Pediatric Bone Marrow Failure: A Broad Landscape in Need of Personalized Management
Abstract
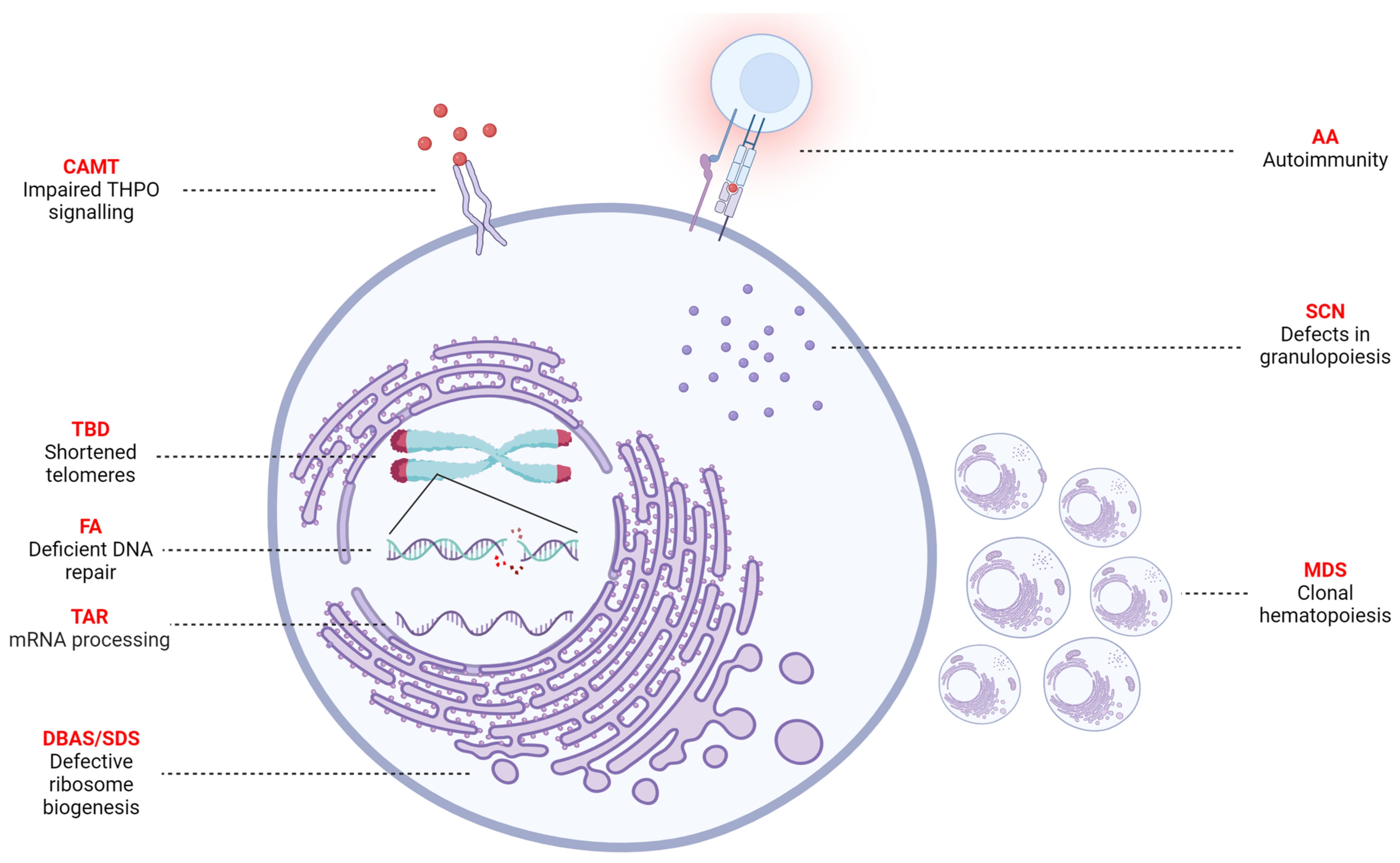
:1. Introduction
2. Hematological Stem Cell Transplantation: General Aspects
3. Inherited Bone Marrow Failure Syndrome
3.1. Fanconi Anemia
3.2. Telomere Biology Disorders (TBDs)
3.3. Diamond–Blackfan Anemia Syndrome
3.4. Shwachman–Diamond Syndrome
3.5. Severe Congenital Neutropenia
3.6. Congenital Amegakaryocytic Thrombocytopenia
3.7. Thrombocytopenia Absent Radii
4. (Idiopathic) Aplastic Anemia
4.1. Paroxysmal Nocturnal Hematuria
4.2. Treatment
5. Syndromes with a Malignant Predisposition
5.1. Myelodysplastic Syndrome
5.2. Other Germline Predisposition for MDS/AML
6. Gene Therapy as a Novel Treatment Strategy
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhatnagar, S.K.; Chandra, J.; Narayan, S.; Sharma, S.; Singh, V.; Dutta, A.K. Pancytopenia in children: Etiological profile. J. Trop. Pediatr. 2005, 51, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Erlacher, M.; Strahm, B. Missing Cells: Pathophysiology, Diagnosis, and Management of (Pan)Cytopenia in Childhood. Front. Pediatr. 2015, 3, 64. [Google Scholar] [CrossRef] [PubMed]
- Memon, S.; Shaikh, S.; Nizamani, M.A. Etiological spectrum of pancytopenia based on bone marrow examination in children. J. Coll. Physicians Surg. Pak. 2008, 18, 163–167. [Google Scholar] [PubMed]
- Dokal, I.; Tummala, H.; Vulliamy, T. Inherited bone marrow failure in the pediatric patient. Blood 2022, 140, 556–570. [Google Scholar] [PubMed]
- Furlong, E.; Carter, T. Aplastic anaemia: Current concepts in diagnosis and management. J. Paediatr. Child. Health 2020, 56, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Avagyan, S.; Shimamura, A. Lessons From Pediatric MDS: Approaches to Germline Predisposition to Hematologic Malignancies. Front. Oncol. 2022, 12, 813149. [Google Scholar] [CrossRef]
- Atmar, K.; Ruivenkamp, C.A.L.; Hooimeijer, L.; Nibbeling, E.A.R.; Eckhardt, C.L.; Huisman, E.J.; Lankester, A.C.; Bartels, M.; Santen, G.W.E.; Smiers, F.J.; et al. Diagnostic Value of a Protocolized In-Depth Evaluation of Pediatric Bone Marrow Failure: A Multi-Center Prospective Cohort Study. Front. Immunol. 2022, 13, 883826. [Google Scholar] [CrossRef]
- Bluteau, O.; Sebert, M.; Leblanc, T.; Peffault de Latour, R.; Quentin, S.; Lainey, E.; Hernandez, L.; Dalle, J.H.; Sicre de Fontbrune, F.; Lengline, E.; et al. A landscape of germ line mutations in a cohort of inherited bone marrow failure patients. Blood 2018, 131, 717–732. [Google Scholar] [CrossRef]
- Keel, S.B.; Scott, A.; Sanchez-Bonilla, M.; Ho, P.A.; Gulsuner, S.; Pritchard, C.C.; Abkowitz, J.L.; King, M.C.; Walsh, T.; Shimamura, A. Genetic features of myelodysplastic syndrome and aplastic anemia in pediatric and young adult patients. Haematologica 2016, 101, 1343–1350. [Google Scholar] [CrossRef]
- Alter, B.P.; Giri, N.; Savage, S.A.; Peters, J.A.; Loud, J.T.; Leathwood, L.; Carr, A.G.; Greene, M.H.; Rosenberg, P.S. Malignancies and survival patterns in the National Cancer Institute inherited bone marrow failure syndromes cohort study. Br. J. Haematol. 2010, 150, 179–188. [Google Scholar]
- Locatelli, F.; Strahm, B. How I treat myelodysplastic syndromes of childhood. Blood 2018, 131, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Giudice, V.; Feng, X.; Lin, Z.; Hu, W.; Zhang, F.; Qiao, W.; Ibanez, M.; Rios, O.; Young, N.S. Deep sequencing and flow cytometric characterization of expanded effector memory CD8+CD57+ T cells frequently reveals T-cell receptor Vβ oligoclonality and CDR3 homology in acquired aplastic anemia. Haematologica 2018, 103, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Pagliuca, S.; Gurnari, C.; Awada, H.; Kishtagari, A.; Kongkiatkamon, S.; Terkawi, L.; Zawit, M.; Guan, Y.; LaFramboise, T.; Jha, B.K.; et al. The similarity of class II HLA genotypes defines patterns of autoreactivity in idiopathic bone marrow failure disorders. Blood 2021, 138, 2781–2798. [Google Scholar] [CrossRef] [PubMed]
- Fassel, H.; Sheth, S. Bone Marrow Failure in Children: Approach to Diagnosis and Treatment. Indian. J. Pediatr. 2020, 87, 141–149. [Google Scholar] [CrossRef]
- Vissers, L.; van der Burg, M.; Lankester, A.; Smiers, F.; Mohseny, A. Optimizing diagnostic methods and stem cell transplantation outcomes in pediatric bone marrow failure: A 50-year single center experience. Eur. J. Pediatr. 2023, 182, 4195–4203. [Google Scholar] [CrossRef]
- Williams, L.; Cirrone, F.; Cole, K.; Abdul-Hay, M.; Luznik, L.; Al-Homsi, A.S. Post-transplantation Cyclophosphamide: From HLA-Haploidentical to Matched-Related and Matched-Unrelated Donor Blood and Marrow Transplantation. Front. Immunol. 2020, 11, 636. [Google Scholar] [CrossRef]
- Peffault de Latour, R.; Peters, C.; Gibson, B.; Strahm, B.; Lankester, A.; de Heredia, C.D.; Longoni, D.; Fioredda, F.; Locatelli, F.; Yaniv, I.; et al. Recommendations on hematopoietic stem cell transplantation for inherited bone marrow failure syndromes. Bone Marrow Transplant. 2015, 50, 1168–1172. [Google Scholar] [CrossRef]
- Fioredda, F.; Iacobelli, S.; van Biezen, A.; Gaspar, B.; Ancliff, P.; Donadieu, J.; Aljurf, M.; Peters, C.; Calvillo, M.; Matthes-Martin, S.; et al. Stem cell transplantation in severe congenital neutropenia: An analysis from the European Society for Blood and Marrow Transplantation. Blood 2015, 126, 1885–1892. [Google Scholar] [CrossRef]
- Peffault de Latour, R.; Purtill, D.; Ruggeri, A.; Sanz, G.; Michel, G.; Gandemer, V.; Maury, S.; Kurtzberg, J.; Bonfim, C.; Aljurf, M.; et al. Influence of nucleated cell dose on overall survival of unrelated cord blood transplantation for patients with severe acquired aplastic anemia: A study by eurocord and the aplastic anemia working party of the European group for blood and marrow transplantation. Biol. Blood Marrow Transpl. 2011, 17, 78–85. [Google Scholar]
- Chaudhry, Q.U.N.; Iftikhar, R.; Satti, T.M.; Mahmood, S.K.; Ghafoor, T.; Shamshad, G.U.; Farhan, M.; Shahbaz, N.; Khan, M.A.; Khattak, T.A.; et al. Outcome of Fludarabine-Based Conditioning in High-Risk Aplastic Anemia Patients Undergoing Matched Related Donor Transplantation: A Single-Center Study from Pakistan. Biol. Blood Marrow Transpl. 2019, 25, 2375–2382. [Google Scholar] [CrossRef]
- Höchsmann, B.; Moicean, A.; Risitano, A.; Ljungman, P.; Schrezenmeier, H.; EBMT Working Party on Aplastic Anemia. Supportive care in severe and very severe aplastic anemia. Bone Marrow Transplant. 2013, 48, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Champlin, R.E.; Horowitz, M.M.; van Bekkum, D.W.; Camitta, B.M.; Elfenbein, G.E.; Gale, R.P.; Gluckman, E.; Good, R.A.; Rimm, A.A.; Rozman, C.; et al. Graft failure following bone marrow transplantation for severe aplastic anemia: Risk factors and treatment results. Blood 1989, 73, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Piccin, A.; O’Marcaigh, A.; Smith, O.; O’Riordan, J.; Crowley, M.; Vandenberg, E.; Gardiner, N.; Mc Cann, S. Outcome of bone marrow transplantation in acquired and inherited aplastic anaemia in the Republic of Ireland. Ir. J. Med. Sci. 2005, 174, 13–19. [Google Scholar] [CrossRef]
- Julen, K.; Volken, T.; Holbro, A.; Infanti, L.; Halter, J.P.; Schaub, S.; Wehmeier, C.; Diesch, T.; Rovó, A.; Passweg, J.R.; et al. Transfusions in Aplastic Anemia Patients Cause HLA Alloimmunization: Comparisons of Current and Past Cohorts Demonstrate Progress. Transplant. Cell. Ther. Off. Publ. Am. Soc. Transplant. Cell. Ther. 2021, 27, e931–e939. [Google Scholar] [CrossRef]
- Killick, S.B.; Win, N.; Marsh, J.C.; Kaye, T.; Yandle, A.; Humphries, C.; Knowles, S.M.; Gordon-Smith, E.C. Pilot study of HLA alloimmunization after transfusion with pre-storage leucodepleted blood products in aplastic anaemia. Br. J. Haematol. 1997, 97, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Ciurea, S.O.; de Lima, M.; Cano, P.; Korbling, M.; Giralt, S.; Shpall, E.J.; Wang, X.; Thall, P.F.; Champlin, R.E.; Fernandez-Vina, M. High risk of graft failure in patients with anti-HLA antibodies undergoing haploidentical stem-cell transplantation. Transplantation 2009, 88, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Satwani, P.; Cooper, N.; Rao, K.; Veys, P.; Amrolia, P. Reduced intensity conditioning and allogeneic stem cell transplantation in childhood malignant and nonmalignant diseases. Bone Marrow Transplant. 2008, 41, 173–182. [Google Scholar] [CrossRef]
- Cancio, M.; Hebert, K.; Kim, S.; Aljurf, M.; Olson, T.; Anderson, E.; Burroughs, L.; Vatsayan, A.; Myers, K.; Hashem, H.; et al. Outcomes in Hematopoietic Stem Cell Transplantation for Congenital Amegakaryocytic Thrombocytopenia. Transpl. Cell Ther. 2022, 28, 101.e1–101.e6. [Google Scholar] [CrossRef]
- Miano, M.; Eikema, D.-J.; de la Fuente, J.; Bosman, P.; Ghavamzadeh, A.; Smiers, F.; Sengeløv, H.; Yesilipek, A.; Formankova, R.; Bader, P.; et al. Stem Cell Transplantation for Diamond–Blackfan Anemia. A Retrospective Study on Behalf of the Severe Aplastic Anemia Working Party of the European Blood and Marrow Transplantation Group (EBMT). Transplant. Cell. Ther. 2021, 27, 274.e1–274.e5. [Google Scholar] [CrossRef]
- Fagioli, F.; Quarello, P.; Zecca, M.; Lanino, E.; Corti, P.; Favre, C.; Ripaldi, M.; Ramenghi, U.; Locatelli, F.; Prete, A. Haematopoietic stem cell transplantation for Diamond Blackfan anaemia: A report from the Italian Association of Paediatric Haematology and Oncology Registry. Br. J. Haematol. 2014, 165, 673–681. [Google Scholar] [CrossRef]
- Strahm, B.; Loewecke, F.; Niemeyer, C.M.; Albert, M.; Ansari, M.; Bader, P.; Bertrand, Y.; Burkhardt, B.; Da Costa, L.M.; Ferster, A.; et al. Favorable outcomes of hematopoietic stem cell transplantation in children and adolescents with Diamond-Blackfan anemia. Blood Adv. 2020, 4, 1760–1769. [Google Scholar] [CrossRef]
- Darrigo Junior, L.G.; Loth, G.; Kuwahara, C.; Vieira, A.; Colturato, V.; Rodrigues, A.L.; Arcuri, L.; Fernandes, J.; Macedo, A.; Tavares, R.; et al. Hematopoietic cell transplantation for Diamond Blackfan anemia: A report from the Pediatric Group of the Brazilian Bone Marrow Transplantation Society. Eur. J. Haematol. 2020, 105, 426–433. [Google Scholar] [CrossRef]
- Fioredda, F.; Iacobelli, S.; Korthof, E.T.; Knol, C.; van Biezen, A.; Bresters, D.; Veys, P.; Yoshimi, A.; Fagioli, F.; Mats, B.; et al. Outcome of haematopoietic stem cell transplantation in dyskeratosis congenita. Br. J. Haematol. 2018, 183, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Eapen, M.; Brazauskas, R.; Carreras, J.; Aljurf, M.; Gale, R.P.; Hale, G.A.; Ilhan, O.; Passweg, J.R.; Ringdén, O.; et al. Impact of age on outcomes after bone marrow transplantation for acquired aplastic anemia using HLA-matched sibling donors. Haematologica 2010, 95, 2119–2125. [Google Scholar] [CrossRef] [PubMed]
- Dokal, I.; Vulliamy, T. Inherited bone marrow failure syndromes. Haematologica 2010, 95, 1236–1240. [Google Scholar] [CrossRef]
- Peake, J.D.; Noguchi, E. Fanconi anemia: Current insights regarding epidemiology, cancer, and DNA repair. Hum. Genet. 2022, 141, 1811–1836. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Nebert, D.W.; Bruford, E.A.; Thompson, D.C.; Joenje, H.; Vasiliou, V. Update of the human and mouse Fanconi anemia genes. Hum. Genom. 2015, 9, 32. [Google Scholar] [CrossRef] [PubMed]
- van de Kooij, B.; van der Wal, F.J.; Rother, M.B.; Creixell, P.; Stout, M.; Wiegant, W.; Joughin, B.A.; Vornberger, J.; van Vugt, M.; Altmeyer, M.; et al. The Fanconi anemia core complex promotes CtIP-dependent end-resection to drive homologous recombination at DNA double-strand breaks. bioRxiv 2023. [Google Scholar] [CrossRef]
- Kawashima, N.; Bezzerri, V.; Corey, S.J. The Molecular and Genetic Mechanisms of Inherited Bone Marrow Failure Syndromes: The Role of Inflammatory Cytokines in Their Pathogenesis. Biomolecules 2023, 13, 1249. [Google Scholar] [CrossRef] [PubMed]
- Moreno, O.M.; Paredes, A.C.; Suarez-Obando, F.; Rojas, A. An update on Fanconi anemia: Clinical, cytogenetic and molecular approaches. Biomed. Rep. 2021, 15, 74. [Google Scholar] [CrossRef]
- Dufour, C.; Pierri, F. Modern management of Fanconi anemia. Hematol. Am. Soc. Hematol. Educ. Program. 2022, 2022, 649–657. [Google Scholar] [CrossRef]
- Dufour, C. How I manage patients with Fanconi anaemia. Br. J. Haematol. 2017, 178, 32–47. [Google Scholar] [CrossRef]
- Wagner, J.E.; Eapen, M.; MacMillan, M.L.; Harris, R.E.; Pasquini, R.; Boulad, F.; Zhang, M.J.; Auerbach, A.D. Unrelated donor bone marrow transplantation for the treatment of Fanconi anemia. Blood 2007, 109, 2256–2262. [Google Scholar] [CrossRef]
- Peffault de Latour, R.; Porcher, R.; Dalle, J.-H.; Aljurf, M.; Korthof, E.T.; Svahn, J.; Willemze, R.; Barrenetxea, C.; Mialou, V.; Soulier, J.; et al. Allogeneic hematopoietic stem cell transplantation in Fanconi anemia: The European Group for Blood and Marrow Transplantation experience. Blood 2013, 122, 4279–4286. [Google Scholar] [CrossRef]
- Xu, L.; Lu, Y.; Chen, J.; Sun, S.; Hu, S.; Wang, S.; Wu, X.; Sun, Y.; Wan, D.; Xu, Y.; et al. Fludarabine- and low-dose cyclophosphamide-based conditioning regimens provided favorable survival and engraftment for unmanipulated hematopoietic cell transplantation from unrelated donors and matched siblings in patients with Fanconi anemia: Results from the CBMTR. Bone Marrow Transplant. 2023, 58, 106–108. [Google Scholar] [PubMed]
- MacMillan, M.L.; DeFor, T.E.; Young, J.A.; Dusenbery, K.E.; Blazar, B.R.; Slungaard, A.; Zierhut, H.; Weisdorf, D.J.; Wagner, J.E. Alternative donor hematopoietic cell transplantation for Fanconi anemia. Blood 2015, 125, 3798–3804. [Google Scholar] [CrossRef] [PubMed]
- Ebens, C.L.; MacMillan, M.L.; Wagner, J.E. Hematopoietic cell transplantation in Fanconi anemia: Current evidence, challenges and recommendations. Expert. Rev. Hematol. 2017, 10, 81–97. [Google Scholar] [CrossRef]
- Rosenberg, P.S.; Socié, G.; Alter, B.P.; Gluckman, E. Risk of head and neck squamous cell cancer and death in patients with Fanconi anemia who did and did not receive transplants. Blood 2005, 105, 67–73. [Google Scholar] [CrossRef]
- Deeg, H.J.; Socié, G.; Schoch, G.; Henry-Amar, M.; Witherspoon, R.P.; Devergie, A.; Sullivan, K.M.; Gluckman, E.; Storb, R. Malignancies after marrow transplantation for aplastic anemia and fanconi anemia: A joint Seattle and Paris analysis of results in 700 patients. Blood 1996, 87, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Pasquini, R.; Carreras, J.; Pasquini, M.C.; Camitta, B.M.; Fasth, A.L.; Hale, G.A.; Harris, R.E.; Marsh, J.C.; Robinson, A.J.; Zhang, M.J.; et al. HLA-matched sibling hematopoietic stem cell transplantation for fanconi anemia: Comparison of irradiation and nonirradiation containing conditioning regimens. Biol. Blood Marrow Transpl. 2008, 14, 1141–1147. [Google Scholar] [CrossRef]
- Benajiba, L.; Salvado, C.; Dalle, J.-H.; Jubert, C.; Galambrun, C.; Soulier, J.; Socié, G.; Peffault de Latour, R. HLA-matched related-donor HSCT in Fanconi anemia patients conditioned with cyclophosphamide and fludarabine. Blood 2015, 125, 417–418. [Google Scholar] [CrossRef] [PubMed]
- Bonfim, C.; Nichele, S.; Loth, G.; Funke, V.A.M.; Nabhan, S.K.; Pillonetto, D.V.; Lima, A.C.M.; Pasquini, R. Transplantation for Fanconi anaemia: Lessons learned from Brazil. Lancet Haematol. 2022, 9, e228–e236. [Google Scholar] [CrossRef] [PubMed]
- Bernard, F.; Uppugunduri, C.R.S.; Meyer, S.; Cummins, M.; Patrick, K.; James, B.; Skinner, R.; Tewari, S.; Carpenter, B.; Wynn, R.; et al. Excellent overall and chronic graft-versus-host-disease-free event-free survival in Fanconi anaemia patients undergoing matched related- and unrelated-donor bone marrow transplantation using alemtuzumab–Flu–Cy: The UK experience. Br. J. Haematol. 2021, 193, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.A.; Davies, S.M.; Leemhuis, T.; Myers, K.; Kernan, N.A.; Prockop, S.E.; Scaradavou, A.; O’Reilly, R.J.; Williams, D.A.; Lehmann, L.; et al. Radiation-free, alternative-donor HCT for Fanconi anemia patients: Results from a prospective multi-institutional study. Blood 2017, 129, 2308–2315. [Google Scholar] [CrossRef]
- Chao, M.M.; Kuehl, J.S.; Strauss, G.; Hanenberg, H.; Schindler, D.; Neitzel, H.; Niemeyer, C.; Baumann, I.; von Bernuth, H.; Rascon, J.; et al. Outcomes of mismatched and unrelated donor hematopoietic stem cell transplantation in Fanconi anemia conditioned with chemotherapy only. Ann. Hematol. 2015, 94, 1311–1318. [Google Scholar] [CrossRef]
- Strocchio, L.; Pagliara, D.; Algeri, M.; Li Pira, G.; Rossi, F.; Bertaina, V.; Leone, G.; Pinto, R.M.; Andreani, M.; Agolini, E.; et al. HLA-haploidentical TCRαβ+/CD19+-depleted stem cell transplantation in children and young adults with Fanconi anemia. Blood Adv. 2021, 5, 1333–1339. [Google Scholar] [CrossRef]
- Bonfim, C.; Ribeiro, L.; Nichele, S.; Loth, G.; Bitencourt, M.; Koliski, A.; Kuwahara, C.; Fabro, A.L.; Pereira, N.F.; Pilonetto, D.; et al. Haploidentical Bone Marrow Transplantation with Post-Transplant Cyclophosphamide for Children and Adolescents with Fanconi Anemia. Biol. Blood Marrow Transpl. 2017, 23, 310–317. [Google Scholar] [CrossRef]
- Ayas, M.; Siddiqui, K.; Al-Jefri, A.; Al-Ahmari, A.; Ghemlas, I.; Al-Saedi, H.; Alanazi, A.; Jafri, R.; Ayas, M.F.; Al-Seraihi, A. Successful Outcome in Patients with Fanconi Anemia Undergoing T Cell-Replete Mismatched Related Donor Hematopoietic Cell Transplantation Using Reduced-Dose Cyclophosphamide Post-Transplantation. Biol. Blood Marrow Transpl. 2019, 25, 2217–2221. [Google Scholar] [CrossRef]
- Zecca, M.; Strocchio, L.; Pagliara, D.; Comoli, P.; Bertaina, A.; Giorgiani, G.; Perotti, C.; Corbella, F.; Brescia, L.; Locatelli, F. HLA-Haploidentical T Cell–Depleted Allogeneic Hematopoietic Stem Cell Transplantation in Children with Fanconi Anemia. Biol. Blood Marrow Transplant. 2014, 20, 571–576. [Google Scholar] [CrossRef]
- Giardino, S.; de Latour, R.P.; Aljurf, M.; Eikema, D.-J.; Bosman, P.; Bertrand, Y.; Tbakhi, A.; Holter, W.; Bornhäuser, M.; Rössig, C.; et al. Outcome of patients with Fanconi anemia developing myelodysplasia and acute leukemia who received allogeneic hematopoietic stem cell transplantation: A retrospective analysis on behalf of EBMT group. Am. J. Hematol. 2020, 95, 809–816. [Google Scholar] [CrossRef]
- Ayas, M.; Saber, W.; Davies, S.M.; Harris, R.E.; Hale, G.A.; Socie, G.; LeRademacher, J.; Thakar, M.; Deeg, H.J.; Al-Seraihy, A.; et al. Allogeneic hematopoietic cell transplantation for fanconi anemia in patients with pretransplantation cytogenetic abnormalities, myelodysplastic syndrome, or acute leukemia. J. Clin. Oncol. 2013, 31, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Yabe, M.; Morio, T.; Tabuchi, K.; Tomizawa, D.; Hasegawa, D.; Ishida, H.; Yoshida, N.; Koike, T.; Takahashi, Y.; Koh, K.; et al. Long-term outcome in patients with Fanconi anemia who received hematopoietic stem cell transplantation: A retrospective nationwide analysis. Int. J. Hematol. 2021, 113, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Paustian, L.; Chao, M.M.; Hanenberg, H.; Schindler, D.; Neitzel, H.; Kratz, C.P.; Ebell, W. Androgen therapy in Fanconi anemia: A retrospective analysis of 30 years in Germany. Pediatr. Hematol. Oncol. 2016, 33, 5–12. [Google Scholar] [CrossRef]
- Ebens, C.L.; DeFor, T.E.; Tryon, R.; Wagner, J.E.; MacMillan, M.L. Comparable Outcomes after HLA-Matched Sibling and Alternative Donor Hematopoietic Cell Transplantation for Children with Fanconi Anemia and Severe Aplastic Anemia. Biol. Blood Marrow Transpl. 2018, 24, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.R.; Wagner, J.E.; Auerbach, A.D.; Coad, J.E.; Dietz, C.A.; Schwarzenberg, S.J.; MacMillan, M.L. Fatal hemorrhage from androgen-related hepatic adenoma after hematopoietic cell transplantation. J. Pediatr. Hematol. Oncol. 2004, 26, 16–18. [Google Scholar] [CrossRef]
- Velazquez, I.; Alter, B.P. Androgens and liver tumors: Fanconi’s anemia and non-Fanconi’s conditions. Am. J. Hematol. 2004, 77, 257–267. [Google Scholar] [CrossRef]
- Niewisch, M.R.; Savage, S.A. An update on the biology and management of dyskeratosis congenita and related telomere biology disorders. Expert. Rev. Hematol. 2019, 12, 1037–1052. [Google Scholar] [CrossRef]
- Grill, S.; Nandakumar, J. Molecular mechanisms of telomere biology disorders. J. Biol. Chem. 2021, 296, 100064. [Google Scholar] [CrossRef]
- Vulliamy, T.J.; Marrone, A.; Knight, S.W.; Walne, A.; Mason, P.J.; Dokal, I. Mutations in dyskeratosis congenita: Their impact on telomere length and the diversity of clinical presentation. Blood 2006, 107, 2680–2685. [Google Scholar] [CrossRef]
- Vieri, M.; Brümmendorf, T.H.; Beier, F. Treatment of telomeropathies. Best. Pract. Res. Clin. Haematol. 2021, 34, 101282. [Google Scholar] [CrossRef]
- Mackintosh, J.A.; Pietsch, M.; Lutzky, V.; Enever, D.; Bancroft, S.; Apte, S.H.; Tan, M.; Yerkovich, S.T.; Dickinson, J.L.; Pickett, H.A.; et al. TELO-SCOPE study: A randomised, double-blind, placebo-controlled, phase 2 trial of danazol for short telomere related pulmonary fibrosis. BMJ Open Respir. Res. 2021, 8, e001127. [Google Scholar] [CrossRef] [PubMed]
- Tummala, H.; Walne, A.; Dokal, I. The biology and management of dyskeratosis congenita and related disorders of telomeres. Expert. Rev. Hematol. 2022, 15, 685–696. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S. Evaluation and Management of Hematopoietic Failure in Dyskeratosis Congenita. Hematol./Oncol. Clin. N. Am. 2018, 32, 669–685. [Google Scholar] [CrossRef] [PubMed]
- Pagliuca, S.; Kulasekararaj, A.G.; Eikema, D.-J.; Piepenbroek, B.; Iftikhar, R.; Satti, T.M.; Griffin, M.; Laurino, M.; Kupesiz, A.; Bertrand, Y.; et al. Current use of androgens in bone marrow failure disorders: A report from the Severe Aplastic Anemia Working Party of the European Society of Blood and Marrow Transplantation. Haematologica 2023. [Google Scholar] [CrossRef]
- Calado, R.T.; Yewdell, W.T.; Wilkerson, K.L.; Regal, J.A.; Kajigaya, S.; Stratakis, C.A.; Young, N.S. Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood 2009, 114, 2236–2243. [Google Scholar] [CrossRef]
- Khincha, P.P.; Bertuch, A.A.; Gadalla, S.M.; Giri, N.; Alter, B.P.; Savage, S.A. Similar telomere attrition rates in androgen-treated and untreated patients with dyskeratosis congenita. Blood Adv. 2018, 2, 1243–1249. [Google Scholar] [CrossRef]
- Maggio, M.; Snyder, P.J.; Ceda, G.P.; Milaneschi, Y.; Luci, M.; Cattabiani, C.; Masoni, S.; Vignali, A.; Volpi, R.; Lauretani, F.; et al. Is the haematopoietic effect of testosterone mediated by erythropoietin? The results of a clinical trial in older men. Andrology 2013, 1, 24–28. [Google Scholar] [CrossRef]
- Townsley, D.M.; Dumitriu, B.; Liu, D.; Biancotto, A.; Weinstein, B.; Chen, C.; Hardy, N.; Mihalek, A.D.; Lingala, S.; Kim, Y.J.; et al. Danazol Treatment for Telomere Diseases. N. Engl. J. Med. 2016, 374, 1922–1931. [Google Scholar] [CrossRef]
- Yeap, B.B.; Knuiman, M.W.; Divitini, M.L.; Hui, J.; Arscott, G.M.; Handelsman, D.J.; McLennan, S.V.; Twigg, S.M.; McQuillan, B.; Hung, J.; et al. Epidemiological and Mendelian Randomization Studies of Dihydrotestosterone and Estradiol and Leukocyte Telomere Length in Men. J. Clin. Endocrinol. Metab. 2016, 101, 1299–1306. [Google Scholar] [CrossRef]
- Khincha, P.P.; Wentzensen, I.M.; Giri, N.; Alter, B.P.; Savage, S.A. Response to androgen therapy in patients with dyskeratosis congenita. Br. J. Haematol. 2014, 165, 349–357. [Google Scholar] [CrossRef]
- Cheung, A.S.; Yeap, B.B.; Hoermann, R.; Hui, J.; Beilby, J.P.; Grossmann, M. Effects of androgen deprivation therapy on telomere length. Clin. Endocrinol. 2017, 87, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Alter, B.P.; Giri, N.; Savage, S.A.; Rosenberg, P.S. Cancer in dyskeratosis congenita. Blood 2009, 113, 6549–6557. [Google Scholar] [CrossRef] [PubMed]
- Barbaro, P.; Vedi, A. Survival after Hematopoietic Stem Cell Transplant in Patients with Dyskeratosis Congenita: Systematic Review of the Literature. Biol. Blood Marrow Transpl. 2016, 22, 1152–1158. [Google Scholar] [CrossRef]
- Renata, B.; Carmen, B.; Vanderson, R.; Gérard, S.; Franco, L.; KaWah, C.; Oscar, R.; Joel, S.; Samir, N.; Eliana, M.; et al. Outcomes after related and unrelated umbilical cord blood transplantation for hereditary bone marrow failure syndromes other than Fanconi anemia. Haematologica 2011, 96, 134–141. [Google Scholar]
- Dietz, A.C.; Orchard, P.J.; Baker, K.S.; Giller, R.H.; Savage, S.A.; Alter, B.P.; Tolar, J. Disease-specific hematopoietic cell transplantation: Nonmyeloablative conditioning regimen for dyskeratosis congenita. Bone Marrow Transpl. 2011, 46, 98–104. [Google Scholar] [CrossRef]
- Nederlof, I.; Lindemans, C.A.; Bierings, M.B.; Mohseny, A.B.; Bresters, D.; Bartels, M. Recognizing a Non-classical Telomeropathy before Hematopoietic Stem Cell Transplantation in Pediatric Patients: A Case Series. Hemasphere 2019, 3, e282. [Google Scholar] [CrossRef]
- Giri, N.; Pitel, P.A.; Green, D.; Alter, B.P. Splenic peliosis and rupture in patients with dyskeratosis congenita on androgens and granulocyte colony-stimulating factor. Br. J. Haematol. 2007, 138, 815–817. [Google Scholar] [CrossRef] [PubMed]
- Shukla, S.; Jeong, H.-C.; Sturgeon, C.M.; Parker, R.; Batista, L.F.Z. Chemical inhibition of PAPD5/7 rescues telomerase function and hematopoiesis in dyskeratosis congenita. Blood Adv. 2020, 4, 2717–2722. [Google Scholar] [CrossRef]
- Nagpal, N.; Wang, J.; Zeng, J.; Lo, E.; Moon, D.H.; Luk, K.; Braun, R.O.; Burroughs, L.M.; Keel, S.B.; Reilly, C.; et al. Small-Molecule PAPD5 Inhibitors Restore Telomerase Activity in Patient Stem Cells. Cell Stem Cell 2020, 26, 896–909.e8. [Google Scholar] [CrossRef]
- Mannherz, W.; Agarwal, S. Thymidine nucleotide metabolism controls human telomere length. Nat. Genet. 2023, 55, 568–580. [Google Scholar] [CrossRef]
- Bartels, M.; Bierings, M. How I manage children with Diamond-Blackfan anaemia. Br. J. Haematol. 2019, 184, 123–133. [Google Scholar] [CrossRef]
- Da Costa, L.; Leblanc, T.; Mohandas, N. Diamond-Blackfan anemia. Blood 2020, 136, 1262–1273. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, L.S.; Gazda, H.T.; Eng, J.C.; Eichhorn, S.W.; Thiru, P.; Ghazvinian, R.; George, T.I.; Gotlib, J.R.; Beggs, A.H.; Sieff, C.A.; et al. Altered translation of GATA1 in Diamond-Blackfan anemia. Nat. Med. 2014, 20, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, L.M.; Marie, I.; Leblanc, T.M. Diamond-Blackfan anemia. Hematol. Am. Soc. Hematol. Educ. Program. 2021, 2021, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, A.; Gupta, A.; Dutta, A.; Potluri, P.; Batti, B. A Review of Diamond-Blackfan Anemia: Current Evidence on Involved Genes and Treatment Modalities. Cureus 2020, 12, e10019. [Google Scholar] [CrossRef]
- Lipton, J.M.; Ellis, S.R. Diamond-Blackfan anemia: Diagnosis, treatment, and molecular pathogenesis. Hematol. Oncol. Clin. N. Am. 2009, 23, 261–282. [Google Scholar] [CrossRef]
- Quarello, P.; Garelli, E.; Carando, A.; Cillario, R.; Brusco, A.; Giorgio, E.; Ferrante, D.; Corti, P.; Zecca, M.; Luciani, M.; et al. A 20-year long term experience of the Italian Diamond-Blackfan Anaemia Registry: RPS and RPL genes, different faces of the same disease? Br. J. Haematol. 2020, 190, 93–104. [Google Scholar] [CrossRef]
- Vlachos, A.; Rosenberg, P.S.; Atsidaftos, E.; Kang, J.; Onel, K.; Sharaf, R.N.; Alter, B.P.; Lipton, J.M. Increased risk of colon cancer and osteogenic sarcoma in Diamond-Blackfan anemia. Blood 2018, 132, 2205–2208. [Google Scholar] [CrossRef]
- Lipton, J.M.; Molmenti, C.L.S.; Desai, P.; Lipton, A.; Ellis, S.R.; Vlachos, A. Early Onset Colorectal Cancer: An Emerging Cancer Risk in Patients with Diamond Blackfan Anemia. Genes 2021, 13, 56. [Google Scholar] [CrossRef]
- Lipton, J.M.; Atsidaftos, E.; Zyskind, I.; Vlachos, A. Improving clinical care and elucidating the pathophysiology of Diamond Blackfan anemia: An update from the Diamond Blackfan Anemia Registry. Pediatr. Blood Cancer 2006, 46, 558–564. [Google Scholar] [CrossRef]
- Vlachos, A.; Ball, S.; Dahl, N.; Alter, B.P.; Sheth, S.; Ramenghi, U.; Meerpohl, J.; Karlsson, S.; Liu, J.M.; Leblanc, T.; et al. Diagnosing and treating Diamond Blackfan anaemia: Results of an international clinical consensus conference. Br. J. Haematol. 2008, 142, 859–876. [Google Scholar] [CrossRef] [PubMed]
- Vlachos, A.; Muir, E. How I treat Diamond-Blackfan anemia. Blood 2010, 116, 3715–3723. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Lodish, H.F.; Sieff, C.A. Critical Issues in Diamond-Blackfan Anemia and Prospects for Novel Treatment. Hematol. Oncol. Clin. N. Am. 2018, 32, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lyssikatos, C.; Atsidaftos, E.; Muir, E.; Gazda, H.; Beggs, A.H.; Lipton, J.M.; Vlachos, A. Remission in Patients with Diamond Blackfan Anemia (DBA) Appears to Be Unrestricted by Phenotype or Genotype. Blood 2008, 112, 3092. [Google Scholar] [CrossRef]
- Roy, V.; Pérez, W.S.; Eapen, M.; Marsh, J.C.W.; Pasquini, M.; Pasquini, R.; Mustafa, M.M.; Bredeson, C.N. Bone Marrow Transplantation for Diamond-Blackfan Anemia. Biol. Blood Marrow Transplant. 2005, 11, 600–608. [Google Scholar] [CrossRef]
- Vlachos, A.; Rosenberg, P.S.; Atsidaftos, E.; Alter, B.P.; Lipton, J.M. Incidence of neoplasia in Diamond Blackfan anemia: A report from the Diamond Blackfan Anemia Registry. Blood 2012, 119, 3815–3819. [Google Scholar] [CrossRef]
- Burroughs, L.M.; Shimamura, A.; Talano, J.A.; Domm, J.A.; Baker, K.K.; Delaney, C.; Frangoul, H.; Margolis, D.A.; Baker, K.S.; Nemecek, E.R.; et al. Allogeneic Hematopoietic Cell Transplantation Using Treosulfan-Based Conditioning for Treatment of Marrow Failure Disorders. Biol. Blood Marrow Transpl. 2017, 23, 1669–1677. [Google Scholar] [CrossRef]
- Koyamaishi, S.; Kamio, T.; Kobayashi, A.; Sato, T.; Kudo, K.; Sasaki, S.; Kanezaki, R.; Hasegawa, D.; Muramatsu, H.; Takahashi, Y.; et al. Reduced-intensity conditioning is effective for hematopoietic stem cell transplantation in young pediatric patients with Diamond–Blackfan anemia. Bone Marrow Transplant. 2021, 56, 1013–1020. [Google Scholar] [CrossRef]
- Wilkes, M.C.; Siva, K.; Varetti, G.; Mercado, J.; Wentworth, E.P.; Perez, C.A.; Saxena, M.; Kam, S.; Kapur, S.; Chen, J.; et al. Metformin-induced suppression of Nemo-like kinase improves erythropoiesis in preclinical models of Diamond-Blackfan anemia through induction of miR-26a. Exp. Hematol. 2020, 91, 65–77. [Google Scholar] [CrossRef]
- Wang, N.; LaVasseur, C.; Riaz, R.; Papoin, J.; Blanc, L.; Narla, A. Targeting of Calbindin 1 rescues erythropoiesis in a human model of Diamond Blackfan anemia. Blood Cells Mol. Dis. 2023, 102, 102759. [Google Scholar] [CrossRef]
- Macari, E.R.; Taylor, A.M.; Raiser, D.; Siva, K.; McGrath, K.; Humphries, J.M.; Flygare, J.; Ebert, B.L.; Zon, L.I. Calmodulin Inhibition Rescues DBA Models with Ribosomal Protein Deficiency through Reduction of RSK Signaling. Blood 2016, 128, 332. [Google Scholar] [CrossRef]
- Ear, J.; Huang, H.; Wilson, T.; Tehrani, Z.; Lindgren, A.; Sung, V.; Laadem, A.; Daniel, T.O.; Chopra, R.; Lin, S. RAP-011 improves erythropoiesis in zebrafish model of Diamond-Blackfan anemia through antagonizing lefty1. Blood 2015, 126, 880–890. [Google Scholar] [CrossRef]
- Payne, E.M.; Virgilio, M.; Narla, A.; Sun, H.; Levine, M.; Paw, B.H.; Berliner, N.; Look, A.T.; Ebert, B.L.; Khanna-Gupta, A. L-Leucine improves the anemia and developmental defects associated with Diamond-Blackfan anemia and del(5q) MDS by activating the mTOR pathway. Blood 2012, 120, 2214–2224. [Google Scholar] [CrossRef] [PubMed]
- Jaako, P.; Debnath, S.; Olsson, K.; Bryder, D.; Flygare, J.; Karlsson, S. Dietary L-leucine improves the anemia in a mouse model for Diamond-Blackfan anemia. Blood 2012, 120, 2225–2228. [Google Scholar] [CrossRef] [PubMed]
- Park, M. Overview of inherited bone marrow failure syndromes. Blood Res. 2022, 57, 49–54. [Google Scholar] [CrossRef]
- Myers, K.C.; Davies, S.M.; Shimamura, A. Clinical and molecular pathophysiology of Shwachman-Diamond syndrome: An update. Hematol. Oncol. Clin. N. Am. 2013, 27, 117–128. [Google Scholar] [CrossRef]
- Woloszynek, J.R.; Rothbaum, R.J.; Rawls, A.S.; Minx, P.J.; Wilson, R.K.; Mason, P.J.; Bessler, M.; Link, D.C. Mutations of the SBDS gene are present in most patients with Shwachman-Diamond syndrome. Blood 2004, 104, 3588–3590. [Google Scholar] [CrossRef]
- Bezzerri, V.; Cipolli, M. Shwachman-Diamond Syndrome: Molecular Mechanisms and Current Perspectives. Mol. Diagn. Ther. 2019, 23, 281–290. [Google Scholar] [CrossRef]
- Myers, K.; Hebert, K.; Antin, J.; Boulad, F.; Burroughs, L.; Hofmann, I.; Kamble, R.; MacMillan, M.L.; Eapen, M. Hematopoietic Stem Cell Transplantation for Shwachman-Diamond Syndrome. Biol. Blood Marrow Transpl. 2020, 26, 1446–1451. [Google Scholar] [CrossRef]
- Cesaro, S.; Oneto, R.; Messina, C.; Gibson, B.E.; Buzyn, A.; Steward, C.; Gluckman, E.; Breddius, R.; Boogaerts, M.; Vermylen, C.; et al. Haematopoietic stem cell transplantation for Shwachman–Diamond disease: A study from the European Group for blood and marrow transplantation. Br. J. Haematol. 2005, 131, 231–236. [Google Scholar] [CrossRef]
- Donadieu, J.; Michel, G.; Merlin, E.; Bordigoni, P.; Monteux, B.; Beaupain, B.; Leverger, G.; Laporte, J.P.; Hermine, O.; Buzyn, A.; et al. Hematopoietic stem cell transplantation for Shwachman-Diamond syndrome: Experience of the French neutropenia registry. Bone Marrow Transpl. 2005, 36, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Cesaro, S.; Pillon, M.; Sauer, M.; Smiers, F.; Faraci, M.; de Heredia, C.D.; Wynn, R.; Greil, J.; Locatelli, F.; Veys, P.; et al. Long-term outcome after allogeneic hematopoietic stem cell transplantation for Shwachman–Diamond syndrome: A retrospective analysis and a review of the literature by the Severe Aplastic Anemia Working Party of the European Society for Blood and Marrow Transplantation (SAAWP-EBMT). Bone Marrow Transplant. 2020, 55, 1796–1809. [Google Scholar]
- Myers, K.C.; Furutani, E.; Weller, E.; Siegele, B.; Galvin, A.; Arsenault, V.; Alter, B.P.; Boulad, F.; Bueso-Ramos, C.; Burroughs, L.; et al. Clinical features and outcomes of patients with Shwachman-Diamond syndrome and myelodysplastic syndrome or acute myeloid leukaemia: A multicentre, retrospective, cohort study. Lancet Haematol. 2020, 7, e238–e246. [Google Scholar] [CrossRef] [PubMed]
- Donadieu, J.; Fenneteau, O.; Beaupain, B.; Beaufils, S.; Bellanger, F.; Mahlaoui, N.; Lambilliotte, A.; Aladjidi, N.; Bertrand, Y.; Mialou, V.; et al. Classification of and risk factors for hematologic complications in a French national cohort of 102 patients with Shwachman-Diamond syndrome. Haematologica 2012, 97, 1312–1319. [Google Scholar] [CrossRef]
- Dror, Y.; Donadieu, J.; Koglmeier, J.; Dodge, J.; Toiviainen-Salo, S.; Makitie, O.; Kerr, E.; Zeidler, C.; Shimamura, A.; Shah, N.; et al. Draft consensus guidelines for diagnosis and treatment of Shwachman-Diamond syndrome. Ann. N. Y. Acad. Sci. 2011, 1242, 40–55. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.T.; Link, D.C. Impaired myelopoiesis in congenital neutropenia: Insights into clonal and malignant hematopoiesis. Hematol. Am. Soc. Hematol. Educ. Program. 2021, 2021, 514–520. [Google Scholar] [CrossRef]
- Zambetti, N.A.; Ping, Z.; Chen, S.; Kenswil, K.J.; Mylona, M.A.; Sanders, M.A.; Hoogenboezem, R.M.; Bindels, E.M.; Adisty, M.N.; Van Strien, P.M.; et al. Mesenchymal Inflammation Drives Genotoxic Stress in Hematopoietic Stem Cells and Predicts Disease Evolution in Human Pre-leukemia. Cell Stem Cell 2016, 19, 613–627. [Google Scholar] [CrossRef]
- Furutani, E.; Liu, S.; Galvin, A.; Steltz, S.; Malsch, M.M.; Loveless, S.K.; Mount, L.; Larson, J.H.; Queenan, K.; Bertuch, A.A.; et al. Hematologic complications with age in Shwachman-Diamond syndrome. Blood Adv. 2022, 6, 297–306. [Google Scholar] [CrossRef]
- Bhatla, D.; Davies, S.M.; Shenoy, S.; Harris, R.E.; Crockett, M.; Shoultz, L.; Smolarek, T.; Bleesing, J.; Hansen, M.; Jodele, S.; et al. Reduced-intensity conditioning is effective and safe for transplantation of patients with Shwachman-Diamond syndrome. Bone Marrow Transpl. 2008, 42, 159–165. [Google Scholar] [CrossRef]
- Dale, D.C.; Link, D.C. The many causes of severe congenital neutropenia. N. Engl. J. Med. 2009, 360, 3–5. [Google Scholar] [CrossRef]
- Xia, J.; Bolyard, A.A.; Rodger, E.; Stein, S.; Aprikyan, A.A.; Dale, D.C.; Link, D.C. Prevalence of mutations in ELANE, GFI1, HAX1, SBDS, WAS and G6PC3 in patients with severe congenital neutropenia. Br. J. Haematol. 2009, 147, 535–542. [Google Scholar] [CrossRef]
- Köllner, I.; Sodeik, B.; Schreek, S.; Heyn, H.; von Neuhoff, N.; Germeshausen, M.; Zeidler, C.; Krüger, M.; Schlegelberger, B.; Welte, K.; et al. Mutations in neutrophil elastase causing congenital neutropenia lead to cytoplasmic protein accumulation and induction of the unfolded protein response. Blood 2006, 108, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Skokowa, J.; Dale, D.C.; Touw, I.P.; Zeidler, C.; Welte, K. Severe congenital neutropenias. Nat. Rev. Dis. Primers 2017, 3, 17032. [Google Scholar] [CrossRef]
- Fioredda, F.; Lanza, T.; Gallicola, F.; Riccardi, F.; Lanciotti, M.; Mastrodicasa, E.; Signa, S.; Zanardi, S.; Calvillo, M.; Dufour, C. Long-term use of pegfilgrastim in children with severe congenital neutropenia: Clinical and pharmacokinetic data. Blood 2016, 128, 2178–2181. [Google Scholar] [CrossRef]
- Deordieva, E.; Shvets, O.; Voronin, K.; Maschan, A.; Welte, K.; Skokowa, J.; Novichkova, G.; Shcherbina, A. Nicotinamide (vitamin B3) treatment improves response to G-CSF in severe congenital neutropenia patients. Br. J. Haematol. 2021, 192, 788–792. [Google Scholar] [CrossRef]
- Dale, D.C.; Bonilla, M.A.; Davis, M.W.; Nakanishi, A.M.; Hammond, W.P.; Kurtzberg, J.; Wang, W.; Jakubowski, A.; Winton, E.; Lalezari, P.; et al. A randomized controlled phase III trial of recombinant human granulocyte colony-stimulating factor (filgrastim) for treatment of severe chronic neutropenia. Blood 1993, 81, 2496–2502. [Google Scholar] [CrossRef]
- Rosenberg, P.S.; Zeidler, C.; Bolyard, A.A.; Alter, B.P.; Bonilla, M.A.; Boxer, L.A.; Dror, Y.; Kinsey, S.; Link, D.C.; Newburger, P.E.; et al. Stable long-term risk of leukaemia in patients with severe congenital neutropenia maintained on G-CSF therapy. Br. J. Haematol. 2010, 150, 196–199. [Google Scholar] [CrossRef]
- Donadieu, J.; Leblanc, T.; Meunier, B.B.; Barkaoui, M.; Fenneteau, O.; Bertrand, Y.; Maier-Redelsperger, M.; Micheau, M.; Stephan, J.L.; Phillipe, N.; et al. Analysis of risk factors for myelodysplasias, leukemias and death from infection among patients with congenital neutropenia. Experience of the French Severe Chronic Neutropenia Study Group. Haematologica 2005, 90, 45–53. [Google Scholar] [PubMed]
- Zeidler, C.; Welte, K.; Barak, Y.; Barriga, F.; Bolyard, A.A.; Boxer, L.; Cornu, G.; Cowan, M.J.; Dale, D.C.; Flood, T.; et al. Stem cell transplantation in patients with severe congenital neutropenia without evidence of leukemic transformation. Blood 2000, 95, 1195–1198. [Google Scholar]
- Sakaguchi, H.; Yoshida, N. Recent advances in hematopoietic cell transplantation for inherited bone marrow failure syndromes. Int. J. Hematol. 2022, 116, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Manuela, G.; Matthias, B. CAMT-MPL: Congenital amegakaryocytic thrombocytopenia caused by MPL mutations—Heterogeneity of a monogenic disorder—A comprehensive analysis of 56 patients. Haematologica 2020, 106, 2439–2448. [Google Scholar] [CrossRef] [PubMed]
- Muraoka, K.; Ishii, E.; Tsuji, K.; Yamamoto, S.; Yamaguchi, H.; Hara, T.; Koga, H.; Nakahata, T.; Miyazaki, S. Defective response to thrombopoietin and impaired expression of c-mpl mRNA of bone marrow cells in congenital amegakaryocytic thrombocytopenia. Br. J. Haematol. 1997, 96, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Hirata, S.; Takayama, N.; Jono-Ohnishi, R.; Endo, H.; Nakamura, S.; Dohda, T.; Nishi, M.; Hamazaki, Y.; Ishii, E.; Kaneko, S.; et al. Congenital amegakaryocytic thrombocytopenia iPS cells exhibit defective MPL-mediated signaling. J. Clin. Investig. 2013, 123, 3802–3814. [Google Scholar] [CrossRef]
- Dasouki, M.J.; Rafi, S.K.; Olm-Shipman, A.J.; Wilson, N.R.; Abhyankar, S.; Ganter, B.; Furness, L.M.; Fang, J.; Calado, R.T.; Saadi, I. Exome sequencing reveals a thrombopoietin ligand mutation in a Micronesian family with autosomal recessive aplastic anemia. Blood 2013, 122, 3440–3449. [Google Scholar] [CrossRef]
- Dalle, J.-H.; Fahd, M. Allogenic Stem Cell Transplantation in Amegacaryocytosis: Results of a Retrospective Study in EBMT Centers. Biol. Blood Marrow Transplant. 2014, 20, S81–S82. [Google Scholar] [CrossRef]
- Mahadeo, K.M.; Tewari, P.; Parikh, S.H.; Driscoll, T.A.; Page, K.; Martin, P.L.; Kurtzberg, J.; Prasad, V.K. Durable engraftment and correction of hematological abnormalities in children with congenital amegakaryocytic thrombocytopenia following myeloablative umbilical cord blood transplantation. Pediatr. Transplant. 2015, 19, 753–757. [Google Scholar] [CrossRef]
- Woods, G.; Bajwa, R.P.; Rose, M.J. Reduced intensity transplantation for congenital amegakaryocytic thrombocytopenia: Report of a case and review of the literature. Pediatr. Transpl. 2014, 18, E31–E34. [Google Scholar] [CrossRef]
- Seo, A.; Ben-Harosh, M.; Sirin, M.; Stein, J.; Dgany, O.; Kaplelushnik, J.; Hoenig, M.; Pannicke, U.; Lorenz, M.; Schwarz, K.; et al. Bone marrow failure unresponsive to bone marrow transplant is caused by mutations in thrombopoietin. Blood 2017, 130, 875–880. [Google Scholar] [CrossRef]
- Pecci, A.; Ragab, I.; Bozzi, V.; De Rocco, D.; Barozzi, S.; Giangregorio, T.; Ali, H.; Melazzini, F.; Sallam, M.; Alfano, C.; et al. Thrombopoietin mutation in congenital amegakaryocytic thrombocytopenia treatable with romiplostim. EMBO Mol. Med. 2018, 10, 63–75. [Google Scholar] [CrossRef]
- Albers, C.A.; Paul, D.S.; Schulze, H.; Freson, K.; Stephens, J.C.; Smethurst, P.A.; Jolley, J.D.; Cvejic, A.; Kostadima, M.; Bertone, P.; et al. Compound inheritance of a low-frequency regulatory SNP and a rare null mutation in exon-junction complex subunit RBM8A causes TAR syndrome. Nat. Genet. 2012, 44, 435–439. [Google Scholar] [CrossRef]
- Hall, J.G.; Levin, J.; Kuhn, J.P.; Ottenheimer, E.J.; van Berkum, K.A.; McKusick, V.A. Thrombocytopenia with absent radius (TAR). Medicine 1969, 48, 411–439. [Google Scholar] [CrossRef] [PubMed]
- Cowan, J.; Parikh, T.; Waghela, R.; Mora, R. Thrombocytopenia with Absent Radii (TAR) Syndrome Without Significant Thrombocytopenia. Cureus 2020, 12, e10557. [Google Scholar] [CrossRef] [PubMed]
- Gallastegui, N.; Dudkiewicz, P.B.; Jy, W.; Horstman, L.L.; Ahn, Y.S. Romiplostim (Nplate®) and Oprelvekin (Neumega®) Correct Thrombocytopenia in TAR Syndrome (Thrombocytopenia with Absent Radii). Blood 2017, 130, 4953. [Google Scholar]
- Jameson-Lee, M.; Chen, K.; Ritchie, E.; Shore, T.; Al-Khattab, O.; Gergis, U. Acute myeloid leukemia in a patient with thrombocytopenia with absent radii: A case report and review of the literature. Hematol./Oncol. Stem Cell Ther. 2018, 11, 245–247. [Google Scholar] [CrossRef]
- Marsh, J.C.; Ball, S.E.; Cavenagh, J.; Darbyshire, P.; Dokal, I.; Gordon-Smith, E.C.; Keidan, J.; Laurie, A.; Martin, A.; Mercieca, J.; et al. Guidelines for the diagnosis and management of aplastic anaemia. Br. J. Haematol. 2009, 147, 43–70. [Google Scholar] [CrossRef] [PubMed]
- Antonio, M.R. (Auto-)immune signature in aplastic anemia. Haematologica 2018, 103, 747–749. [Google Scholar]
- Lin, F.C.; Karwan, M.; Saleh, B.; Hodge, D.L.; Chan, T.; Boelte, K.C.; Keller, J.R.; Young, H.A. IFN-γ causes aplastic anemia by altering hematopoietic stem/progenitor cell composition and disrupting lineage differentiation. Blood 2014, 124, 3699–3708. [Google Scholar] [CrossRef]
- de Latour, R.P.; Visconte, V.; Takaku, T.; Wu, C.; Erie, A.J.; Sarcon, A.K.; Desierto, M.J.; Scheinberg, P.; Keyvanfar, K.; Nunez, O.; et al. Th17 immune responses contribute to the pathophysiology of aplastic anemia. Blood 2010, 116, 4175–4184. [Google Scholar] [CrossRef]
- Kordasti, S.; Costantini, B.; Seidl, T.; Perez Abellan, P.; Martinez Llordella, M.; McLornan, D.; Diggins, K.E.; Kulasekararaj, A.; Benfatto, C.; Feng, X.; et al. Deep phenotyping of Tregs identifies an immune signature for idiopathic aplastic anemia and predicts response to treatment. Blood 2016, 128, 1193–1205. [Google Scholar] [CrossRef]
- Liu, S.; Li, Q.; Zhang, Y.; Li, Q.; Ye, B.; Wu, D.; Wu, L.; Lu, H.; Ji, C. Association of Human Leukocyte Antigen DRB1*15 and DRB1*15:01 Polymorphisms with Response to Immunosuppressive Therapy in Patients with Aplastic Anemia: A Meta-Analysis. PLoS ONE 2016, 11, e0162382. [Google Scholar] [CrossRef]
- Narita, A.; Muramatsu, H.; Okuno, Y.; Sekiya, Y.; Suzuki, K.; Hamada, M.; Kataoka, S.; Taniguchi, R.; Ichikawa, D.; Murakami, N.; et al. Development of Paroxysmal Nocturnal Hemoglobinuria in Children with Aplastic Anemia. Blood 2016, 128, 1499. [Google Scholar] [CrossRef]
- Urbano-Ispizua, Á.; Kulasekararaj, A.G.; Bartels, M.; Patriquin, C.J.; Hoechsmann, B.; Maschan, A.A.; Wilson, A.; Gustovic, P.; Schrezenmeier, H. Efficacy of Eculizumab in Pediatric Patients with Paroxysmal Nocturnal Hemoglobinuria in the International PNH Registry. Blood 2018, 132, 3614. [Google Scholar] [CrossRef]
- Hillmen, P.; Szer, J.; Weitz, I.; Röth, A.; Höchsmann, B.; Panse, J.; Usuki, K.; Griffin, M.; Kiladjian, J.-J.; de Castro, C.; et al. Pegcetacoplan versus Eculizumab in Paroxysmal Nocturnal Hemoglobinuria. N. Engl. J. Med. 2021, 384, 1028–1037. [Google Scholar] [CrossRef] [PubMed]
- Röth, A.; Rottinghaus, S.T.; Hill, A.; Bachman, E.S.; Kim, J.S.; Schrezenmeier, H.; Terriou, L.; Urbano-Ispizua, Á.; Wells, R.A.; Jang, J.H.; et al. Ravulizumab (ALXN1210) in patients with paroxysmal nocturnal hemoglobinuria: Results of 2 phase 1b/2 studies. Blood Adv. 2018, 2, 2176–2185. [Google Scholar] [CrossRef]
- Dufour, C.; Veys, P.; Carraro, E.; Bhatnagar, N.; Pillon, M.; Wynn, R.; Gibson, B.; Vora, A.J.; Steward, C.G.; Ewins, A.M.; et al. Similar outcome of upfront-unrelated and matched sibling stem cell transplantation in idiopathic paediatric aplastic anaemia. A study on behalf of the UK Paediatric BMT Working Party, Paediatric Diseases Working Party and Severe Aplastic Anaemia Working Party of EBMT. Br. J. Haematol. 2015, 171, 585–594. [Google Scholar] [PubMed]
- Young, M.E.; Potter, V.; Kulasekararaj, A.G.; Mufti, G.J.; Marsh, J.C. Haematopoietic stem cell transplantation for acquired aplastic anaemia. Curr. Opin. Hematol. 2013, 20, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Townsley, D.M.; Scheinberg, P.; Winkler, T.; Desmond, R.; Dumitriu, B.; Rios, O.; Weinstein, B.; Valdez, J.; Lotter, J.; Feng, X.; et al. Eltrombopag Added to Standard Immunosuppression for Aplastic Anemia. N. Engl. J. Med. 2017, 376, 1540–1550. [Google Scholar] [CrossRef]
- Peffault de Latour, R.; Kulasekararaj, A.; Iacobelli, S.; Terwel, S.R.; Cook, R.; Griffin, M.; Halkes, C.J.M.; Recher, C.; Barraco, F.; Forcade, E.; et al. Eltrombopag Added to Immunosuppression in Severe Aplastic Anemia. N. Engl. J. Med. 2022, 386, 11–23. [Google Scholar] [CrossRef]
- Yoshida, N.; Kobayashi, R.; Yabe, H.; Kosaka, Y.; Yagasaki, H.; Watanabe, K.; Kudo, K.; Morimoto, A.; Ohga, S.; Muramatsu, H.; et al. First-line treatment for severe aplastic anemia in children: Bone marrow transplantation from a matched family donor versus immunosuppressive therapy. Haematologica 2014, 99, 1784–1791. [Google Scholar] [CrossRef]
- Dufour, C.; Pillon, M.; Sociè, G.; Rovò, A.; Carraro, E.; Bacigalupo, A.; Oneto, R.; Passweg, J.; Risitano, A.; Tichelli, A.; et al. Outcome of aplastic anaemia in children. A study by the severe aplastic anaemia and paediatric disease working parties of the European group blood and bone marrow transplant. Br. J. Haematol. 2015, 169, 565–573. [Google Scholar] [CrossRef]
- Locasciulli, A.; Oneto, R.; Bacigalupo, A.; Socié, G.; Korthof, E.; Bekassy, A.; Schrezenmeier, H.; Passweg, J.; Führer, M. Outcome of patients with acquired aplastic anemia given first line bone marrow transplantation or immunosuppressive treatment in the last decade: A report from the European Group for Blood and Marrow Transplantation (EBMT). Haematologica 2007, 92, 11–18. [Google Scholar] [CrossRef]
- Schrezenmeier, H.; Passweg, J.R.; Marsh, J.C.; Bacigalupo, A.; Bredeson, C.N.; Bullorsky, E.; Camitta, B.M.; Champlin, R.E.; Gale, R.P.; Fuhrer, M.; et al. Worse outcome and more chronic GVHD with peripheral blood progenitor cells than bone marrow in HLA-matched sibling donor transplants for young patients with severe acquired aplastic anemia. Blood 2007, 110, 1397–1400. [Google Scholar] [CrossRef]
- Bacigalupo, A.; Socié, G.; Schrezenmeier, H.; Tichelli, A.; Locasciulli, A.; Fuehrer, M.; Risitano, A.M.; Dufour, C.; Passweg, J.R.; Oneto, R.; et al. Bone marrow versus peripheral blood as the stem cell source for sibling transplants in acquired aplastic anemia: Survival advantage for bone marrow in all age groups. Haematologica 2012, 97, 1142–1148. [Google Scholar] [CrossRef]
- Bejanyan, N.; Kim, S.; Hebert, K.M.; Kekre, N.; Abdel-Azim, H.; Ahmed, I.; Aljurf, M.; Badawy, S.M.; Beitinjaneh, A.; Boelens, J.J.; et al. Choice of conditioning regimens for bone marrow transplantation in severe aplastic anemia. Blood Adv. 2019, 3, 3123–3131. [Google Scholar] [CrossRef]
- Bacigalupo, A.; Socié, G.; Hamladji, R.M.; Aljurf, M.; Maschan, A.; Kyrcz-Krzemien, S.; Cybicka, A.; Sengelov, H.; Unal, A.; Beelen, D.; et al. Current outcome of HLA identical sibling versus unrelated donor transplants in severe aplastic anemia: An EBMT analysis. Haematologica 2015, 100, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zheng, X.; Yan, H.; Li, D.; Wang, H. Good outcome of haploidentical hematopoietic SCT as a salvage therapy in children and adolescents with acquired severe aplastic anemia. Bone Marrow Transpl. 2014, 49, 1481–1485. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.P.; Liu, K.Y.; Liu, D.H.; Han, W.; Chen, H.; Chen, Y.H.; Zhang, X.H.; Wang, Y.; Wang, F.R.; Wang, J.Z.; et al. A novel protocol for haploidentical hematopoietic SCT without in vitro T-cell depletion in the treatment of severe acquired aplastic anemia. Bone Marrow Transpl. 2012, 47, 1507–1512. [Google Scholar] [CrossRef]
- Gao, L.; Li, Y.; Zhang, Y.; Chen, X.; Gao, L.; Zhang, C.; Liu, Y.; Kong, P.; Wang, Q.; Su, Y.; et al. Long-term outcome of HLA-haploidentical hematopoietic SCT without in vitro T-cell depletion for adult severe aplastic anemia after modified conditioning and supportive therapy. Bone Marrow Transpl. 2014, 49, 519–524. [Google Scholar] [CrossRef]
- Zhang, Y.; Guo, Z.; Liu, X.D.; He, X.P.; Yang, K.; Chen, P.; Chen, H.R. Comparison of Haploidentical Hematopoietic Stem Cell Transplantation and Immunosuppressive Therapy for the Treatment of Acquired Severe Aplastic Anemia in Pediatric Patients. Am. J. Ther. 2017, 24, e196–e201. [Google Scholar] [CrossRef]
- Xu, L.P.; Jin, S.; Wang, S.Q.; Xia, L.H.; Bai, H.; Gao, S.J.; Liu, Q.F.; Wang, J.M.; Wang, X.; Jiang, M.; et al. Upfront haploidentical transplant for acquired severe aplastic anemia: Registry-based comparison with matched related transplant. J. Hematol. Oncol. 2017, 10, 25. [Google Scholar] [CrossRef] [PubMed]
- Kudo, K.; Muramatsu, H.; Narita, A.; Yoshida, N.; Kobayashi, R.; Yabe, H.; Endo, M.; Inoue, M.; Hara, J.; Kounami, S.; et al. Unrelated cord blood transplantation in aplastic anemia: Is anti-thymocyte globulin indispensable for conditioning? Bone Marrow Transplant. 2017, 52, 1659–1661. [Google Scholar] [CrossRef] [PubMed]
- Niemeyer, C.M.; Baumann, I. Classification of Childhood Aplastic Anemia and Myelodysplastic Syndrome. Hematology 2011, 2011, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Khoury, J.D.; Solary, E.; Abla, O.; Akkari, Y.; Alaggio, R.; Apperley, J.F.; Bejar, R.; Berti, E.; Busque, L.; Chan, J.K.C.; et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia 2022, 36, 1703–1719. [Google Scholar] [CrossRef] [PubMed]
- Kardos, G.; Baumann, I.; Passmore, S.J.; Locatelli, F.; Hasle, H.; Schultz, K.R.; Starý, J.; Schmitt-Graeff, A.; Fischer, A.; Harbott, J.; et al. Refractory anemia in childhood: A retrospective analysis of 67 patients with particular reference to monosomy 7. Blood 2003, 102, 1997–2003. [Google Scholar] [CrossRef]
- Sahoo, S.S.; Kozyra, E.J.; Wlodarski, M.W. Germline predisposition in myeloid neoplasms: Unique genetic and clinical features of GATA2 deficiency and SAMD9/SAMD9L syndromes. Best. Pract. Res. Clin. Haematol. 2020, 33, 101197. [Google Scholar] [CrossRef]
- Starý, J.; Locatelli, F.; Niemeyer, C.M.; on behalf of the European Working Group on Myelodysplastic Syndrome (EWOG-MDS); Pediatric Diseases Working Party of the EBMT. Stem cell transplantation for aplastic anemia and myelodysplastic syndrome. Bone Marrow Transplant. 2005, 35, S13–S16. [Google Scholar] [CrossRef]
- Strahm, B.; Locatelli, F.; Bader, P.; Ehlert, K.; Kremens, B.; Zintl, F.; Führer, M.; Stachel, D.; Sykora, K.W.; Sedlacek, P.; et al. Reduced intensity conditioning in unrelated donor transplantation for refractory cytopenia in childhood. Bone Marrow Transplant. 2007, 40, 329–333. [Google Scholar] [CrossRef]
- Strahm, B.; Albert, M.; Bierings, M.; Bordon, V.; Burkhardt, B.; Catala, A.; DeMoerloose, B.; Dworzak, M.; Halse, H.; Kremens, B.; et al. EWOG-MDS study SCT RC RIC 06: Reduced intensity conditioning for children and adolescents with refractory cytopenia of childhood. Bone Marrow Transpl. 2017, 52, S103. [Google Scholar]
- EWOG-MDS. Guidelines for Hematopoietic Stem Cell Transplantation (HSCT) in Childhood MDS and JMML for Patients enrolled in EWOG-MDS Studies. In Proceedings of the EWOG-MDS Consensus Conference, Freiburg, Germany, 25–26 October 2016. Version 1.3. [Google Scholar]
- Strahm, B.; Nöllke, P.; Zecca, M.; Korthof, E.T.; Bierings, M.; Furlan, I.; Sedlacek, P.; Chybicka, A.; Schmugge, M.; Bordon, V.; et al. Hematopoietic stem cell transplantation for advanced myelodysplastic syndrome in children: Results of the EWOG-MDS 98 study. Leukemia 2011, 25, 455–462. [Google Scholar] [CrossRef]
- Choijilsuren, H.B.; Park, Y.; Jung, M. Mechanisms of somatic transformation in inherited bone marrow failure syndromes. Hematol. Am. Soc. Hematol. Educ. Program. 2021, 2021, 390–398. [Google Scholar] [CrossRef]
- Davidsson, J.; Puschmann, A.; Tedgård, U.; Bryder, D.; Nilsson, L.; Cammenga, J. SAMD9 and SAMD9L in inherited predisposition to ataxia, pancytopenia, and myeloid malignancies. Leukemia 2018, 32, 1106–1115. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.; Ariagno, S.; Kohorst, M.A. Pediatric Germline Predisposition to Myeloid Neoplasms. Curr. Hematol. Malig. Rep. 2022, 17, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.H.; Below, J.E.; Shimamura, A.; Keel, S.B.; Matsushita, M.; Wolff, J.; Sul, Y.; Bonkowski, E.; Castella, M.; Taniguchi, T.; et al. Ataxia-Pancytopenia Syndrome Is Caused by Missense Mutations in SAMD9L. Am. J. Hum. Genet. 2016, 98, 1146–1158. [Google Scholar] [CrossRef] [PubMed]
- Tesi, B.; Davidsson, J.; Voss, M.; Rahikkala, E.; Holmes, T.D.; Chiang, S.C.C.; Komulainen-Ebrahim, J.; Gorcenco, S.; Rundberg Nilsson, A.; Ripperger, T.; et al. Gain-of-function SAMD9L mutations cause a syndrome of cytopenia, immunodeficiency, MDS, and neurological symptoms. Blood 2017, 129, 2266–2279. [Google Scholar] [CrossRef]
- Schwartz, J.R.; Wang, S.; Ma, J.; Lamprecht, T.; Walsh, M.; Song, G.; Raimondi, S.C.; Wu, G.; Walsh, M.F.; McGee, R.B.; et al. Germline SAMD9 mutation in siblings with monosomy 7 and myelodysplastic syndrome. Leukemia 2017, 31, 1827–1830. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, G.; Thrasher, A.J.; Aiuti, A. Gene therapy using haematopoietic stem and progenitor cells. Nat. Rev. Genet. 2021, 22, 216–234. [Google Scholar] [CrossRef] [PubMed]
- Kohn, D.B. Gene therapy for blood diseases. Curr. Opin. Biotechnol. 2019, 60, 39–45. [Google Scholar] [CrossRef]
- Dufait, I.; Liechtenstein, T.; Lanna, A.; Bricogne, C.; Laranga, R.; Padella, A.; Breckpot, K.; Escors, D. Retroviral and lentiviral vectors for the induction of immunological tolerance. Scientifica 2012, 2012, 694137. [Google Scholar] [CrossRef] [PubMed]
- Daniel-Moreno, A.; Lamsfus-Calle, A.; Raju, J.; Antony, J.S.; Handgretinger, R.; Mezger, M. CRISPR/Cas9-modified hematopoietic stem cells—Present and future perspectives for stem cell transplantation. Bone Marrow Transplant. 2019, 54, 1940–1950. [Google Scholar] [CrossRef]
- Uddin, F.; Rudin, C.M.; Sen, T. CRISPR Gene Therapy: Applications, Limitations, and Implications for the Future. Front. Oncol. 2020, 10, 1387. [Google Scholar] [CrossRef]
- Río, P.; Navarro, S.; Wang, W.; Sánchez-Domínguez, R.; Pujol, R.M.; Segovia, J.C.; Bogliolo, M.; Merino, E.; Wu, N.; Salgado, R.; et al. Successful engraftment of gene-corrected hematopoietic stem cells in non-conditioned patients with Fanconi anemia. Nat. Med. 2019, 25, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Adair, J.E.; Becker, P.S.; Chandrasekaran, D.; Choi, G.; Woolfrey, A.E.; Burroughs, L.; Kiem, H.-P. Gene Therapy for Fanconi Anemia in Seattle: Clinical Experience and Next Steps. Blood 2016, 128, 3510. [Google Scholar] [CrossRef]
- Osborn, M.; Lonetree, C.L.; Webber, B.R.; Patel, D.; Dunmire, S.; McElroy, A.N.; DeFeo, A.P.; MacMillan, M.L.; Wagner, J.; Balzar, B.R.; et al. CRISPR/Cas9 Targeted Gene Editing and Cellular Engineering in Fanconi Anemia. Stem Cells Dev. 2016, 25, 1591–1603. [Google Scholar] [CrossRef] [PubMed]
- Skvarova Kramarzova, K.; Osborn, M.J.; Webber, B.R.; DeFeo, A.P.; McElroy, A.N.; Kim, C.J.; Tolar, J. CRISPR/Cas9-Mediated Correction of the FANCD1 Gene in Primary Patient Cells. Int. J. Mol. Sci. 2017, 18, 1269. [Google Scholar] [CrossRef]
- Malouf, C.; Loughran, S.J.; Wilkinson, A.C.; Shimamura, A.; Río, P. Translational research for bone marrow failure patients. Exp. Hematol. 2022, 105, 18–21. [Google Scholar] [CrossRef]
- Román-Rodríguez, F.J.; Ugalde, L.; Álvarez, L.; Díez, B.; Ramírez, M.J.; Risueño, C.; Cortón, M.; Bogliolo, M.; Bernal, S.; March, F.; et al. NHEJ-Mediated Repair of CRISPR-Cas9-Induced DNA Breaks Efficiently Corrects Mutations in HSPCs from Patients with Fanconi Anemia. Cell Stem Cell 2019, 25, 607–621.e7. [Google Scholar] [CrossRef]
- Myers, K.C.; Davies, S.M.; Lutzko, C.; Wahle, R.; Aubert, G.; Amano, T.; Amano, M.; Yu, H.; Ko, M.S.H. Successful Ex Vivo Telomere Elongation with Exg-001 in a Patient with a Dyskeratosis Congenita. Blood 2022, 140, 1895–1896. [Google Scholar] [CrossRef]
- Flygare, J.; Olsson, K.; Richter, J.; Karlsson, S. Gene therapy of Diamond Blackfan anemia CD34+ cells leads to improved erythroid development and engraftment following transplantation. Exp. Hematol. 2008, 36, 1428–1435. [Google Scholar] [CrossRef]
- Liu, Y.; Dahl, M.; Debnath, S.; Rothe, M.; Smith, E.M.; Grahn, T.H.M.; Warsi, S.; Chen, J.; Flygare, J.; Schambach, A.; et al. Successful gene therapy of Diamond-Blackfan anemia in a mouse model and human CD34+ cord blood hematopoietic stem cells using a clinically applicable lentiviral vector. Haematologica 2022, 107, 446–456. [Google Scholar] [CrossRef]
- Lannutti, B.J.; Epp, A.; Roy, J.; Chen, J.; Josephson, N.C. Incomplete restoration of Mpl expression in the mpl−/− mouse produces partial correction of the stem cell-repopulating defect and paradoxical thrombocytosis. Blood 2009, 113, 1778–1785. [Google Scholar] [CrossRef]
- Heckl, D.; Wicke, D.C.; Brugman, M.H.; Meyer, J.; Schambach, A.; Büsche, G.; Ballmaier, M.; Baum, C.; Modlich, U. Lentiviral gene transfer regenerates hematopoietic stem cells in a mouse model for Mpl-deficient aplastic anemia. Blood 2011, 117, 3737–3747. [Google Scholar] [CrossRef] [PubMed]
- Cleyrat, C.; Girard, R.; Choi, E.H.; Jeziorski, É.; Lavabre-Bertrand, T.; Hermouet, S.; Carillo, S.; Wilson, B.S. Gene editing rescue of a novel MPL mutant associated with congenital amegakaryocytic thrombocytopenia. Blood Adv. 2017, 1, 1815–1826. [Google Scholar] [CrossRef]
- Rao, S.; Brito-Frazao, J.; Serbin, A.V.; Yao, Q.; Luk, K.; Wu, Y.; Zeng, J.; Ren, C.; Watkinson, R.; Armant, M.; et al. Gene Editing ELANE in Human Hematopoietic Stem and Progenitor Cells Reveals Disease Mechanisms and Therapeutic Strategies for Severe Congenital Neutropenia. Blood 2019, 134, 3. [Google Scholar] [CrossRef]
- Farajifard, H.; Zavvar, M.; Rajaei, T.; Noorbakhsh, F.; Nikougoftar-zarif, M.; Azadmanesh, K.; Kompani, F.; Rezaei, N. In vitro study of HAX1 gene therapy by retro viral transduction as a therapeutic target in severe congenital neutropenia. Eur. Cytokine Netw. 2018, 29, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Tran, N.T.; Graf, R.; Wulf-Goldenberg, A.; Stecklum, M.; Strauß, G.; Kühn, R.; Kocks, C.; Rajewsky, K.; Chu, V.T. CRISPR-Cas9-Mediated ELANE Mutation Correction in Hematopoietic Stem and Progenitor Cells to Treat Severe Congenital Neutropenia. Mol. Ther. 2020, 28, 2621–2634. [Google Scholar] [CrossRef] [PubMed]
- Morishima, T.; Watanabe, K.; Niwa, A.; Hirai, H.; Saida, S.; Tanaka, T.; Kato, I.; Umeda, K.; Hiramatsu, H.; Saito, M.K.; et al. Genetic correction of HAX1 in induced pluripotent stem cells from a patient with severe congenital neutropenia improves defective granulopoiesis. Haematologica 2014, 99, 19–27. [Google Scholar] [CrossRef] [PubMed]
| Disorder | Main Hematological Manifestation | Drug Based Treatment | Cellular Therapy |
|---|---|---|---|
| Fanconi anemia | Pancytopenia | Supportive care, androgens | HSCT, gene therapy trials ongoing (NCT01331018, NCT03351868, NCT00272857, NCT03157804, NCT04069533, NCT00001399) |
| Telomere biology disorders (mainly dyskeratosis congenita) | Pancytopenia | Androgen therapy, e.g., danazol 1 | HSCT, gene therapy at single case level (NCT04211714) |
| Diamond–Blackfan anemia syndrome | Anemia | <1 year: transfusions >1 year: + chelation therapy, steroids, e.g., prednisone | HSCT, gene therapy trials expected soon |
| Schwachman–Diamond syndrome | Neutropenia | Supportive care, G-CSF | HSCT |
| Severe congenital neutropenia | Neutropenia | Supportive care, G-CSF | HSCT |
| Congenital amegakaryocytic thrombocytopenia | Thrombocytopenia | - | HSCT |
| Thrombocytopenia absent radii | Thrombocytopenia | Platelet transfusions Platelet-stimulating agents, e.g., romiplostim and oprelvekin | HSCT |
| Aplastic anemia | Pancytopenia | IST + Epag | HSCT |
| Childhood MDS with low blasts | Multilineage dysplasia | IST | HSCT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vissers, L.T.W.; van der Burg, M.; Lankester, A.C.; Smiers, F.J.W.; Bartels, M.; Mohseny, A.B. Pediatric Bone Marrow Failure: A Broad Landscape in Need of Personalized Management. J. Clin. Med. 2023, 12, 7185. https://doi.org/10.3390/jcm12227185
Vissers LTW, van der Burg M, Lankester AC, Smiers FJW, Bartels M, Mohseny AB. Pediatric Bone Marrow Failure: A Broad Landscape in Need of Personalized Management. Journal of Clinical Medicine. 2023; 12(22):7185. https://doi.org/10.3390/jcm12227185
Chicago/Turabian StyleVissers, Lotte T. W., Mirjam van der Burg, Arjan C. Lankester, Frans J. W. Smiers, Marije Bartels, and Alexander B. Mohseny. 2023. "Pediatric Bone Marrow Failure: A Broad Landscape in Need of Personalized Management" Journal of Clinical Medicine 12, no. 22: 7185. https://doi.org/10.3390/jcm12227185





