The Value of Exercise Electrocardiography in Outpatients with Stable Chest Pain and Low Pre-Test Probability of Significant Coronary Artery Disease
Abstract
:1. Introduction
2. Materials and Methods
3. Results
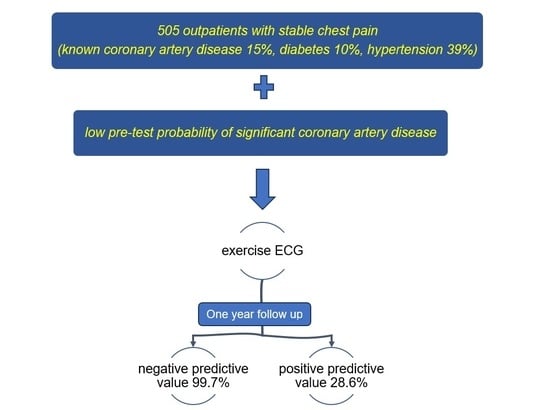
3.1. Low Pre-Test Probability Patients
3.2. One-Year Outcome in Low Pre-Test Probability Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 144, e368–e454. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diamond, G.A.; Forrester, J.S. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N. Engl. J. Med. 1979, 300, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Juarez-Orozco, L.E.; Saraste, A.; Capodanno, D.; Prescott, E.; Ballo, H.; Bax, J.J.; Wijns, W.; Knuuti, J. Impact of a decreasing pre-test probability on the performance of diagnostic tests for coronary artery disease. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1198–1207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pugh, S.L.; Torres-Saavedra, P.A. Fundamental Statistical Concepts in Clinical Trials and Diagnostic Testing. J. Nucl. Med. 2021, 62, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Garner, K.K.; Pomeroy, W.; Arnold, J.J. Exercise Stress Testing: Indications and Common Questions. Am. Fam. Physician 2017, 96, 293–299. [Google Scholar] [PubMed]
- Bourque, J.M.; Charlton, G.T.; Holland, B.H.; Belyea, C.M.; Watson, D.D.; Beller, G.A. Prognosis in patients achieving ≥10 METS on exercise stress testing: Was SPECT imaging useful? J. Nucl. Cardiol. 2011, 18, 230–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraen, M.; Akil, S.; Hedén, B.; Berg, J.; Ostenfeld, E.; Carlsson, M.; Arheden, H.; Engblom, H. Incremental Value of Exercise ECG to Myocardial Perfusion Single-Photon Emission Computed Tomography for Prediction of Cardiac Events. J. Am. Heart Assoc. 2023, 12, e028313. [Google Scholar] [CrossRef]
- Vaidya, G.N. Application of exercise ECG stress test in the current high cost modern-era healthcare system. Indian Heart J. 2017, 69, 551–555. [Google Scholar] [CrossRef]
- Banerjee, A.; Newman, D.R.; Van den Bruel, A.; Heneghan, C. Diagnostic accuracy of exercise stress testing for coronary artery disease: A systematic review and meta-analysis of prospective studies. Int. J. Clin. Pract. 2012, 66, 477–492. [Google Scholar] [CrossRef]
- Gibbons, R.J.; Carryer, D.; Hodge, D.; Miller, T.D.; Roger, V.L.; Askew, J.W. Stress Testing in the Evaluation of Stable Chest Pain in a Community Population. Mayo Clin. Proc. 2020, 95, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.J.; Mieres, J.H.; Hendel, R.H.; Boden, W.E.; Gulati, M.; Veledar, E.; Hachamovitch, R.; Arrighi, J.A.; Merz, C.N.; Gibbons, R.J.; et al. Comparative effectiveness of exercise electrocardiography with or without myocardial perfusion single photon emission computed tomography in women with suspected coronary artery disease: Results from the What Is the Optimal Method for Ischemia Evaluation in Women (WOMEN) trial. Circulation 2011, 124, 1239–1249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, T.; Bing, R.; Dweck, M.R.; van Beek, E.J.R.; Mills, N.L.; Williams, M.C.; Villines, T.C.; Newby, D.E.; Adamson, P.D. Exercise Electrocardiography and Computed Tomography Coronary Angiography for Patients with Suspected Stable Angina Pectoris: A Post Hoc Analysis of the Randomized SCOT-HEART Trial. JAMA Cardiol. 2020, 5, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, U.; Ferencik, M.; Udelson, J.E.; Picard, M.H.; Truong, Q.A.; Patel, M.R.; Huang, M.; Pencina, M.; Mark, D.B.; Heitner, J.F.; et al. Prognostic Value of Noninvasive Cardiovascular Testing in Patients with Stable Chest Pain: Insights from the PROMISE Trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain). Circulation 2017, 135, 2320–2332. [Google Scholar] [CrossRef] [PubMed]
- Seitun, S.; Clemente, A.; Maffei, E.; Toia, P.; La Grutta, L.; Cademartiri, F. Prognostic value of cardiac CT. Radiol. Med. 2020, 125, 1135–1147. [Google Scholar] [CrossRef] [PubMed]


| All Patients | N = 505 |
|---|---|
| Mean age, years (±SD) | 59.6 (±13.6) |
| Women | 284 (56.2%) |
| Coronary heart disease | 73 (14.5%) |
| Current smoking | 38 (7.5%) |
| Hypertension | 196 (38.8%) |
| Hyperlipidemia | 123 (24.4%) |
| Diabetes mellitus | 50 (9.9%) |
| Heart failure | 7 (1.4%) |
| Exercise ECG Results | |||
|---|---|---|---|
| Negative | Inconclusive | Positive | |
| Acute coronary syndrome | 2 (0.4%) | 0 | 1 (0.2%) |
| All-cause mortality | 0 | 0 | 1 (0.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thorild, P.; Mourtzinis, G. The Value of Exercise Electrocardiography in Outpatients with Stable Chest Pain and Low Pre-Test Probability of Significant Coronary Artery Disease. J. Clin. Med. 2023, 12, 4670. https://doi.org/10.3390/jcm12144670
Thorild P, Mourtzinis G. The Value of Exercise Electrocardiography in Outpatients with Stable Chest Pain and Low Pre-Test Probability of Significant Coronary Artery Disease. Journal of Clinical Medicine. 2023; 12(14):4670. https://doi.org/10.3390/jcm12144670
Chicago/Turabian StyleThorild, Pontus, and Georgios Mourtzinis. 2023. "The Value of Exercise Electrocardiography in Outpatients with Stable Chest Pain and Low Pre-Test Probability of Significant Coronary Artery Disease" Journal of Clinical Medicine 12, no. 14: 4670. https://doi.org/10.3390/jcm12144670