Preoperative and Postoperative Kinesiophobia Influences Postoperative Outcome Measures Following Anterior Cruciate Ligament Reconstruction: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Tampa Scale for Kinesiophobia (TSK)
2.2. Postoperative Scores
2.2.1. Anterior Cruciate Ligament—Return to Sport after Injury
2.2.2. Short-Form Health Survey-36
2.2.3. Knee Injury and Osteoarthritis Outcome Score
2.2.4. Oxford Knee Score
2.3. Statistical Analysis
3. Results
3.1. Preoperative Kinesiophobia
3.2. Postoperative Kinesiophobia
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Longo, U.G.; Nagai, K.; Salvatore, G.; Cella, E.; Candela, V.; Cappelli, F.; Ciccozzi, M.; Denaro, V. Epidemiology of Anterior Cruciate Ligament Reconstruction Surgery in Italy: A 15-Year Nationwide Registry Study. J. Clin. Med. 2021, 10, 223. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef]
- Coronado, R.A.; Sterling, E.K.; Fenster, D.E.; Bird, M.L.; Heritage, A.J.; Woosley, V.L.; Burston, A.M.; Henry, A.L.; Huston, L.J.; Vanston, S.W.; et al. Cognitive-behavioral-based physical therapy to enhance return to sport after anterior cruciate ligament reconstruction: An open pilot study. Phys. Ther. Sport 2020, 42, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; King, J.B.; Denaro, V.; Maffulli, N. Double-bundle arthroscopic reconstruction of the anterior cruciate ligament: Does the evidence add up? J. Bone Joint Surg. Br. 2008, 90, 995–999. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Salvatore, G.; Ruzzini, L.; Risi Ambrogioni, L.; de Girolamo, L.; Viganò, M.; Facchini, F.; Cella, E.; Candela, V.; Ciccozzi, M.; et al. Trends of anterior cruciate ligament reconstruction in children and young adolescents in Italy show a constant increase in the last 15 years. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1728–1733. [Google Scholar] [CrossRef]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; Casciaro, C.; Mannering, N.; Candela, V.; Salvatore, G.; Denaro, V. Anterior cruciate ligament reconstruction in skeletally immature patients: A systematic review. Bone Joint J. 2017, 99, 1053–1060. [Google Scholar] [CrossRef]
- Longo, U.G.; Rizzello, G.; Frnaceschi, F.; Campi, S.; Maffulli, N.; Denaro, V. The architecture of the ipsilateral quadriceps two years after successful anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft. Knee 2014, 21, 721–725. [Google Scholar] [CrossRef]
- Healey, E.L.; Lewis, M.; Corp, N.; Shivji, N.A.; van der Windt, D.A.; Babatunde, O.O.; Simkins, J.; Bartlam, B.; Rowlands, G.; Protheroe, J. Supported self-management for all with musculoskeletal pain: An inclusive approach to intervention development: The EASIER study. BMC Musculoskelet. Disord. 2023, 24, 474. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Denaro, V. Anterior cruciate ligament tear. N. Engl. J. Med. 2009, 360, 1463. [Google Scholar] [CrossRef]
- Booth, J.; Moseley, G.L.; Schiltenwolf, M.; Cashin, A.; Davies, M.; Hübscher, M. Exercise for chronic musculoskeletal pain: A biopsychosocial approach. Musculoskelet. Care 2017, 15, 413–421. [Google Scholar] [CrossRef]
- Luque-Suarez, A.; Martinez-Calderon, J.; Falla, D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: A systematic review. Br. J. Sports Med. 2019, 53, 554–559. [Google Scholar] [CrossRef]
- Pontillo, M.; Gunterstockman, B.M.; Mauntel, T.C.; Farrokhi, S. The association between kinesiophobia and functional limitations in service members with knee pain. Musculoskelet. Sci. Pract. 2023, 65, 102766. [Google Scholar] [CrossRef]
- Núñez-Cortés, R.; Horment-Lara, G.; Tapia-Malebran, C.; Castro, M.; Barros, S.; Vera, N.; Pérez-Alenda, S.; Pablo Santelices, J.; Rivera-Lillo, G.; Cruz-Montecinos, C. Role of kinesiophobia in the selective motor control during gait in patients with low back-related leg pain. J. Electromyogr. Kinesiol. 2023, 71, 102793. [Google Scholar] [CrossRef]
- Neblett, R.; Hartzell, M.M.; Mayer, T.G.; Bradford, E.M.; Gatchel, R.J. Establishing clinically meaningful severity levels for the Tampa Scale for Kinesiophobia (TSK-13). Eur. J. Pain 2016, 20, 701–710. [Google Scholar] [CrossRef]
- Eiger, B.; Errebo, M.; Straszek, C.L.; Vaegter, H.B. Less is more: Reliability and measurement error for three versions of the Tampa Scale of Kinesiophobia (TSK-11, TSK-13, and TSK-17) in patients with high-impact chronic pain. Scand. J. Pain 2023, 23, 217–224. [Google Scholar] [CrossRef]
- Monticone, M.; Giorgi, I.; Baiardi, P.; Barbieri, M.; Rocca, B.; Bonezzi, C. Development of the Italian version of the Tampa Scale of Kinesiophobia (TSK-I): Cross-cultural adaptation, factor analysis, reliability, and validity. Spine 2010, 35, 1241–1246. [Google Scholar] [CrossRef]
- Tortoli, E.; Francini, L.; Giovannico, G.; Ramponi, C. Translation, cross-cultural adaptation and validation of the Italian version of the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1180–1186. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, validation and norming. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Monticone, M.; Ferrante, S.; Salvaderi, S.; Rocca, B.; Totti, V.; Foti, C.; Roi, G.S. Development of the Italian version of the knee injury and osteoarthritis outcome score for patients with knee injuries: Cross-cultural adaptation, dimensionality, reliability, and validity. Osteoarthr. Cartil. 2012, 20, 330–335. [Google Scholar] [CrossRef]
- Padua, R.; Zanoli, G.; Ceccarelli, E.; Romanini, E.; Bondì, R.; Campi, A. The Italian version of the Oxford 12-item Knee Questionnaire-cross-cultural adaptation and validation. Int. Orthop. 2003, 27, 214–216. [Google Scholar] [CrossRef] [PubMed]
- Brown, O.S.; Hu, L.; Demetriou, C.; Smith, T.O.; Hing, C.B. The effects of kinesiophobia on outcome following total knee replacement: A systematic review. Arch. Orthop. Trauma Surg. 2020, 140, 2057–2070. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.; Tanzer, M.; Reardon, G.; Amirault, D.; Dunbar, M.; Stanish, W. The role of presurgical expectancies in predicting pain and function one year following total knee arthroplasty. Pain 2011, 152, 2287–2293. [Google Scholar] [CrossRef] [PubMed]
- Fadyl, J.; McPherson, K. Return to work after injury: A review of evidence regarding expectations and injury perceptions, and their influence on outcome. J. Occup. Rehabil. 2008, 18, 362–374. [Google Scholar] [CrossRef]
- Kocic, M.; Stankovic, A.; Lazovic, M.; Dimitrijevic, L.; Stankovic, I.; Spalevic, M.; Stojiljkovic, P.; Milenkovic, M.; Stojanovic, Z.; Nikolic, D. Influence of fear of movement on total knees arthroplasty outcome. Ann. Ital. Chir. 2015, 86, 148–155. [Google Scholar]
- Paterno, M.V.; Flynn, K.; Thomas, S.; Schmitt, L.C. Self-Reported Fear Predicts Functional Performance and Second ACL Injury After ACL Reconstruction and Return to Sport: A Pilot Study. Sports Health 2018, 10, 228–233. [Google Scholar] [CrossRef]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- Ohrnberger, J.; Fichera, E.; Sutton, M. The relationship between physical and mental health: A mediation analysis. Soc. Sci. Med. 2017, 195, 42–49. [Google Scholar] [CrossRef]



| Parameter | Correlation between Preoperative TSK-13 and Postoperative Scores | Correlation between Postoperative TSK-13 and Postoperative Scores | ||
|---|---|---|---|---|
| rho | p-Value | rho | p-Value | |
| ACL-RSI | −0.013 | 0.926 | −0.486 | <0.001 * |
| SF-36 PCS | −0.292 | 0.040 * | −0.248 | 0.083 |
| SF-36 MCS | −0.094 | 0.516 | −0.095 | 0.512 |
| SF-36 Health change | −0.111 | 0.441 | 0.227 | 0.113 |
| KOOS Symptoms | −0.041 | 0.776 | −0.513 | <0.001 * |
| KOOS Pain | 0.025 | 0.866 | −0.565 | <0.001 * |
| KOOS ADL | −0.040 | 0.785 | −0.496 | <0.001 * |
| KOOS Sport/Rec | 0.051 | 0.726 | −0.274 | 0.054 |
| KOOS QoL | 0.121 | 0.401 | −0.186 | 0.196 |
| OKS | −0.107 | 0.459 | −0.703 | <0.001 * |
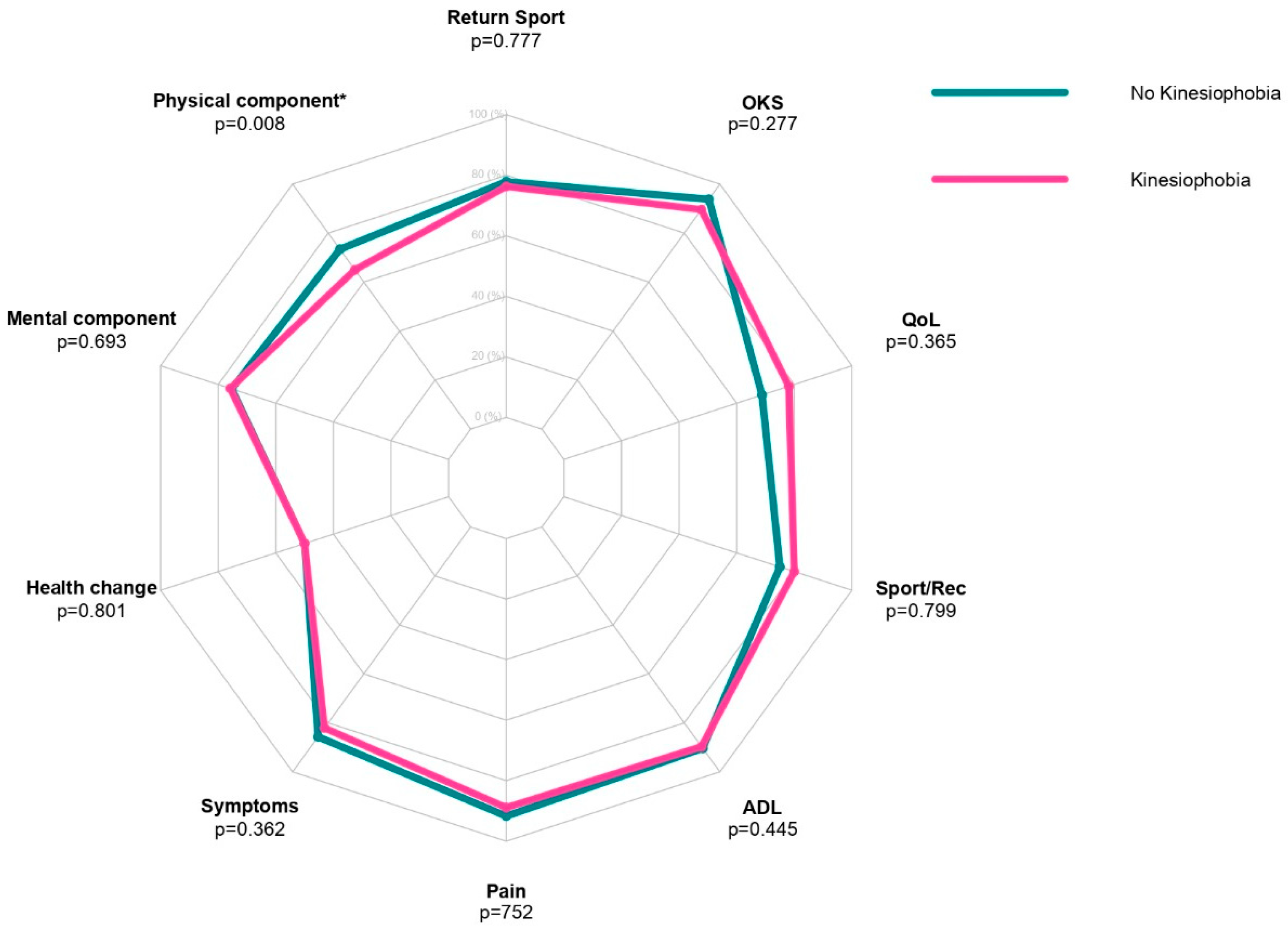
| Parameter | No Kinesiophobia (N = 18) | Kinesiophobia (N = 32) | p-Value | ||
|---|---|---|---|---|---|
| Median | Range | Median | Range | ||
| ACL-RSI | 77.9 | 52.5–100 | 76.3 | 42.5–96.7 | 0.777 |
| SF-36 PCS | 73.4 | 45–91.3 | 65.0 | 29.4–87.5 | 0.008 * |
| SF-36 MCS | 75.3 | 57–97.5 | 75.8 | 48–93.3 | 0.693 |
| SF-36 Health change | 50.0 | 25–100 | 50.0 | 25–100 | 0.801 |
| KOOS Symptoms | 85.7 | 60.7–100 | 82.1 | 50–100 | 0.362 |
| KOOS Pain | 91.7 | 66.7–100 | 88.9 | 52.8–100 | 0.752 |
| KOOS ADL | 90.4 | 61.8–100 | 89.7 | 51.5–98.5 | 0.445 |
| KOOS Sport/Rec | 75.0 | 45–100 | 80.0 | 20–100 | 0.799 |
| KOOS QoL | 68.8 | 31.3–100 | 78.1 | 12.5–100 | 0.365 |
| OKS | 93.8 | 45.8–100 | 89.6 | 41.7–100 | 0.277 |
| Parameter | No Kinesiophobia (N = 29) | Kinesiophobia (N = 21) | p-Value | ||
|---|---|---|---|---|---|
| Median | Range | Median | Range | ||
| ACL-RSI | 82.5 | 63.3–100 | 66.7 | 42.5–88.3 | <0.001 * |
| SF-36 PCS | 71.9 | 38.8–91.3 | 66.9 | 29.4–91.3 | 0.190 |
| SF-36 MCS | 75.6 | 57–97.5 | 75.8 | 48–97.5 | 0.798 |
| SF-36 Health change | 50.0 | 25–100 | 75.0 | 25–100 | 0.092 |
| KOOS Symptoms | 85.7 | 78.6–100 | 75.0 | 50–92.9 | <0.001 * |
| KOOS Pain | 94.4 | 77.8–100 | 77.8 | 52.8–94.4 | <0.001* |
| KOOS ADL | 91.2 | 77.9–100 | 86.8 | 51.5–98.5 | <0.001 * |
| KOOS Sport/Rec | 85.0 | 50–100 | 75.0 | 20–100 | 0.250 |
| KOOS QoL | 75.0 | 37.5–100 | 75.0 | 12.5–100 | 0.272 |
| OKS | 95.8 | 81.3–100 | 79.2 | 41.7–95.8 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Marino, M.; Rizzello, G.; De Salvatore, S.; Piergentili, I.; Denaro, V. Preoperative and Postoperative Kinesiophobia Influences Postoperative Outcome Measures Following Anterior Cruciate Ligament Reconstruction: A Prospective Study. J. Clin. Med. 2023, 12, 4858. https://doi.org/10.3390/jcm12144858
Longo UG, Marino M, Rizzello G, De Salvatore S, Piergentili I, Denaro V. Preoperative and Postoperative Kinesiophobia Influences Postoperative Outcome Measures Following Anterior Cruciate Ligament Reconstruction: A Prospective Study. Journal of Clinical Medicine. 2023; 12(14):4858. https://doi.org/10.3390/jcm12144858
Chicago/Turabian StyleLongo, Umile Giuseppe, Martina Marino, Giacomo Rizzello, Sergio De Salvatore, Ilaria Piergentili, and Vincenzo Denaro. 2023. "Preoperative and Postoperative Kinesiophobia Influences Postoperative Outcome Measures Following Anterior Cruciate Ligament Reconstruction: A Prospective Study" Journal of Clinical Medicine 12, no. 14: 4858. https://doi.org/10.3390/jcm12144858
APA StyleLongo, U. G., Marino, M., Rizzello, G., De Salvatore, S., Piergentili, I., & Denaro, V. (2023). Preoperative and Postoperative Kinesiophobia Influences Postoperative Outcome Measures Following Anterior Cruciate Ligament Reconstruction: A Prospective Study. Journal of Clinical Medicine, 12(14), 4858. https://doi.org/10.3390/jcm12144858








