The Relationship between Hypertension and Periodontitis: A Cross-Sectional Study
Abstract
:1. Introduction
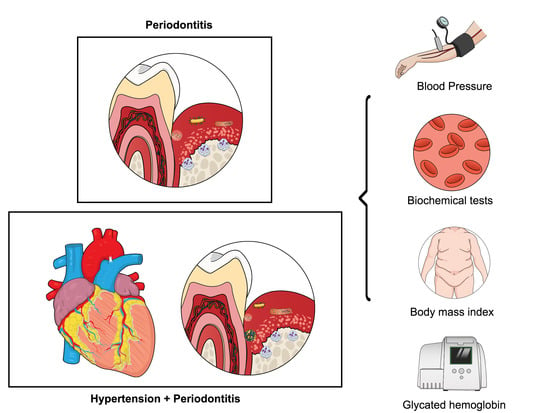
2. Materials and Methods
2.1. Experimental Design
2.2. Sample Calculation
2.3. Sample Selection
2.4. Physical Examination
2.5. Periodontal Exam
2.6. Biochemical Analysis
2.7. Examiner Calibration
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Virdis, A.; Dell’Agnello, U.; Taddei, S. Impact of inflammation on vascular disease in hypertension. Maturitas 2014, 78, 179–183. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [Green Version]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Munoz Aguilera, E.; Suvan, J.; Buti, J.; Czesnikiewicz-Guzik, M.; Ribeiro, A.B.; Orlandi, M.; Guzik, T.J.; Hingorani, A.D.; Nart, J.; D’Aiuto, F. Periodontitis is associated with hypertension: A systematic review and meta-analysis. Cardiovasc. Res. 2020, 116, 28–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munoz Aguilera, E.; Suvan, J.; Orlandi, M.; Catalina, Q.M.; Nart, J.; D’Aiuto, F. Association Between Periodontitis and Blood Pressure Highlighted in Systemically Healthy Individuals: Results From a Nested Case-Control Study. Hypertension 2021, 77, 1765–1774. [Google Scholar] [CrossRef]
- Czesnikiewicz-Guzik, M.; Osmenda, G.; Siedlinski, M.; Nosalski, R.; Pelka, P.; Nowakowski, D.; Wilk, G.; Mikolajczyk, T.P.; Schramm-Luc, A.; Furtak, A.; et al. Causal association between periodontitis and hypertension: Evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur. Heart J. 2019, 40, 3459–3470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin-Cabezas, R.; Seelam, N.; Petit, C.; Agossa, K.; Gaertner, S.; Tenenbaum, H.; Davideau, J.L.; Huck, O. Association between periodontitis and arterial hypertension: A systematic review and meta-analysis. Am. Heart J. 2016, 180, 98–112. [Google Scholar] [CrossRef]
- Sanz, M.; Del Castillo, A.M.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and Cardiovascular Diseases: Consensus Report. Glob. Heart 2020, 15, 1023–1027. [Google Scholar] [CrossRef] [Green Version]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. 1), S173–S182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dyke, T.E.; Bartold, P.M.; Reynolds, E.C. The Nexus Between Periodontal Inflammation and Dysbiosis. Front. Immunol. 2020, 11, 511. [Google Scholar] [CrossRef] [PubMed]
- Cao, R.; Li, Q.; Wu, Q.; Yao, M.; Chen, Y.; Zhou, H. Effect of non-surgical periodontal therapy on glycemic control of type 2 diabetes mellitus: A systematic review and Bayesian network meta-analysis. BMC Oral Health 2019, 19, 176. [Google Scholar] [CrossRef]
- Ferreira, M.C.; Dias-Pereira, A.C.; Branco-de-Almeida, L.S.; Martins, C.C.; Paiva, S.M. Impact of periodontal disease on quality of life: A systematic review. J. Periodontal Res. 2017, 52, 651–665. [Google Scholar] [CrossRef]
- de Molon, R.S.; Rossa, C., Jr.; Thurlings, R.M.; Cirelli, J.A.; Koenders, M.I. Linkage of Periodontitis and Rheumatoid Arthritis: Current Evidence and Potential Biological Interactions. Int. J. Mol. Sci. 2019, 20, 4541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J.; et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. 1), S237–S248. [Google Scholar] [CrossRef] [PubMed]
- Del Pinto, R.; Pietropaoli, D.; Munoz-Aguilera, E.; D’Aiuto, F.; Czesnikiewicz-Guzik, M.; Monaco, A.; Guzik, T.J.; Ferri, C. Periodontitis and Hypertension: Is the Association Causal? High Blood Press. Cardiovasc. Prev. 2020, 27, 281–289. [Google Scholar] [CrossRef]
- Khocht, A.; Rogers, T.; Janal, M.N.; Brown, M. Gingival Fluid Inflammatory Biomarkers and Hypertension in African Americans. JDR Clin. Trans. Res. 2017, 2, 269–277. [Google Scholar] [CrossRef] [Green Version]
- de Medeiros Vanderlei, J.M.; Messora, M.R.; Fernandes, P.G.; Novaes, A.B., Jr.; Palioto, D.B.; Grisi, M.F.M.; Souza, S.L.S.; Gerlach, R.F.; Antoniali, C.; Taba, M., Jr. Arterial hypertension perpetuates alveolar bone loss. Clin. Exp. Hypertens. 2013, 35, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Czesnikiewicz-Guzik, M.; Nosalski, R.; Mikolajczyk, T.P.; Vidler, F.; Dohnal, T.; Dembowska, E.; Graham, D.; Harrison, D.G.; Guzik, T.J. Th1-type immune responses to Porphyromonas gingivalis antigens exacerbate angiotensin II-dependent hypertension and vascular dysfunction. Br. J. Pharmacol. 2019, 176, 1922–1931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidal, F.; Figueredo, C.M.; Cordovil, I.; Fischer, R.G. Higher prevalence of periodontitis in patients with refractory arterial hypertension: A case-control study. Oral Dis. 2011, 17, 560–563. [Google Scholar] [CrossRef]
- Buhlin, K.; Gustafsson, A.; Pockley, A.G.; Frostegard, J.; Klinge, B. Risk factors for cardiovascular disease in patients with periodontitis. Eur. Heart J. 2003, 24, 2099–2107. [Google Scholar] [CrossRef] [Green Version]
- Paddmanabhan, P.; Gita, B.; Chandrasekaran, S.C. Association between chronic periodontitis and hypertension in South Indian population: A cross-sectional study. J. Pharm. Bioallied Sci. 2015, 7, S543–S547. [Google Scholar] [CrossRef]
- Rodrigues, J.V.S.; Cláudio, M.M.; Franciscon, J.P.S.; Cabrera-Rosa, R.A.; Cirelli, T.; De Molon, R.S.; Figueredo, C.M.; Garcia, V.G.; Theodoro, L.H. The Effect of Non-Surgical Periodontal Treatment on Patients with Combined Refractory Arterial Hypertension and Stage III, Grade B Periodontitis: A Preliminary Prospective Clinical Study. J. Clin. Med. 2023, 12, 4277. [Google Scholar] [CrossRef]
- Lwanga, S.K.; Lemeshow, S. Sample Size Determination in Health Studies: A Practical Manual; World Health Organization: Geneva, Switzerland, 1991; p. 80. [Google Scholar]
- Cao, Q.; Yu, S.; Xiong, W.; Li, Y.; Li, H.; Li, J.; Li, F. Waist-hip ratio as a predictor of myocardial infarction risk: A systematic review and meta-analysis. Medicine 2018, 97, e11639. [Google Scholar] [CrossRef]
- Kablak-Ziembicka, A.; Przewlocki, T.; Sokolowski, A.; Tracz, W.; Podolec, P. Carotid intima-media thickness, hs-CRP and TNF-alpha are independently associated with cardiovascular event risk in patients with atherosclerotic occlusive disease. Atherosclerosis 2011, 214, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Theodoro, L.H.; Lopes, A.B.; Nuernberg, M.A.A.; Cláudio, M.M.; Miessi, D.M.J.; Alves, M.L.F.; Duque, C.; Mombelli, A.; Garcia, V.G. Comparison of repeated applications of aPDT with amoxicillin and metronidazole in the treatment of chronic periodontitis: A short-term study. J. Photochem. Photobiol. B 2017, 174, 364–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89 (Suppl. 1), S159–S172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosadurga, R.; Kyaw Soe, H.H.; Peck Lim, A.T.; Adl, A.; Mathew, M. Association between tooth loss and hypertension: A cross-sectional study. J. Fam. Med. Prim. Care 2020, 9, 925–932. [Google Scholar] [CrossRef]
- Peres, M.A.; Tsakos, G.; Barbato, P.R.; Silva, D.A.S.; Peres, K.G. Tooth loss is associated with increased blood pressure in adults—A multidisciplinary population-based study. J. Clin. Periodontol. 2012, 39, 824–833. [Google Scholar] [CrossRef]
- Volzke, H.; Schwahn, C.; Dorr, M.; Schwarz, S.; Robinson, D.; Dören, M.; Rettig, R.; Felix, S.B.; John, U.; Kocher, T. Gender differences in the relation between number of teeth and systolic blood pressure. J. Hypertens. 2006, 24, 1257–1263. [Google Scholar] [CrossRef]
- Pejcic, A.; Kostic, M.; Marko, I.; Obradovic, R.; Minic, I.; Bradic-Vasic, M.; Gligorijevic, N.; Kurtagic, D. Tooth loss and periodontal status in patients with cardiovascular disease in the Serbian population: A randomized prospective study. Int. J. Dent. Hyg. 2023, 21, 317–327. [Google Scholar] [CrossRef]
- Al-Ahmad, B.E.M.; Kashmoola, M.A.; Mustafa, N.S.; Hassan, H.; Arzmi, M.H. The relationship between tooth loss, body mass index, and hypertension in postmenopausal female. Eur. J. Dent. 2018, 12, 120–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietropaoli, D.; Del Pinto, R.; Ferri, C.; Wright Jr, J.T.; Giannoni, M.; Ortu, E.; Monaco, A. Poor Oral Health and Blood Pressure Control Among US Hypertensive Adults. Hypertension 2018, 72, 1365–1373. [Google Scholar] [CrossRef] [PubMed]
- Munoz Aguilera, E.; Leira, Y.; Miro Catalina, Q.; Orlandi, M.; Czesnikiewicz-Guzik, M.; Guzik, T.J.; Hingorani, A.D.; Nart, J.; D’Aiuto, F. Is systemic inflammation a missing link between periodontitis and hypertension? Results from two large population-based surveys. J. Intern Med. 2021, 289, 532–546. [Google Scholar] [CrossRef] [PubMed]
- Santos, C.F.; Morandini, A.C.; Dionisio, T.J.; Faria, F.A.; Lima, M.C.; Figueiredo, C.M.; Colombini-Ishikiriama, B.L.; Sipert, C.R.; Maciel, R.P.; Akashi, A.P.; et al. Functional Local Renin-Angiotensin System in Human and Rat Periodontal Tissue. PLoS ONE 2015, 10, e0134601. [Google Scholar] [CrossRef]
- Araujo, A.A.; Souza, T.O.; Moura, L.M.; Brito, G.A.C.; Aragão, K.S.; Araújo, L.S.; Medeiros, C.A.X.; Alves, M.S.C.F.; Araújo Jr, R.F. Effect of telmisartan on levels of IL-1, TNF-alpha, down-regulated COX-2, MMP-2, MMP-9 and RANKL/RANK in an experimental periodontitis model. J. Clin. Periodontol. 2013, 40, 1104–1111. [Google Scholar] [CrossRef] [Green Version]
- Brito, V.G.B.; Patrocinio, M.S.; de Sousa, M.C.L.; Barreto, A.E.A.; Frasnelli, S.C.T.; Lara, V.S.; Santos, C.F.; Oliveira, S.H.P. Telmisartan Prevents Alveolar Bone Loss by Decreasing the Expression of Osteoclasts Markers in Hypertensive Rats with Periodontal Disease. Front. Pharmacol. 2020, 11, 579926. [Google Scholar] [CrossRef]
- Paraskevas, S.; Huizinga, J.D.; Loos, B.G. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J. Clin. Periodontol. 2008, 35, 277–290. [Google Scholar] [CrossRef] [PubMed]
- Yuan, M.; Wang, B.; Tan, S. Mecobalamin and early functional outcomes of ischemic stroke patients with H-type hypertension. Rev. Assoc. Med. Bras. (1992) 2018, 64, 428–432. [Google Scholar] [CrossRef]
- Amar, S.; Gokce, N.; Morgan, S.; Looukideli, M.; Van Dyke, T.E.; Vita, J.A. Periodontal disease is associated with brachial artery endothelial dysfunction and systemic inflammation. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 1245–1249. [Google Scholar] [CrossRef] [Green Version]
- Houcken, W.; Teeuw, W.J.; Bizzarro, S.; Rodriguez, E.A.; Mulders, T.A.; Van Den Born, B.J.H.; Loos, B.G. Arterial stiffness in periodontitis patients and controls. A case-control and pilot intervention study. J. Hum. Hypertens. 2016, 30, 24–29. [Google Scholar] [CrossRef]
- Sasaki, N.; Ozono, R.; Higashi, Y.; Maeda, R.; Kihara, Y. Association of Insulin Resistance, Plasma Glucose Level, and Serum Insulin Level With Hypertension in a Population With Different Stages of Impaired Glucose Metabolism. J. Am. Heart Assoc. 2020, 9, e015546. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Omran, J.; Mehra, A.; Ardhanari, S. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog. Cardiovasc. Dis. 2014, 56, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Qi, Y.; Zheng, Z.; Wang, Y.; Zhang, X.Y.; Li, H.J.; Liu, H.H.; Zhang, X.T.; Du, J.; Liu, J. Dietary factors associated with hypertension. Nat. Rev. Cardiol. 2011, 8, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Tsakos, G.; Sabbah, W.; Hingorani, A.D.; Netuveli, G.; Donos, N.; Watt, R.G.; D’Aiuto, F. Is periodontal inflammation associated with raised blood pressure? Evidence from a National US survey. J. Hypertens. 2010, 28, 2386–2393. [Google Scholar] [CrossRef] [PubMed]

| Hypertension | Non-Hypertension | p-Value | |
|---|---|---|---|
| n = 50 | n = 50 | ||
| Demographic Characteristics | |||
| Age, Mean (±SD) | 60.4 (±8.5) | 51.8 (±8.6) | <0.0001 |
| Gender, n (%) | |||
| Man | 25 (50.0) | 21 (42.0) | ns |
| Woman | 25 (50.0) | 29 (58.0) | ns |
| Periodontal Parameters, Median (IQR) | |||
| Number of teeth | 22.5 (15.7–26.0) | 26.0 (22.0–28.0) | 0.016 |
| BOP (% of sites) | 35.5 (24.8–52.4) | 44.4 (26.7–62.8) | ns |
| PD ≤ 4 mm (% of sites) | 94.5 (86.4–98.1) | 95.1 (82.0–98.3) | ns |
| PD ≥ 5 mm (% of sites) | 5.4 (1.9–13.6) | 4.9 (1.1–18.1) | ns |
| CAL ≤ 3 mm (% of sites) | 6.6 (2.0–12.3) | 4.9 (1.1–18.8) | ns |
| CAL = 4–5 mm (% of sites) | 64.9 (50.3–76.8) | 68.8 (35.9–80.6) | ns |
| CAL ≥ 6 mm (% of sites) | 27.9 (16.4–39.2) | 25.6 (16.2–40.1) | ns |
| Biochemical and Physical Data, Median (IQR) | |||
| HbA1c (%) | 6.0 (5.6–6.4) | 5.6 (5.2–6.1) | 0.0104 |
| Fasting Blood Glucose (mg/dL) | 102.0 (93.0–117.5) | 95.2 (84.5–108.8) | 0.0253 |
| Estimated Blood Glucose (mg/dL) | 118.5 (102.0–128.1) | 111.1 (99.3–124.0) | ns |
| Total cholesterol (mg/dL) | 170.0 (147.5–222.0) | 186.0 (144.0–217.0) | ns |
| HDL cholesterol (mg/dL) | 53.0 (31.9–57.0) | 45.3 (37.1–57.1) | ns |
| Risk Factor | Adj OR (95% CI) | p-Value |
| Demographic Characteristics | ||
| Gender | 0.76 (0.30–1.92) | 0.46 |
| Periodontal Parameters | ||
| Number of teeth | 0.97 (0.89–1.06) | 0.46 |
| BOP | 0.99 (0.96–1.01) | 0.18 |
| PD ≤ 4 mm | 1.03 (0.97–1.07) | 0.32 |
| PD ≥ 5 mm | 0.98 (0.94–1.02) | 0.32 |
| CAL ≤ 3 mm | 0.97 (0.93–1.01) | 0.17 |
| CAL = 4–5 mm | 1.02 (0.99–1.04) | 0.05 |
| CAL ≥ 6 mm | 0.96 (0.93–1.01) | 0.05 |
| Biochemical and Physical Data | ||
| HbA1c (%) | 2.39 (1.01–5.67) | 0.04 |
| Fasting Blood Glucose (mg/dL) | 1.03 (1.01–1.07) | 0.01 |
| Estimated Blood Glucose (mg/dL) | 1.02 (0.99–1.05) | 0.11 |
| Total cholesterol (mg/dL) | 0.99 (0.98–1.01) | 0.99 |
| HDL cholesterol (mg/dL) | 1.01 (0.93–1.09) | 0.79 |
| C-reactive protein | 6.31 (0.71–5.62) | 0.09 |
| Creatinine (mg/dL) | 0.68 (0.08–5.75) | 0.72 |
| GPT | 1.02 (0.99–1.05) | 0.23 |
| GOT | 1.05 (0.98–1.11) | 0.16 |
| Waist/Hip Ratio (cm) | 27.1 (0.12–6.15) | 0.24 |
| BMI (Kg/m2) | 1.12 (1.02–1.24) | 0.01 |
| Blood Pressure Variables | ||
| Systolic blood pressure | 1.06 (1.02–1.09) | 0.005 |
| Diastolic blood pressure | 1.05 (0.99–1.09) | 0.09 |
| Mean blood pressure | 1.08 (1.02–1.13) | 0.008 |
| Differential blood pressure | 1.05 (1.01–1.09) | 0.04 |
| Risk Factor | Adjusted β (95% CI) | p-Value |
| Demographic Characteristics | ||
| Gender | −0.05 (−0.25–0.14) | 0.59 |
| Periodontal Parameters | ||
| Number of teeth | −0.21 (−0.04–−0.004) | 0.01 |
| BOP | −0.003 (−0.009–0.002) | 0.18 |
| PD ≤ 4 mm | 0.004 (−0.004–0.01) | 0.31 |
| PD ≥ 5 mm | −0.004 (−0.13–0.004) | 0.30 |
| CAL ≤ 3 mm | −0.005 (−0.01–0.002) | 0.19 |
| CAL = 4–5 mm | 0.003 (0.001–0.008) | 0.06 |
| CAL ≥ 6 mm | −0.007 (−0.014–−0.0001) | 0.05 |
| Biochemical and Physical Data | ||
| HbA1c (%) | 0.16 (0.42–0.33) | 0.04 |
| Fasting Blood Glucose (mg/dL) | 0.004 (0.002–0.011) | 0.004 |
| Estimated Blood Glucose (mg/dL) | 0.005 (−0.00–0.01) | 0.10 |
| Total cholesterol (mg/dL) | −0.000 (−0.002–0.003) | 0.97 |
| HDL cholesterol (mg/dL) | 0.003 (−0.02–0.03) | 0.82 |
| Creatinine (mg/dL) | −0.81 (−0.53–0.37) | 0.72 |
| GPT | 0.004 (−0.002–0.11) | 0.21 |
| GOT | 0.008 (−0.002–0.02) | 0.12 |
| Waist/Hip Ratio (cm) | 0.66 (−0.38–1.73) | 0.21 |
| BMI (Kg/m2) | 0.02 (0.006–0.38) | 0.006 |
| Pressure Variables | ||
| Systolic blood pressure | 0.007 (0.003–0.02) | 0.003 |
| Diastolic blood pressure | 0.008 (−0.002–0.18) | 0.12 |
| Mean blood pressure | 0.02 (0.003–0.02) | 0.007 |
| Differential blood pressure | 0.008 (0.008–0.02) | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, R.A.C.; Rodrigues, J.V.S.; Cláudio, M.M.; Franciscon, J.P.S.; Mulinari-Santos, G.; Cirelli, T.; de Molon, R.S.; Gouveia Garcia, V.; Theodoro, L.H. The Relationship between Hypertension and Periodontitis: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 5140. https://doi.org/10.3390/jcm12155140
Rosa RAC, Rodrigues JVS, Cláudio MM, Franciscon JPS, Mulinari-Santos G, Cirelli T, de Molon RS, Gouveia Garcia V, Theodoro LH. The Relationship between Hypertension and Periodontitis: A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(15):5140. https://doi.org/10.3390/jcm12155140
Chicago/Turabian StyleRosa, Rossana Abud Cabrera, João Victor Soares Rodrigues, Marina Module Cláudio, João Paulo Soares Franciscon, Gabriel Mulinari-Santos, Thamiris Cirelli, Rafael Scaf de Molon, Valdir Gouveia Garcia, and Leticia Helena Theodoro. 2023. "The Relationship between Hypertension and Periodontitis: A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 15: 5140. https://doi.org/10.3390/jcm12155140