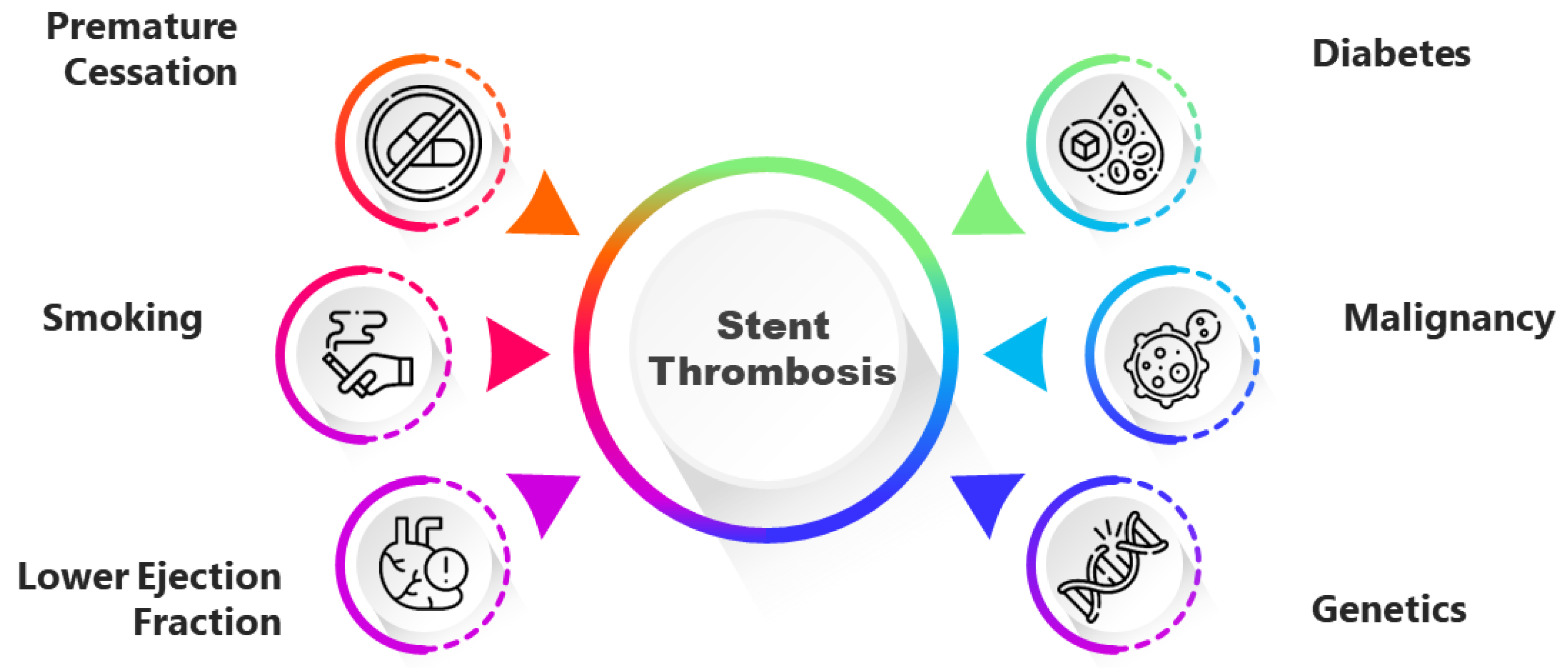
Patient-Related Factors Predicting Stent Thrombosis in Percutaneous Coronary Interventions
Abstract
:1. Introduction
2. Methods
3. Premature Cessation of Dual Antiplatelet Therapy
4. Percutaneous Coronary Intervention for Acute Coronary Syndrome
5. Smoking
6. Lower Ejection Fraction
7. Malignancy
8. Diabetes Mellitus
9. Clopidogrel Unresponsiveness
10. Genetics
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valgimigli, M.; Bueno, H.; Byrne, R.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar] [CrossRef] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.-A.; Steg, P.G.; Morel, M.-A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef] [PubMed]
- Al-Obaidi, F.R.; Hutchings, H.A.; Yong, A.S.; Alrubaiy, L.; Al-Farhan, H.; Al-Ali, M.H.; Al-Kinani, T.; Al-Myahi, M.; Al-Kenzawi, H.; Al-Sudani, N. Efficacy and Safety Outcomes of Short Duration Antiplatelet Therapy with Early Cessation of Aspirin Post Percutaneous Coronary Intervention: A Systematic Review and Meta-analysis. Curr. Cardiol. Rev. 2021, 17, e051121190712. [Google Scholar] [CrossRef]
- Valgimigli, M.; Frigoli, E.; Heg, D.; Tijssen, J.; Jüni, P.; Vranckx, P.; Ozaki, Y.; Morice, M.-C.; Chevalier, B.; Onuma, Y.; et al. Dual Antiplatelet Therapy after PCI in Patients at High Bleeding Risk. N. Engl. J. Med. 2021, 385, 1643–1655. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention 2019, 14, 1435–1534. [Google Scholar] [CrossRef] [PubMed]
- Kuramitsu, S.; Sonoda, S.; Ando, K.; Otake, H.; Natsuaki, M.; Anai, R.; Honda, Y.; Kadota, K.; Kobayashi, Y.; Kimura, T. Drug-eluting stent thrombosis: Current and future perspectives. Cardiovasc. Interv. Ther. 2021, 36, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Vogel, B.; Chandrasekhar, J.; Baber, U.; Mastoris, I.; Sartori, S.; Aquino, M.; Krucoff, M.W.; Moliterno, D.J.; Henry, T.D.; Weisz, G.; et al. Geographical Variations in Patterns of DAPT Cessation and Two-Year PCI Outcomes: Insights from the PARIS Registry. Arthritis Res. Ther. 2019, 119, 1704–1711. [Google Scholar] [CrossRef]
- Palmerini, T.; Della Riva, D.; Benedetto, U.; Reggiani, L.B.; Feres, F.; Abizaid, A.; Gilard, M.; Morice, M.-C.; Valgimigli, M.; Hong, M.-K.; et al. Three, six, or twelve months of dual antiplatelet therapy after DES implantation in patients with or without acute coronary syndromes: An individual patient data pairwise and network meta-analysis of six randomized trials and 11,473 patients. Eur. Heart J. 2017, 38, 1034–1043. [Google Scholar] [CrossRef]
- Zwart, B.; Godschalk, T.C.; Kelder, J.C.; Berg, J.M.T. High risk of stent thrombosis in the first 6 months after coronary stenting: Do not discontinue clopidogrel early after ACS. J. Interv. Cardiol. 2017, 30, 421–426. [Google Scholar] [CrossRef]
- Mazlan-Kepli, W.; Dawson, J.; Berry, C.; Walters, M. Cessation of dual antiplatelet therapy and cardiovascular events following acute coronary syndrome. Heart 2019, 105, 67–74. [Google Scholar] [CrossRef]
- Vranckx, P.; Valgimigli, M.; Jüni, P.; Hamm, C.; Steg, P.G.; Heg, D.; van Es, G.A.; McFadden, E.P.; Onuma, Y.; van Meijeren, C.; et al. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months after implantation of a drug-eluting stent: A multicentre, open-label, randomised superiority trial. Lancet 2018, 392, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Domei, T.; Morimoto, T.; Natsuaki, M.; Shiomi, H.; Toyota, T.; Ohya, M.; Suwa, S.; Takagi, K.; Nanasato, M.; et al. Effect of 1-Month Dual Antiplatelet Therapy Followed by Clopidogrel vs 12-Month Dual Antiplatelet Therapy on Cardiovascular and Bleeding Events in Patients Receiving PCI: The STOPDAPT-2 Randomized Clinical Tria. JAMA 2019, 321, 2414–2427. [Google Scholar] [CrossRef] [PubMed]
- Parfrey, S.; Abdelrahman, A.; Blackman, D.; Blaxill, J.M.; Cunnington, M.S.; Greenwood, J.P.; Malkin, C.J.; Mozid, A.M.; Rossington, J.A.; Veerasamy, M.; et al. Safety and efficacy of interrupting dual antiplatelet therapy one month following percutaneous coronary intervention: A meta-analysis of randomized controlled trials. BMC Cardiovasc. Disord. 2022, 22, 450. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, S.; Giustino, G.; Baber, U.; Sartori, S.; Cohen, D.J.; Henry, T.D.; Farhan, S.; Sharma, M.; Ariti, C.; Dangas, G.; et al. Dual Antiplatelet Therapy Cessation and Adverse Events after Drug-Eluting Stent Implantation in Patients at High Risk for Atherothrombosis (from the PARIS Registry). Am. J. Cardiol. 2018, 122, 1638–1646. [Google Scholar] [CrossRef]
- Sorrentino, S.; Sartori, S.; Baber, U.; Claessen, B.E.; Giustino, G.; Chandrasekhar, J.; Chandiramani, R.; Cohen, D.J.; Henry, T.D.; Guedeney, P.; et al. Bleeding Risk, Dual Antiplatelet Therapy Cessation, and Adverse Events after Percutaneous Coronary Intervention: The PARIS Registry. Circ. Cardiovasc. Interv. 2020, 13, e008226. [Google Scholar] [CrossRef] [PubMed]
- Baber, U.; Li, S.X.; Pinnelas, R.; Pocock, S.J.; Krucoff, M.W.; Ariti, C.; Gibson, C.M.; Steg, P.G.; Weisz, G.; Witzenbichler, B.; et al. Incidence, Patterns, and Impact of Dual Antiplatelet Therapy Cessation among Patients with and without Chronic Kidney Disease Undergoing Percutaneous Coronary Intervention: Results from the PARIS Registry (Patterns of Non-Adherence to Anti-Platelet Regimens in Stented Patients). Circ. Cardiovasc. Interv. 2018, 11, e006144. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, J.; Sartori, S.; Aquino, M.B.; Baber, U.; Hájek, P.; Atzev, B.; Hudec, M.; Ong, T.K.; Mates, M.; Borisov, B.; et al. Comparison of One-Year Outcomes in Patients >75 versus ≤75 Years with Coronary Artery Disease Treated with COMBO Stents (From The MASCOT Registry). Am. J. Cardiol. 2020, 127, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Joyce, L.C.; Baber, U.; Claessen, B.E.; Sartori, S.; Chandrasekhar, J.; Cohen, D.J.; Henry, T.D.; Ariti, C.; Dangas, G.; Faggioni, M.; et al. Dual-Antiplatelet Therapy Cessation and Cardiovascular Risk in Relation to Age: Analysis from the PARIS Registry. JACC Cardiovasc. Interv. 2019, 12, 983–992. [Google Scholar] [CrossRef]
- Kinlay, S.; Young, M.M.; Sherrod, R.; Gagnon, D.R. Long-Term Outcomes and Duration of Dual Antiplatelet Therapy after Coronary Intervention with Second-Generation Drug-Eluting Stents: The Veterans Affairs Extended DAPT Study. J. Am. Heart Assoc. 2023, 12, e027055. [Google Scholar] [CrossRef]
- Silva, J.S.N.; de Barros, I.M.L.; Cantarelli, F.L.; Alves, R.C.; Falcão, F.J.d.A.; Silva, J.M.d.S.; de Oliveira, F.R.A.; Pedrosa, R.P. Predictors of coronary stent thrombosis: A case–control study. J. Thromb. Thrombolysis 2018, 46, 420–426. [Google Scholar] [CrossRef]
- Vranken, N.P.A.; Rasoul, S.; Luijkx, J.J.P.; Pustjens, T.F.S.; Postma, S.; Kolkman, E.J.; Kedhi, E.; Rifqi, S.; Lee, M.K.Y.; Ebelt, H.; et al. Short-term dual antiplatelet therapy in diabetic patients admitted for acute coronary syndrome treated with a new-generation drug-eluting stent. Diabetes/Metab. Res. Rev. 2022, 38, e3530. [Google Scholar] [CrossRef] [PubMed]
- Katsikis, A.; Keeble, T.R.; Davies, J.R.; Jagathesan, R.; Kabir, A.; Sayer, J.W.; Robinson, N.M.; Kalogeropoulos, A.S.; Aggarwal, R.K.; Gamma, R.A.; et al. Contemporary management of stent thrombosis: Predictors of mortality and the role of new-generation drug-eluting stents. Catheter. Cardiovasc. Interv. 2020, 96, E8–E16. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Ammar, A.; Saghir, T.; Sial, J.A.; Shah, J.A.; Kumar, A.; Shaikh, A.H.; Achakzai, A.S.; Qamar, N.; Karim, M. Incidence, Predictors, and Outcomes of Acute and Sub-acute Stent Thrombosis after Emergency Percutaneous Coronary Revascularization with Drug-Eluting Stents: A Prospective Observational Study. Glob. Heart 2022, 17, 24. [Google Scholar] [CrossRef]
- Ozaki, Y.; Katagiri, Y.; Onuma, Y.; Amano, T.; Muramatsu, T.; Kozuma, K.; Otsuji, S.; Ueno, T.; Shiode, N.; Kawai, K.; et al. CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) in 2018. Cardiovasc. Interv. Ther. 2018, 33, 178–203. [Google Scholar] [CrossRef]
- Clemmensen, P.; Wiberg, S.; Hof, A.V.; Deliargyris, E.N.; Coste, P.; Berg, J.T.; Cavallini, C.; Hamon, M.; Dudek, D.; Zeymer, U.; et al. Acute stent thrombosis after primary percutaneous coronary intervention: Insights from the EUROMAX trial (European Ambulance Acute Coronary Syndrome Angiography). JACC Cardiovasc. Interv. 2015, 8, 214–220. [Google Scholar] [CrossRef]
- Nakano, M.; Yahagi, K.; Otsuka, F.; Sakakura, K.; Finn, A.V.; Kutys, R.; Ladich, E.; Fowler, D.R.; Joner, M.; Virmani, R. Causes of early stent thrombosis in patients presenting with acute coronary syndrome: An ex vivo human autopsy study. J. Am. Coll. Cardiol. 2014, 63, 2510–2520. [Google Scholar] [CrossRef] [PubMed]
- Claessen, B.E.; Henriques, J.P.; Jaffer, F.A.; Mehran, R.; Piek, J.J.; Dangas, G.D. Stent thrombosis: A clinical perspective. JACC Cardiovasc. Interv. 2014, 7, 1081–1092. [Google Scholar] [CrossRef]
- Kohsaka, S. Identification of Patient-Related Factors in Stent Thrombosis. Circ. J. 2020, 84, 1464–1466. [Google Scholar] [CrossRef]
- Mehran, R.; Baber, U.; Steg, P.G.; Ariti, C.; Weisz, G.; Witzenbichler, B.; Henry, T.D.; Kini, A.S.; Stuckey, T.; Cohen, D.J.; et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 2013, 382, 1714–1722. [Google Scholar] [CrossRef]
- Chichareon, P.; Modolo, R.; Collet, C.; Tenekecioglu, E.; Vink, M.A.; Oh, P.C.; Ahn, J.-M.; Musto, C.; de la Llera, L.S.D.; Cho, Y.-S.; et al. Efficacy and Safety of Stents in ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2019, 74, 2572–2584. [Google Scholar] [CrossRef]
- Yano, H.; Horinaka, S.; Watahiki, M.; Watanabe, T.; Ishimitsu, T. Five-year outcomes after first- and second-generation drug-eluting stent implantation in all patients undergoing percutaneous coronary intervention. J. Cardiol. 2019, 74, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Tariq, S.; Kumar, R.; Fatima, M.; Saghir, T.; Masood, S.; Karim, M. Acute and sub-acute stent thrombosis: Frequency, predictors and features in patients undergoing primary percutaneous intervention at a tertiary care cardiac centre. IJC Heart Vasc. 2020, 26, 100427. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Tariq, S.; Fatima, M.; Saghir, T.; Batra, M.K.; Karim, M.; Sial, J.A.; Khan, N.; Rizvi, S.N.H. Validity of the Stent Thrombosis Risk Score in Predicting Early Stent Thrombosis after Primary Percutaneous Coronary Intervention. J. Saudi Heart Assoc. 2020, 32, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Rashid, M.; So, D.Y.; Glover, C.A.; Froeschl, M.; Hibbert, B.; Chong, A.; Dick, A.; Labinaz, M.; Le May, M. Incidence, predictors, and clinical outcomes of early stent thrombosis in acute myocardial infarction patients treated with primary percutaneous coronary angioplasty (insights from the University of Ottawa Heart Institute STEMI registry). Catheter. Cardiovasc. Interv. 2018, 91, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.-X.; Liu, Y.; Li, X.-W.; Lu, P.-J.; Wang, J.; Li, C.-P.; Gao, J. Clinical outcomes after percutaneous coronary intervention for early versus late and very late stent thrombosis: A systematic review and meta-analysis. J. Thromb. Thrombolysis 2021, 51, 682–692. [Google Scholar] [CrossRef]
- Ramotowski, B.; Gurbel, P.A.; Tantry, U.; Bracha, J.S.; Karaźniewicz-Łada, M.; Lewandowski, Z.; Budaj, A. Effect of Smoking Cessation on the Pharmacokinetics and Pharmacodynamics of Clopidogrel after PCI: The Smoking Cessation Paradox Study. Thromb. Haemost. 2020, 120, 449–456. [Google Scholar] [CrossRef]
- Kim, Y.H.; Her, A.-Y.; Jeong, M.H.; Kim, B.-K.; Hong, S.-J.; Kim, S.; Ahn, C.-M.; Kim, J.-S.; Ko, Y.-G.; Choi, D.; et al. Sex difference after acute myocardial infarction patients with a history of current smoking and long-term clinical outcomes: Results of KAMIR Registry. Cardiol. J. 2022, 29, 954–965. [Google Scholar] [CrossRef]
- Tamis-Holland, J.E. Sex and Outcomes after Percutaneous Coronary Intervention: A Cause for Concern for Young Women and Those with ST-Segment Elevation Myocardial Infarction? J. Am. Heart Assoc. 2017, 6, e005739. [Google Scholar] [CrossRef]
- Kim, Y.H.; Her, A.-Y.; Jeong, M.H.; Kim, B.-K.; Hong, S.-J.; Lee, S.-J.; Ahn, C.-M.; Kim, J.-S.; Ko, Y.-G.; Choi, D.; et al. ST-segment elevation versus non-ST-segment elevation myocardial infarction in current smokers after newer-generation drug-eluting stent implantation. Medicine 2021, 100, e28214. [Google Scholar] [CrossRef]
- Kim, Y.H.; Her, A.-Y.; Jeong, M.H.; Kim, B.-K.; Hong, S.-J.; Shin, D.-H.; Kim, J.-S.; Ko, Y.-G.; Choi, D.; Hong, M.-K.; et al. Impact of current smoking on 2-year clinical outcomes between durable-polymer-coated stents and biodegradable-polymer-coated stents in acute myocardial infarction after successful percutaneous coronary intervention: Data from the KAMIR. PLoS ONE 2018, 13, e0205046. [Google Scholar] [CrossRef]
- Gupta, R.; Kirtane, A.J.; Liu, Y.; Crowley, A.; Witzenbichler, B.; Rinaldi, M.J.; Metzger, D.C.; Weisz, G.; Stuckey, T.D.; Brodie, B.R.; et al. Impact of Smoking on Platelet Reactivity and Clinical Outcomes after Percutaneous Coronary Intervention: Findings from the ADAPT-DES Study. Circ. Cardiovasc. Interv. 2019, 12, e007982. [Google Scholar] [CrossRef]
- Oh, S.; Kim, J.H.; Cho, K.H.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Ahn, Y.; Jeong, M.H. Association between baseline smoking status and clinical outcomes following myocardial infarction. Front. Cardiovasc. Med. 2022, 9, 918033. [Google Scholar] [CrossRef]
- Hazin, F.M.; Jamil, D.; Sharma, C.; Yasin, J.; Jamil, G.; Alkaabi, J. Re-catheterization in a young patient with acute myocardial infarction: Is it preventable? Am. J. Transl. Res. 2023, 15, 281–287. [Google Scholar] [PubMed]
- Elliott, J.; Kelly, S.E.; Bai, Z.; Skidmore, B.; Boucher, M.; So, D.; Wells, G.A. Extended dual antiplatelet therapy following percutaneous coronary intervention in clinically important patient subgroups: A systematic review and meta-analysis. CMAJ Open 2023, 11, E118–E130. [Google Scholar] [CrossRef] [PubMed]
- Franchin, L.; Kang, J.; De Filippo, O.; Gwon, H.-C.; Piroli, F.; Kim, H.-S.; Wańha, W.; Bin Song, Y.; Patti, G.; Hong, S.-J.; et al. Incidence and Predictors of Stent Thrombosis in Patients Treated with Stents for Coronary Bifurcation Narrowing (From the BIFURCAT Registry). Am. J. Cardiol. 2021, 156, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Yadav, M.; Mintz, G.S.; Généreux, P.; Liu, M.; McAndrew, T.; Redfors, B.; Madhavan, M.V.; Leon, M.B.; Stone, G.W. The Smoker’s Paradox Revisited: A Patient-Level Pooled Analysis of 18 Randomized Controlled Trials. JACC Cardiovasc. Interv. 2019, 12, 1941–1950. [Google Scholar] [CrossRef] [PubMed]
- Sardi, G.L.; Gaglia, M.A.; Maluenda, G.; Torguson, R.; Laynez-Carnicero, A.; Ben-Dor, I.; Hauville, C.; Xue, Z.; Suddath, W.O.; Kent, K.M.; et al. Outcome of Percutaneous Coronary Intervention Utilizing Drug-Eluting Stents in Patients with Reduced Left Ventricular Ejection Fraction. Am. J. Cardiol. 2012, 109, 344–351. [Google Scholar] [CrossRef]
- Yeh, R.W.; Secemsky, E.A.; Kereiakes, D.J.; Normand, S.-L.T.; Gershlick, A.H.; Cohen, D.J.; Spertus, J.A.; Steg, P.G.; Cutlip, D.E.; Rinaldi, M.J.; et al. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year after Percutaneous Coronary Intervention. JAMA 2016, 315, 1735–1749. [Google Scholar] [CrossRef] [PubMed]
- Iakovou, I.; Schmidt, T.; Bonizzoni, E.; Ge, L.; Sangiorgi, G.M.; Stankovic, G.; Airoldi, F.; Chieffo, A.; Montorfano, M.; Carlino, M.; et al. Incidence, Predictors, and Outcome of Thrombosis after Successful Implantation of Drug-Eluting Stents. JAMA 2005, 293, 2126–2130. [Google Scholar] [CrossRef]
- Chen, M.S.; John, J.M.; Chew, D.P.; Lee, D.S.; Ellis, S.G.; Bhatt, D.L. Bare metal stent restenosis is not a benign clinical entity. Am. Heart J. 2006, 151, 1260–1264. [Google Scholar] [CrossRef]
- Ullrich, H.; Münzel, T.; Gori, T. Coronary Stent Thrombosis—Predictors and Prevention. Dtsch. Aerzteblatt Online 2020, 117, 320–326. [Google Scholar] [CrossRef]
- Nusca, A.; Lipinski, M.J.; Varma, A.; Appleton, D.L.; Goudreau, E.; Cowley, M.J.; Wittkamp, M.J.; Di Sciascio, G.; Vetrovec, G.W.; Abbate, A. Safety of Drug-Eluting Stents in Patients with Left Ventricular Dysfunction Undergoing Percutaneous Coronary Intervention. Am. J. Cardiol. 2008, 102, 679–682. [Google Scholar] [CrossRef]
- Wisman, P.P.; Roest, M.; Asselbergs, F.W.; de Groot, P.; Moll, F.L.; van der Graaf, Y.; de Borst, G. Platelet-reactivity tests identify patients at risk of secondary cardiovascular events: A systematic review and meta-analysis. J. Thromb. Haemost. 2014, 12, 736–747. [Google Scholar] [CrossRef]
- Clarke, T.A.; Waskell, L.A. The Metabolism of Clopidogrel Is Catalyzed by Human Cytochrome P450 3A and Is Inhibited by Atorvastatin. Drug Metab. Dispos. 2003, 31, 53–59. [Google Scholar] [CrossRef]
- Sandek, A.; Swidsinski, A.; Schroedl, W.; Watson, A.; Valentova, M.; Herrmann, R.; Scherbakov, N.; Cramer, L.; Rauchhaus, M.; Grosse-Herrenthey, A.; et al. Intestinal Blood Flow in Patients with Chronic Heart Failure. J. Am. Coll. Cardiol. 2014, 64, 1092–1102. [Google Scholar] [CrossRef] [PubMed]
- Poelzl, G.; Ess, M.; Von der Heidt, A.; Rudnicki, M.; Frick, M.; Ulmer, H. Concomitant renal and hepatic dysfunctions in chronic heart failure: Clinical implications and prognostic significance. Eur. J. Intern. Med. 2013, 24, 177–182. [Google Scholar] [CrossRef]
- Cabrera-Cano, A.; Dávila-Borja, V.M.; Juárez-Méndez, S.; Marcial-Quino, J.; Gómez-Manzo, S.; Castillo-Rodríguez, R.A. Hypoxia as a modulator of cytochromes P450: Overexpression of the cytochromes CYP2S1 and CYP24A1 in human liver cancer cells in hypoxia. Cell Biochem. Funct. 2021, 39, 478–487. [Google Scholar] [CrossRef]
- Motovska, Z.; Ondrakova, M.; Doktorova, M.; Widimsky, P. Severe Left Ventricular Systolic Dysfunction is Independently Associated with High On-Clopidogrel Platelet Reactivity. Am. J. Cardiovasc. Drugs 2014, 14, 313–318. [Google Scholar] [CrossRef]
- Chau, K.H.; Kirtane, A.J.; Easterwood, R.M.; Redfors, B.; Zhang, Z.; Witzenbichler, B.; Weisz, G.; Stuckey, T.D.; Brodie, B.R.; Rinaldi, M.J.; et al. Stent Thrombosis Risk over Time on the Basis of Clinical Presentation and Platelet Reactivity. JACC Cardiovasc. Interv. 2021, 14, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Stähli, B.E.; Wischnewsky, M.B.; Jakob, P.; Klingenberg, R.; Obeid, S.; Heg, D.; Räber, L.; Windecker, S.; Roffi, M.; Mach, F.; et al. Predictive value of the age, creatinine, and ejection fraction (ACEF) score in patients with acute coronary syndromes. Int. J. Cardiol. 2018, 270, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, F.; Natsuaki, M.; Kuramitsu, S.; Ohya, M.; Otake, H.; Horie, K.; Yamanaka, F.; Shiomi, H.; Nakazawa, G.; Ando, K.; et al. Outcomes of Drug-Eluting Stent Thrombosis after Treatment for Acute versus Chronic Coronary Syndrome. JACC Cardiovasc. Interv. 2021, 14, 1082–1090. [Google Scholar] [CrossRef]
- Navi, B.B.; Reiner, A.S.; Kamel, H.; Iadecola, C.; Okin, P.M.; Elkind, M.S.; Panageas, K.S.; DeAngelis, L.M. Risk of Arterial Thromboembolism in Patients with Cancer. J. Am. Coll. Cardiol. 2017, 70, 926–938. [Google Scholar] [CrossRef]
- Falanga, A.; Le Gal, G.; Carrier, M.; Abdel-Razeq, H.; Ay, C.; Martin, A.J.M.; Rocha, A.T.C.; Agnelli, G.; Elalamy, I.; Brenner, B. Management of Cancer-Associated Thrombosis: Unmet Needs and Future Perspectives. TH Open 2021, 05, e376–e386. [Google Scholar] [CrossRef]
- Herrmann, J.; Yang, E.H.; Iliescu, C.A.; Cilingiroglu, M.; Charitakis, K.; Hakeem, A.; Toutouzas, K.; Leesar, M.A.; Grines, C.L.; Marmagkiolis, K.; et al. Vascular Toxicities of Cancer Therapies. Circulation 2016, 133, 1272–1289. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Cornell, R.F.; Lenihan, D.; Slosky, D.; Jagasia, M.; Piazza, G.; Moslehi, J. Cardiovascular Complications of Novel Multiple Myeloma Treatments. Circulation 2016, 133, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Douglas, G.; Van Kampen, E.; Hale, A.B.; McNeill, E.; Patel, J.; Crabtree, M.J.; Ali, Z.; Hoerr, R.A.; Alp, N.J.; Channon, K.M. Endothelial cell repopulation after stenting determines in-stent neointima formation: Effects of bare-metal vs. drug-eluting stents and genetic endothelial cell modification. Eur. Heart J. 2013, 34, 3378–3388. [Google Scholar] [CrossRef] [PubMed]
- Ramcharan, K.S.; Lip, G.Y.H.; Stonelake, P.S.; Blann, A.D. Effect of standard chemotherapy and antiangiogenic therapy on plasma markers and endothelial cells in colorectal cancer. Br. J. Cancer 2014, 111, 1742–1749. [Google Scholar] [CrossRef]
- Shoji, K.; Zen, K.; Ookura, T.; Yanishi, K.; Matoba, S. Early stent thrombosis confirmed in a cancer patient receiving regorafenib, despite triple antithrombotic therapy: A case report. BMC Cardiovasc. Disord. 2021, 21, 60. [Google Scholar] [CrossRef]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef]
- Liang, J.J.; Sio, T.T.; Slusser, J.P.; Lennon, R.J.; Miller, R.C.; Sandhu, G.; Prasad, A. Outcomes after Percutaneous Coronary Intervention with Stents in Patients Treated with Thoracic External Beam Radiation for Cancer. JACC Cardiovasc. Interv. 2014, 7, 1412–1420. [Google Scholar] [CrossRef]
- Gori, T.; Polimeni, A.; Indolfi, C.; Räber, L.; Adriaenssens, T.; Münzel, T. Predictors of stent thrombosis and their implications for clinical practice. Nat. Rev. Cardiol. 2019, 16, 243–256. [Google Scholar] [CrossRef]
- Gross, C.M.; Posch, M.G.; Geier, C.; Olthoff, H.; Krämer, J.; Dechend, R.; Dietz, R.; Özcelik, C. Subacute Coronary Stent Thrombosis in Cancer Patients. J. Am. Coll. Cardiol. 2008, 51, 1232–1233. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chen, X.; Sun, W.; Tian, T.; Zhou, S.; Zhang, Z.; Gao, M.; Qiao, B.; Zheng, Y. Very Late Stent Thrombosis in Drug-Eluting Stents New Observations and Clinical Implications. Cardiol. Rev. 2019, 27, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Fan, X.; Lewis, B.R.; Johnson, M.P.; Rihal, C.S.; Lerman, A.; Herrmann, J. Cancer Patients Have a Higher Risk of Thrombotic and Ischemic Events after Percutaneous Coronary Intervention. JACC Cardiovasc. Interv. 2021, 14, 1094–1105. [Google Scholar] [CrossRef]
- Garg, P.; Normand, S.L.; Silbaugh, T.S.; Wolf, R.E.; Zelevinsky, K.; Lovett, A.; Varma, M.R.; Zhou, Z.; Mauri, L. Drug-Eluting or Bare-Metal Stenting in Patients with Diabetes Mellitus. Circulation 2008, 118, 2277–2285. [Google Scholar] [CrossRef]
- Creager, M.A.; Lüscher, T.F.; Cosentino, F.; Beckman, J.A. Diabetes and Vascular Disease. Circulation 2003, 108, 1527–1532. [Google Scholar] [CrossRef] [PubMed]
- Biondi-Zoccai, G.G.; Abbate, A.; Liuzzo, G.; Biasucci, L.M. Atherothrombosis, inflammation, and diabetes. J. Am. Coll. Cardiol. 2003, 41, 1071–1077. [Google Scholar] [CrossRef]
- Arthur, J.F.; Jandeleit-Dahm, K.; Andrews, R.K. Platelet Hyperreactivity in Diabetes: Focus on GPVI Signaling—Are Useful Drugs Already Available? Diabetes 2017, 66, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Geisler, T.; Anders, N.; Paterok, M.; Langer, H.; Stellos, K.; Lindemann, S.; Herdeg, C.; May, A.E.; Gawaz, M. Platelet response to clopidogrel is attenuated in diabetic patients undergoing coronary stent implantation. Diabetes Care 2007, 30, 372–374. [Google Scholar] [CrossRef]
- Goraya, T.Y.; Leibson, C.L.; Palumbo, P.J.; A Weston, S.; Killian, J.M.; A Pfeifer, E.; Jacobsen, S.J.; Frye, R.L.; Roger, V.L. Coronary atherosclerosis in diabetes mellitus: A population-based autopsy study. J. Am. Coll. Cardiol. 2002, 40, 946–953. [Google Scholar] [CrossRef]
- Mak, K.-H.; Faxon, D.P. Clinical studies on coronary revascularization in patients with type 2 diabetes. Eur. Heart J. 2003, 24, 1087–1103. [Google Scholar] [CrossRef]
- Moreno, P.R.; Murcia, A.M.; Palacios, I.F.; Leon, M.N.; Bernardi, V.H.; Fuster, V.; Fallon, J.T. Coronary composition and macrophage infiltration in atherectomy specimens from patients with diabetes mellitus. Circulation 2000, 102, 2180–2184. [Google Scholar] [CrossRef] [PubMed]
- Abacı, A.; Oguzhan, A.; Kahraman, S.; Eryol, N.K.; Ünal, S.; Arınç, H.; Ergin, A. Effect of diabetes mellitus on formation of coronary collateral vessels. Circulation 1999, 99, 2239–2242. [Google Scholar] [CrossRef] [PubMed]
- Vavuranakis, M.; Stefanadis, C.; Toutouzas, K.; Pitsavos, C.; Spanos, V.; Toutouzas, P. Impaired compensatory coronary artery enlargement in atherosclerosis contributes to the development of coronary artery stenosis in diabetic patients. An in vivo intravascular ultrasound study. Eur. Heart J. 1997, 18, 1090–1094. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, T.; Joner, M.; Godschalk, T.C.; Malik, N.; Alfonso, F.; Xhepa, E.; De Cock, D.; Komukai, K.; Tada, T.; Cuesta, J.; et al. Optical Coherence Tomography Findings in Patients with Coronary Stent Thrombosis. Circulation 2017, 136, 1007–1021. [Google Scholar] [CrossRef] [PubMed]
- Franzone, A.; Pilgrim, T.; Heg, D.; Roffi, M.; Tüller, D.; Vuilliomenet, A.; Muller, O.; Cook, S.; Weilenmann, D.; Kaiser, C.; et al. Clinical Outcomes According to Diabetic Status in Patients Treated with Biodegradable Polymer Sirolimus-Eluting Stents Versus Durable Polymer Everolimus-Eluting Stents. Circ. Cardiovasc. Interv. 2015, 8, e002319. [Google Scholar] [CrossRef]
- Jensen, L.O.; Maeng, M.; Thayssen, P.; Kaltoft, A.; Tilsted, H.H.; Lassen, J.F.; Hansen, K.N.; Bottcher, M.; Rasmussen, K.; Madsen, M.; et al. Long-term outcomes after percutaneous coronary intervention in patients with and without diabetes mellitus in western denmark. Am. J. Cardiol. 2010, 105, 1513–1519. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.K.; Lotan, C.; Meredith, I.T.; Feres, F.; Zambahari, R.; Sinha, N.; Rothman, M.T.; for the E-Five Registry Investigators. Twelve-month outcomes in patients with diabetes implanted with a zotarolimus-eluting stent: Results from the E-Five Registry. Heart 2010, 96, 848–853. [Google Scholar] [CrossRef]
- Yuan, J.; Xu, G.M. Early and Late Stent Thrombosis in Patients with versus without Diabetes Mellitus Following Percutaneous Coronary Intervention with Drug-Eluting Stents: A Systematic Review and Meta-Analysis. Am. J. Cardiovasc. Drugs 2018, 18, 483–492. [Google Scholar] [CrossRef]
- Flaherty, J.D.; Davidson, C.J. Diabetes and Coronary Revascularization. JAMA 2005, 293, 1501–1508. [Google Scholar] [CrossRef]
- Nogic, J.; Nerlekar, N.; Soon, K.; Freeman, M.; Chan, J.; Roberts, L.; Brennan, A.; Dinh, D.; Lefkovits, J.; Brown, A.J. Diabetes mellitus is independently associated with early stent thrombosis in patients undergoing drug eluting stent implantation: Analysis from the Victorian cardiac outcomes registry. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2022, 99, 554–562. [Google Scholar] [CrossRef]
- Ouyang, H.; Zeng, X.; Zhang, C.; Song, L.; Xu, J.; Hou, Z.; Xie, S.; Tao, Z.; He, J. A meta-analysis of everolimus-eluting stents versus sirolimus-eluting stents and paclitaxel-eluting stents in diabetic patients. J. Cardiothorac. Surg. 2021, 16, 90. [Google Scholar] [CrossRef]
- Ploumen, E.H.; Pinxterhuis, T.H.; Zocca, P.; Roguin, A.; Anthonio, R.L.; Schotborgh, C.E.; Benit, E.; Aminian, A.; Danse, P.W.; Doggen, C.J.M.; et al. Impact of prediabetes and diabetes on 3-year outcome of patients treated with new-generation drug-eluting stents in two large-scale randomized clinical trials. Cardiovasc. Diabetol. 2021, 20, 217. [Google Scholar] [CrossRef]
- Martínez, G.J.; Robertson, S.; Barraclough, J.; Xia, Q.; Mallat, Z.; Bursill, C.; Celermajer, D.S.; Patel, S. Colchicine Acutely Suppresses Local Cardiac Production of Inflammatory Cytokines in Patients with an Acute Coronary Syndrome. J. Am. Heart Assoc. 2015, 4, e002128. [Google Scholar] [CrossRef]
- Tardif, J.-C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef]
- Yaseen, I.F.; Farhan, H.A.; Abbas, H.M. Clopidogrel non-responsiveness in patients undergoing percutaneous coronary intervention using the VerifyNow test: Frequency and predictors. Eur. J. Hosp. Pharm. 2019, 26, 113–116. [Google Scholar] [CrossRef]
- Westphal, E.S.; Aladeen, T.; Vanini, D.; Rainka, M.; McCadden, K.; Gengo, F.M.; Bates, V. Generic Clopidogrel: Has Substitution for Brand Name Plavix® Been Effective? J. Pharm. Pract. 2022, 35, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Alakbarzade, V.; Huang, X.; Ster, I.C.; McEntagart, M.; Pereira, A.C. High on-clopidogrel platelet reactivity in ischaemic stroke or transient ischaemic attack: Systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 2020, 29, 104877. [Google Scholar] [CrossRef] [PubMed]
- Dikshit, M.; Pandey, C.P.; Misra, A.; Negi, M.P.S.; Kanuri, B.N.; Chhonker, Y.S.; Bhatta, R.S.; Narain, V.S. Aspirin & clopidogrel non-responsiveness & its association with genetic polymorphisms in patients with myocardial infarction. Indian J. Med. Res. 2019, 150, 50–61. [Google Scholar] [CrossRef]
- Zhang, Z.; Chen, M.; Zhang, L.; Zhao, Q. The impact of cytochrome 450 and Paraoxonase polymorphisms on clopidogrel resistance and major adverse cardiac events in coronary heart disease patients after percutaneous coronary intervention. BMC Pharmacol. Toxicol. 2020, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Akram, N.; Mustafa, G.; A Hanif, A.; Tawwab, S.; Hussain, S.; Kaul, H.; Mohsin, S. Cytochrome 2C19 and paraoxonase-1 polymorphisms and clopidogrel resistance in ischemic heart disease patients. Pers. Med. 2019, 16, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Madan, M.; Abbott, J.D.; Lennon, R.; So, D.Y.F.; MacDougall, A.M.; McLaughlin, M.A.; Murthy, V.; Saw, J.; Rihal, C.; Farkouh, M.E.; et al. Sex-Specific Differences in Clinical Outcomes after Percutaneous Coronary Intervention: Insights from the TAILOR-PCI Trial. J. Am. Heart Assoc. 2022, 11, e024709. [Google Scholar] [CrossRef] [PubMed]
- Duconge, J.; Santiago, E.; Hernandez-Suarez, D.F.; Moneró, M.; López-Reyes, A.; Rosario, M.; Renta, J.Y.; González, P.; Fernández-Morales, L.I.; Vélez-Figueroa, L.A.; et al. Pharmacogenomic polygenic risk score for clopidogrel responsiveness among Caribbean Hispanics: A candidate gene approach. Clin. Transl. Sci. 2021, 14, 2254–2266. [Google Scholar] [CrossRef] [PubMed]
- Ezer, E.; Schrick, D.; Tőkés-Füzesi, M.; Szapary, L.; Bogar, L.; Molnar, T. A novel approach of platelet function test for prediction of attenuated response to clopidogrel. Clin. Hemorheol. Microcirc. 2019, 73, 359–369. [Google Scholar] [CrossRef]
- Cirillo, P.; Taglialatela, V.; Pellegrino, G.; Morello, A.; Conte, S.; Di Serafino, L.; Cimmino, G. Effects of colchicine on platelet aggregation in patients on dual antiplatelet therapy with aspirin and clopidogrel. J. Thromb. Thrombolysis 2020, 50, 468–472. [Google Scholar] [CrossRef]
- Fox, S.C.; May, J.A.; Dovlatova, N.; Glenn, J.R.; Johnson, A.; White, A.E.; Radhakrishnan, A.; Heptinstall, S. How does measurement of platelet P-selectin compare with other methods of measuring platelet function as a means of determining the effectiveness of antiplatelet therapy? Platelets 2019, 30, 290–295. [Google Scholar] [CrossRef]
- Ko, Y.M.; Kim, J.K.; Park, S.-H.; Choi, R.K. Comparison of antiplatelet treatment in patients with clopidogrel nonresponders with or without carriage of CYP2C19 polymorphism. Korean J. Intern. Med. 2018. ahead of print. [Google Scholar] [CrossRef]
- Sheng, X.; An, H.; He, Y.; Ye, Y.; Zhao, J.; Li, S. High-Dose Clopidogrel versus Ticagrelor in CYP2C19 intermediate or poor metabolizers after percutaneous coronary intervention: A Meta-Analysis of Randomized Trials. J. Clin. Pharm. Ther. 2022, 47, 1112–1121. [Google Scholar] [CrossRef]
- Al-Rubaish, A.M.; Al-Muhanna, F.A.; Alshehri, A.M.; Al-Mansori, M.A.; Alali, R.A.; Khalil, R.M.; Al Faraidy, K.A.; Cyrus, C.; Sulieman, M.M.; Vatte, C.; et al. Bedside testing of CYP2C19 gene for treatment of patients with PCI with antiplatelet therapy. BMC Cardiovasc. Disord. 2020, 20, 268. [Google Scholar] [CrossRef]
- Lyu, S.-Q.; Zhu, J.; Wang, J.; Wu, S.; Zhang, H.; Shao, X.-H.; Yang, Y.-M. Utility of a pharmacogenetic-driven algorithm in guiding dual antiplatelet therapy for patients undergoing coronary drug-eluting stent implantation in China. Eur. J. Clin. Pharmacol. 2022, 78, 215–225. [Google Scholar] [CrossRef]
- Parcha, V.; Heindl, B.F.; Li, P.; Kalra, R.; Limdi, N.A.; Pereira, N.L.; Arora, G.; Arora, P. Genotype-Guided P2Y12 Inhibitor Therapy after Percutaneous Coronary Intervention: A Bayesian Analysis. Circ. Genom. Precis. Med. 2021, 14, e003353. [Google Scholar] [CrossRef]
- Capodanno, D.; Angiolillo, D.J.; Lennon, R.J.; Goodman, S.G.; Kim, S.; O’Cochlain, F.; So, D.Y.; Sweeney, J.; Rihal, C.S.; Farkouh, M.; et al. ABCD-GENE Score and Clinical Outcomes Following Percutaneous Coronary Intervention: Insights from the TAILOR-PCI Trial. J. Am. Heart Assoc. 2022, 11, e024156. [Google Scholar] [CrossRef] [PubMed]
- Claassens, D.M.F.; Vos, G.J.; Bergmeijer, T.O.; Hermanides, R.S.; Hof, A.W.V. ’T.; Van Der Harst, P.; Barbato, E.; Morisco, C.; Gin, R.M.T.J.; Asselbergs, F.W.; et al. A Genotype-Guided Strategy for Oral P2Y12 Inhibitors in Primary PCI. N. Engl. J. Med. 2019, 381, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-L.; Fu, Y.; Qin, S.-B.; Liang, G.-K.; Liu, J.; Nie, X.-Y.; Chen, J.; Shi, L.-W.; Shao, H.; Lu, Y. Association between P2RY12 gene polymorphisms and adverse clinical events in coronary artery disease patients treated with clopidogrel: A systematic review and meta-analysis. Gene 2018, 657, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Zhu, K.-X.; Song, P.-Y.; Li, H.; Li, M.-P.; Du, Y.-X.; Ma, Q.-L.; Peng, L.-M.; Chen, X.-P. Association of FMO3 rs1736557 polymorphism with clopidogrel response in Chinese patients with coronary artery disease. Eur. J. Clin. Pharmacol. 2021, 77, 359–368. [Google Scholar] [CrossRef]
- Kessler, T.; Wolf, B.; Eriksson, N.; Kofink, D.; Mahmoodi, B.K.; Rai, H.; Tragante, V.; Åkerblom, A.; Becker, R.C.; Bernlochner, I.; et al. Association of the coronary artery disease risk gene GUCY1A3 with ischaemic events after coronary intervention. Cardiovasc. Res. 2019, 115, 1512–1518. [Google Scholar] [CrossRef]
| Stent Thrombosis Classification | Criteria | ||
|---|---|---|---|
| Stent type | Bare metal stents | First-generation drug-eluting stents (DES) | Second-generation drug-eluting stents (DES) |
| Event timing | Early stent thrombosis (within 24 h) | Late stent thrombosis (1 to 12 months) | Very late stent thrombosis (after 12 months) |
| Event certainty | Definite: ACS with angiographic or autopsy confirmation of ST | Probable:
| Possible: Unexplained death after 30 days of stent implantation without autopsy |
|
|
|
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anghel, L.; Tudurachi, B.-S.; Tudurachi, A.; Zăvoi, A.; Clement, A.; Roungos, A.; Benchea, L.-C.; Zota, I.M.; Prisacariu, C.; Sascău, R.A.; et al. Patient-Related Factors Predicting Stent Thrombosis in Percutaneous Coronary Interventions. J. Clin. Med. 2023, 12, 7367. https://doi.org/10.3390/jcm12237367
Anghel L, Tudurachi B-S, Tudurachi A, Zăvoi A, Clement A, Roungos A, Benchea L-C, Zota IM, Prisacariu C, Sascău RA, et al. Patient-Related Factors Predicting Stent Thrombosis in Percutaneous Coronary Interventions. Journal of Clinical Medicine. 2023; 12(23):7367. https://doi.org/10.3390/jcm12237367
Chicago/Turabian StyleAnghel, Larisa, Bogdan-Sorin Tudurachi, Andreea Tudurachi, Alexandra Zăvoi, Alexandra Clement, Alexandros Roungos, Laura-Cătălina Benchea, Ioana Mădălina Zota, Cristina Prisacariu, Radu Andy Sascău, and et al. 2023. "Patient-Related Factors Predicting Stent Thrombosis in Percutaneous Coronary Interventions" Journal of Clinical Medicine 12, no. 23: 7367. https://doi.org/10.3390/jcm12237367








