Post-Inflammatory Hypopigmentation: Review of the Etiology, Clinical Manifestations, and Treatment Options
Abstract
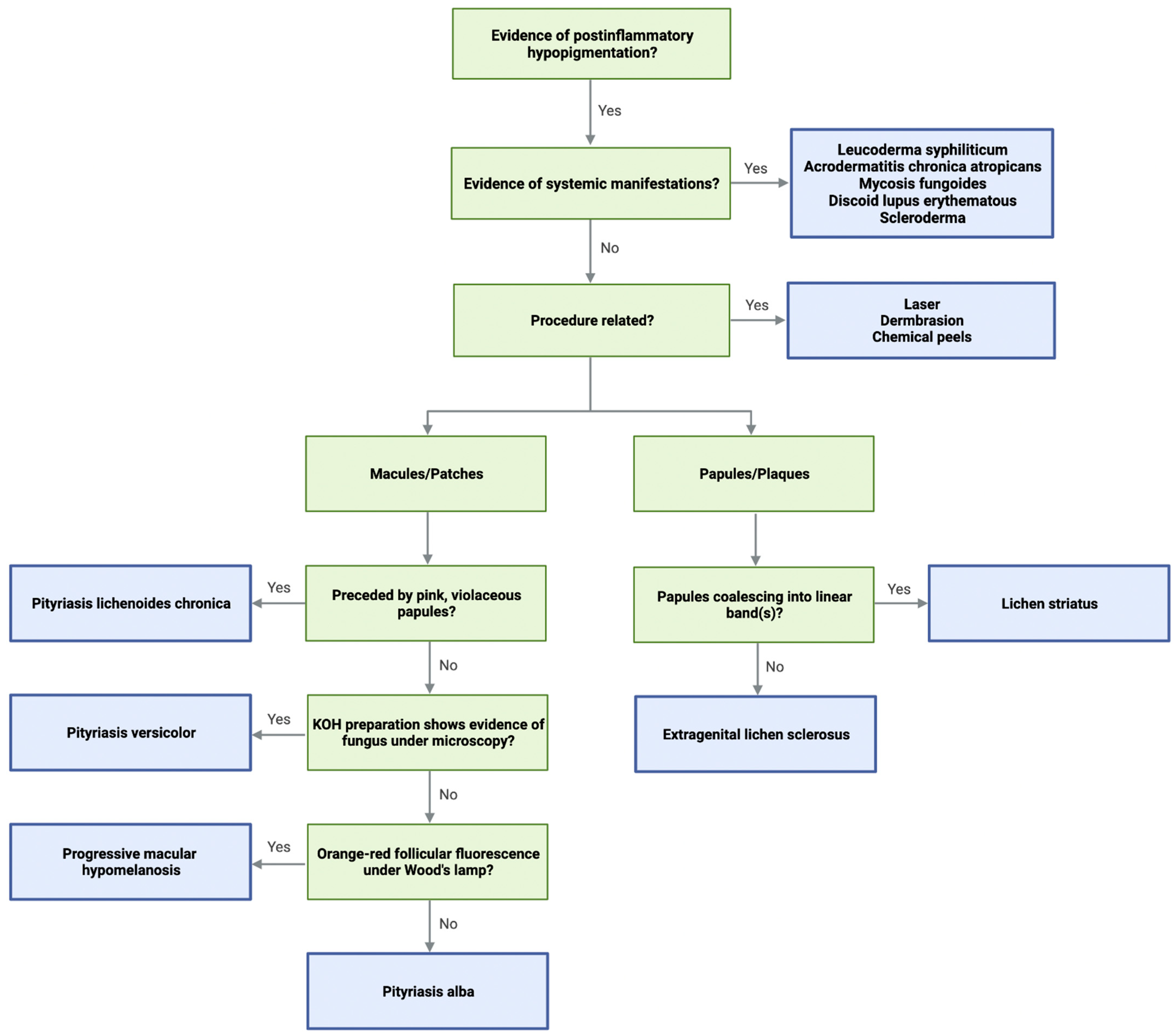
:1. Introduction
2. Methods
3. Pityriasis Alba
3.1. Etiology
3.2. Clinical Manifestations
3.3. Treatment
4. Lichen Striatus
4.1. Etiology
4.2. Clinical Manifestations
4.3. Treatment
5. Pityriasis Lichenoides Chronica (PLC)
5.1. Etiology
5.2. Clinical Manifestations
5.3. Treatment
6. Extragenital Lichen Sclerosus (EGLS)
6.1. Etiology
6.2. Clinical Manifestations
6.3. Treatment
7. Progressive Macular Hypomelanosis
7.1. Etiology
7.2. Clinical Manifestations
7.3. Treatment
8. Inflammatory Diseases
8.1. Scleroderma
8.1.1. Etiology
8.1.2. Clinical Manifestations
8.1.3. Treatment
8.2. Discoid Lupus Erythematosus
8.2.1. Etiology
8.2.2. Clinical Manifestations
8.2.3. Treatment
9. Infectious Diseases
9.1. Pityriasis Versicolor Alba
9.1.1. Etiology
9.1.2. Clinical Manifestations
9.1.3. Treatment
9.2. Leucoderma Syphiliticum (LSy)
9.2.1. Etiology
9.2.2. Clinical Manifestations
9.2.3. Treatment
9.3. Acrodermatitis Chronica Atrophicans
9.3.1. Etiology
9.3.2. Clinical Manifestations
9.3.3. Treatment
10. Mycosis Fungoides (MF)
10.1. Etiology
10.2. Clinical Manifestations
10.3. Treatment
11. Iatrogenic Hypopigmentation
11.1. Etiology
11.2. Clinical Manifestations
11.3. Treatment
12. Discussion
Limitation/Bias
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Vachiramon, V.; Thadanipon, K. Postinflammatory hypopigmentation. Clin. Exp. Dermatol. 2011, 36, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Madu, P.N.; Syder, N.; Elbuluk, N. Postinflammatory hypopigmentation: A comprehensive review of treatments. J. Dermatolog. Treat. 2022, 33, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Maldonado, R.; Orozco-Covarrubias, M.L. Postinflammatory hypopigmentation and hyperpigmentation. Semin. Cutan. Med. Surg. 1997, 16, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.; Pawaskar, M.; Taylor, S.L.; Balkrishnan, R.; Feldman, S.R. Prevalence of pigmentary disorders and their impact on quality of life: A prospective cohort study. J. Cosmet. Dermatol. 2008, 7, 164–168. [Google Scholar] [CrossRef]
- Dabas, G.; Vinay, K.; Parsad, D.; Kumar, A.; Kumaran, M.S. Psychological disturbances in patients with pigmentary disorders: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 392–399. [Google Scholar] [CrossRef]
- Halder, R.M.; Nootheti, P.K. Ethnic skin disorders overview. J. Am. Acad. Dermatol. 2003, 48 (Suppl. 6), S143–S148. [Google Scholar] [CrossRef]
- Kang, S.J.; Davis, S.A.; Feldman, S.R.; McMichael, A.J. Dyschromia in skin of color. J. Drugs Dermatol. 2014, 13, 401–406. [Google Scholar]
- Blessmann Weber, M.; Sponchiado de Avila, L.G.; Albaneze, R.; Magalhaes de Oliveira, O.L.; Sudhaus, B.D.; Cestari, T.F. Pityriasis alba: A study of pathogenic factors. J. Eur. Acad. Dermatol. Venereol. 2002, 16, 463–468. [Google Scholar] [CrossRef]
- Urano-Suehisa, S.; Tagami, H. Functional and morphological analysis of the horny layer of pityriasis alba. Acta Derm. Venereol. 1985, 65, 164–167. [Google Scholar]
- Bolognia, J.; Schaffer, J.V.; Cerroni, L. Dermatology, 4th ed.; Elsevier: Philadelphia, PA, USA, 2018. [Google Scholar]
- Martinez-Fierro, M.L.; Cabral-Pacheco, G.A.; Garza-Veloz, I.; Campuzano-Garcia, A.E.; Diaz-Alonso, A.P.; Flores-Morales, V.; Rodriguez-Sanchez, I.P.; Delgado-Enciso, I.; Rios-Jasso, J. Expression Levels of Inflammatory and Oxidative Stress-Related Genes in Skin Biopsies and Their Association with Pityriasis Alba. Medicina 2020, 56, 359. [Google Scholar] [CrossRef]
- Karanfilian, K.M.; Behbahani, S.; Lambert, M.W.; Alhatem, A.; Masessa, J.; Espinal-Mariotte, J.; Schwartz, R.A.; Lambert, W.C. The pathophysiology of pityriasis alba: Time-dependent histologic changes. Clin. Dermatol. 2020, 38, 354–356. [Google Scholar] [CrossRef]
- Zaynoun, S.T.; Aftimos, B.G.; Tenekjian, K.K.; Bahuth, N.; Kurban, A.K. Extensive pityriasis alba: A histological histochemical and ultrastructural study. Br. J. Dermatol. 1983, 108, 83–90. [Google Scholar] [CrossRef]
- In, S.I.; Yi, S.W.; Kang, H.Y.; Lee, E.S.; Sohn, S.; Kim, Y.C. Clinical and histopathological characteristics of pityriasis alba. Clin. Exp. Dermatol. 2009, 34, 591–597. [Google Scholar] [CrossRef]
- Miazek, N.; Michalek, I.; Pawlowska-Kisiel, M.; Olszewska, M.; Rudnicka, L. Pityriasis Alba—Common Disease, Enigmatic Entity: Up-to-Date Review of the Literature. Pediatr. Dermatol. 2015, 32, 786–791. [Google Scholar] [CrossRef]
- D’Orazio, J.; Jarrett, S.; Amaro-Ortiz, A.; Scott, T. UV radiation and the skin. Int. J. Mol. Sci. 2013, 14, 12222–12248. [Google Scholar] [CrossRef]
- Khafagy, G.M.; Nada, H.R.; Rashid, L.A.; El-Samanoudy, S.I.; Abd El-Sattar, E.M. Role of trace elements in pityriasis Alba. J. Trace Elem. Med. Biol. 2020, 59, 126422. [Google Scholar] [CrossRef]
- Elesawy, F.M.; Akl, E.M.; Abdel Halim, W.A. Zinc has a Role in Pathogenesis of Pityriasis Alba. Indian J. Paediatr. Dermatol. 2020, 21, 178–183. [Google Scholar]
- Wiriyasermkul, P.; Moriyama, S.; Nagamori, S. Membrane transport proteins in melanosomes: Regulation of ions for pigmentation. Biochim. Biophys. Acta (BBA)-Biomembr. 2020, 1862, 183318. [Google Scholar] [CrossRef]
- Givler, D.N.; Basit, H.; Givler, A. Pityriasis Alba. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Jadotte, Y.T.; Janniger, C.K. Pityriasis alba revisited: Perspectives on an enigmatic disorder of childhood. Cutis 2011, 87, 66–72. [Google Scholar]
- Lin, R.L.; Janniger, C.K. Pityriasis alba. Cutis 2005, 76, 21–24. [Google Scholar]
- Abdel-Wahab, H.M.; Ragaie, M.H. Pityriasis alba: Toward an effective treatment. J. Dermatolog. Treat. 2022, 33, 2285–2289. [Google Scholar] [CrossRef] [PubMed]
- Fujita, W.H.; McCormick, C.L.; Parneix-Spake, A. An exploratory study to evaluate the efficacy of pimecrolimus cream 1% for the treatment of pityriasis alba. Int. J. Dermatol. 2007, 46, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Rigopoulos, D.; Gregoriou, S.; Charissi, C.; Kontochristopoulos, G.; Kalogeromitros, D.; Georgala, S. Tacrolimus ointment 0.1% in pityriasis alba: An open-label, randomized, placebo-controlled study. Br. J. Dermatol. 2006, 155, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.Y.; Choi, Y.M. FK506 increases pigmentation and migration of human melanocytes. Br. J. Dermatol. 2006, 155, 1037–1040. [Google Scholar] [CrossRef]
- Birlea, S.A.; Costin, G.E.; Norris, D.A. Cellular and molecular mechanisms involved in the action of vitamin D analogs targeting vitiligo depigmentation. Curr. Drug Targets 2008, 9, 345–359. [Google Scholar] [CrossRef]
- Moreno-Cruz, B.; Torres-Alvarez, B.; Hernandez-Blanco, D.; Castanedo-Cazares, J.P. Double-blind, placebo-controlled, randomized study comparing 0.0003% calcitriol with 0.1% tacrolimus ointments for the treatment of endemic pityriasis alba. Dermatol. Res. Pract. 2012, 2012, 303275. [Google Scholar] [CrossRef]
- Al-Mutairi, N.; Hadad, A.A. Efficacy of 308-nm xenon chloride excimer laser in pityriasis alba. Dermatol. Surg. 2012, 38, 604–609. [Google Scholar] [CrossRef]
- Li, L.; Liang, Y.; Zhang, D.; Wang, C.; Pan, N.; Hong, J.; Xiao, H.; Xie, Z. The 308-nm excimer laser stimulates melanogenesis via the wnt/beta-Catenin signaling pathway in B16 cells. J. Dermatolog. Treat. 2019, 30, 826–830. [Google Scholar] [CrossRef]
- Zaynoun, S.; Jaber, L.A.; Kurban, A.K. Oral methoxsalen photochemotherapy of extensive pityriasis alba. Preliminary report. J. Am. Acad. Dermatol. 1986, 15, 61–65. [Google Scholar] [CrossRef]
- Shenoi, S.D.; Prabhu, S. Photochemotherapy (PUVA) in psoriasis and vitiligo. Indian J. Dermatol. Venereol. Leprol. 2014, 80, 497–504. [Google Scholar]
- Gupta, A.; Gautam, R.K.; Bhardwaj, M. Bilateral Lichen Striatus: A Case Report with Review of Literature. Indian Dermatol. Online J. 2017, 8, 264–266. [Google Scholar] [CrossRef]
- Charifa, A.; Jamil, R.T.; Ramphul, K. Lichen Striatus. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Patrizi, A.; Neri, I.; Fiorentini, C.; Bonci, A.; Ricci, G. Lichen striatus: Clinical and laboratory features of 115 children. Pediatr. Dermatol. 2004, 21, 197–204. [Google Scholar] [CrossRef]
- Kennedy, D.; Rogers, M. Lichen striatus. Pediatr. Dermatol. 1996, 13, 95–99. [Google Scholar] [CrossRef]
- Taieb, A.; el Youbi, A.; Grosshans, E.; Maleville, J. Lichen striatus: A Blaschko linear acquired inflammatory skin eruption. J. Am. Acad. Dermatol. 1991, 25, 637–642. [Google Scholar] [CrossRef]
- Zhang, Y.; McNutt, N.S. Lichen striatus. Histological, immunohistochemical, and ultrastructural study of 37 cases. J. Cutan. Pathol. 2001, 28, 65–71. [Google Scholar] [CrossRef]
- Staricco, R.G. Lichen striatus; a study of fifteen new cases with special emphasis on the histopathological changes and a review of the literature. AMA Arch. Derm. 1959, 79, 311–324. [Google Scholar] [CrossRef]
- Bae, J.M.; Choo, J.Y.; Chang, H.S.; Kim, H.; Lee, J.H.; Kim, G.M. Effectiveness of the 308-nm excimer laser on hypopigmentation after lichen striatus: A retrospective study of 12 patients. J. Am. Acad. Dermatol. 2016, 75, 637–639. [Google Scholar] [CrossRef]
- Stewart, W.M. Proceedings: Pathology of lichen striatus. Br. J. Dermatol. 1976, 95 (Suppl. 14), 18–19. [Google Scholar] [CrossRef]
- Peramiquel, L.; Baselga, E.; Dalmau, J.; Roe, E.; del Mar Campos, M.; Alomar, A. Lichen striatus: Clinical and epidemiological review of 23 cases. Eur. J. Pediatr. 2006, 165, 267–269. [Google Scholar] [CrossRef]
- Jo, J.H.; Jang, H.S.; Park, H.J.; Kim, M.B.; Oh, C.K.; Kwon, K.S. Early treatment of multiple and spreading lichen striatus with topical tacrolimus. J. Am. Acad. Dermatol. 2007, 57, 904–905. [Google Scholar] [CrossRef]
- Fujimoto, N.; Tajima, S.; Ishibashi, A. Facial lichen striatus: Successful treatment with tacrolimus ointment. Br. J. Dermatol. 2003, 148, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Bowers, S.; Warshaw, E.M. Pityriasis lichenoides and its subtypes. J. Am. Acad. Dermatol. 2006, 55, 557–572. [Google Scholar] [CrossRef] [PubMed]
- Durusu, I.N.; Gurel, G.; Tokyol, C. A Case of Pityriasis Lichenoides Chronica in a Patient with COVID-19 Infection. Actas Dermosifiliogr. 2022, 11, S18–S19. [Google Scholar] [CrossRef] [PubMed]
- Gil-Bistes, D.; Kluger, N.; Bessis, D.; Guillot, B.; Raison-Peyron, N. Pityriasis lichenoides chronic after measles-mumps-rubella vaccination. J. Dermatol. 2012, 39, 492–493. [Google Scholar] [CrossRef]
- Magro, C.M.; Crowson, A.N.; Morrison, C.; Li, J. Pityriasis lichenoides chronica: Stratification by molecular and phenotypic profile. Hum. Pathol. 2007, 38, 479–490. [Google Scholar] [CrossRef]
- Shieh, S.; Mikkola, D.L.; Wood, G.S. Differentiation and clonality of lesional lymphocytes in pityriasis lichenoides chronica. Arch. Dermatol. 2001, 137, 305–308. [Google Scholar]
- Elbendary, A.; Abdel-Halim, M.R.E.; Youssef, R.; Abdel Halim, D.; Elmasry, M.F.; Gad, A.; El Sharkawy, D.A. Hypopigmented lesions in pityriasis lichenoides chronica patients: Are they only post-inflammatory hypopigmentation? Australas. J. Dermatol. 2022, 63, 68–73. [Google Scholar] [CrossRef]
- Singh, Z.N.; Tretiakova, M.S.; Shea, C.R.; Petronic-Rosic, V.M. Decreased CD117 expression in hypopigmented mycosis fungoides correlates with hypomelanosis: Lessons learned from vitiligo. Mod. Pathol. 2006, 19, 1255–1260. [Google Scholar] [CrossRef]
- Seif El Nasr, H.; Shaker, O.G.; Fawzi, M.M.; El-Hanafi, G. Basic fibroblast growth factor and tumour necrosis factor alpha in vitiligo and other hypopigmented disorders: Suggestive possible therapeutic targets. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 103–108. [Google Scholar] [CrossRef]
- Khachemoune, A.; Blyumin, M.L. Pityriasis lichenoides: Pathophysiology, classification, and treatment. Am. J. Clin. Dermatol. 2007, 8, 29–36. [Google Scholar] [CrossRef]
- Clayton, R.; Warin, A. Pityriasis lichenoides chronica presenting as hypopigmentation. Br. J. Dermatol. 1979, 100, 297–302. [Google Scholar] [CrossRef]
- Ersoy-Evans, S.; Greco, M.F.; Mancini, A.J.; Subasi, N.; Paller, A.S. Pityriasis lichenoides in childhood: A retrospective review of 124 patients. J. Am. Acad. Dermatol. 2007, 56, 205–210. [Google Scholar] [CrossRef]
- Koh, W.L.; Koh, M.J.; Tay, Y.K. Pityriasis lichenoides in an Asian population. Int. J. Dermatol. 2013, 52, 1495–1499. [Google Scholar] [CrossRef]
- Onsun, N.; Kural, Y.; Su, O.; Demirkesen, C.; Buyukbabani, N. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr. Dermatol. 2006, 23, 493–496. [Google Scholar] [CrossRef]
- Rodney, I.J.; Kindred, C.; Angra, K.; Qutub, O.N.; Villanueva, A.R.; Halder, R.M. Hypopigmented mycosis fungoides: A retrospective clinicohistopathologic study. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 808–814. [Google Scholar] [CrossRef]
- Kanokrungsee, S.; Rajatanavin, N.; Rutnin, S.; Vachiramon, V. Efficacy of narrowband ultraviolet B twice weekly for hypopigmented mycosis fungoides in Asians. Clin. Exp. Dermatol. 2012, 37, 149–152. [Google Scholar] [CrossRef]
- Aydogan, K.; Saricaoglu, H.; Turan, H. Narrowband UVB (311 nm, TL01) phototherapy for pityriasis lichenoides. Photodermatol. Photoimmunol. Photomed. 2008, 24, 128–133. [Google Scholar] [CrossRef]
- Myers, E.; Kheradmand, S.; Miller, R. An Update on Narrowband Ultraviolet B Therapy for the Treatment of Skin Diseases. Cureus 2021, 13, e19182. [Google Scholar] [CrossRef]
- Bellinato, F.; Maurelli, M.; Gisondi, P.; Girolomoni, G. A systematic review of treatments for pityriasis lichenoides. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2039–2049. [Google Scholar] [CrossRef]
- Longley, J.; Demar, L.; Feinstein, R.P.; Miller, R.L.; Silvers, D.N. Clinical and histologic features of pityriasis lichenoides et varioliformis acuta in children. Arch. Dermatol. 1987, 123, 1335–1339. [Google Scholar] [CrossRef]
- Wang, C.Q.F.; Akalu, Y.T.; Suarez-Farinas, M.; Gonzalez, J.; Mitsui, H.; Lowes, M.A.; Orlow, S.J.; Manga, P.; Krueger, J.G. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: Potential relevance to psoriasis. J. Investig. Dermatol. 2013, 133, 2741–2752. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Chen, J.; Lu, J.; Yi, L.; Tong, X.; Kang, L.; Pei, S.; Ouyang, Y.; Jiang, L.; Ding, Y.; et al. Roles of inflammation factors in melanogenesis (Review). Mol. Med. Rep. 2020, 21, 1421–1430. [Google Scholar] [CrossRef] [PubMed]
- Arif, T.; Fatima, R.; Sami, M. Extragenital lichen sclerosus: A comprehensive review. Australas. J. Dermatol. 2022. [CrossRef] [PubMed]
- Tran, D.A.; Tan, X.; Macri, C.J.; Goldstein, A.T.; Fu, S.W. Lichen Sclerosus: An autoimmunopathogenic and genomic enigma with emerging genetic and immune targets. Int. J. Biol. Sci. 2019, 15, 1429–1439. [Google Scholar] [CrossRef] [PubMed]
- Chan, I. The role of extracellular matrix protein 1 in human skin. Clin. Exp. Dermatol. 2004, 29, 52–56. [Google Scholar] [CrossRef]
- Oyama, N.; Merregaert, J. The Extracellular Matrix Protein 1 (ECM1) in Molecular-Based Skin Biology. In Textbook of Aging Skin; Farage, M.A., Miller, K.W., Maibach, H.I., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 91–110. [Google Scholar]
- Carlson, J.A.; Grabowski, R.; Mu, X.C.; Del Rosario, A.; Malfetano, J.; Slominski, A. Possible mechanisms of hypopigmentation in lichen sclerosus. Am. J. Dermatopathol. 2002, 24, 97–107. [Google Scholar] [CrossRef]
- Farrell, A.M.; Dean, D.; Millard, P.R.; Charnock, F.M.; Wojnarowska, F. Cytokine alterations in lichen sclerosus: An immunohistochemical study. Br. J. Dermatol. 2006, 155, 931–940. [Google Scholar] [CrossRef]
- Carlson, J.A.; Mihm, M.C. Vulvar nevi, lichen sclerosus et atrophicus, and vitiligo. Arch. Dermatol. 1997, 133, 1314–1316. [Google Scholar]
- Regauer, S.; Liegl, B.; Reich, O. Early vulvar lichen sclerosus: A histopathological challenge. Histopathology 2005, 47, 340–347. [Google Scholar] [CrossRef]
- Burshtein, A.; Burshtein, J.; Rekhtman, S. Extragenital lichen sclerosus: A comprehensive review of clinical features and treatment. Arch. Dermatol. Res. 2022. [Google Scholar] [CrossRef]
- Meffert, J.J.; Davis, B.M.; Grimwood, R.E. Lichen sclerosus. J. Am. Acad. Dermatol. 1995, 32, 393–416; quiz 417–398. [Google Scholar] [CrossRef]
- Libow, L.F.; Coots, N.V. Lichen sclerosus following the lines of Blaschko. J. Am. Acad. Dermatol. 1998, 38, 831–833. [Google Scholar] [CrossRef]
- Neill, S.M.; Lewis, F.M.; Tatnall, F.M.; Cox, N.H. British Association of Dermatologists’ guidelines for the management of lichen sclerosus 2010. Br. J. Dermatol. 2010, 163, 672–682. [Google Scholar] [CrossRef]
- Coondoo, A.; Phiske, M.; Verma, S.; Lahiri, K. Side-effects of topical steroids: A long overdue revisit. Indian Dermatol. Online J. 2014, 5, 416–425. [Google Scholar] [CrossRef]
- Venkatesan, P.; Fangman, W.L. Linear hypopigmentation and cutaneous atrophy following intra-articular steroid injections for de Quervain’s tendonitis. J. Drugs Dermatol. 2009, 8, 492–493. [Google Scholar]
- Kim, Y.J.; Kang, H.Y. Pigmentation after using topical tacrolimus to treat lichen sclerosus: Possible role of stem cell factor. J. Am. Acad. Dermatol. 2007, 57 (Suppl. 5), S125–S127. [Google Scholar] [CrossRef]
- Kreuter, A.; Gambichler, T.; Avermaete, A.; Happe, M.; Bacharach-Buhles, M.; Hoffmann, K.; Jansen, T.; Altmeyer, P.; von Kobyletzki, G. Low-dose ultraviolet A1 phototherapy for extragenital lichen sclerosus: Results of a preliminary study. J. Am. Acad. Dermatol. 2002, 46, 251–255. [Google Scholar] [CrossRef]
- Abdel-Naser, M.B.; Seltmann, H.; Altenburg, A.; Zouboulis, C.C. Endothelins and alpha-melanocyte-stimulating hormone are increased in plasma of patients treated with UVA1 and psoralen plus UVA. Photodermatol. Photoimmunol. Photomed. 2022, 38, 611–613. [Google Scholar] [CrossRef]
- Bohm, M.; Wolff, I.; Scholzen, T.E.; Robinson, S.J.; Healy, E.; Luger, T.A.; Schwarz, T.; Schwarz, A. α-Melanocyte-stimulating hormone protects from ultraviolet radiation-induced apoptosis and DNA damage. J. Biol. Chem. 2005, 280, 5795–5802. [Google Scholar] [CrossRef] [Green Version]
- McDowell, A.; McLaughlin, J.; Layton, A.M. Is Cutibacterium (previously Propionibacterium) acnes a potential pathogenic factor in the aetiology of the skin disease progressive macular hypomelanosis? J. Eur. Acad. Dermatol. Venereol. 2021, 35, 338–344. [Google Scholar] [CrossRef]
- Neynaber, S.; Kirschner, C.; Kamann, S.; Plewig, G.; Flaig, M.J. Progressive macular hypomelanosis: A rarely diagnosed hypopigmentation in Caucasians. Dermatol. Res. Pract. 2009, 2009, 607682. [Google Scholar] [CrossRef] [PubMed]
- Barnard, E.; Liu, J.; Yankova, E.; Cavalcanti, S.M.; Magalhaes, M.; Li, H.; Patrick, S.; McDowell, A. Strains of the Propionibacterium acnes type III lineage are associated with the skin condition progressive macular hypomelanosis. Sci. Rep. 2016, 6, 31968. [Google Scholar] [CrossRef] [PubMed]
- Westerhof, W.; Relyveld, G.N.; Kingswijk, M.M.; de Man, P.; Menke, H.E. Propionibacterium acnes and the pathogenesis of progressive macular hypomelanosis. Arch. Dermatol. 2004, 140, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.; Palmer, M. Characterization of Streptococcus agalactiae CAMP factor as a pore-forming toxin. J. Biol. Chem. 2003, 278, 38167–38173. [Google Scholar] [CrossRef]
- Farrar, M.D.; Ingham, E.; Holland, K.T. Heat shock proteins and inflammatory acne vulgaris: Molecular cloning, overexpression and purification of a propionibacterium acnes GroEL and DnaK homologue. FEMS Microbiol. Lett. 2000, 191, 183–186. [Google Scholar] [CrossRef]
- Relyveld, G.N.; Menke, H.E.; Westerhof, W. Progressive macular hypomelanosis: An overview. Am. J. Clin. Dermatol. 2007, 8, 13–19. [Google Scholar] [CrossRef]
- Kuznetsov, A.V.; Flaig, M.J.; Ruzicka, T.; Herzinger, T. Progressive macular hypomelanosis Guillet-Helenon: Structural and immunohistochemical findings. J. Clin. Pathol. 2011, 64, 734–736. [Google Scholar] [CrossRef]
- Weedon, D. Weedon’s Skin Pathology, 3rd ed.; Churchill Livingstone Elsevier: London, UK, 2009. [Google Scholar]
- Relyveld, G.N.; Dingemans, K.P.; Menke, H.E.; Bos, J.D.; Westerhof, W. Ultrastructural findings in progressive macular hypomelanosis indicate decreased melanin production. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 568–574. [Google Scholar] [CrossRef]
- Selim, M.K.; Ahmed, E.S.F.; Abdelgawad, M.M.; El-Kamel, M.F. Progressive macular hypomelanosis among Egyptian patients: A clinicopathological study. Dermatol. Pract. Concept. 2011, 1, 5–11. [Google Scholar] [CrossRef] [Green Version]
- Hassan, A.M.; El-Badawi, M.A.; Abd-Rabbou, F.A.; Gamei, M.M.; Moustafa, K.A.; Almokadem, A.H. Progressive macular hypomelanosis pathogenesis and treatment: A randomized clinical trial. J. Microsc. Ultrastruct. 2014, 2, 205–216. [Google Scholar] [CrossRef]
- Leonard, N.; Krueger, S.; Rashighi, M. Successful treatment of progressive macular hypomelanosis. Dermatol. Rep. 2020, 12, 8509. [Google Scholar] [CrossRef]
- Guillet, G.; Helenon, R.; Gauthier, Y.; Surleve-Bazeille, J.E.; Plantin, P.; Sassolas, B. Progressive macular hypomelanosis of the trunk: Primary acquired hypopigmentation. J. Cutan. Pathol. 1988, 15, 286–289. [Google Scholar] [CrossRef]
- Relyveld, G.N.; Kingswijk, M.M.; Reitsma, J.B.; Menke, H.E.; Bos, J.D.; Westerhof, W. Benzoyl peroxide/clindamycin/UVA is more effective than fluticasone/UVA in progressive macular hypomelanosis: A randomized study. J. Am. Acad. Dermatol. 2006, 55, 836–843. [Google Scholar] [CrossRef]
- Fluhr, J.W.; Gloor, M. The antimicrobial effect of narrow-band UVB (313 nm) and UVA1 (345–440 nm) radiation in vitro. Photodermatol. Photoimmunol. Photomed. 1997, 13, 197–201. [Google Scholar] [CrossRef]
- Kanwar, A.J.; Dogra, S.; Parsad, D.; Kumar, B. Narrow-band UVB for the treatment of vitiligo: An emerging effective and well-tolerated therapy. Int. J. Dermatol. 2005, 44, 57–60. [Google Scholar] [CrossRef]
- Thng, S.T.; Long, V.S.; Chuah, S.Y.; Tan, V.W. Efficacy and relapse rates of different treatment modalities for progressive macular hypomelanosis. Indian J. Dermatol. Venereol. Leprol. 2016, 82, 673–676. [Google Scholar] [CrossRef]
- Sim, J.H.; Lee, D.J.; Lee, J.S.; Kim, Y.C. Comparison of the clinical efficacy of NBUVB and NBUVB with benzoyl peroxide/clindamycin in progressive macular hypomelanosis. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 1318–1323. [Google Scholar] [CrossRef]
- Ferreli, C.; Gasparini, G.; Parodi, A.; Cozzani, E.; Rongioletti, F.; Atzori, L. Cutaneous Manifestations of Scleroderma and Scleroderma-Like Disorders: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2017, 53, 306–336. [Google Scholar] [CrossRef]
- De Villiers, W.J.; Jordaan, H.F.; Bates, W. Systemic sclerosis sine scleroderma presenting with vitiligo-like depigmentation and interstitial pulmonary fibrosis. Clin. Exp. Dermatol. 1992, 17, 127–131. [Google Scholar] [CrossRef]
- Sung, J.J.; Chen, T.S.; Gilliam, A.C.; McCalmont, T.; Gilliam, A.E. Clinicohistopathological correlations in juvenile localized scleroderma: Studies on a subset of children with hypopigmented juvenile localized scleroderma due to loss of epidermal melanocytes. J. Am. Acad. Dermatol. 2011, 65, 364–373. [Google Scholar] [CrossRef]
- Rai, V.M.; Balachandran, C. Pseudovitiligo in Systemic Sclerosis. Dermatol. Online J. 2005, 11, 41. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.K.; Mondal, S. Sparing phenomenon in salt and pepper pigmentation of systemic sclerosis: An unusual observation. Clin. Exp. Dermatol. 2022, 47, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Lu, L. Salt-and-pepper appearance with supravenous pigment retention in systemic sclerosis. Clin. Exp. Dermatol. 2022, 47, 1359–1360. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, J.L.; Vazquez, M.; Sanchez, N.P. Vitiligolike macules in systemic scleroderma. Arch. Dermatol. 1983, 119, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Ee, H.L.; Tan, S.H. Reticulate hyperpigmented scleroderma: A new pigmentary manifestation. Clin. Exp. Dermatol. 2005, 30, 131–133. [Google Scholar] [CrossRef]
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef]
- Freiman, A.; Khanna, M.; Muhn, C.Y.; Billick, R.C. Ultraviolet autorepigmentation in scleroderma. J. Am. Acad. Dermatol. 2003, 49, 960–961. [Google Scholar] [CrossRef]
- Hassani, J.; Feldman, S.R. Phototherapy in Scleroderma. Dermatol. Ther. 2016, 6, 519–553. [Google Scholar] [CrossRef]
- Falabella, R.; Barona, M.I. Update on skin repigmentation therapies in vitiligo. Pigment. Cell Melanoma Res. 2009, 22, 42–65. [Google Scholar] [CrossRef]
- Kahn, J.S.; Deverapalli, S.C.; Rosmarin, D.M. JAK-STAT signaling pathway inhibition: A role for treatment of discoid lupus erythematosus and dermatomyositis. Int. J. Dermatol. 2018, 57, 1007–1014. [Google Scholar] [CrossRef]
- Joseph, A.K.; Abbas, L.F.; Chong, B.F. Treatments for disease damage in cutaneous lupus erythematosus: A narrative review. Dermatol. Ther. 2021, 34, e15034. [Google Scholar] [CrossRef]
- McDaniel, B.; Sukumaran, S.; Koritala, T.; Tanner, L.S. Discoid Lupus Erythematosus. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Lu, Q.; Long, H.; Chow, S.; Hidayat, S.; Danarti, R.; Listiawan, Y.; Deng, D.; Guo, Q.; Fang, H.; Tao, J.; et al. Guideline for the diagnosis, treatment and long-term management of cutaneous lupus erythematosus. J. Autoimmun. 2021, 123, 102707. [Google Scholar] [CrossRef]
- Rerknimitr, P.; Tekacharin, N.; Panchaprateep, R.; Wititsuwannakul, J.; Tangtanatakul, P.; Hirankarn, N.; Asawanonda, P. Pulsed-dye laser as an adjuvant treatment for discoid lupus erythematosus: A randomized, controlled trial. J. Dermatolog. Treat. 2019, 30, 81–86. [Google Scholar] [CrossRef]
- Gupta, S. Epidermal grafting for depigmentation due to discoid lupus erythematosus. Dermatology 2001, 202, 320–323. [Google Scholar] [CrossRef]
- Gupta, A.K.; Bluhm, R.; Summerbell, R. Pityriasis versicolor. J. Eur. Acad. Dermatol. Venereol. 2002, 16, 19–33. [Google Scholar] [CrossRef]
- Thoma, W.; Kramer, H.J.; Mayser, P. Pityriasis versicolor alba. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 147–152. [Google Scholar] [CrossRef]
- De Luca, C.; Picardo, M.; Breathnach, A.; Passi, S. Lipoperoxidase activity of Pityrosporum: Characterisation of by-products and possible role in pityriasis versicolor. Exp. Dermatol. 1996, 5, 49–56. [Google Scholar] [CrossRef]
- Nazzaro-Porro, M.; Passi, S. Identification of tyrosinase inhibitors in cultures of Pityrosporum. J. Investig. Dermatol. 1978, 71, 205–208. [Google Scholar] [CrossRef]
- Schallreuter, K.U.; Wood, J.W. A possible mechanism of action for azelaic acid in the human epidermis. Arch. Dermatol. Res. 1990, 282, 168–171. [Google Scholar] [CrossRef]
- Kramer, H.J.; Podobinska, M.; Bartsch, A.; Battmann, A.; Thoma, W.; Bernd, A.; Kummer, W.; Irlinger, B.; Steglich, W.; Mayser, P. Malassezin, a novel agonist of the aryl hydrocarbon receptor from the yeast Malassezia furfur, induces apoptosis in primary human melanocytes. Chembiochem 2005, 6, 860–865. [Google Scholar] [CrossRef]
- Savin, R. Diagnosis and treatment of tinea versicolor. J. Fam. Pract. 1996, 43, 127–132. [Google Scholar] [PubMed]
- Chopra, V.; Jain, V.K. Comparative study of topical terbinafine and topical ketoconazole in pityriasis versicolor. Indian J. Dermatol. Venereol. Leprol. 2000, 66, 299–300. [Google Scholar] [PubMed]
- Shi, T.W.; Zhang, J.A.; Tang, Y.B.; Yu, H.X.; Li, Z.G.; Yu, J.B. A randomized controlled trial of combination treatment with ketoconazole 2% cream and adapalene 0.1% gel in pityriasis versicolor. J. Dermatolog. Treat. 2015, 26, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Lyons, D.C. Pityriasis versicolor: An update on pharmacological treatment options. Expert Opin Pharmacother. 2014, 15, 1707–1713. [Google Scholar] [CrossRef]
- Cam, V.T.; Van, T.N.; Hau, K.T.; Huu, D.L.; Minh, P.P.T.; Huu, S.N.; Minh, T.N.; Gandolfi, M.; Satolli, F.; Feliciani, C.; et al. Efficacy of Azole Antifungal in Treatment of Pityriasis Versicolor. Open Access Maced. J. Med. Sci. 2019, 7, 272–274. [Google Scholar] [CrossRef]
- Eyer-Silva, W.A.; Martins, C.J.; Silva, G.; Acakpovi, G.; Pinto, J. Secondary syphilis presenting as leucoderma syphiliticum: Case report and review. Rev. Inst. Med. Trop. São Paulo 2017, 59, e74. [Google Scholar] [CrossRef]
- Poulsen, A.; Secher, L.; Kobayasi, T.; Weismann, K. Treponema pallidum in leukoderma syphiliticum demonstrated by electron microscopy. Acta Derm. Venereol. 1988, 68, 102–106. [Google Scholar]
- Pandhi, R.K.; Bedi, T.R.; Bhutani, L.K. Leucoderma in early syphilis. Br. J. Vener. Dis. 1977, 53, 19–22. [Google Scholar] [CrossRef]
- Miranda, M.F.; Bittencourt, M.d.J.S.; Lopes, I.d.C.; Cumino, S.s.S.M. Leucoderma syphiliticum: A rare expression of the secondary stage diagnosed by histopathology. An. Bras. Dermatol. 2010, 85, 512–515. [Google Scholar] [CrossRef]
- Little, E.G.G. Case of Leucoderma Syphiliticum. Proc. R. Soc. Med. 1911, 4, 102–103. [Google Scholar] [CrossRef] [Green Version]
- McDonagh, J.E.R. Case of Leucoderma Syphiliticum. Proc. R. Soc. Med. 1910, 3, 114. [Google Scholar] [CrossRef]
- Gade, A.; Matin, T.; Rubenstein, R.; Robinson, C.A. Acrodermatitis Chronica Atrophicans. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Silberer, M.; Koszik, F.; Stingl, G.; Aberer, E. Downregulation of class II molecules on epidermal Langerhans cells in Lyme borreliosis. Br. J. Dermatol. 2000, 143, 786–794. [Google Scholar] [CrossRef]
- Steere, A.C.; Strle, F.; Wormser, G.P.; Hu, L.T.; Branda, J.A.; Hovius, J.W.; Li, X.; Mead, P.S. Lyme borreliosis. Nat. Rev. Dis. Prim. 2016, 2, 16090. [Google Scholar] [CrossRef]
- Kempf, W.; Kazakov, D.V.; Hubscher, E.; Gugerli, O.; Gerbig, A.W.; Schmid, R.; Palmedo, G.; Kutzner, H. Cutaneous borreliosis associated with T cell-predominant infiltrates: A diagnostic challenge. J. Am. Acad. Dermatol. 2015, 72, 683–689. [Google Scholar] [CrossRef]
- de Koning, J.; Tazelaar, D.J.; Hoogkamp-Korstanje, J.A.; Elema, J.D. Acrodermatitis chronica atrophicans: A light and electron microscopic study. J. Cutan. Pathol. 1995, 22, 23–32. [Google Scholar] [CrossRef]
- Parveen, N.; Leong, J.M. Identification of a candidate glycosaminoglycan-binding adhesin of the Lyme disease spirochete Borrelia burgdorferi. Mol. Microbiol. 2000, 35, 1220–1234. [Google Scholar] [CrossRef]
- Tee, S.I.; Martinez-Escaname, M.; Zuriel, D.; Fried, I.; Wolf, I.; Massone, C.; Cerroni, L. Acrodermatitis chronica atrophicans with pseudolymphomatous infiltrates. Am. J. Dermatopathol. 2013, 35, 338–342. [Google Scholar] [CrossRef]
- Buechner, S.A.; Rufli, T.; Erb, P. Acrodermatitis chronic atrophicans: A chronic T-cell-mediated immune reaction against Borrelia burgdorferi? Clinical, histologic, and immunohistochemical study of five cases. J. Am. Acad. Dermatol. 1993, 28, 399–405. [Google Scholar] [CrossRef]
- Brandt, F.C.; Ertas, B.; Falk, T.M.; Metze, D.; Boer-Auer, A. Histopathology and immunophenotype of acrodermatitis chronica atrophicans correlated with ospA and ospC genotypes of Borrelia species. J. Cutan. Pathol. 2015, 42, 674–692. [Google Scholar] [CrossRef]
- Flisiak, R.; Pancewicz, S. Diagnostics and treatment of Lyme borreliosis. Recommendations of Polish Society of Epidemiology and Infectious Diseases. Przegl. Epidemiol. 2008, 62, 193–199. [Google Scholar]
- Pancewicz, S.A.; Garlicki, A.M.; Moniuszko-Malinowska, A.; Zajkowska, J.; Kondrusik, M.; Grygorczuk, S.; Czupryna, P.; Dunaj, J. Diagnosis and treatment of tick-borne diseases recommendations of the Polish Society of Epidemiology and Infectious Diseases. Przegl. Epidemiol. 2015, 69, 309–316, 421–308. [Google Scholar] [PubMed]
- Moniuszko-Malinowska, A.; Czupryna, P.; Dunaj, J.; Pancewicz, S.; Garkowski, A.; Kondrusik, M.; Grygorczuk, S.; Zajkowska, J. Acrodermatitis chronica atrophicans: Various faces of the late form of Lyme borreliosis. Adv. Dermatol. Allergol./Postępy Dermatol. I Alergol. 2018, 35, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Fujii, K. New Therapies and Immunological Findings in Cutaneous T-Cell Lymphoma. Front. Oncol. 2018, 8, 198. [Google Scholar] [CrossRef] [PubMed]
- Blaizot, R.; Ouattara, E.; Fauconneau, A.; Beylot-Barry, M.; Pham-Ledard, A. Infectious events and associated risk factors in mycosis fungoides/Sezary syndrome: A retrospective cohort study. Br. J. Dermatol. 2018, 179, 1322–1328. [Google Scholar] [CrossRef]
- Slodownik, D.; Moshe, S.; Sprecher, E.; Goldberg, I. Occupational mycosis fungoides–a case series. Int. J. Dermatol. 2017, 56, 733–737. [Google Scholar] [CrossRef]
- Vaisanen, E.; Fu, Y.; Koskenmies, S.; Fyhrquist, N.; Wang, Y.; Keinonen, A.; Makisalo, H.; Vakeva, L.; Pitkanen, S.; Ranki, A.; et al. Cutavirus DNA in Malignant and Nonmalignant Skin of Cutaneous T-Cell Lymphoma and Organ Transplant Patients but Not of Healthy Adults. Clin. Infect. Dis. 2019, 68, 1904–1910. [Google Scholar] [CrossRef]
- Bergallo, M.; Dapra, V.; Fava, P.; Ponti, R.; Calvi, C.; Montanari, P.; Novelli, M.; Quaglino, P.; Galliano, I.; Fierro, M.T. DNA from Human Polyomaviruses, MWPyV, HPyV6, HPyV7, HPyV9 and HPyV12 in Cutaneous T-cell Lymphomas. Anticancer Res. 2018, 38, 4111–4114. [Google Scholar] [CrossRef]
- Cerroni, L. Mycosis fungoides-clinical and histopathologic features, differential diagnosis, and treatment. Semin. Cutan. Med. Surg. 2018, 37, 2–10. [Google Scholar] [CrossRef]
- Ryan, E.A.; Sanderson, K.V.; Bartak, P.; Samman, P.D. Can mycosis fungoides begin in the epidermis? A hypothesis. Br. J. Dermatol. 1973, 88, 419–429. [Google Scholar] [CrossRef]
- Aranha, J.; dos Anjos Cabeças, M.; Afonso, A.; Pereira, F. Mycosis fungoides bullosa. J. Eur. Acad. Dermatol. Venereol. 1997, 8, 46–50. [Google Scholar] [CrossRef]
- Price, N.M.; Fuks, Z.Y.; Hoffman, T.E. Hyperkeratotic and Verrucous Features of Mycosis Fungoides. Arch. Dermatol. 1977, 113, 57–60. [Google Scholar] [CrossRef]
- Camisa, C.; Aulisio, A. Pustular mycosis fungoides. Cutis 1994, 54, 202–204. [Google Scholar]
- Dominguez-Gomez, M.A.; Baldassarri-Ortego, L.F.; Morales-Sanchez, M.A. Hypopigmented mycosis fungoides: A 48-case retrospective series. Australas. J. Dermatol. 2021, 62, e419–e420. [Google Scholar] [CrossRef]
- Furlan, F.C.; Sanches, J.A. Hypopigmented mycosis fungoides: A review of its clinical features and pathophysiology. An. Bras. Dermatol. 2013, 88, 954–960. [Google Scholar] [CrossRef]
- Lambroza, E.; Cohen, S.R.; Phelps, R.; Lebwohl, M.; Braverman, I.M.; DiCostanzo, D. Hypopigmented variant of mycosis fungoides: Demography, histopathology, and treatment of seven cases. J. Am. Acad. Dermatol. 1995, 32, 987–993. [Google Scholar] [CrossRef]
- El-Shabrawi-Caelen, L.; Cerroni, L.; Medeiros, L.J.; McCalmont, T.H. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am. J. Surg. Pathol. 2002, 26, 450–457. [Google Scholar] [CrossRef]
- Breathnach, S.M.; Mckee, P.H.; Smith, N.P. Hypopigmented mycosis fungoides: Report of five cases with ultrastructural observations. Br. J. Dermatol. 1982, 106, 643–649. [Google Scholar] [CrossRef]
- Goldberg, D.J.; Schinella, R.S.; Kechijian, P. Hypopigmented mycosis fungoides. Speculations about the mechanism of hypopigmentation. Am. J. Dermatopathol. 1986, 8, 326–330. [Google Scholar] [CrossRef]
- Munoz-Gonzalez, H.; Molina-Ruiz, A.M.; Requena, L. Clinicopathologic Variants of Mycosis Fungoides. Actas Dermosifiliogr. 2017, 108, 192–208. [Google Scholar] [CrossRef]
- Martinez Villarreal, A.; Gantchev, J.; Lagace, F.; Barolet, A.; Sasseville, D.; Odum, N.; Charli-Joseph, Y.V.; Hernandez Salazar, A.; Litvinov, I.V. Hypopigmented Mycosis Fungoides: Loss of Pigmentation Reflects Antitumor Immune Response in Young Patients. Cancers 2020, 12, 2007. [Google Scholar] [CrossRef]
- Lovgren, M.L.; Scarisbrick, J.J. Update on skin directed therapies in mycosis fungoides. Chin. Clin. Oncol. 2019, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Jia, Q.; Tian, W.; Li, B.; Chen, W.; Zhang, W.; Xie, Y.; Cheng, N.; Chen, Q.; Xiao, J.; Zhang, Y.; et al. Transient Receptor Potential channels, TRPV1 and TRPA1 in melanocytes synergize UV-dependent and UV-independent melanogenesis. Br. J. Pharmacol. 2021, 178, 4646–4662. [Google Scholar] [CrossRef] [PubMed]
- Bashir, M.M.; Sharma, M.R.; Werth, V.P. UVB and proinflammatory cytokines synergistically activate TNF-alpha production in keratinocytes through enhanced gene transcription. J. Investig. Dermatol. 2009, 129, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Baadsgaard, O.; Wulf, H.C.; Wantzin, G.L.; Cooper, K.D. UVB and UVC, but not UVA, potently induce the appearance of T6- DR+ antigen-presenting cells in human epidermis. J. Investig. Dermatol. 1987, 89, 113–118. [Google Scholar] [CrossRef]
- Kim, Y.H.; Martinez, G.; Varghese, A.; Hoppe, R.T. Topical nitrogen mustard in the management of mycosis fungoides: Update of the Stanford experience. Arch. Dermatol. 2003, 139, 165–173. [Google Scholar] [CrossRef]
- Fulton, J.E., Jr.; Rahimi, A.D.; Mansoor, S.; Helton, P.; Shitabata, P. The treatment of hypopigmentation after skin resurfacing. Dermatol. Surg. 2004, 30, 95–101. [Google Scholar]
- Grimes, P.E.; Bhawan, J.; Kim, J.; Chiu, M.; Lask, G. Laser resurfacing-induced hypopigmentation: Histologic alterations and repigmentation with topical photochemotherapy. Dermatol. Surg. 2001, 27, 515–520. [Google Scholar] [CrossRef]
- Baugh, E.G.; Anagu, O.; Kelly, K.M. Laser Treatment of Hypopigmentation in Scars: A Review. Dermatol. Surg. 2022, 48, 201–206. [Google Scholar] [CrossRef]
- Burks, J.W.; Marascalco, J.; Clark, W.H., Jr. Half-Face Planing of Precancerous Skin after Five Years. An Evaluation. Arch. Dermatol. 1963, 88, 572–585. [Google Scholar] [CrossRef]
- Kligman, A.M.; Baker, T.J.; Gordon, H.L. Long-term histologic follow-up of phenol face peels. Plast. Reconstr. Surg. 1985, 75, 652–659. [Google Scholar] [CrossRef]
- Laws, R.A.; Finley, E.M.; McCollough, M.L.; Grabski, W.J. Alabaster skin after carbon dioxide laser resurfacing with histologic correlation. Dermatol. Surg. 1998, 24, 633–636. [Google Scholar] [CrossRef]
- Gupta, A.K.; Gover, M.D.; Nouri, K.; Taylor, S. The treatment of melasma: A review of clinical trials. J. Am. Acad. Dermatol. 2006, 55, 1048–1065. [Google Scholar] [CrossRef]
- Kwon, H.H.; Suh, D.H. Linear extensions of hypopigmentation as a side effect of topical corticosteroid application. Int. J. Dermatol. 2016, 55, e315–e317. [Google Scholar] [CrossRef]
- Damiani, G.; Finelli, R.; Kridin, K.; Pacifico, A.; Bragazzi, N.L.; Malagoli, P.; Fabbrocini, G.; Annunziata, M.; Grada, A.; Santus, P.; et al. Facial atopic dermatitis may be exacerbate by masks: Insights from a multicenter, teledermatology, prospective study during COVID-19 pandemic. Ital. J. Dermatol. Venereol. 2022, 157, 505–509. [Google Scholar] [CrossRef]
- Damiani, G.; Gironi, L.C.; Kridin, K.; Pacifico, A.; Buja, A.; Bragazzi, N.L.; Spalkowska, M.; Pigatto, P.D.M.; Santus, P.; Young Dermatologists Italian, N.; et al. Mask-induced Koebner phenomenon and its clinical phenotypes: A multicenter, real-life study focusing on 873 dermatological consultations during COVID-19 pandemics. Dermatol. Ther. 2021, 34, e14823. [Google Scholar] [CrossRef]
- Damiani, G.; Finelli, R.; Kridin, K.; Pacifico, A.; Buja, A.; Bragazzi, N.L.; Malagoli, P.; Savoia, P.; Gironi, L.C.; Grada, A.; et al. Masks trigger facial seborrheic dermatitis and psoriasis: Evidence from a multicenter, case-control study during COVID-19 pandemic. Ital. J. Dermatol. Venerol. 2022, 157, 419–423. [Google Scholar] [CrossRef]
- Hua, W.; Zuo, Y.; Wan, R.; Xiong, L.; Tang, J.; Zou, L.; Shu, X.; Li, L. Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermat. 2020, 83, 115–121. [Google Scholar] [CrossRef]
- Teo, W.L. The “Maskne” microbiome–pathophysiology and therapeutics. Int. J. Dermatol. 2021, 60, 799–809. [Google Scholar] [CrossRef]
- Damiani, G.; Gironi, L.C.; Pacifico, A.; Cristaudo, A.; Malagoli, P.; Allocco, F.; Bragazzi, N.L.; Linder, D.M.; Santus, P.; Buja, A.; et al. Masks use and facial dermatitis during COVID-19 outbreak: Is there a difference between CE and non-CE approved masks? Multi-center, real-life data from a large Italian cohort. Ital. J. Dermatol. Venerol. 2021, 156, 220–225. [Google Scholar] [CrossRef]
- Potter, K.; Konda, S.; Ren, V.Z.; Wang, A.L.; Srinivasan, A.; Chilukuri, S. Techniques for Optimizing Surgical Scars, Part 3: Erythema, Hyperpigmentation, and Hypopigmentation. Skinmed 2018, 16, 113–117. [Google Scholar]
- Carney, B.C.; McKesey, J.P.; Rosenthal, D.S.; Shupp, J.W. Treatment Strategies for Hypopigmentation in the Context of Burn Hypertrophic Scars. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1642. [Google Scholar] [CrossRef] [PubMed]
- Omi, T.; Yamashita, R.; Kawana, S.; Sato, S.; Naito, Z. Low Fluence Q-Switched Nd: YAG Laser Toning and Q-Switched Ruby Laser in the Treatment of Melasma: A Comparative Split-Face Ultrastructural Study. Laser Ther. 2012, 21, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Reszko, A.; Sukal, S.A.; Geronemus, R.G. Reversal of laser-induced hypopigmentation with a narrow-band UV-B light source in a patient with skin type VI. Dermatol. Surg. 2008, 34, 1423–1426. [Google Scholar] [PubMed]
- Mysore, V.; Anitha, B.; Hosthota, A. Successful treatment of laser induced hypopigmentation with narrowband ultraviolet B targeted phototherapy. J. Cutan. Aesthetic Surg. 2013, 6, 117–119. [Google Scholar]
- Gundogan, C.; Greve, B.; Hausser, I.; Raulin, C. Repigmentation of persistent laser-induced hypopigmentation after tattoo ablation with the excimer laser. Hautarzt 2004, 55, 549–552. [Google Scholar] [CrossRef]
- Tierney, E.P.; Hanke, C.W. Treatment of CO2 laser induced hypopigmentation with ablative fractionated laser resurfacing: Case report and review of the literature. J. Drugs Dermatol. 2010, 9, 1420–1426. [Google Scholar]
- Savory, S.A.; Agim, N.G.; Mao, R.; Peter, S.; Wang, C.; Maldonado, G.; Bearden Dietert, J.; Lieu, T.J.; Wang, C.; Pretzlaff, K.; et al. Reliability assessment and validation of the postacne hyperpigmentation index (PAHPI), a new instrument to measure postinflammatory hyperpigmentation from acne vulgaris. J. Am. Acad. Dermatol. 2014, 70, 108–114. [Google Scholar] [CrossRef]
- Taylor, S.C.; Arsonnaud, S.; Czernielewski, J. The Taylor Hyperpigmentation Scale: A new visual assessment tool for the evaluation of skin color and pigmentation. Cutis 2005, 76, 270–274. [Google Scholar]
- Pandya, A.G.; Hynan, L.S.; Bhore, R.; Riley, F.C.; Guevara, I.L.; Grimes, P.; Nordlund, J.J.; Rendon, M.; Taylor, S.; Gottschalk, R.W.; et al. Reliability assessment and validation of the Melasma Area and Severity Index (MASI) and a new modified MASI scoring method. J. Am. Acad. Dermatol. 2011, 64, 78–83.e2. [Google Scholar] [CrossRef]
- Feily, A. Vitiligo Extent Tensity Index (VETI) score: A new definition, assessment and treatment evaluation criteria in vitiligo. Dermatol. Pract. Concept. 2014, 4, 81–84. [Google Scholar] [CrossRef]
- Tey, H.L. Approach to hypopigmentation disorders in adults. Clin. Exp. Dermatol. 2010, 35, 829–834. [Google Scholar] [CrossRef]
- Tey, H.L. A practical classification of childhood hypopigmentation disorders. Acta Derm. Venereol. 2010, 90, 6–11. [Google Scholar] [CrossRef]
- Saleem, M.D.; Oussedik, E.; Picardo, M.; Schoch, J.J. Acquired disorders with hypopigmentation: A clinical approach to diagnosis and treatment. J. Am. Acad. Dermatol. 2019, 80, 1233–1250.e1210. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rao, M.; Young, K.; Jackson-Cowan, L.; Kourosh, A.; Theodosakis, N. Post-Inflammatory Hypopigmentation: Review of the Etiology, Clinical Manifestations, and Treatment Options. J. Clin. Med. 2023, 12, 1243. https://doi.org/10.3390/jcm12031243
Rao M, Young K, Jackson-Cowan L, Kourosh A, Theodosakis N. Post-Inflammatory Hypopigmentation: Review of the Etiology, Clinical Manifestations, and Treatment Options. Journal of Clinical Medicine. 2023; 12(3):1243. https://doi.org/10.3390/jcm12031243
Chicago/Turabian StyleRao, Medha, Katherine Young, Ladonya Jackson-Cowan, Arianne Kourosh, and Nicholas Theodosakis. 2023. "Post-Inflammatory Hypopigmentation: Review of the Etiology, Clinical Manifestations, and Treatment Options" Journal of Clinical Medicine 12, no. 3: 1243. https://doi.org/10.3390/jcm12031243





