Utilization of Mental Health Provision, Epistemic Stance and Comorbid Psychopathology of Individuals with Complex Post-Traumatic Stress Disorders (CPTSD)—Results from a Representative German Observational Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Adverse Childhood Experiences Questionnaire (ACE)
2.2.2. International Trauma Questionnaire (ITQ)
2.2.3. Psychological Distress, Depression, and Anxiety (BSI-18, PHQ-9, GAD-7)
2.2.4. Work Ability Index (WAI)
2.2.5. Operationalized Psychodynamic Diagnosis Structure Questionnaire—Short Form (OPD-SQS)
2.2.6. Epistemic Trust, Mistrust, and Credulity Questionnaire (ETMCQ)
2.2.7. Mental Health Treatment
2.3. Statistics
3. Results
3.1. Sociodemographic Data
3.2. Clinical Data
3.3. Trauma Characteristics of Participants with CPTSD
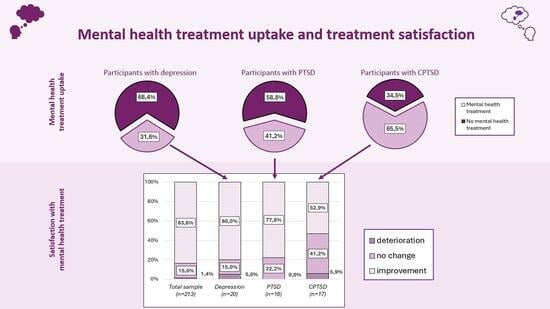
3.4. Mental Health Treatment Uptake
3.5. Comorbidity and Personality Functioning
4. Discussion
Strengths and Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herman, J.L. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. J. Trauma. Stress 1992, 5, 377–391. [Google Scholar] [CrossRef]
- Maercker, A.; Brewin, C.R.; Bryant, R.A.; Cloitre, M.; van Ommeren, M.; Jones, L.M.; Humayan, A.; Kagee, A.; Llosa, A.E.; Rousseau, C.; et al. Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry 2013, 12, 198–206. [Google Scholar] [CrossRef]
- World Health Organization. 6B41 Complex Post Traumatic Stress Disorder. Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559 (accessed on 13 June 2023).
- Maercker, A.; Hecker, T.; Augsburger, M.; Kliem, S. ICD-11 Prevalence Rates of Posttraumatic Stress Disorder and Complex Posttraumatic Stress Disorder in a German Nationwide Sample. J. Nerv. Ment. Dis. 2018, 206, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Karatzias, T.; Shevlin, M.; Fyvie, C.; Hyland, P.; Efthymiadou, E.; Wilson, D.; Roberts, N.; Bisson, J.I.; Brewin, C.R.; Cloitre, M. Evidence of distinct profiles of Posttraumatic Stress Disorder (PTSD) and Complex Posttraumatic Stress Disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). J. Affect. Disord. 2017, 207, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, I.; Gast, U.; Hofmann, A.; Knaevelsrud, C.; Lampe, A.; Liebermann, P.; Lotzin, A.; Maercker, A.; Rosner, R.; Wöllner, W. S3-Leitlinie Posttraumatische Belastungsstörung; Springer Verlag: Berlin, Germany, 2019. [Google Scholar]
- Taubner, S.; Fonagy, P.; Bateman, A. Mentalisierungsbasierte Theraoie; Hogrefe: Göttingen, Germany, 2019; Volume 1. [Google Scholar]
- Bateman, A.; Fonagy, P. Handbook of Mentalizing in Mental Health Practice, 2nd ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2019. [Google Scholar]
- Fonagy, P.; Allison, E. The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy (Chic) 2014, 51, 372–380. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. What we have changed our minds about: Part 2. Borderline personality disorder, epistemic trust and the developmental significance of social communication. Borderline Personal. Disord. Emot. Dysregulation 2017, 4, 9. [Google Scholar] [CrossRef]
- Bateman, A. Mentalization based treatment—Trauma focused (MBT-TF): Rationale of a mentalizing model for treatment of people who have experienced developmental trauma. 2023, in press. [Google Scholar]
- Fonagy, P.; Luyten, P.; Allison, E. Epistemic Petrification and the Restoration of Epistemic Trust: A New Conceptualization of Borderline Personality Disorder and Its Psychosocial Treatment. J. Personal. Disord. 2015, 29, 575–609. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.; Tanzer, M.; Saunders, R.; Booker, T.; Allison, E.; Li, E.; O’Dowda, C.; Luyten, P.; Fonagy, P. Development and validation of a self-report measure of epistemic trust. PLoS ONE 2021, 16, e0250264. [Google Scholar] [CrossRef]
- Karatzias, T.; Hyland, P.; Bradley, A.; Cloitre, M.; Roberts, N.P.; Bisson, J.I.; Shevlin, M. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress. Anxiety 2019, 36, 887–894. [Google Scholar] [CrossRef]
- Karatzias, T.; Shevlin, M.; Hyland, P.; Brewin, C.R.; Cloitre, M.; Bradley, A.; Kitchiner, N.J.; Jumbe, S.; Bisson, J.I.; Roberts, N.P. The role of negative cognitions, emotion regulation strategies, and attachment style in complex post-traumatic stress disorder: Implications for new and existing therapies. Br. J. Clin. Psychol. 2018, 57, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Karatzias, T.; Murphy, P.; Cloitre, M.; Bisson, J.; Roberts, N.; Shevlin, M.; Hyland, P.; Maercker, A.; Ben-Ezra, M.; Coventry, P.; et al. Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychol. Med. 2019, 49, 1761–1775. [Google Scholar] [CrossRef] [PubMed]
- Lampe, A.; Riedl, D.; Kampling, H.; Nolte, T.; Kirchhoff, C.; Grote, V.; Fischer, M.J.; Kruse, J. Improvements of complex post-traumatic stress disorder symptoms during a multimodal psychodynamic inpatient rehabilitation treatment—Results of an observational single-centre pilot study. Eur. J. Psychotraumatology 2024, 15, 2333221. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Wingenfeld, K.; Schäfer, I.; Terfehr, K.; Grabski, H.; Driessen, M.; Grabe, H.; Löwe, B.; Spitzer, C. Reliable, valide und ökonomische Erfassung früher Traumatisierung: Erste psychometrische Charakterisierung der deutschen Version des Adverse Childhood Experiences Questionnaire (ACE). Psychother. Psychosom. Med. Psychol. 2011, 61, e10–e14. [Google Scholar] [CrossRef] [PubMed]
- Witt, A.; Sachser, C.; Plener, P.L.; Brähler, E.; Fegert, J.M. The Prevalence and Consequences of Adverse Childhood Experiences in the German Population. Dtsch. Arztebl. Int. 2019, 116, 635–642. [Google Scholar] [CrossRef]
- Cloitre, M.; Shevlin, M.; Brewin, C.R.; Bisson, J.I.; Roberts, N.P.; Maercker, A.; Karatzias, T.; Hyland, P. The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr. Scand. 2018, 138, 536–546. [Google Scholar] [CrossRef]
- Christen, D.; Killikelly, C.; Maercker, A.; Augsburger, M. Item Response Model Validation of the German ICD-11 International Trauma Questionnaire for PTSD and CPTSD. Clin. Psychol. Eur. 2021, 3, e5501. [Google Scholar] [CrossRef]
- Maercker, A.; Cloitre, M.; Bachem, R.; Schlumpf, Y.R.; Khoury, B.; Hitchcock, C.; Bohus, M. Complex post-traumatic stress disorder. Lancet 2022, 400, 60–72. [Google Scholar] [CrossRef]
- Seiler, N.; Davoodi, K.; Keem, M.; Das, S. Assessment tools for complex post traumatic stress disorder: A systematic review. Int. J. Psychiatry Clin. Pract. 2023, 27, 292–300. [Google Scholar] [CrossRef]
- Karatzias, T.; Cloitre, M.; Maercker, A.; Kazlauskas, E.; Shevlin, M.; Hyland, P.; Bisson, J.I.; Roberts, N.P.; Brewin, C.R. PTSD and Complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. Eur. J. Psychotraumatology 2017, 8, 1418103. [Google Scholar] [CrossRef] [PubMed]
- Franke, G.H. Mini-Symptom-Checklist (BSI-18). Manual; Hogrefe: Göttingen, Germany, 2017. [Google Scholar]
- Franke, G.H.; Jaeger, S.; Glaesmer, H.; Barkmann, C.; Petrowski, K.; Braehler, E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Med. Res. Methodol. 2017, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Spitzer, R.L.; Zipfel, S.; Herzog, W. Health-Questionnaire for Patients (PHQ-D). Complete Version and Short Form—Manual; Pfizer: Karlsruhe, Germany, 2002; Volume 2. [Google Scholar]
- Mitchell, A.J.; Yadegarfar, M.; Gill, J.; Stubbs, B. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: A diagnostic meta-analysis of 40 studies. BJPsych Open 2016, 2, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Rief, W.; Klaiberg, A.; Braehler, E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2006, 28, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Hinz, A.; Klein, A.M.; Brähler, E.; Glaesmer, H.; Luck, T.; Riedel-Heller, S.G.; Wirkner, K.; Hilbert, A. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J. Affect. Disord. 2017, 210, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and Standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the General Population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Hasselhorn, H.M.; Freude, G. The Work Ability Index—A guideline; Wirtschaftsverl NW Verl für neue Wiss: Bremerhaven, Germany, 2007. [Google Scholar]
- Ehrenthal, J.C.; Dinger, U.; Schauenburg, H.; Horsch, L.; Dahlbender, R.W.; Gierk, B. [Development of a 12-item version of the OPD-Structure Questionnaire (OPD-SQS)]. Z Psychosom. Med. Psychother. 2015, 61, 262–274. [Google Scholar] [CrossRef] [PubMed]
- Ehrenthal, J.C.; Kruse, J.; Schmalbach, B.; Dinger, U.; Werner, S.; Schauenburg, H.; Brähler, E.; Kampling, H. Measuring personality functioning with the 12-item version of the OPD-Structure Questionnaire (OPD-SQS): Reliability, factor structure, validity, and measurement invariance in the general population. Front. Psychol. 2023, 14, 1248992. [Google Scholar] [CrossRef]
- Nolte, T.; Schwarzer, N.; Riedl, D.; Lashani, E.; Kamplig, H.; Lampe, A.; Kruse, J.; Campbell, C.; Montague, P.R.; Fonagy, P.; et al. Validation of the German version of the Epistemic Trust, Mistrust and Credulity Questionnaire (ETMCQ). 2023. in preparation. [Google Scholar]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2010. [Google Scholar]
- Zhang, L.; Pan, R.; Cai, Y.; Pan, J. The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis. Psychiatry Investig. 2021, 18, 426–433. [Google Scholar] [CrossRef]
- Grubaugh, A.L.; Zinzow, H.M.; Paul, L.; Egede, L.E.; Frueh, B.C. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: A critical review. Clin. Psychol. Rev. 2011, 31, 883–899. [Google Scholar] [CrossRef]
- Mauritz, M.W.; Goossens, P.J.J.; Draijer, N.; van Achterberg, T. Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness. Eur. J. Psychotraumatology 2013, 4, 19985. [Google Scholar] [CrossRef] [PubMed]
- Riedl, D.; Rothmund, M.S.; Grote, V.; Fischer, M.J.; Kampling, H.; Kruse, J.; Nolte, T.; Labek, K.; Lampe, A. Mentalizing and epistemic trust as critical success factors in psychosomatic rehabilitation: Results of a single center longitudinal observational study. Front. Psychiatry 2023, 14, 1150422. [Google Scholar] [CrossRef]
- Riedl, D.; Kampling, H.; Kruse, J.; Nolte, T.; Labek, K.; Kirchhoff, C.; Grote, V.; Fischer, M.J.; Lampe, A. Epistemic trust is a critical success factor in psychosomatic rehabilitation—Results from a naturalistic multi-center observational study. Psychol. Psychother. Theory Res. Pract. 2023. under review. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. Mentalizing, Epistemic Trust and the Phenomenology of Psychotherapy. Psychopathology 2019, 52, 94–103. [Google Scholar] [CrossRef]
- Li, E.T.; Midgley, N.; Luyten, P.; Sprecher, E.A.; Campbell, C. Mapping the journey from epistemic mistrust in depressed adolescents receiving psychotherapy. J. Couns. Psychol. 2022, 69, 678–690. [Google Scholar] [CrossRef]
- Bateman, A.; Campbell, C.; Luyten, P.; Fonagy, P. A mentalization-based approach to common factors in the treatment of borderline personality disorder. Curr. Opin. Psychol. 2018, 21, 44–49. [Google Scholar] [CrossRef]
- Riffer, F.; Knopp, M.; Burghardt, J.; Sprung, M. Geschlechtsspezifische Unterschiede in der psychotherapeutischen Versorgung. Psychotherapeut 2021, 66, 511–517. [Google Scholar] [CrossRef]
- Riffer, F.; Knopp, M.; Oppenauer, C.; Sprung, M. Psychotherapeutische Versorgung in Österreich: Kassenfinanzierte Psychotherapie für Menschen mit chronisch psychischen Erkrankungen im Jahresvergleich 2017 bis 2020. Psychother. Forum 2022, 26, 10–17. [Google Scholar] [CrossRef]
- Brenner, L.; Köllner, V.; Bachem, R. Symptom burden and work-related impairment among patients with PTSD and complex PTSD. Eur. J. Psychotraumatology 2019, 10, 1694766. [Google Scholar] [CrossRef] [PubMed]
- Puschner, B.; Bauer, S.; Kraft, S.; Kordy, H. Zufriedenheit von Patienten und Therapeuten mit ambulanter Psychotherapie. Psychother. Psychosom. Med. Psychol. 2005, 55, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Riedl, D.; Labek, K.; Gstrein, I.; Rothmund, M.S.; Sperner-Unterweger, B.; Kantner-Rumplmair, W. Large improvement of mental health during in outpatient short-term group psychotherapy treatment-a naturalistic pre-/post-observational study. Neuropsychiatr 2022, 37, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Cloitre, M.; Henn-Haase, C.; Herman, J.L.; Jackson, C.; Kaslow, N.; Klein, C.; Mendelsohn, M.; Petkova, E. A multi-site single-blind clinical study to compare the effects of STAIR Narrative Therapy to treatment as usual among women with PTSD in public sector mental health settings: Study protocol for a randomized controlled trial. Trials 2014, 15, 197. [Google Scholar] [CrossRef]
- Wöller, W.; Lampe, A.; Schellong, J.; Leichsenring, F.; Kruse, J.; Mattheß, H. [Psychodynamic Treatment for Complex Posttraumatic Stress Disorder]; Klett-Cotta: Stuttgart, Germany, 2020. [Google Scholar]
- Wöller, W.; Leichsenring, F.; Leweke, F.; Kruse, J. Psychodynamic psychotherapy for posttraumatic stress disorder related to childhood abuse--Principles for a treatment manual. Bull. Menn. Clin. 2012, 76, 69–93. [Google Scholar] [CrossRef]



| Total Sample (n = 1918) | Participants with Depression (n = 79) | Participants with PTSD (n = 51) | Participants with CPTSD (n = 29) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | χ2 | p-Value | |
| Gender | 2.369 | 0.67 | ||||||||
| male | 905 | 47.2% | 33 | 41.8% | 19 | 37.3% | 11 | 37.9% | ||
| female | 1010 | 52.7% | 46 | 58.2% | 31 | 60.8% | 18 | 62.1% | ||
| diverse | 3 | 0.2% | 0 | 0.0% | 1 | 2.0% | 0 | 0.0% | ||
| Age | 28.805 | 0.001 | ||||||||
| <30 years | 303 | 15.8% | 9 | 11.4% | 12 | 23.5% | 5 | 17.2% | ||
| 30–39 years | 239 | 12.5% | 5 | 6.3% | 9 | 17.6% | 10 | 34.5% | ||
| 40–49 years | 290 | 15.1% | 10 | 12.7% | 3 | 5.9% | 4 | 13.8% | ||
| 50–59 years | 405 | 21.1% | 14 | 17.7% | 9 | 17.6% | 6 | 20.7% | ||
| 60–60 years | 335 | 17.5% | 14 | 17.7% | 11 | 21.6% | 3 | 10.3% | ||
| >70 years | 346 | 18.0% | 27 | 34.2% | 7 | 13.7% | 1 | 3.4% | ||
| Marital Status | 7.929 | 0.44 | ||||||||
| married | 880 | 45.9% | 27 | 34.2% | 23 | 45.1% | 13 | 44.8% | ||
| single | 545 | 28.4% | 24 | 30.4% | 17 | 33.3% | 11 | 37.9% | ||
| divorced | 275 | 14.3% | 14 | 17.7% | 5 | 9.8% | 3 | 10.3% | ||
| widowed | 211 | 11.0% | 14 | 17.7% | 5 | 9.8% | 2 | 6.9% | ||
| missing | 7 | 0.4% | 0 | 0.0% | 1 | 2.0% | 0 | 0.0% | ||
| Living with partner | 6.677 | 0.15 | ||||||||
| living with partner | 1101 | 57.4% | 34 | 43.0% | 27 | 52.9% | 16 | 55.2% | ||
| not living with partner | 786 | 41.0% | 45 | 57.0% | 24 | 47.1% | 12 | 41.4% | ||
| Missing | 31 | 1.6% | 0 | 0.0% | 0 | 0.0% | 1 | 3.4% | ||
| Migration background | 1.837 | 0.40 | ||||||||
| No | 1539 | 87.3% | 67 | 84.8% | 46 | 90.2% | 23 | 79.3% | ||
| Yes | 220 | 12.7% | 12 | 15.2% | 5 | 9.8% | 6 | 20.7% | ||
| Monthly family net household income | 17.001 | 0.030 | ||||||||
| EUR < 1500 | 405 | 21.1% | 33 | 41.8% | 10 | 19.6% | 7 | 24.1% | ||
| EUR 1500–2500 | 611 | 31.9% | 28 | 35.4% | 14 | 27.5% | 10 | 34.5% | ||
| EUR 2500–3500 | 437 | 22.8% | 6 | 7.6% | 14 | 27.5% | 7 | 24.1% | ||
| EUR > 3500 | 420 | 21.9% | 10 | 12.7% | 11 | 21.6% | 5 | 17.2% | ||
| missing | 45 | 2.3% | 2 | 2.5% | 2 | 3.9% | 0 | 0.0% | ||
| Highest level of education | 8.582 | 0.38 | ||||||||
| school not finished/still in school | 77 | 4.0% | 5 | 6.3% | 3 | 5.9% | 2 | 6.9% | ||
| compulsory school | 539 | 28.1% | 33 | 41.8% | 12 | 23.5% | 10 | 34.5% | ||
| higher education | 1097 | 57.2% | 35 | 44.3% | 30 | 58.8% | 17 | 58.6% | ||
| university degree | 189 | 9.9% | 4 | 5.1% | 5 | 9.8% | 0 | 0.0% | ||
| missing | 16 | 0.8% | 2 | 2.5% | 1 | 2.0% | 0 | 0.0% | ||
| Employment | 30.430 | 0.002 | ||||||||
| full-time employment | 796 | 41.5% | 14 | 17.7% | 21 | 41.2% | 11 | 37.9% | ||
| part-time employment | 238 | 12.4% | 7 | 8.9% | 9 | 17.6% | 3 | 10.3% | ||
| unemployed | 155 | 8.1% | 15 | 19.0% | 3 | 5.9% | 9 | 31.0% | ||
| in training | 102 | 5.3% | 4 | 5.1% | 4 | 7.8% | 2 | 6.9% | ||
| retired | 604 | 31.5% | 38 | 48.1% | 13 | 25.5% | 3 | 10.3% | ||
| missing | 23 | 1.2% | 1 | 1.3% | 1 | 2.0% | 1 | 3.4% | ||
| ETMCQ Total | ETMCQ Trust | ETMCQ Mistrust | ETMCQ Credulity | |
|---|---|---|---|---|
| Re-experiencing | −0.10 *** | 0.01 | 0.07 ** | 0.17 *** |
| Avoidance | −0.13 *** | 0.01 | 0.09 *** | 0.19 *** |
| Persistent perception of heightened current threat | −0.23 *** | −0.09 *** | 0.18 *** | 0.24 *** |
| Functional impairment (PTSD) | −0.20 *** | −0.07 ** | 0.17 *** | 0.21 *** |
| Affective dysregulation | −0.35 *** | −0.15 *** | 0.30 *** | 0.33 *** |
| Negative self-concept | −0.33 *** | −0.16 *** | 0.24 *** | 0.35 *** |
| Problematic relationships | −0.35 *** | −0.15 *** | 0.28 *** | 0.35 *** |
| Functional impairment (DSO) | −0.30 *** | −0.11 *** | 0.25 *** | 0.31 *** |
| Total Sample (n = 1918) | CPTSD (n = 29) | PTSD (n = 51) | Depression (n = 79) | |||||||
| n | % | n | % | n | % | n | % | χ2 | p-Value | |
| Mental health treatment 1 | 252 | 13.1% | 19 | 65.5% | 21 | 41.2% | 25 | 31.6% | 138.943 | <0.001 |
| Psychotherapy 2 | 218 | 11.4% | 17 | 58.6% | 18 | 35.3% | 21 | 26.6% | 123.590 | <0.001 |
| Missing | 52 | 2.7% | 1 | 3.4% | 1 | 2.0% | 2 | 2.5% | ||
| Total Sample (n = 252) | CPTSD (n = 19) | PTSD (n = 21) | Depression (n = 25) | χ2 | p-value | |||||
| If yes, which type of therapy? | ||||||||||
| Outpatient psychotherapy | 184 | 73.0% | 15 | 88.2% | 17 | 81.0% | 15 | 78.9% | 1.592 | 0.66 |
| missing | 39 | 15.5% | 2 | 10.5% | 3 | 14.3% | 4 | 16.0% | ||
| Psychosomatic inpatient treatment | 56 | 22.2% | 7 | 36.8% | 5 | 23.8% | 12 | 48.0% | 3.949 | 0.27 |
| missing | 56 | 22.2% | 2 | 10.5% | 7 | 33.3% | 5 | 20.0% | ||
| Psychiatric inpatient treatment | 51 | 20.2% | 8 | 47.4% | 4 | 19.0% | 7 | 28.0% | 8.908 | 0.031 |
| missing | 56 | 22.2% | 2 | 10.5% | 7 | 33.3% | 5 | 20.0% | ||
| Psychotherapy outpatient clinic | 45 | 19.6% | 8 | 44.4% | 4 | 23.5% | 5 | 21.7% | 8.134 | 0.043 |
| missing | 35 | 15.2% | 2 | 11.1% | 3 | 17.6% | 4 | 17.4% | ||
| Group A: CPTSD (n = 29) | Group B: PTSD (n = 51) | Group C: Depression (n = 79) | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | p-Value | η2 | |
| ACE | 3.7 | 2.7 | 2.0 | 2.5 | 2.8 | 2.8 | 0.043 a | 0.04 |
| BSI-18 | ||||||||
| Depression | 11.3 | 6.5 | 5.9 | 5.2 | 10.3 | 3.8 | <0.001 a,c | 0.14 |
| Anxiety | 8.7 | 5.3 | 4.5 | 4.7 | 6.3 | 3.9 | <0.001 a,b | 0.09 |
| Somatization | 6.5 | 5.6 | 4.2 | 4.0 | 6.1 | 4.5 | 0.031 a | 0.05 |
| PHQ-9 total score | 14.7 | 6.8 | 8.2 | 5.0 | 11.9 | 3.8 | <0.001 a,b,c | 0.18 |
| GAD-7 total score | 11.8 | 5.2 | 7.6 | 4.7 | 8.7 | 3.5 | <0.001 a,b | 0.10 |
| WAI | 5.2 | 2.7 | 5.6 | 2.5 | 4.0 | 2.5 | 0.43 | 0.01 |
| OPD-SQS | ||||||||
| total score | 41.6 | 8.0 | 32.3 | 9.4 | 36.5 | 8.8 | <0.001 a,c | 0.11 |
| self-perception | 12.9 | 3.4 | 10.0 | 3.9 | 10.7 | 4.0 | 0.005 a | 0.07 |
| interpersonal contact | 13.6 | 3.0 | 9.8 | 3.4 | 12.2 | 3.2 | <0.001 a,c | 0.14 |
| relationship model | 15.1 | 3.3 | 12.5 | 3.9 | 13.6 | 3.5 | 0.040 a | 0.04 |
| ETMCQ | ||||||||
| Trust | 21.5 | 5.9 | 23.9 | 4.8 | 22.2 | 6.0 | 0.16 | 0.02 |
| Mistrust | 23.8 | 5.1 | 20.4 | 5.2 | 20.8 | 5.7 | 0.043 a | 0.04 |
| Credulity | 22.5 | 4.8 | 18.8 | 4.8 | 19.3 | 5.6 | 0.018 a | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riedl, D.; Kampling, H.; Nolte, T.; Kirchhoff, C.; Kruse, J.; Sachser, C.; Fegert, J.M.; Gündel, H.; Brähler, E.; Grote, V.; et al. Utilization of Mental Health Provision, Epistemic Stance and Comorbid Psychopathology of Individuals with Complex Post-Traumatic Stress Disorders (CPTSD)—Results from a Representative German Observational Study. J. Clin. Med. 2024, 13, 2735. https://doi.org/10.3390/jcm13102735
Riedl D, Kampling H, Nolte T, Kirchhoff C, Kruse J, Sachser C, Fegert JM, Gündel H, Brähler E, Grote V, et al. Utilization of Mental Health Provision, Epistemic Stance and Comorbid Psychopathology of Individuals with Complex Post-Traumatic Stress Disorders (CPTSD)—Results from a Representative German Observational Study. Journal of Clinical Medicine. 2024; 13(10):2735. https://doi.org/10.3390/jcm13102735
Chicago/Turabian StyleRiedl, David, Hanna Kampling, Tobias Nolte, Christina Kirchhoff, Johannes Kruse, Cedric Sachser, Jörg M. Fegert, Harald Gündel, Elmar Brähler, Vincent Grote, and et al. 2024. "Utilization of Mental Health Provision, Epistemic Stance and Comorbid Psychopathology of Individuals with Complex Post-Traumatic Stress Disorders (CPTSD)—Results from a Representative German Observational Study" Journal of Clinical Medicine 13, no. 10: 2735. https://doi.org/10.3390/jcm13102735