Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Moraissi, E.A.; Ellis, E. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef]
- Chrcanovic, B.R. Surgical versus non-surgical treatment of mandibular condylar fractures: A meta-analysis. J. Oral Maxillofac. Surg. 2015, 44, 158–179. [Google Scholar] [CrossRef]
- Kozakiewicz, M.; Walczyk, A. Current Frequency of Mandibular Condylar Process Fractures. J. Clin. Med. 2023, 12, 1394. [Google Scholar] [CrossRef] [PubMed]
- Durmuş Kocaaslan, N.; Karadede Ünal, B.; Çavuş Özkan, M.; Karadede, B.; Çelebiler, Ö. Comparison of different treatment techniques in the mandibular condyle fracture. Turk. J. Trauma Emerg. Surg. 2022, 28, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Zhou, J.; Li, Z. Contrast analysis of open reduction and internal fixation and non-surgical treatment of condylar fracture: A meta-analysis. J. Craniofac. Surg. 2014, 25, 2077–2080. [Google Scholar] [CrossRef] [PubMed]
- Shiju, M.; Rastogi, S.; Gupta, P.; Kukreja, S.; Thomas, R.; Bhugra, A.K.; Parvatha Reddy, M.; Choudhury, R. Fractures of the mandibular condyle—Open versus closed—A treatment dilemma. J. Craniomaxillofac. Surg. 2015, 43, 448–451. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Neff, A.; Kaur, A.; Falci, S.G.M.; de Souza, G.M.; Ellis, E. Treatment for Adult Mandibular Condylar Process Fractures: A Network Meta-Analysis of Randomized Clinical Trials. J. Oral Maxillofac. Surg. 2023, 81, 1252–1269. [Google Scholar] [CrossRef] [PubMed]
- Karan, A.; Kedarnath, N.S.; Reddy, G.S.; Harish Kumar, T.V.S.; Neelima, C.; Bhavani, M.; Nayyar, A.S. Condylar Fractures: Surgical Versus Conservative Management. Ann. Maxillofac. Surg. 2019, 9, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M. Złamania Wyrostka Kłykciowego Żuchwy; PZWL: Warszawa, Poland, 2019; ISBN 978-83-200-5778-2. [Google Scholar]
- Shakya, S.; Zhang, X.; Liu, L. Key points in surgical management of mandibular condylar fractures. Chin. J. Traumatol. 2020, 23, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.kronosedm.pl/tytan-r56401/ (accessed on 27 October 2023).
- ASTMF 1839-08; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. ASTM International: West Conshohocken, PA, USA, 2016.
- Assari, S.; Darvish, K.; Ilyas, A.M. Biomechanical analysis of second-generation headless compression screws. Injury 2012, 43, 1159–1165. [Google Scholar] [CrossRef]
- Baran, O.; Sagol, E.; Oflaz, H.; Sarikanat, M.; Havitcioglu, H. A biomechanical study on preloaded compression effect on headless screws. Arch. Orthop. Trauma. Surg. 2009, 129, 1601–1605. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, R.; Evans, S.; Kosashvili, Y. Holding power of variable pitch screws in osteoporotic, osteopenic and normal bone: Are all screws created equal? Injury 2010, 41, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.A.; Kuiper, J.H.; Kelly, C.P. Biomechanical Evaluation of a New Composite Bioresorbable Screw. J. Hand Surg. 2006, 31, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Okulski, J.; Krasowski, M.; Konieczny, B.; Zieliński, R. Which of 51 Plate Designs Can Most Stably Fixate the Fragments in a Fracture of the Mandibular Condyle Base? J. Clin. Med. 2023, 12, 4508. [Google Scholar] [CrossRef] [PubMed]
- Mittermiller, P.A.; Bidwell, S.S.; Thieringer, F.M.; Cornelius, C.P.; Trickey, A.W.; Kontio, R.; Girod, S.; AO Trauma Classification Study Group. The Comprehensive AO CMF Classification System for Mandibular Fractures: A Multicenter Validation Study. Craniomaxillofac. Trauma Reconstr. 2019, 12, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Zieliński, R.; Krasowski, M.; Okulski, J. Forces Causing One-Millimeter Displacement of Bone Fragments of Condylar Base Fractures of the Mandible after Fixation by All Available Plate Designs. Materials 2019, 12, 3122. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, R.; Kozakiewicz, M.; Konieczny, B.; Krasowski, M.; Okulski, J. Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible. Materials 2020, 13, 592. [Google Scholar] [CrossRef]
- Goldstein, S. The mechanical properties of trabecular bone: Dependence on anatomic location and function. J. Biomech. 1987, 20, 1055–1061. [Google Scholar] [CrossRef]
- Chapman, J.R.; Harrington, R.M.; Lee, K.M.; Anderson, P.A.; Tencer, A.F.; Kowalski, D. Factors Affecting the Pullout Strength of Cancellous Bone Screws. J. Biomech. Eng. 1996, 118, 391–398. [Google Scholar] [CrossRef]
- Schindeler, A.; Mills, R.J.; Bobyn, J.D.; Little, D.G. Preclinical models for orthopedic research and bone tissue engineering. J. Orthop. Res. 2018, 36, 832–840. [Google Scholar] [CrossRef]
- Cutcliffe, H.C.; DeFrate, L.E. Four-Point Bending Testing for Mechanical Assessment of Mouse Bone Structural Properties. Methods Mol. Biol. 2021, 2230, 199–215. [Google Scholar] [CrossRef]
- Alkan, A.; Metin, M.; Muğlali, M.; Ozden, B.; Celebi, N. Biomechanical comparison of plating techniques for fractures of the mandibular condyle. Br. J. Oral Maxillofac. Surg. 2007, 45, 145–149. [Google Scholar] [CrossRef]
- Pilling, E.; Eckelt, U.; Loukota, R.; Schneider, K.; Stadlinger, B. Comparative evaluation of ten different condylar base fracture osteosynthesis techniques. Br. J. Oral Maxillofac. Surg. 2010, 48, 527–531. [Google Scholar] [CrossRef]
- Kot, C.C.S.; Verstraete, F.J.M.; Garcia, T.C.; Stover, S.M.; Arzi, B. Biomechanical evaluation of locking versus nonlocking 2.0-mm malleable L-miniplate fixation of simulated caudal mandibular fractures in cats. Am. J. Vet Res. 2022, 83, ajvr.22.03.0043. [Google Scholar] [CrossRef]
- Olivera, L.B.; Sant’ Ana, E.; Manzato, A.J.; Guerra, F.L.; Arnett, G.W. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: A study in sheep mandibles. J. Appl. Oral Sci. 2012, 20, 419–426. [Google Scholar] [CrossRef]
- Cheng, C.K.; Wang, X.H.; Luan, Y.C.; Zhang, N.Z.; Liu, B.L.; Ma, X.Y.; Nie, M.D. Challenges of pre-clinical testing in orthopedic implant development. Med. Eng. Phys. 2019, 72, 49–54. [Google Scholar] [CrossRef]
- Marturello, D.M.; Wei, F.; Déjardin, L.M. Characterization of the torsional structural properties of feline femurs and surrogate bone models for mechanical testing of orthopedic implants. Vet Surg. 2019, 48, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Chęciński, M.; Nowak, Z.; Chęcińska, K.; Olszowski, T.; Chlubek, D. The Use of Titanium 3D Mini-Plates in the Surgical Treatment of Fractures of the Mandibular Condyle: A Systematic Review and Meta-Analysis of Clinical Trials. J. Clin. Med. 2021, 10, 3604. [Google Scholar] [CrossRef] [PubMed]
- Agnihotry, A.; Fedorowicz, Z.; Nasser, M.; Gill, K.S. Resorbable versus titanium plates for orthognathic surgery. Cochrane Database Syst. Rev. 2017, 10, CD006204. [Google Scholar] [CrossRef] [PubMed]
- Dorri, M.; Oliver, R. WITHDRAWN: Resorbable versus titanium plates for facial fractures. Cochrane Database Syst. Rev. 2018, 5, CD007158. [Google Scholar] [CrossRef] [PubMed]
- Fuessinger, M.A.; Gass, M.; Woelm, C.; Cornelius, C.P.; Zimmerer, R.M.; Poxleitner, P.; Schlager, S.; Metzger, M.C. Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures. J. Clin. Med. 2021, 10, 5975. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Kawamata, S.; Suzuki, S.; Ishikawa, Y.; Ikeda, Y.; Yasuge, E.; Kogi, S.; Ogawa, A.; Izumisawa, M.; Yamada, H. Condyle Fracture Fixed with Custom-Made Titanium Mesh and a Miniplate: A Case Report. Am. J. Case Rep. 2023, 24, e940681. [Google Scholar] [CrossRef] [PubMed]


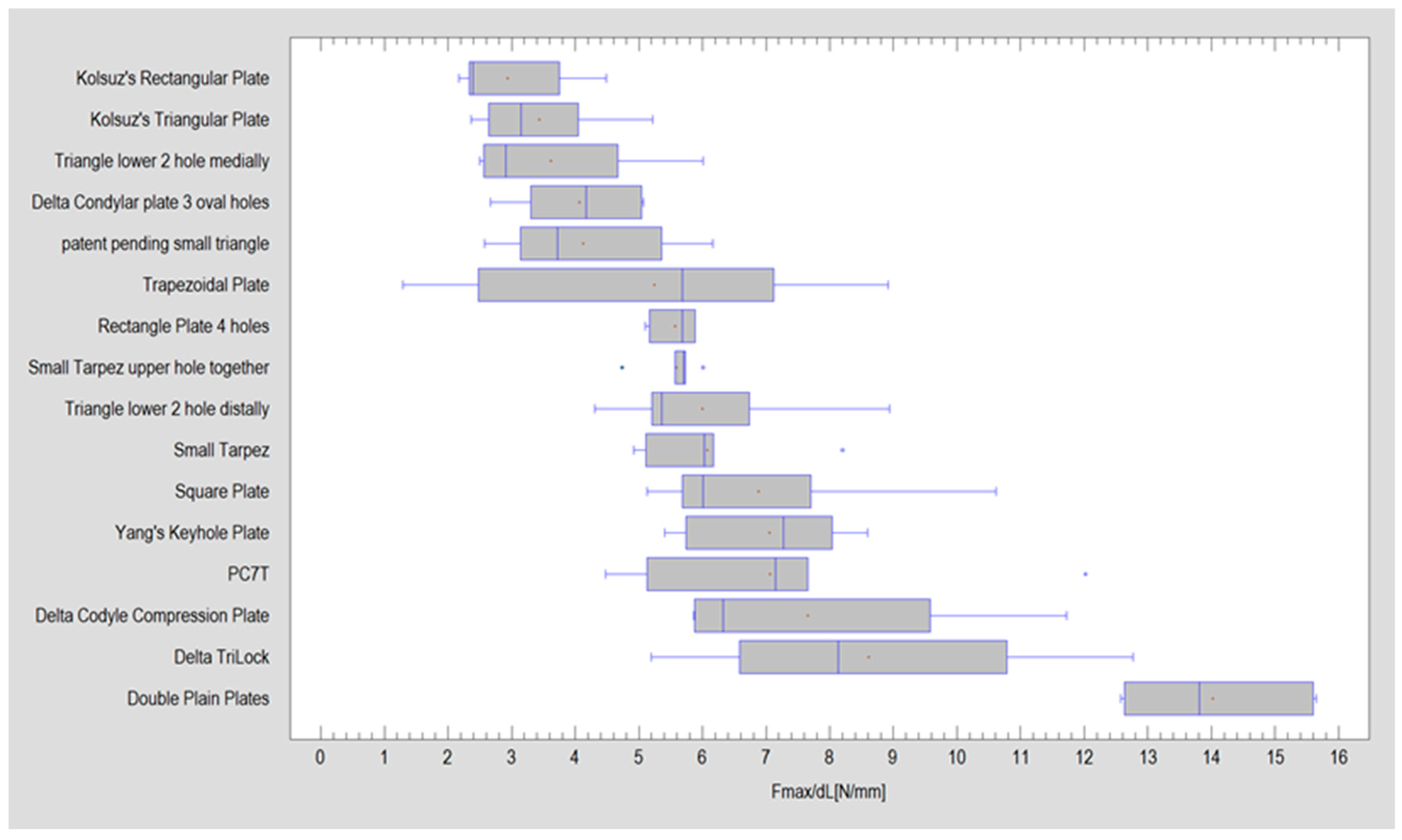
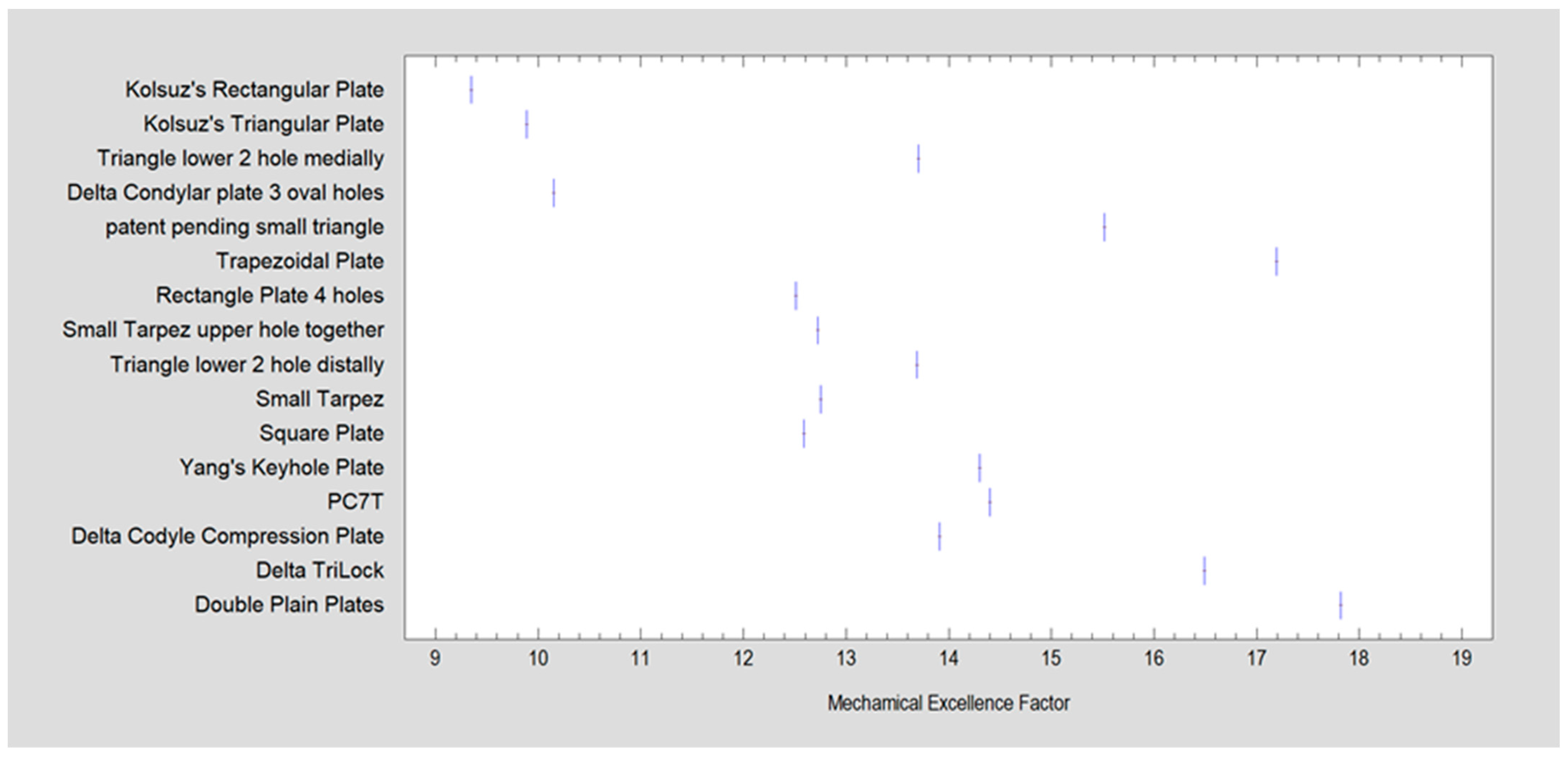
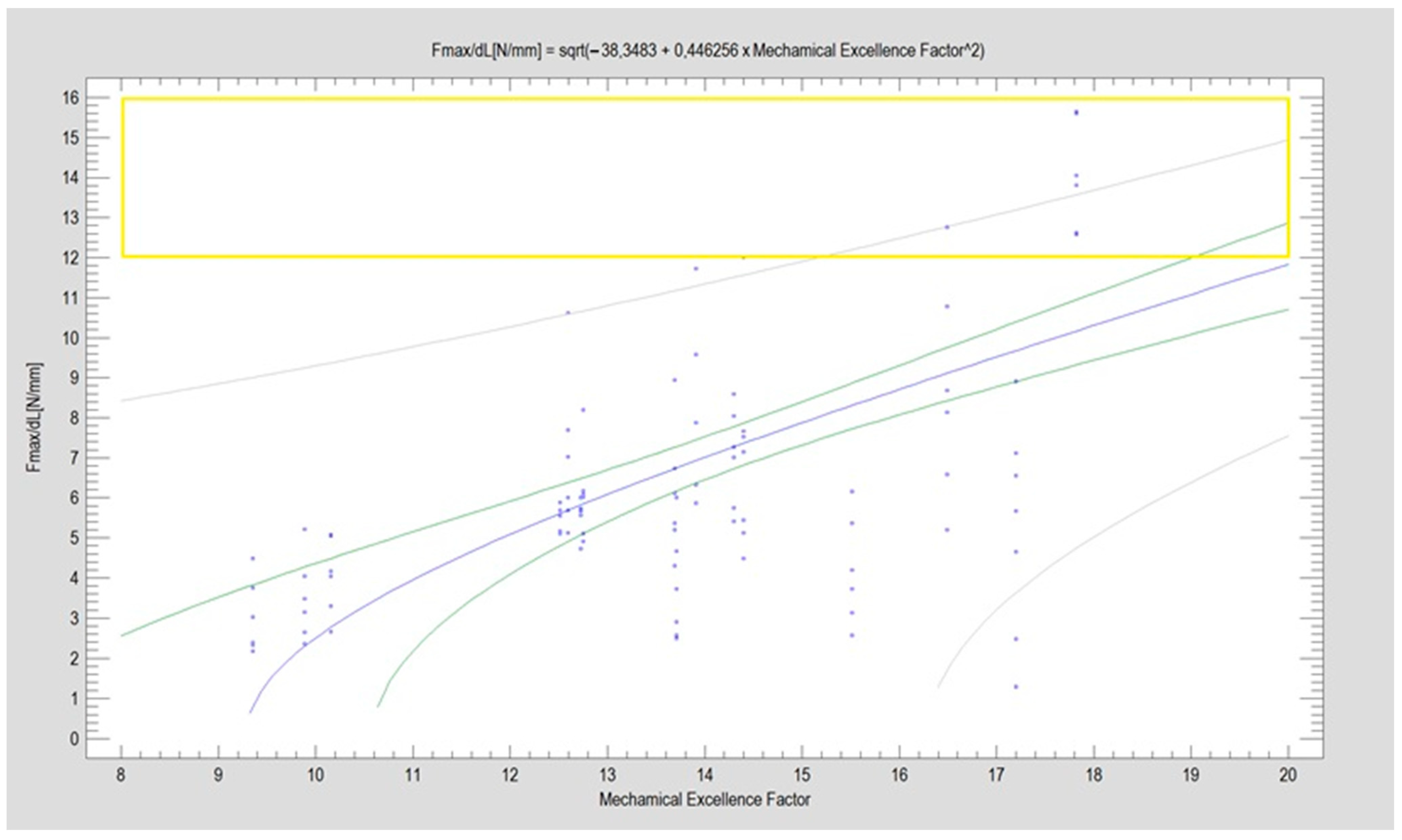
| Name | Design Code | Design | H [mm] | W [mm] | S [mm2] | MEF | Fmax/dL [N/mm] | |
|---|---|---|---|---|---|---|---|---|
| Kolsuz’s rectangular plate | Plate 48 |  | 11.4 | 10.1 | 49 | 67 | 9.4 | 2.94 ± 0.88 |
| Kolsuz’s triangular plate | Plate 47 |  | 14 | 10.4 | 58 | 79 | 9.9 | 3.43 ± 0.96 |
| Triangle lower 2 holes medially | Plate 45 |  | 18.1 | 9.8 | 67 | 90 | 13.7 | 3.61 ± 1.31 |
| Delta condylar plate 3 oval holes | Plate 37 |  | 17 | 11.4 | 64 | 87 | 10.2 | 4.07 ± 0.87 |
| Patent pending small triangle * | Plate 11 |  | 13.5 | 8 | 138 | 151 | 15.5 | 4.12 ± 1.25 |
| Trapezoidal plate | Plate 51 |  | 20 | 18 | 189 | 213 | 17.2 | 5.24 ± 2.66 |
| Rectangular plate 4 holes | Plate 32 |  | 11 | 8.5 | 37 | 55 | 12.5 | 5.57 ± 0.32 |
| Small trapeze upper hole together | Plate 34 |  | 11.1 | 12.1 | 40 | 61 | 12.7 | 5.60 ± 0.40 |
| Triangle lower 2 holes distally | Plate 42 |  | 17.8 | 10 | 67 | 90 | 13.7 | 6.00 ± 1.50 |
| Small trapeze | Plate 33 |  | 11.6 | 11.6 | 41 | 61 | 12.8 | 6.08 ± 1.06 |
| Square plate | Plate 31 |  | 10 | 10 | 39 | 57 | 12.6 | 6.88 ± 1.85 |
| Yang’s keyhole plate | Plate 46 |  | 19.7 | 9.9 | 80 | 106 | 14.3 | 7.05 ± 1.15 |
| PC7T | Plate 49 |  | 15 | 12.8 | 86 | 110 | 14.4 | 7.06 ± 2.52 |
| Delta condyle compression plate * | Plate 14 |  | 15.3 | 8.8 | 179 | 191 | 13.9 | 7.65 ± 2.24 |
| Delta TriLock * | Plate 02 |  | 15.4 | 8.8 | 174 | 187 | 16.5 | 8.61 ± 2.52 |
| Double plain plates * | Plate 20 |  | 16.5 | 3.4 | 227 | 236 | 17.8 | 14.02 ± 1.24 |
| Homogenous Groups 1 | Mean Fmax/dL | Name |
|---|---|---|
| X | 2.94 | Kolsuz’s rectangular plate |
| X | 3.43 | Kolsuz’s triangular plate |
| XX | 3.61 | Triangle lower 2 holes medially |
| XXX | 4.07 | Delta condylar plate 3 oval holes |
| XXX | 4.12 | Patent pending small triangle |
| XXX | 5.24 | Trapezoidal plate |
| XXX | 5.57 | Rectangle plate 4 holes |
| XXX | 5.6 | Small trapeze upper hole together |
| XXX | 6 | Triangle lower 2 holes distally |
| XXX | 6.08 | Small trapeze |
| XXX | 6.88 | Square plate |
| XXX | 7.05 | Yang’s keyhole plate |
| XXX | 7.06 | PC7T |
| XX | 7.65 | Delta condyle compression plate |
| X | 8.61 | Delta TriLock |
| X | 14.02 | Double plain plates |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okulski, J.; Kozakiewicz, M.; Krasowski, M.; Zieliński, R.; Szymor, P. Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options. J. Clin. Med. 2024, 13, 905. https://doi.org/10.3390/jcm13030905
Okulski J, Kozakiewicz M, Krasowski M, Zieliński R, Szymor P. Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options. Journal of Clinical Medicine. 2024; 13(3):905. https://doi.org/10.3390/jcm13030905
Chicago/Turabian StyleOkulski, Jakub, Marcin Kozakiewicz, Michał Krasowski, Rafał Zieliński, and Piotr Szymor. 2024. "Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options" Journal of Clinical Medicine 13, no. 3: 905. https://doi.org/10.3390/jcm13030905






