Elective Ascending Aortic Aneurysm Surgery in the Elderly
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Operative Characteristics
3.3. Short-Term Postoperative Outcomes
3.4. Long-Term Survival
4. Discussion
4.1. Patient Characteristics
4.2. Operative Characteristics
4.3. Short-Term Postoperative Outcomes
4.4. Long-Term Survival
4.5. Study Limitations
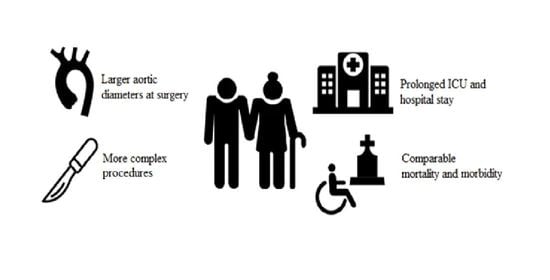
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AA | Ascending Aorta |
| ACP | Antegrade Cerebral Perfusion |
| AVR | Aortic Valve Replacement |
| BSA | Body Surface Area |
| CABG | Coronary Artery Bypass Grafting |
| CCS | Canadian Cardiovascular Society |
| COPD | Chronic Obstructive Pulmonary Disease |
| CVA | Cerebrovascular Accident |
| DHCA | Deep Hypothermic Cardiac Arrest |
| EuroSCORE | European System for Cardiac Operative Risk Evaluation score |
| eGFR | estimated Glomerular Filtration Rate |
| HR | Hazard Rate |
| HTAD | Hereditary Thoracic Aortic Diseases |
| ICU | Intensive Care Unit |
| IQR | Interquartile Range |
| LCC | Left Coronary Cusp |
| LVEF | Left Ventricle Ejection Fraction |
| NE/E | Non-elderly/Elderly |
| NCC | Non Coronary Cusp |
| NYHA | New York Heart Association |
| RCC | Right Coronary Cusp |
| SCAR | Supracoronary aorta replacement |
| TIA | Transient Ischemic Attack |
| VSARR | Valve Sparing Aortic Root Replacement |
References
- Rudnicka, E.; Napierała, P.; Podfigurna, A. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, L.; Giallauria, F.; Guralnik, J.M. Epidemiology of Aging. Radiol. Clin. N. Am. 2008, 46, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef] [PubMed]
- Ganapathi, A.M.; Englum, B.R.; Hanna, J.M.; Schechter, M.A.; Gaca, J.G.; Hurwitz, L.M.; Hughes, G.C. Frailty and risk in proximal aortic surgery. J. Thorac. Cardiovasc. Surg. 2014, 147, 186–191.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turrentine, F.E.; Wang, H.; Simpson, V.B.; Jones, R.S. Surgical risk factors, morbidity, and mortality in elderly patients. J. Am. Coll. Surg. 2006, 203, 865–877. [Google Scholar] [CrossRef]
- Sorabella, R.A.; Wu, Y.S.; Bader, A.; Kim, M.J.; Smith, C.R.; Takayama, H.; Borger, M.A.; George, I. Aortic Root Replacement in Octogenarians Offers Acceptable Perioperative and Late Outcomes. Ann. Thorac. Surg. 2016, 101, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Wanamaker, K.M.; Hirji, S.A.; Del Val, F.R.; Yammine, M.; Lee, J.; McGurk, S.; Shekar, P.; Kaneko, T. Proximal aortic surgery in the elderly population: Is advanced age a contraindication for surgery? J. Thorac. Cardiovasc. Surg. 2019, 157, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Kilic, A.; Arnaoutakis, G.J.; Bavaria, J.E.; Sultan, I.; Desai, N.D.; Vallabhajosyula, P.; Williams, M.L.; Milewski, R.K.; Szeto, W.Y. Outcomes of Elective Aortic Hemiarch Reconstruction for Aneurysmal Disease in the Elderly. Ann. Thorac. Surg. 2017, 104, 1522–1530. [Google Scholar] [CrossRef] [Green Version]
- Shah, P.J.; Estrera, A.L.; Miller, C.C., 3rd; Lee, T.Y.; Irani, A.D.; Meada, R.; Safi, H.J. Analysis of ascending and transverse aortic arch repair in octogenarians. Ann. Thorac. Surg. 2008, 86, 774–779. [Google Scholar] [CrossRef]
- Peterss, S.; Mansour, A.M.; Zafar, M.A.; Thombre, K.; Rizzo, J.A.; Ziganshin, B.A.; Darr, U.M.; Elefteriades, J.A. Elective surgery for ascending aortic aneurysm in the elderly: Should there be an age cut-off? Eur. J. Cardiothorac. Surg. 2017, 51, 965–970. [Google Scholar] [CrossRef] [Green Version]
- Du Bois, D.; Du Bois, E.F. A formula to estimate the approximate surface area if height and weight be known. Nutrition 1989, 5, 303–311; discussion 312–313. [Google Scholar] [PubMed]
- Akins, C.W.; Miller, D.C.; Turina, M.I.; Kouchoukos, N.T.; Blackstone, E.H.; Grunkemeier, G.L.; Takkenberg, J.J.; David, T.E.; Butchart, E.G.; Adams, D.H.; et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. Eur. J. Cardiothorac. Surg. 2008, 33, 523–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devereux, R.B.; de Simone, G.; Arnett, D.K.; Best, L.G.; Boerwinkle, E.; Howard, B.V.; Kitzman, D.; Lee, E.T.; Mosley, T.H., Jr.; Weder, A.; et al. Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons ≥15 years of age. Am. J. Cardiol. 2012, 110, 1189–1194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolak, A.; Gransar, H.; Thomson, L.E.; Friedman, J.D.; Hachamovitch, R.; Gutstein, A.; Shaw, L.J.; Polk, D.; Wong, N.D.; Saouaf, R.; et al. Aortic size assessment by noncontrast cardiac computed tomography: Normal limits by age, gender, and body surface area. JACC Cardiovasc. Imaging 2008, 1, 200–209. [Google Scholar] [CrossRef] [Green Version]
- Erbel, R.; Aboyans, V.; Boileau, C.; Bossone, E.; Di Bartolomeo, R.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Gaemperli, O. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2873–2926. [Google Scholar]
- Cury, M.; Zeidan, F.; Lobato, A.C. Aortic disease in the young: Genetic aneurysm syndromes, connective tissue disorders, and familial aortic aneurysms and dissections. Int. J. Vasc. Med. 2013, 2013, 267215. [Google Scholar] [CrossRef] [Green Version]
- Goldstone, A.B.; Chiu, P.; Baiocchi, M.; Lingala, B.; Patrick, W.L.; Fischbein, M.P.; Woo, Y.J. Mechanical or Biologic Prostheses for Aortic-Valve and Mitral-Valve Replacement. N. Engl. J. Med. 2017, 377, 1847–1857. [Google Scholar] [CrossRef]
- Esaki, J.; Leshnower, B.G.; Binongo, J.N. The David V Valve-Sparing Root Replacement Provides Improved Survival Compared with Mechanical Valve-conduits in the Treatment of Young Patients with Aortic Root Pathology. Ann. Thorac. Surg. 2016, 102, 1522–1530. [Google Scholar] [CrossRef] [Green Version]
- Yokawa, K.; Ikeno, Y.; Koda, Y.; Henmi, S.; Matsueda, T.; Takahashi, H.; Nakai, H.; Yamanaka, K.; Gotake, Y.; Tanaka, H.; et al. Valve-Sparing Root Replacement in Elderly Patients with Annuloaortic Ectasia. Ann. Thorac. Surg. 2019, 107, 1342–1347. [Google Scholar] [CrossRef]
- Guo, M.H.; Tran, D.; Ahmadvand, A.; Coutinho, T.; Glineur, D.; Al-Atassi, T.; Boodhwani, M. Perioperative and Long-Term Morbidity and Mortality for Elderly Patients Undergoing Thoracic Aortic Surgery. Semin. Thorac. Cardiovasc. Surg. 2020, 32, 644–652. [Google Scholar] [CrossRef]
- Arakawa, M.; Miyata, H.; Uchida, N.; Motomura, N.; Katayama, A.; Tamura, K.; Sueda, T.; Takamoto, S. Postoperative atrial fibrillation after thoracic aortic surgery. Ann. Thorac. Surg. 2015, 99, 103–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fowler, V.G.; Jr O’Brien, S.M.; Muhlbaier, L.H.; Corey, G.R.; Ferguson, T.B.; Peterson, E.D. Clinical predictors of major infections after cardiac surgery. Circulation 2005, 112 (Suppl. S9), I358–I365. [Google Scholar] [CrossRef] [PubMed]
- Kirfel, A.; Menzenbach, J.; Guttenthaler, V.; Feggeler, J.; Mayr, A.; Coburn, M.; Wittmann, M. Postoperative delirium after cardiac surgery of elderly patients as an independent risk factor for prolonged length of stay in intensive care unit and in hospital. Aging Clin. Exp. Res. 2021, 33, 3047–3056. [Google Scholar] [CrossRef]
- Loef, B.G.; Henning, R.H.; Navis, G.; Rankin, A.J.; Van Oeveren, W.; Ebels, T.; Epema, A.H. Changes in glomerular filtration rate after cardiac surgery with cardiopulmonary bypass in patients with mild preoperative renal dysfunction. Br. J. Anaesth. 2008, 100, 759–764. [Google Scholar] [CrossRef] [Green Version]
- Vives, M.; Hernandez, A.; Parramon, F.; Estanyol, N.; Pardina, B.; Muñoz, A.; Alvarez, P.; Hernandez, C. Acute kidney injury after cardiac surgery: Prevalence, impact and management challenges. Int. J. Nephrol. Renov. Dis. 2019, 12, 153–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bentall, H.; De Bono, A. A technique for complete replacement of the ascending aorta. Thorax 1968, 23, 338–339. [Google Scholar] [CrossRef] [Green Version]
- David, T.E.; David, C.M.; Manlhiot, C.; Colman, J.; Crean, A.M.; Bradley, T. Outcomes of Aortic Valve-Sparing Operations in Marfan Syndrome. J. Am. Coll. Cardiol. 2015, 66, 1445–1453. [Google Scholar] [CrossRef] [Green Version]
- Yacoub, M. Valve-Conserving Operation for Aortic Root Aneurysm or Dissection. Oper. Tech. Card. Thorac. Surg. 1996, 1, 57–67. [Google Scholar] [CrossRef] [Green Version]



| Total (n = 955) | Non-Elderly (n = 724) | Elderly (n = 231) | p-Value | Missings (NE/E) 1 | |
|---|---|---|---|---|---|
| Age (years) | 61.0 (50.0–69.0) | 55.0 (45.0–63.0) | 74.0 (72.0–77.0) | <0.0001 ** | 0/955 |
| Sex (% male) | 621 (65.0) | 509 (70.3) | 112 (48.3) | <0.001 ** | 0/955 |
| BSA | 2.02 ± 0.22 | 2.05 ± 0.23 | 1.95 ± 0.17 | <0.001 ** | (1/724)/(0/231) |
| History of Hypertension | 570 (59.7) | 384 (54.4) | 186 (81.6) | <0.001 ** | (18/724)/(3/231) |
| History of Dyslipidemia | 291 (30.5) | 200 (28.5) | 91 (40.3) | 0.001 ** | (22/724)/(5/231) |
| History of Diabetes Mellitus | 62 (6.5) | 41 (5.7) | 21 (9.3) | 0.067 | (10/724)/(4/231) |
| History of CVA/TIA | 110 (11.5) | 74 (10.4) | 36 (15.7) | 0.034 * | (12/724)/(1/231) |
| History of COPD | 90 (9.4) | 60 (8.4) | 30 (13.2) | 0.039 * | (13/724)/(3/231) |
| History of Smoking | (302/724)/(87/231) | ||||
| Never | 182 (19.1) | 134 (31.8) | 48 (33.3) | 0.76 | |
| Currently | 149 (15.6) | 124 (29.4) | 25 (17.4) | 0.004 ** | |
| In past | 235 (24.6) | 164 (38.9) | 71 (49.3) | 0.031 * | |
| History of Chronic Kidney Disease | 48 (5.0) | 25 (3.5) | 23 (10.1) | <0.001 ** | (10/724)/(3/231) |
| eGFR (mL/min) | <0.001 ** | (0/724)/(1/231) | |||
| <60 | 121 (12.7) | 56 (7.7) | 65 (28.3) | ||
| ≥60 | 833 (87.2) | 668 (92.3) | 165 (71.7) | ||
| History of Myocardial Infarction | 50 (5.2) | 37 (5.1) | 13 (5.8) | 0.73 | (2/724)/(6/231) |
| Family History of Aortic Pathology | 134 (14.0) | 120 (42.0) | 14 (19.7) | 0.001 ** | (438/724)/(161/231) |
| Diagnosis of HTAD Prior to Surgery | 129 (13.5) | 123 (17.0) | 6 (2.6) | <0.001 ** | (504/724)/(216/231) |
| Marfan Syndrome | 48 (5.0) | 47 (6.5) | 1 (0.4) | <0.001 ** | |
| Loeys–Dietz Syndrome | 5 (0.5) | 5 (0.7) | 0 (0.0) | 0.34 | |
| SMAD3 Mutation | 10 (1.0) | 10 (1.4) | 0 (0.0) | 0.13 | |
| Turner Syndrome | 8 (0.8) | 8 (1.1) | 0 (0.0) | 0.21 | |
| Suspected | 42 (4.4) | 39 (5.4) | 3 (1.3) | 0.005 ** | |
| Other | 16 (1.7) | 14 (1.9) | 2 (0.9) | 0.38 | |
| Prior Cardiac Surgery | 97 (10.2) | 81 (11.2) | 16 (6.9) | 0.062 | 0/955 |
| Prior Aortic Surgery | 85 (8.9) | 73 (10.1) | 12 (5.2) | 0.024 * | (1/724)/(1/231) |
| Aortic Valve | |||||
| Stenosis | 221 (23.1) | 178 (26.2) | 43 (20.6) | 0.099 | (45/724)/(23/231) |
| Insufficiency | 397 (41.6) | 289 (42.2) | 108 (50.7) | 0.033 * | (39/725)/(19/231) |
| NYHA Classification | (64/724)/(23/231) | ||||
| Class I | 500 (52.4) | 402 (60.9) | 98 (47.1) | <0.001 ** | |
| Class II | 224 (23.5) | 159 (24.1) | 65 (31.3) | 0.040 * | |
| Class III | 135 (14.1) | 91 (13.8) | 44 (21.2) | 0.010 * | |
| Class IV | 9 (0.9) | 8 (1.2) | 1 (0.5) | 0.695 | |
| CCS Classification | (87/724)/(35/231) | ||||
| Class I | 711 (74.5) | 551 (86.5) | 160 (81.6) | 0.092 | |
| Class II | 79 (8.3) | 53 (8.3) | 26 (13.3) | 0.039 * | |
| Class III | 36 (3.8) | 27 (4.2) | 9 (4.6) | 0.84 | |
| Class IV | 7 (0.7) | 6 (0.9) | 1 (0.5) | 1.00 | |
| LVEF | (57/724)/(14/231) | ||||
| Good (>55%) | 680 (71.2) | 524 (78.6) | 156 (71.9) | 0.043 * | |
| Reduced (44–55%) | 112 (11.7) | 80 (12.0) | 32 (14.7) | 0.29 | |
| Moderate (30–45%) | 85 (8.9) | 60 (9.0) | 25 (11.5) | 0.27 | |
| Poor (<30%) | 7 (0.7) | 3 (0.5) | 4 (1.8) | 0.067 | |
| Bicuspid Aortic Valve | 0/955 (21/724)/(12/231) (21/724)/(12/231) (21/724)/(12/231) 0/955 | ||||
| Location of Maximal Aortic Diameter | 375 (39.3) | 332 (45.9) | 43 (18.6) | <0.001 ** | |
| Sinuses of Valsalva | 191 (20.0) | 170 (24.1) | 21 (9.6) | <0.001 ** | |
| Ascending Aorta | 722 (75.6) | 527 (74.8) | 195 (89.0) | <0.001 ** | |
| Aortic Arch | 10 (1.0) | 7 (1.0) | 3 (1.4) | 0.71 | |
| Descending Aorta | 1 (0.1) | 1 (0.1) | 0 (0.0) | 1.00 | |
| Maximal Absolute Aortic Diameter (mm) | 54.0 (50.0–59.0) | 53.0 (49.0–58.0) | 57.0 (53.0–63.0) | <0.001 ** | |
| Maximal Indexed Aortic Diameter (mm/m2) | 26.7 (24.0–30.3) | 25.9 (23.4–29.2) | 30.3 (26.9–34.5) | <0.00 ** | |
| Logistic EUROscore | 9.0 (5.3–14.4) | 7.0 (5.0–11.6) | 17.4 (13.0–22.7) | <0.001 ** |
| Total (n = 955) | Non-Elderly (n = 724) | Elderly (n = 231) | p-Value | Missings (NE/E) 1 | |
|---|---|---|---|---|---|
| Bentall Procedure | 491 (51.4) | 389 (53.7) | 102 (44.0) | 0.010 * | 0/955 |
| Mechanical | 324 (33.9) | 304 (42.0) | 20 (8.6) | <0.001 ** | |
| Biological | 167 (17.5) | 85 (11.7) | 82 (35.3) | <0.001 ** | |
| David technique | 117 (12.3) | 110 (15.2) | 7 (3.0) | <0.001 ** | 0/955 |
| (Partial) Yacoub technique | 24 (2.5) | 17 (2.3) | 7 (3.0) | 0.63 | 0/955 |
| SCAR | 390 (40.8) | 264 (36.5) | 126 (54.3) | <0.001 ** | 0/955 |
| No AVR | 219 (22.9) | 152 (21.0) | 67 (28.9) | 0.013 * | |
| Mechanical AVR | 53 (5.5) | 52 (7.2) | 1 (0.4) | <0.001 ** | |
| Biological AVR a | 89 (9.3) | 44 (6.1) | 45 (19.4) | <0.001 ** | |
| Valve repair | 27 (2.8) | 14 (1.9) | 13 (5.6) | 0.003 ** | |
| Concomitant Procedures | 514 (53.8) | 359 (49.6) | 155 (66.8) | <0.001 ** | 0/955 |
| (Hemi-)arch | 392 (41.0) | 269 (37.2) | 123 (53.0) | <0.001 ** | |
| CABG | 106 (11.1) | 67 (9.3) | 39 (16.8) | 0.002 ** | |
| Mitral valve surgery | 32 (3.4) | 20 (2.8) | 12 (5.2) | 0.076 | |
| Other b | 59 (6.2) | 44 (6.1) | 15 (6.5) | 0.83 | |
| Perfusion Time (min) | 163.0 (125.0–198.0) | 163.0 (124.0–198.5) | 162.0 (129.5–197.3) | 0.69 | (7/724)/(1/231) |
| Aortic Cross-Clamp Time (min) | 107.0 (83.3–136.0) | 108.0 (84.0–138.0) | 103.0 (82.0–132.5) | 0.12 | (8/724)/(4/231) |
| DHCA c | 420 (44.0) | 290 (40.1) | 131 (56.5) | <0.001 ** | |
| Circulatory Arrest Time (min) | 19.0 (15.0–28.0) | 18.0 (14.0–27.0) | 20.0 (16.0–37.0) | 0.021 ** | (450/724)/(108/231) |
| Cerebral Protection c | 420 (44.0) | 290 (40.1) | 131 (56.5) | <0.001 ** | (3/724)/(3/231) |
| Antegrade Unilateral | 26 (2.7) | 19 (2.6) | 7 (3.0) | 0.82 | |
| Antegrade Bilateral | 388 (40.6) | 268 (37.0) | 120 (51.7) | <0.001 ** | |
| ACP time (min) c | 33.0 (20.0–68.0) | 29.0 (18.0–69.0) | 35.0 (25.8–63.5) | 0.26 | (199/724)/(80/231) |
| Total (n = 955) | Non-Elderly (n = 724) | Elderly (n = 231) | p-Value | Missings (NE/E) 1 | |
|---|---|---|---|---|---|
| In-hospital or 30-day Mortality | 18 (1.9) | 11 (1.5) | 7 (3.0) | 0.16 | 0/955 |
| Cause of Mortality | 0/955 | ||||
| Cardiac (incl. Tamponade) | 8 (0.8) | 6 (0.8) | 2 (0.9) | 1.00 | |
| Bleeding | 3 (0.3) | 2 (0.3) | 1 (0.4) | 0.57 | |
| Aortic Rupture | 2 (0.2) | 2 (0.3) | 0 (0.0) | 1.00 | |
| Organ Failure | 1 (0.1) | 0 (0.0) | 1 (0.4) | 0.24 | |
| Sepsis | 2 (0.2) | 0 (0.0) | 2 (0.9) | 0.06 | |
| Other | 1 (0.1) | 0 (0.0) | 1 (0.4) | 0.24 | |
| Number of Days the Patient Was Admitted a | 0/955 | ||||
| 1–4 | 23 (2.4) | 18 (2.5) | 5 (2.2) | 1.00 | |
| 5–9 | 590 (61.8) | 460 (63.5) | 130 (56.3) | 0.048 * | |
| 10–14 | 205 (21.5) | 154 (21.3) | 51 (22.1) | 0.78 | |
| 15–19 | 66 (6.9) | 47 (6.5) | 19 (8.2) | 0.37 | |
| ≥20 | 71 (7.4) | 45 (6.2) | 26 (11.3) | 0.014 * | |
| Total # | 8.0 (7.0–11.0) | 8.0 (7.0–11.0) | 7.0 (9.0–13.0) | 0.028 * | |
| Number of Days in ICU 1 After Surgery a | (20/724)/(4/231) | ||||
| 1–4 | 827 (86.6) | 641 (91.1) | 186 (81.9) | <0.001 ** | |
| 5–9 | 71 (7.4) | 41 (5.8) | 30 (13.2) | <0.001 ** | |
| 10–14 | 18 (1.9) | 11 (1.6) | 7 (3.1) | 0.17 | |
| 15–19 | 5 (0.5) | 4 (0.6) | 1 (0.4) | 1.0 | |
| ≥20 | 10 (1.0) | 7 (1.0) | 3 (1.3) | 0.71 | |
| Total # | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 2.0 (2.0–4.0) | <0.001 ** | |
| Number of Days on Ventilation Support After Surgery a | (28/724)/(9/231) | ||||
| 1 | 551 (57.7) | 455 (65.3) | 96 (43.2) | <0.001 ** | |
| 2 | 308 (32.3) | 205 (29.4) | 103 (46.4) | <0.001 ** | |
| 3 | 19 (2.0) | 10 (1.4) | 9 (4.1) | 0.027 * | |
| 4 | 10 (1.0) | 6 (0.9) | 4 (1.8) | 0.27 | |
| ≥5 | 31 (3.2) | 21 (3.0) | 10 (4.5) | 0.29 | |
| Total # | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | <0.001 ** | |
| Total Reoperations | 230 (24.1) | 155 (21.4) | 75 (32.3) | <0.001 ** | (127/724)/(59/231) |
| Bleeding | 157 (16.4) | 112 (15.5) | 45 (19.4) | 0.16 | |
| Tamponade | 31 (3.2) | 21 (2.9) | 10 (4.3) | 0.29 | |
| Mediastinitis | 16 (1.7) | 5 (0.7) | 11 (4.7) | <0.001 ** | |
| Cardiac Ischemia | 1 (0.1) | 1 (0.1) | 0 (0.0) | 0.76 | |
| Other Visceral Ischemia | 2 (0.2) | 0 (0.0) | 2 (0.2) | 0.059 | |
| Structural Valve Deterioration | 1 (0.1) | 1 (0.1) | 0 (0.0) | 0.57 | |
| Non-Structural Valve Deterior. | 1 (0.1) | 1 (0.1) | 0 (0.0) | 0.76 | |
| Endocarditis | 1 (0.1) | 1 (0.1) | 0 (0.0) | 0.76 | |
| Other | 20 (2.1) | 13 (1.8) | 7 (3.0) | 0.19 |
| Total (n = 955) | Non-Elderly (n = 724) | Elderly (n = 231) | p-Value | Missings (NE/E) 1 | |
|---|---|---|---|---|---|
| Tracheostoma Implantation | 8 (0.8) | 5 (0.7) | 3 (1.3) | 0.41 | (1/724)/(0/231) |
| New Permanent Heart Rhythm Disturbances | 245 (25.7) | 154 (21.3) | 91 (39.4) | <0.001 ** | (3/724)/(0/231) |
| Supraventricular | 211 (22.1) | 125 (17.3) | 86 (37.2) | <0.001 ** | |
| Ventricular | 6 (0.6) | 6 (0.8) | 0 (0.0) | 0.35 | |
| AV-block | 27 (2.8) | 22 (3.0) | 5 (2.2) | 0.65 | |
| Pacemaker or ICD Implanted | 32 (3.4) | 26 (3.6) | 6 (2.6) | 0.54 | 0/955 |
| Myocardial Infarction or Ischemia | 18 (1.9) | 13 (1.8) | 5 (2.2) | 0.78 | 0/955 |
| Infective Endocarditis | 4 (0.4) | 3 (0.4) | 1 (0.4) | 1.00 | (2/724)/(1/231) |
| Non-Structural Valve Dysfunction | 2 (0.2) | 2 (0.3) | 0 (0.0) | 1.00 | 0/955 |
| CVA/TIA | 43 (4.5) | 33 (4.6) | 10 (4.3) | 0.89 | (1/724)/(1/231) |
| New Recurrence Nerve Lesion | 12 (1.3) | 11 (1.5) | 1 (0.4) | 0.31 | 0/955 |
| Diagnosis of Delirium | 146 (15.3) | 80 (11.0) | 66 (28.6) | <0.001 ** | 0/955 |
| Diagnosis of Infection | 130 (13.6) | 82 (11.3) | 48 (20.8) | 0.001 ** | 0/955 |
| Diagnosis of Sepsis | 11 (1.2) | 7 (1.0) | 4 (1.7) | 0.31 | 0/955 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Memis, F.; Thijssen, C.G.E.; Gökalp, A.L.; Notenboom, M.L.; Meccanici, F.; Mokhles, M.M.; van Kimmenade, R.R.J.; Veen, K.M.; Geuzebroek, G.S.C.; Sjatskig, J.; et al. Elective Ascending Aortic Aneurysm Surgery in the Elderly. J. Clin. Med. 2023, 12, 2015. https://doi.org/10.3390/jcm12052015
Memis F, Thijssen CGE, Gökalp AL, Notenboom ML, Meccanici F, Mokhles MM, van Kimmenade RRJ, Veen KM, Geuzebroek GSC, Sjatskig J, et al. Elective Ascending Aortic Aneurysm Surgery in the Elderly. Journal of Clinical Medicine. 2023; 12(5):2015. https://doi.org/10.3390/jcm12052015
Chicago/Turabian StyleMemis, Feyza, Carlijn G. E. Thijssen, Arjen L. Gökalp, Maximiliaan L. Notenboom, Frederike Meccanici, Mohammad Mostafa Mokhles, Roland R. J. van Kimmenade, Kevin M. Veen, Guillaume S. C. Geuzebroek, Jelena Sjatskig, and et al. 2023. "Elective Ascending Aortic Aneurysm Surgery in the Elderly" Journal of Clinical Medicine 12, no. 5: 2015. https://doi.org/10.3390/jcm12052015