1. Introduction
The sodium-glucose co-transporter 2 inhibitors (SGLT2i) are new effective anti-diabetic drugs, which act by inhibiting glucose and sodium reabsorption at the level of proximal convoluted tubule of the nephron, and improving glycemic control in patients with type 2 diabetes mellitus (T2DM) [
1]. Currently, four SGLT2i are approved by the European Medicines Agency and the Food and Drug Administration and available to prescribe: canagliflozin, dapagliflozin, empagliflozin and ertugliflozin [
1].
Two features of SGLT2i are of particular interest: (i) a mechanism of action not linked to insulin secretion, which makes the detrimental occurrence of hypoglycemia less likely compared to other anti-diabetic drug classes; and (ii) cardiovascular and renal protective effects independent of its’ glycemic control and noted early after initiation of the therapy, suggesting mechanisms of action beyond blood glucose lowering [
1,
2].
Three randomized clinical trials, the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME) [
3], CANagliflozin cardioVascular Assessment Study (CANVAS) [
4], and Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE-TIMI 58) trial [
5], have reported that SGLT2i improved cardiovascular outcomes in patients with T2DM, including a reduced risk of cardiovascular death and hospitalization for heart failure. In expanding the applicability of SGLT2i therapy, the ‘EMPagliflozin outcomE tRial in patients with chrOnic heaRt failure (EMPEROR-reduced)’ investigated 3730 patients with reduced ejection fraction (<40%) of whom 49% had T2DM, and showed a reduction of the combined primary endpoints (cardiovascular death and heart failure hospitalization) in the empagliflozin group compared to placebo (19.4% vs. 24.7% respectively; hazard ratio (HR) 0.76, 95% confidence interval (CI) 0.67–0.87;
p < 0.0001). The ‘Empagliflozin Outcome Trial in Patients with Chronic Heart Failure with Preserved Ejection Fraction (EMPEROR-Preserved)’ showed that empagliflozin was superior to placebo in improving heart failure outcomes (cardiovascular death and hospitalization) among patients with symptomatic stable heart failure and preserved ejection fraction (>40%), irrespective of diabetes status (HR 0.79, 95% CI 0.69–0.90,
p < 0.001).
The Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial [
6] testing the efficacy of SGLT2i in patients with T2DM and evidence of albuminuric chronic kidney disease showed a reduction in the risk of progression toward end-stage renal failure (HR 0.68, 95% CI 0.54–0.86;
p = 0.002). A sub-analysis of the CREDENCE trial suggested that there may be a potential effect of SGLT2i on ischaemic stroke prevention and reduction in non-traumatic brain haemorrhages [
7]. More recently, a sub-analysis of the DECLARE-TIMI 58 trial found a decrease in new episodes of atrial fibrillation (AF) or atrial flutter (AFl) with SGLT2i independent from the prior history of AF, atherosclerotic cardiovascular disease or heart failure [
8].
Together these data lead to the hypothesis that SGLT2i may be beneficial in patients with AF which are at risk of developing incident comorbidities including heart failure and dementia. This is further supported by the anti-inflammatory, metabolic and neuro-modulatory actions of this class of medications [
2]. Nonetheless, there is limited evidence from large-scale datasets on whether these trial data translate into real-world clinical practice.
Therefore, in this study we investigated the effect of SGLT2i therapy in reducing the occurrence and risk of adverse cerebrovascular cardiovascular, and cognitive outcomes using a cohort of patients with AF and T2DM.
2. Materials and Methods
This is an observational and retrospective study using TriNetX, a global federated health research network with real-time updates of anonymised electronic medical records (EMRs). The network includes healthcare organisations (HCOs, academic medical centres, specialty physician practices and community hospitals) with data for >85 million real-world patients, predominately based in the United States. In brief, the TriNetX research network database encompasses anonymized EMRs of patients registered with the network and has information on patient demographics, clinical details including diagnoses (using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes), medications and investigations as well as any procedures, from settings such as general practice surgeries, community and secondary hospitals. To comply with legal frameworks and ethical guidelines guarding against data re-identification, the identity of participating HCOs and their individual contribution to each dataset are not disclosed. As a federated research network, studies using the TriNetX health research network do not require ethical approval as no patient is identifiable.
For the present study, the TriNetX research network was searched for the inclusion of patients from 1 January 2018 to 31 December 2019. To be included in the study, all patients were aged ≥18 years with a diagnosis of AF (ICD-10-CM code: I48) and diabetes mellitus (ICD-10-CM code: E08-E13) during this period, and received oral anticoagulation therapy either with a vitamin K antagonist (VKA) or a non-VKA oral anticoagulant (NOAC). Patients were divided into two groups according to SGLT2i use (empagliflozin, dapagliflozin, or canagliflozin). In the group of patients on SGLT2i, only prevalent SGLT2i users were considered. Patients not receiving SGLT2i at inclusion, who were subsequently prescribed it, were censored when the drug was initiated. Patients with chronic rheumatic heart diseases (ICD-10-CM code I05-I09), acute rheumatic fever (ICD-10-CM code I00–I02) or prosthetic heart valves (ICD-10-CM code Z95.2) were excluded, with no other exclusion criteria.
We collected data on baseline demographics, ethnicity, comorbidities (e.g., hypertension, coronary artery disease, heart failure, cerebrovascular disease, peripheral vascular disease, hyperlipidemia, overweight/obesity, chronic obstructive pulmonary disease (COPD), renal impairment, diseases of the nervous system, diseases of liver and cancer), and medication use (e.g., anticoagulants, antiplatelets, beta-blockers, calcium channel blockers, antiarrhythmics, angiotensin-converting enzyme inhibitors, angiotensin II inhibitors, antilipemic agents, diuretics, and blood glucose regulation agents).
We used ICD-10-CM codes to identify relevant diagnoses and the Anatomic Therapeutic Chemical (ATC) codes to identify pharmacotherapy. The searches were run in TriNetX on 3 May 2022. At the time of the search, there were 58 participating HCOs within the TriNetX research network.
2.1. Follow-Up and Clinical Outcomes
All patients were followed-up for three years. The primary endpoints were ischaemic stroke/transient ischemic attack (TIA) (ICD-10-CM codes: G45 or I63), intracranial haemorrhage (ICH, ICD-10-CM codes: I60, I61 or I62), and incident dementia (either vascular dementia, Alzheimer’s disease or unspecified dementia, i.e., ICD-10-CM codes: F01, F02, F03 or G30). Secondary end-points were incident heart failure (ICD-10-CM code: I50) and all-cause mortality. We used ICD-10-CM codes to identify the primary and secondary endpoints reported in the EMRs through the TriNetX platform.
2.2. Statistical Analysis
Continuous variables (age) were expressed as mean and standard deviation (SD), and tested for differences with independent-sample
t test. Categorical variables (sex, ethnicity, comorbidities, and pharmacological therapy) were expressed as absolute frequencies and percentages, and tested for differences with chi-squared test. The TriNetX platform was used to run 1:1 propensity score matching (PSM) using logistic regression. The platform uses ‘greedy nearest-neighbour matching’ with a caliper of 0.1 pooled standard deviations and difference between propensity scores ≤0.1. Covariate balance between groups was assessed using standardised mean differences (SMDs). Any baseline characteristic with a SMD between cohorts <0.1 is considered well-matched [
9].
HR and 95% CI were calculated following PSM, and displayed as Kaplan-Meier survival curves with log-rank tests. No imputations were made for missing data. Two-sided p-values < 0.05 were accepted as statistically significant. Statistical analysis was performed using the TriNetX Analytics function in the online research platform.
3. Results
The study identified 89,356 patients with AF and T2DM, and of these, 5061 (5.7%) patients were taking a SGLT2i.
Table 1 summarises the baseline characteristics of patients with and without SGLT2i therapy. Prior to PSM, patients receiving SGLT2i were likely be male, not Hispanic or Latino, and suffered from ischemic heart disease, hyperlipidemia, and overweight/obesity. On the contrary, patients on SGLT2i presented lower prevalence of cerebrovascular disease, COPD, and renal disease, and were more frequently treated with NOACs instead of VKAs. These differences were attenuated after PSM and both cohorts, each including 5049 patients, were balanced.
3.1. Cerebrovascular Events and Incident Dementia According to SGLT2i Therapy
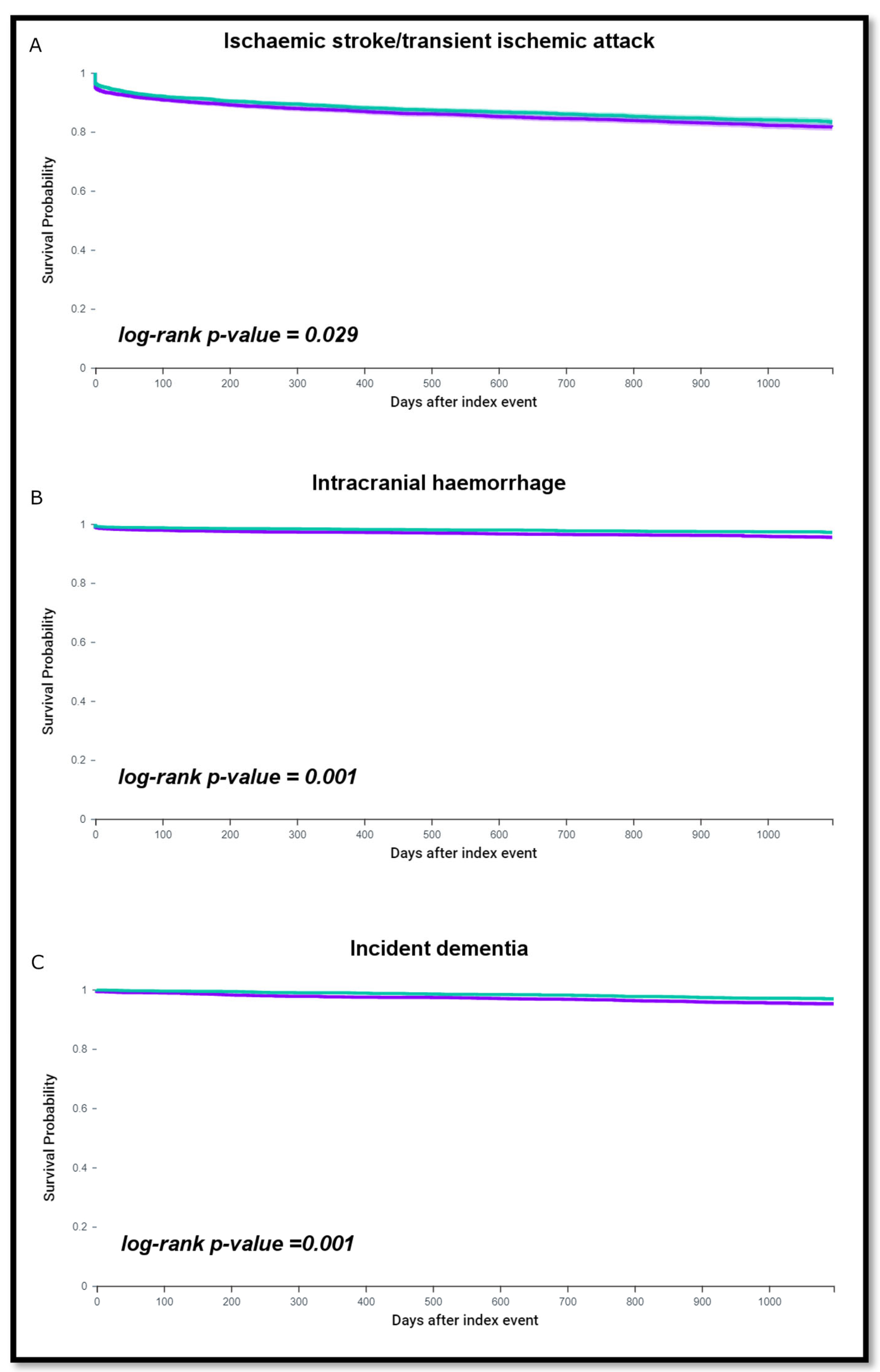
After a follow-up of three years, 767 (15.2%) patients without SGLT2i therapy and 693 (13.7%) patients on SGLT2i therapy had an ischemic stroke or TIA. The risk of ischemic stroke/TIA was increased in patients without SGLT2i compared to those taking SGLT2i (HR 1.12, 95% CI 1.01–1.24, log-rank
p = 0.029) (
Figure 1A). In addition, 183 (3.6%) patients without SGLT2i and 115 (2.3%) taking SGLT2i had an ICH. The risk of ICH was greater in AF patients without SGLT2i therapy (HR 1.57, 95% CI 1.25–1.99; log-rank
p = 0.001), (
Figure 1B).
During the 3-year follow up, 174 patients (3.6%) without SGLT2i therapy and 104 (2.1%) on SGLT2i therapy had a diagnosis of incident dementia. The risk of dementia was higher among patients without SGLT2i therapy (HR 1.66, 95% CI 1.30–2.12; log-rank
p = 0.001), as shown in the survival analysis (
Figure 1C).
3.2. Incident Heart Failure and Mortality
During follow-up, 736 (24.3%) AF patients without SGLT2i and 496 (16.9%) patients on SGLT2i had incident heart failure. Survival free from incident heart failure was lower in patients using SGLT2i compared to those not receiving a SGLT2i (HR 1.50, 95% CI 1.34–1.68; log-rank p < 0.001). Mortality risk was higher among patients not on SGLT2i (HR 1.77, 95% CI 1.58–1.99; log rank p < 0.001).
4. Discussion
The main findings of our analysis demonstrate that SGLT2i therapy is associated with a reduced incidence of cerebrovascular events and dementia in patients with AF and T2DM. In addition, there was a decrease in heart failure episodes and improved survival in patients with AF and T2DM treated with SGLT2i.
Given the high prevalence of AF and dementia worldwide, in particular among older people, our finding of a decreased incidence of dementia in the cohort of patients with AF treated with SGLT2i is important. Numerous observational studies over the past 10 years, including two meta-analyses, [
10,
11] have shown that AF is associated with cognitive impairment and dementia, even in the absence of clinically overt previous stroke. Patients with AF are also exposed to a significant risk of Alzheimer’s disease [
12]. This finding identifies a more complex interaction between AF and cognitive decline in which vascular and degenerative mechanisms, including cerebral amyloid deposition, co-exist and interact. Recently a novel SGLT2i mechanistic theory linking changes in glucose, free fatty acids (FFA) and AA metabolism to improvements in mitochondrial functioning, was proposed [
13]. The SGLT2i drugs promote the loss of glucose in the urine, which can impact the mTOR signalling pathway and modulate AMPK activity; and both molecular pathways play a role in cerebral amyloid deposition and development of Alzheimer’s disease [
14]. Finally, in patients with non-alcoholic fatty liver disease, treatment with SGLT2i improves neural mitochondrial function as indicated by increased levels of circulating
n-acetyl aspartate (NAA), a biomarker of neural mitochondrial viability [
15]. Depletion of NAA, as occurs in Alzheimer’s disease, may also play a direct role in promoting amyloid deposition [
15]. One ongoing pilot study is evaluating the impact of dapagliflozin treatment on patients with Alzheimer’s disease (NCT03801642). Considering the link between vascular amyloid angiopathy and Alzheimer’s disease related amyloidosis, it may be hypothesized that SGLT2i may be effective in modifying the risk of dementia in patients with AF.
Sub-analysis of the major randomised controlled trials (RCTs) and a subsequent meta-analysis have proposed a possible benefit of SGLT2i in reducing the incidence of stroke; the effect seems to correlate with baseline kidney function being more evident for those with low estimated glomerular filtration rate [
7,
16]. Increasing evidence also suggests anti-arrhythmic effects of SGLT2i with a reduced incidence of newly diagnosed AF or AF burden in patients with already diagnosed AF [
8,
17]. Such anti-arrhythmic properties preventing the development of new incident AF/AFL, may underline the suggested impact of SGLT2i therapy on reducing stroke incidence. Indeed, the risk of AF is increased in patients with chronic kidney disease, thereby justifying the benefit in this group of patients. In our study, the two cohorts identified were adjusted for chronic kidney disease after PSM, which may confirm a benefit from SGLT2i therapy independently from baseline renal function. In addition, various vascular and systemic effects of SGLT2i have been described beside the lowering of blood glucose, which can help decrease the risk of cerebrovascular events, including modulation of anti-inflammatory effects with a decrease in epicardial fat, leptin and TNFα production, and improvements in vascular function with a decrease in blood pressure, vascular stiffness and uric acid levels [
18].
Of note, our analysis shows a benefit of SGLT2i on reducing non-traumatic ICH.
Our findings report an absolute difference in means of approximately 1.3% and the risk of ICH was 1.57-fold higher in AF patients without SGLT2i therapy, which may underline important clinical implication. Indeed, currently there are no drugs that have shown effect in preventing ICH.
Large prospective studies have shown that both hypoglycaemic and hyperglycaemic episode are associated with ICH [
19]. The SGLT2i have a mechanism of action not linked to insulin secretion, which makes the detrimental occurrence of hypoglycemia less likely compared to other classes of anti-diabetic drugs and also allows the achievement of steady levels of blood glucose. This feature along with the aforementioned actions on blood pressure lowering and improvement in endothelial function and vascular stiffness may explain the possible benefits of SGLT2i on ICH.
In our analysis, the benefits of SGLT2i on the risk of heart failure and overall survival among patients with AF were evident from the early stages of follow-up. Indeed, large RCTs of SGLT2i have demonstrated improved cardiovascular outcomes in patients with T2DM, including a reduced risk of cardiovascular death and hospitalisations for heart failure [
3,
4,
5]. Both the DAPA-HF [
20] and EMPEROR-Reduced trial [
21] have shown that in patients with heart failure and reduced ejection fraction, the benefit of SGLT2i are independent of diabetes mellitus. The EMPEROR-Preserved trial [
22] has further extended this finding showing similar effects in terms of reduction of cardiovascular morbidity and mortality in patients with and without T2DM who have concomitant heart failure with preserved ejection fraction.
Limitations
Several limitations should be considered when interpreting the results of the current study. First our analysis was a retrospective study performed on EMR, and from this dose and duration of SGTL2i treatment could not be ascertained. Accordingly, a comparison between different SGLT2i and dose could not be performed. It is also possible that some changes to prescriptions may have been made outside of HCOs and not been captured within the TriNetX health research network. Furthermore, in our analysis, the cohorts were matched for factors including age, sex, ethnicity and co-morbidities, but residual confounding may still be present and some health conditions may be underreported in EMRs. Finally, an assessment of socio-economic and genetic factors biasing the associations between AF and dementia could not be performed.
5. Conclusions
In our large ‘real-world’ analysis of patients with concomitant AF and T2DM, SGLT2i therapy significantly reduced the risk of cerebrovascular events and incident dementia, heart failure and mortality. Considering the epidemiological relevance of the link between AF and dementia, the possible benefit of the metabolic effect of SGLT2i in preventing cognitive deterioration in this group of patients requires testing in a prospective study.
Author Contributions
Conceptualization R.P.; methodology, R.P., J.M.R.-C., S.L.H.; software J.M.R.-C., S.L.H.; validation, J.M.R.-C., R.P.; formal analysis J.M.R.-C., R.P.; writing—original draft preparation R.P., J.M.R.-C., R.L.-G.; writing—review and editing S.L.H., F.M., E.S., G.M., M.V., R.D., C.G., D.A.L. and G.Y.H.L., supervision, G.Y.H.L.; project administration P.U. All authors have read and agreed to the published version of the manuscript.
Funding
This is independent research funded by the National Institute for Health Research Applied Research Collaboration North West Coast (ARC NWC). The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Institutional Review Board Statement
As a federated research network, studies using the TriNetX health research network do not require ethical approval as no patient is identifiable.
Data Availability Statement
The data that support the findings of this study are available from TriNetX. To gain access to the data, a request can be made to TriNetX (
https://live.trinetx.com, accessed on 20 March 2023), but costs may be incurred, and a data sharing agreement is needed.
Conflicts of Interest
G.Y.H.L.: Consultant and speaker for BMS/Pfizer, Boehringer Ingelheim and Daiichi-Sankyo. No fees are received personally, J.M.R.C.: Consultant for Idorsia Pharmaceuticals LTD. There is nothing to disclose for other authors, DAL has received investigator-initiated educational grants from Bristol Myers Squibb (BMS) and Pfizer; been a speaker for Boehringer Ingelheim, Bayer, and BMS/Pfizer and consulted for Boehringer Ingelheim and BMS/Pfizer; all outside the submitted work. She is a co-applicant of the AFFIRMO project on multimorbidity in AF, which has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 899871.
References
- Brown, E.; Heerspink, H.J.L.; Cuthbertson, D.J.; Wilding, J.P.H. SGLT2 inhibitors and GLP-1 receptor agonists: Established and emerging indications. Lancet 2021, 398, 262–276. [Google Scholar] [CrossRef] [PubMed]
- Fathi, A.; Vickneson, K.; Singh, J.S. SGLT2-inhibitors; more than just glycosuria and diuresis. Heart Fail. Rev. 2021, 26, 623–642. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neal, B.; Perkovic, V.; Mahaffey, K.W.; de Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef] [PubMed]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Z.; Jardine, M.J.; Li, Q.; Neuen, B.L.; Cannon, C.P.; de Zeeuw, D.; Edwards, R.; Levin, A.; Mahaffey, K.W.; Perkovic, V.; et al. Effect of SGLT2 inhibitors on stroke and atrial fibrillation in diabetic kidney disease: Results from the CREDENCE trial and meta-analysis. Stroke 2021, 52, 1545–1556. [Google Scholar] [CrossRef]
- Zelniker, T.A.; Bonaca, M.P.; Furtado, R.H.M.; Mosenzon, O.; Kuder, J.F.; Murphy, S.A.; Bhatt, D.L.; Leiter, L.A.; McGuire, D.K.; Wilding, J.P.H.; et al. Effect of dapagliflozin on atrial fibrillation in patients with type 2 diabetes mellitus: Insights from the DECLARE-TIMI 58 Trial. Circulation 2020, 141, 1227–1234. [Google Scholar] [CrossRef]
- Haukoos, J.S.; Lewis, R.J. The propensity score. JAMA 2015, 314, 1637–1638. [Google Scholar] [CrossRef]
- Kalantarian, S.; Ruskin, J.N. Atrial Fibrillation and Cognitive Decline. Cardiol. Clin. 2016, 34, 279–285. [Google Scholar] [CrossRef]
- Santangeli, P.; Di Biase, L.; Bai, R.; Mohanty, S.; Pump, A.; Brantes, M.C.; Horton, R.; Burkhardt, J.D.; Lakkireddy, D.; Reddy, Y.M.; et al. Atrial fibrillation and the risk of incident dementia: A meta-analysis. Heart Rhythm. 2012, 9, 1761–1768. [Google Scholar] [CrossRef]
- Proietti, R.; Alturki, A.; Vio, R.; Licchelli, L.; Rivezzi, F.; Marafi, M.; Russo, V.; Potpara, T.S.; Kalman, J.M.; De Villers-Sidani, E.; et al. The association between atrial fibrillation and Alzheimer’s disease: Fact or fallacy? A systematic review and meta-analysis. J. Cardiovasc. Med. 2020, 21, 106–112. [Google Scholar] [CrossRef]
- Jin, C.; Li, G.; Rexrode, K.M.; Gurol, M.E.; Yuan, X.; Hui, Y.; Ruan, C.; Vaidya, A.; Wang, Y.; Wu, S.; et al. Prospective study of fasting blood glucose and intracerebral hemorrhagic risk. Stroke 2018, 49, 27–33. [Google Scholar] [CrossRef]
- Esterline, R.; Oscarsson, J.; Burns, J. A role for sodium glucose cotransporter 2 inhibitors (SGLT2is) in the treatment of Alzheimer’s disease? Int. Rev. Neurobiol. 2020, 155, 113–140. [Google Scholar] [CrossRef]
- Eriksson, J.W.; Lundkvist, P.; Jansson, P.A.; Johansson, L.; Kvarnström, M.; Moris, L.; Miliotis, T.; Forsberg, G.B.; Risérus, U.; Lind, L.; et al. Effects of dapagliflozin and n-3 carboxylic acids on non-alcoholic fatty liver disease in people with type 2 diabetes: A double-blind randomised placebo-controlled study. Diabetologia 2018, 61, 1923–1934. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Z.; Lindley, R.I.; Rådholm, K.; Jenkins, B.; Watson, J.; Perkovic, V.; Mahaffey, K.W.; de Zeeuw, D.; Fulcher, G.; Shaw, W.; et al. Canagliflozin and Stroke in Type 2 Diabetes Mellitus: Results from the Randomized CANVAS Program Trials. Stroke 2019, 50, 396–404. [Google Scholar] [CrossRef] [Green Version]
- Li, H.L.; Lip, G.Y.H.; Feng, Q.; Fei, Y.; Tse, Y.K.; Wu, Z.M.; Wen, R.Q.; Tse, H.F.; Cheung, B.M.Y.; Yiu, K.H. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) and cardiac arrhythmias: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2021, 20, 100. [Google Scholar] [CrossRef]
- Verma, S.; McMurray, J.J.V. SGLT2 inhibitors and mechanisms of cardiovascular benefit: A state-of-the-art review. Diabetologia 2018, 61, 2108–2117. [Google Scholar] [CrossRef] [Green Version]
- Esterline, R.L.; Vaag, A.; Oscarsson, J.; Vora, J. SGLT2 inhibitors: Clinical benefits by restoration of normal diurnal metabolism? Eur. J. Endocrinol. 2018, 178, R113–R125. [Google Scholar] [CrossRef] [Green Version]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [Green Version]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner-La Rocca, H.-P.; Choi, D.-J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).