Kinematic Effects of Derotational Osteotomy of the Humerus in Patients with Internal Shoulder Contracture Secondary to Erb’s Palsy—A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Protocol for Internal Contractures Due to Erb’s Palsy
2.3. Biomechanical Model for Motion-Capture Analysis
2.4. Marker-Setup across Distinct Anatomic Landmarks
2.5. Measurement Procedure for Selected Single Movements and Movement Velocity
2.6. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. Pre- and Post-Operative Global Upper Extremity Kinematics
3.2.1. Persisting OBPP Leads to Kinematic Restrictions of the Entire Upper Limb
3.2.2. Humerus Derotation Osteotomy Addresses Global Upper Extremity Kinematics
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caron, E.; Gienapp, A.J.; Files, H.; Ridley-Pryor, T. Brachial Plexus Birth Injury: A Single-Center Study. Clin. Pediatr. 2023, 62, 99228231163698. [Google Scholar] [CrossRef]
- Lagerkvist, A.-L.; Johansson, U.; Johansson, A.; Bager, B.; Uvebrant, P. Obstetric brachial plexus palsy: A prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev. Med. Child. Neurol. 2010, 52, 529–534. [Google Scholar] [CrossRef]
- Sibinski, M.; Sherlock, D.A.; Hems, T.E.; Sharma, H. Forearm rotational profile in obstetric brachial plexus injury. J. Shoulder Elb. Surg. 2007, 16, 784–787. [Google Scholar] [CrossRef] [PubMed]
- Abid, A. Brachial plexus birth palsy: Management during the first year of life. Orthop. Traumatol. Surg. Res. 2016, 102, S125–S132. [Google Scholar] [CrossRef] [PubMed]
- Hoeksma, A.F.; Ter Steeg, A.M.; Dijkstra, P.; Nelissen, R.G.H.H.; Beelen, A.; de Jong, B.A. Shoulder contracture and osseous deformity in obstetrical brachial plexus injuries. J. Bone Jt. Surg. Am. 2003, 85, 316–322. [Google Scholar] [CrossRef]
- Sheffler, L.C.; Lattanza, L.; Hagar, Y.; Bagley, A.; James, M.A. The prevalence, rate of progression, and treatment of elbow flexion contracture in children with brachial plexus birth palsy. J. Bone Jt. Surg. Am. 2012, 94, 403–409. [Google Scholar] [CrossRef]
- De Joode, S.G.C.J.; Meijer, R.; Samijo, S.; Heymans, M.J.L.F.; Chen, N.; van Rhijn, L.W.; Schotanus, M.G.M. Long-term functional outcome of secondary shoulder surgery in brachial plexus birth palsy patients. Bone Jt. J. 2023, 105-B, 455–464. [Google Scholar] [CrossRef]
- Park, E.; Fox, P.M.; Curtin, C.; Hentz, V.R. Management of Brachial Plexus Birth Palsies: The Stanford Experience. Semin. Plast. Surg. 2023, 37, 085–088. [Google Scholar] [CrossRef]
- Al-Qattan, M.M. Total obstetric brachial plexus palsy in children with internal rotation contracture of the shoulder, flexion contracture of the elbow, and poor hand function: Improving the cosmetic appearance of the limb with rotation osteotomy of the humerus. Ann. Plast. Surg. 2010, 65, 38–42. [Google Scholar] [CrossRef]
- Waters, P.M.; Bae, D.S. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J. Bone Jt. Surg. Am. 2006, 88, 1035–1042. [Google Scholar] [CrossRef]
- Croft, P.; Pope, D.; Boswell, R.; Rigby, A.; Silman, A. Observer variability in measuring elevation and external rotation of the shoulder. Prim. Care Rheumatol. Soc. Shoulder Study Group. Br. J. Rheumatol. 1994, 33, 942–946. [Google Scholar] [CrossRef] [PubMed]
- Pospischill, M.; Kranzl, A.; Attwenger, B.; Knahr, K. Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: A comparative gait analysis. J. Bone Jt. Surg. Am. 2010, 92, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.; Edo, M.; Yokomizo, M.; Togawa, K. Comparative study on gait abnormality in patients with vestibular neuronitis and patients with large acoustic neuroma. Acta Otolaryngol. Suppl. 1995, 519, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Menychtas, D.; Petrou, N.; Kansizoglou, I.; Giannakou, E.; Grekidis, A.; Gasteratos, A.; Gourgoulis, V.; Douda, E.; Smilios, I.; Michalopoulou, M.; et al. Gait analysis comparison between manual marking, 2D pose estimation algorithms, and 3D marker-based system. Front. Rehabil. Sci. 2023, 4, 1238134. [Google Scholar] [CrossRef] [PubMed]
- Rau, G.; Disselhorst-Klug, C.; Schmidt, R. Movement biomechanics goes upwards: From the leg to the arm. J. Biomech. 2000, 33, 1207–1216. [Google Scholar] [CrossRef] [PubMed]
- Rab, G.; Petuskey, K.; Bagley, A. A method for determination of upper extremity kinematics. Gait Posture 2002, 15, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Le Roy, L.; van Bladel, A.; De Mits, S.; Vanden Bossche, L.; Van der Looven, R. Three-Dimensional Upper Limb Movement Analysis in Children and Adolescents With Brachial Plexus Birth Injury: A Systematic Review. Pediatr. Neurol. 2024, 153, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Sohn, W.J.; Sipahi, R.; Sanger, T.D.; Sternad, D. Portable Motion-Analysis Device for Upper-Limb Research, Assessment, and Rehabilitation in Non-Laboratory Settings. IEEE J. Transl. Eng. Health Med. 2019, 7, 2800314. [Google Scholar] [CrossRef]
- Petuskey, K.; Bagley, A.; Abdala, E.; James, M.A.; Rab, G. Upper extremity kinematics during functional activities: Three-dimensional studies in a normal pediatric population. Gait Posture 2007, 25, 573–579. [Google Scholar] [CrossRef]
- Chen, W.; Xiong, C.; Huang, X.; Sun, R.; Xiong, Y. Kinematic analysis and dexterity evaluation of upper extremity in activities of daily living. Gait Posture 2010, 32, 475–481. [Google Scholar] [CrossRef]
- Mosqueda, T.; James, M.A.; Petuskey, K.; Bagley, A.; Abdala, E.; Rab, G. Kinematic assessment of the upper extremity in brachial plexus birth palsy. J. Pediatr. Orthop. 2004, 24, 695–699. [Google Scholar] [CrossRef]
- Alt Murphy, M.; Murphy, S.; Persson, H.C.; Bergström, U.-B.; Sunnerhagen, K.S. Kinematic Analysis Using 3D Motion Capture of Drinking Task in People with and without Upper-extremity Impairments. J. Vis. Exp. 2018, 133, 57228. [Google Scholar] [CrossRef]
- Kim, K.; Song, W.-K.; Lee, J.; Lee, H.-Y.; Park, D.S.; Ko, B.-W.; Kim, J. Kinematic analysis of upper extremity movement during drinking in hemiplegic subjects. Clin. Biomech. 2014, 29, 248–256. [Google Scholar] [CrossRef]
- Van der Helm, F.C.; Pronk, G.M. Three-dimensional recording and description of motions of the shoulder mechanism. J. Biomech. Eng. 1995, 117, 27–40. [Google Scholar] [CrossRef]
- Schmidt, R.; Disselhorst-Klug, C.; Silny, J.; Rau, G. A marker-based measurement procedure for unconstrained wrist and elbow motions. J. Biomech. 1999, 32, 615–621. [Google Scholar] [CrossRef]
- Veeger, H.E.; Yu, B.; An, K.N.; Rozendal, R.H. Parameters for modeling the upper extremity. J. Biomech. 1997, 30, 647–652. [Google Scholar] [CrossRef]
- Wang, W.; Wang, D.; Wesseling, M.; Xue, B.; Li, F. Comparison of modelling and tracking methods for analysing elbow and forearm kinematics. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 1113–1121. [Google Scholar] [CrossRef]
- Wang, J.S.; Petuskey, K.; Bagley, A.M.; James, M.A.; Rab, G. The contralateral unimpaired arm as a control for upper extremity kinematic analysis in children with brachial plexus birth palsy. J. Pediatr. Orthop. 2007, 27, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Simon-Martinez, C.; Dos Santos, G.L.; Jaspers, E.; Vanderschueren, R.; Mailleux, L.; Klingels, K.; Ortibus, E.; Desloovere, K.; Feys, H. Age-related changes in upper limb motion during typical development. PLoS ONE 2018, 13, e0198524. [Google Scholar] [CrossRef] [PubMed]


| Patients | Sex | Age (Years) | Affected Arm | Surgery | Complications |
|---|---|---|---|---|---|
| 1 | M | 9 | Left | 2 | None |
| 2 | F | 10 | Left | 1 | None |
| 3 | F | 8 | Right | 2 | None |
| 4 | F | 9 | Right | 2 | None |
| 5 | F | 8 | Left | 3 | None |
| 6 | F | 8 | Right | 3 | None |
| 7 | M | 13 | Right | 3 | None |
| 8 | M | 7 | Left | 1 | None |
| 9 | F | 10 | Right | 2 | None |
| 10 | M | 5 | Left | 3 | None |
| 11 | M | 10 | Right | 1 | None |
| 12 | F | 8 | Left | 3 | None |
| Median (Range) | 1. Affected Pre-OP | 2. Unaffected Pre-OP | 3. Affected Post-OP | 4. Unaffected Post-OP | p-Value (1 vs. 2) | p-Value (1 vs. 3) | p-Value (3 vs. 4) | p-Value (2 vs. 4) |
|---|---|---|---|---|---|---|---|---|
| Shoulder internal rotation at PAR | 57.6 (−7.1–77.1) | 32.9 (−4.1–45.8) | 9.3 (−24.5–44.9) | 12.31 (−16.2–66.2) | 0.1934 | 0.0186 | 0.1953 | 0.20 |
| Shoulder internal rotation | 84.4 (15.5–116.3) | 84.7 (43.2–117.6) | 9.9 (−17.1–54.1) | 58.8 (7.2–80.4) | 0.5771 | 0.0098 | 0.010 | 0.1289 |
| Shoulder external rotation | 37.2 (−12.0–52.3) | −19.4 (−42.7–35.0) | −20.9 (−53.9–23.6) | −57.5 (−100.6–25.7) | 0.0322 | 0.0068 | 0.01 | 0.0547 |
| Shoulder rotation ROM | 39.0 (17–76) | 86.0 (56–147) | 31.0 (24–75) | 108.0 (54–181) | 0.0010 | 0.6172 | 0.002 | 0.30 |
| Shoulder abduction at PAR | 17.8 (7.5–39.5) | 18.4 (5.8–30.4) | 16.6 (6.9–39.6) | 10.1 (5.4–27.9) | 0.5566 | 0.4316 | 0.99 | 0.20 |
| Shoulder adduction | 16.7 (3.2–26.7) | 10.0 (−2.1–22.1) | 14.4 (5.2–28.3) | 7.4 (0.9–25.6) | 0.1230 | 0.8311 | 0.006 | 0.43 |
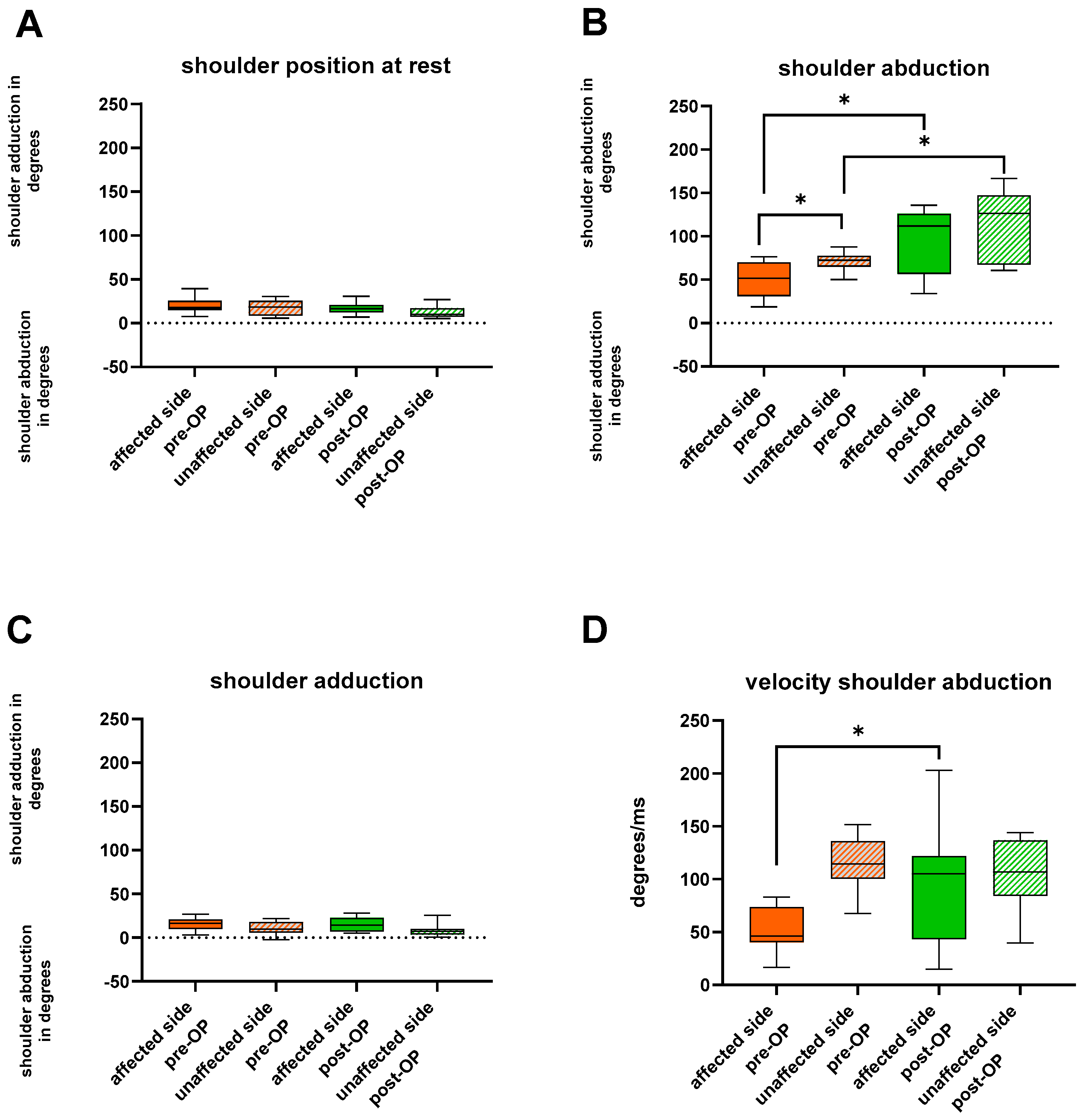
| Shoulder abduction | 51.7 (18.6–76.3) | 72.5 (50.0–87.7) | 111.8 (34.2–135.9) | 126.5 (60.8–166.5) | 0.0244 | 0.0322 | 0.002 | 0.0195 |
| Shoulder abduction velocity (*) | 46.2 (16.7–82.9) | 114.4 (67.4–151.4) | 104.9 (14.8–188.0) | 106.9 (39.4–144.1) | 0.0020 | 0.0273 | 0.16 | 0.8203 |
| Shoulder anteversion | 91.3 (31.9–136.4) | 114.5 (92.4–150.2) | 117.0 (46.3–143.3) | 148.7 (106.6–171.6) | 0.0137 | 0.0645 | 0.004 | 0.02 |
| Shoulder retroversion | 14.5 (−19.7–44.0) | 1.3 (−25.3–51.0) | −3.9 (−44.1–14.9) | −11.0 (−157.1–18.5) | 0.2334 | 0.1230 | 0.76 | 0.15 |
| Elbow at PAR | 31.4 (15.7–43.5) | 10.8 (7.0–43.8) | 39.2 (22.8–77.3) | 34.3 (9.2–53.2) | 0.0420 | 0.0645 | 0.010 | 0.003 |
| Elbow flexion | 122.2 (56.1–132.3) | 138.1 (105.5–147.1) | 137.4 (121.5–158.3) | 150.8 (132.0–161.4) | 0.0244 | 0.0020 | 0.02 | 0.0137 |
| Elbow extension | 17.6 (−53.7–91.6) | −2.1 (−61.0–29.7) | 38.8 (13.9–75.9( | 28.7 (−7.5–47.4) | 0.0322 | 0.1602 | <0.001 | 0.0098 |
| Elbow flexion velocity (*) | 114.9 (55.4–185.4) | 117.2 (66.4–202.6) | 106.9 (66.8–252.3) | 172.5 (108.4–196.6) | 0.91 | 0.8203 | 0.05 | 0.0547 |
| Wrist at PAR | −35.1 (−54.6–53.3) | 0.1 (−16.6–39.0) | 4.3 (−21.9–39.9) | 5.9 (−32.6–39.7) | 0.18 | 0.03 | 0.76 | 0.70 |
| Wrist ROM pro/supination | 37.0 (17.0–89.9) | 74.5 (35.0–114.0) | 69.0 (1.0–144.0) | 144.5 (75.0–165.0) | 0.0024 | 0.0391 | 0.002 | 0.0098 |
| Thoracic abduction at PAR | 1.3 (−8.0–18.7) | −1.6 (−6.9–2.1) | −1.6 (−13.4–5.4) | −3.1 (−37.4–3.0) | 0.3652 | 0.0840 | 0.24 | 0.0840 |
| Thoracic abduction at max. elbow flexion | 3.2 (−18.7–17.0) | 0.1 (−6.4–8.8) | −1.0 (−17.0–12.2) | −2.7 (−33.3–2.6) | 0.8984 | 0.8457 | 0.24 | 0.16 |
| Thoracic flexion at PAR | 5.3 (−74.9–39.4) | 6.4 (−0.1–34.1) | −2.2 (−17.0–9.6) | −0.9 (−15.3–14.6) | 0.2676 | 0.4143 | 0.14 | 0.0681 |
| Thoracic flexion at max. elbow flexion | −9.2 (−54.0–10.6) | 3.4 (−16.8–19.6) | −4.3 (−17.0–12.7) | −2.7 (−15.3–12.7) | 0.0006 | 0.1909 | 0.50 | 0.38 |
| Thoracic rotation at PAR | −1.7 (−18.5–6.2) | −2.5 (−31.0–10.4) | −9.4 (−88.9–86.3) | −3.4 (−89.9–88.2) | 0.9032 | 0.2163 | 0.90 | 0.64 |
| Thoracic rotation at max. elbow flexion | 1.6 (−35.9–27.7) | 0.4 (−16.1–5.1) | −9.7 (−85.6–88.4) | −2.8 (−89.7–88.2) | 0.5016 | 0.3054 | 0.76 | 0.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pignet, A.-L.; Kranzl, A.; Hecker, A.; Weigel, G.; Kamolz, L.-P.; Girsch, W. Kinematic Effects of Derotational Osteotomy of the Humerus in Patients with Internal Shoulder Contracture Secondary to Erb’s Palsy—A Retrospective Cohort Study. J. Clin. Med. 2024, 13, 2759. https://doi.org/10.3390/jcm13102759
Pignet A-L, Kranzl A, Hecker A, Weigel G, Kamolz L-P, Girsch W. Kinematic Effects of Derotational Osteotomy of the Humerus in Patients with Internal Shoulder Contracture Secondary to Erb’s Palsy—A Retrospective Cohort Study. Journal of Clinical Medicine. 2024; 13(10):2759. https://doi.org/10.3390/jcm13102759
Chicago/Turabian StylePignet, Anna-Lisa, Andreas Kranzl, Andrzej Hecker, Gerlinde Weigel, Lars-Peter Kamolz, and Werner Girsch. 2024. "Kinematic Effects of Derotational Osteotomy of the Humerus in Patients with Internal Shoulder Contracture Secondary to Erb’s Palsy—A Retrospective Cohort Study" Journal of Clinical Medicine 13, no. 10: 2759. https://doi.org/10.3390/jcm13102759





