Pulmonary | 3 (27.3) | 1 (12.5) | 1 (5.0) | |
| Metabolic | 6 (54.5) | 3 (37.5) | 9 (45.0) | |
| Traumatic | 9 (81.8) | 3 (37.5) | 6 (30.0) | |
| Neurological | 0 (0.0) | 2 (25.0) | 6 (30.0) | |
| Psychiatrically | 3 (27.3) | 1 (12.5) | 2 (10.0) | |
| Allergies | 0 (0.0) | 0 (0.0) | 2 (10.0) | |
| Cancer | 0 (0.0) | 0 (0.0) | 2 (10.0) | |
| Other | 3 (27.3) | 2 (25.0) | 3 (15.0) | |
| Concomitant spine injuries, n (%) | ||||
| Upper cervical spine | 6 (54.5) | 4 (50.0) | 6 (30.0) | |
| Lower cervical spine | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Spinal column | 0 (0.0) | 1 (12.5) | 0 (0.0) | |
| Concomitant injuries, n (%) | ||||
| Traumatic brain injury | 5 (54.5) | 0 (0.0) | 2 (10.0) | |
| Pelvic fracture | 0 (0.0) | 1 (12.5) | 0 (0.0) | |
| Fracture of the extremities | 2 (18.2) | 2 (25.0) | 3 (15.0) | |
| Skull fracture | 6 (54.5) | 2 (25.0) | 4 (20.0) | |
| Traumatic neurological deficits | 0 (0.0) | 1 (12.5) | 3 (15.0) |
| Treatment, Complications | Conservative Treatment n = 11 | Ventral Surgery n = 8 | Dorsal Surgery n = 20 | p |
|---|---|---|---|---|
| Mean operation time, minutes (range) | 52.3 (23–85) | 176.2 (86–315) | <0.0001 | |
| Median time at the hospital, days (CI) | 5.0 (3–10) | 11.0 (5–20) | 14.5 (13–21) | <0.0001 |
| Surgical adverse events, n (%) | ||||
| Grade I | 0 (0.0) | 0 (0.0) | 1 (5.0) | |
| Grade II | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Grade III | 0 (0.0) | 1 (12.5) | 1 (5.0) | |
| Grade IV | 0 (0.0) | 0 (0.0) | 2 (10.0) | |
| Grade V | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Non-surgical adverse events, n (%) | ||||
| Grade I | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Grade II | 1 (9.1) | 0 (0.0) | 3 (15.0) | |
| Grade III | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Grade IV | 0 (0.0) | 0 (0.0) | 2 (10.0) | |
| Grade V | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Functional Outcome | Conservative Treatment n = 9 | Ventral Surgery n = 5 | Dorsal Surgery n = 11 | p |
|---|---|---|---|---|
| Mean ROM, | ||||
| degree (range) | ||||
| Flexion | 26.0 (20–30) | 24.0 (20–30) | 25.0 (20–30) | 0.7863 |
| Extension | 23.3 (10–40) | 22.0 (10–40) | 26.0 (10–40) | 0.8743 |
| Lateral bending right | 23.1 (10–35) | 23.0 (10–35) | 16.4 (10–30) | 0.1452 |
| Lateral bending left | 23.8 (15–35) | 23.0 (10–35) | 18.6 (10–30) | 0.3191 |
| Rotation right | 33.1 (10–45) | 35.0 (10–60) | 37.7 (10–60) | 0.8565 |
| Rotation left | 30.6 (15–40) | 33.0 (10–60) | 38.6 (15–60) | 0.4966 |
| Pain, n (%) | ||||
| Yes | 1 (11.1) | 3 (60.0) | 5 (45.5) | |
| No | 8 (88.9) | 2 (40.0) | 6 (54.5) | |
| Neurology, n (%) | ||||
| Yes | 1 (11.1) | 0 (0.0) | 3 (27.3) | |
| No | 8 (88.9) | 5 (100.0) | 8 (72.7) | |
| Radiological Outcome | Conservative Treatment n = 9 | Ventral Surgery n = 5 | Dorsal Surgery n = 11 | |
| Dislocation, n (%) | ||||
| Yes | 1 (11.1) | 2 (40.0) | 1 (9.1) | |
| No | 8 (88.9) | 3 (60.0) | 10 (90.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kreinest, M.; Raisch, P.; Hörnig, L.; Vetter, S.Y.; Grützner, P.A.; Jung, M.K. Odontoid Fracture with Accompanying Severe Atlantoaxial Instability in Elderly Patients—Analysis of Treatment, Adverse Events, and Outcome. J. Clin. Med. 2024, 13, 1326. https://doi.org/10.3390/jcm13051326
Kreinest M, Raisch P, Hörnig L, Vetter SY, Grützner PA, Jung MK. Odontoid Fracture with Accompanying Severe Atlantoaxial Instability in Elderly Patients—Analysis of Treatment, Adverse Events, and Outcome. Journal of Clinical Medicine. 2024; 13(5):1326. https://doi.org/10.3390/jcm13051326
Chicago/Turabian StyleKreinest, Michael, Philipp Raisch, Lukas Hörnig, Sven Y. Vetter, Paul A. Grützner, and Matthias K. Jung. 2024. "Odontoid Fracture with Accompanying Severe Atlantoaxial Instability in Elderly Patients—Analysis of Treatment, Adverse Events, and Outcome" Journal of Clinical Medicine 13, no. 5: 1326. https://doi.org/10.3390/jcm13051326






