Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III)
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Patients
2.2. Clinical Setting and Data Collection
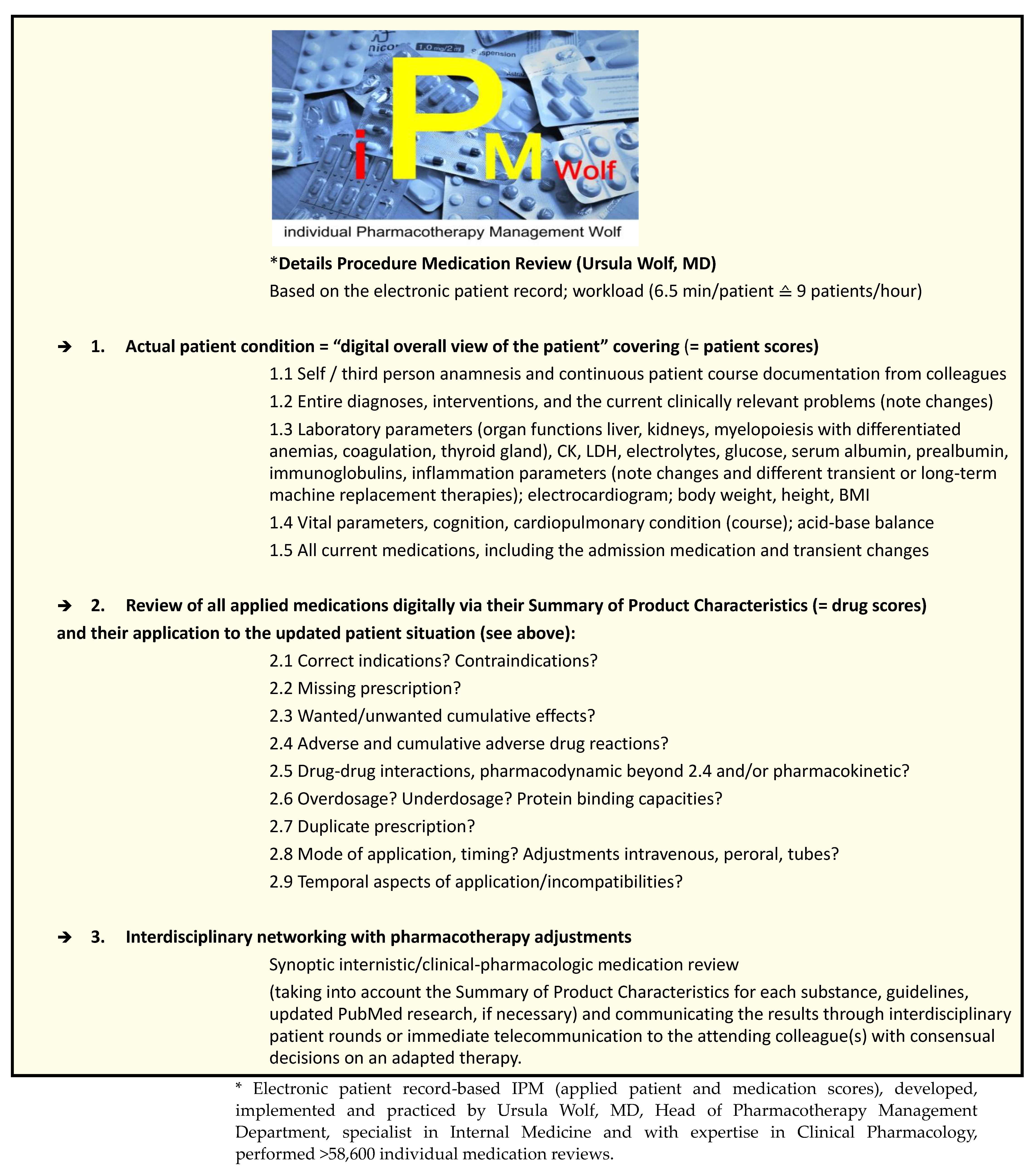
2.3. Individual Pharmacotherapy Management (IPM)
2.4. Biomedical Statistics
3. Results
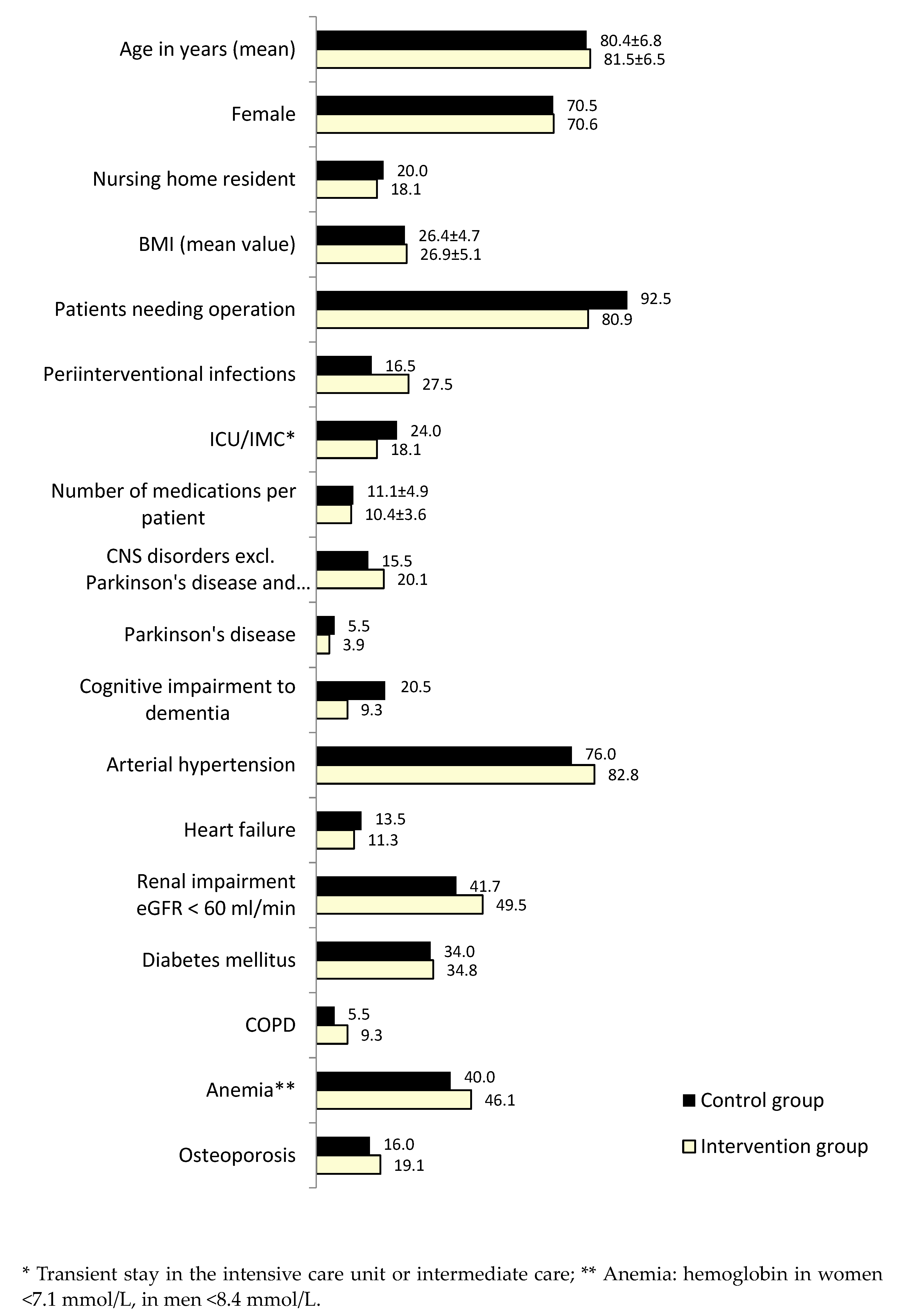
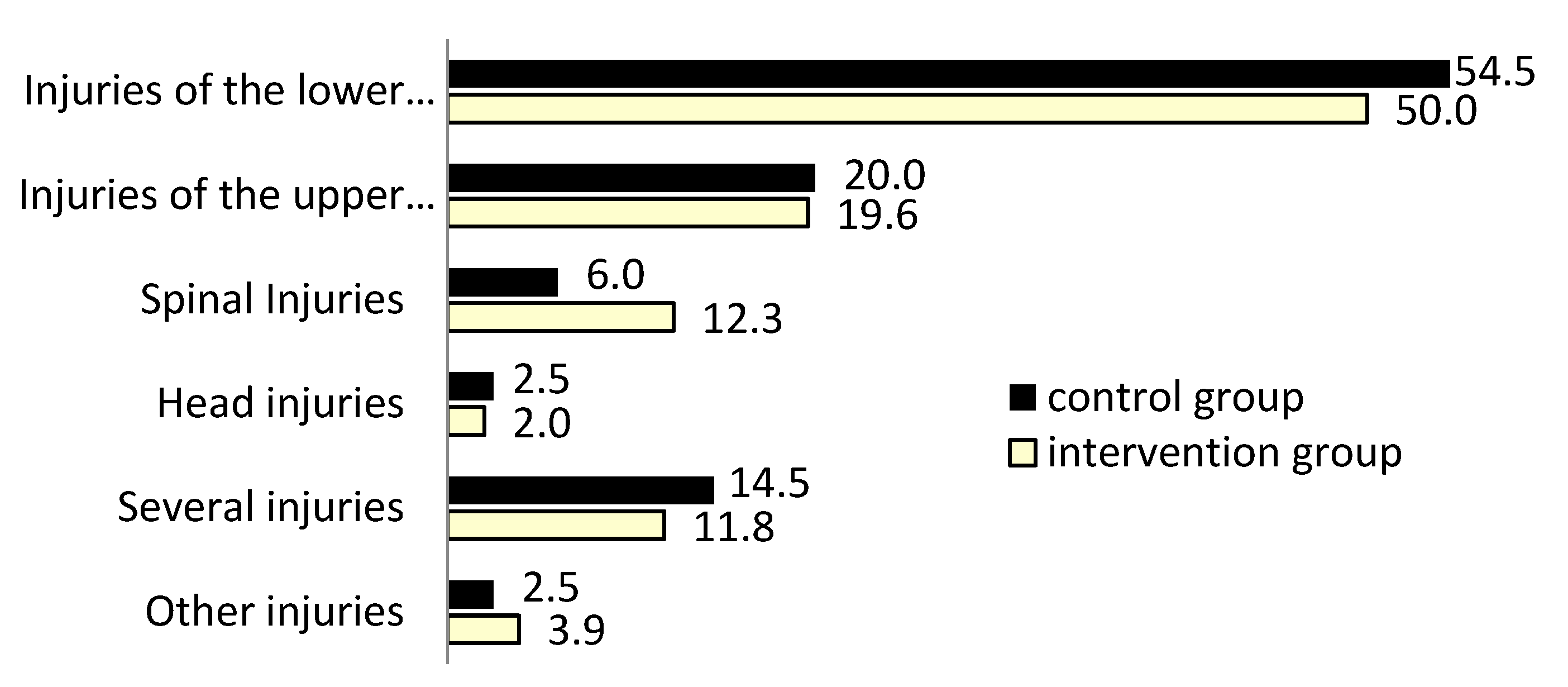
3.1. Study Groups’ Characteristics
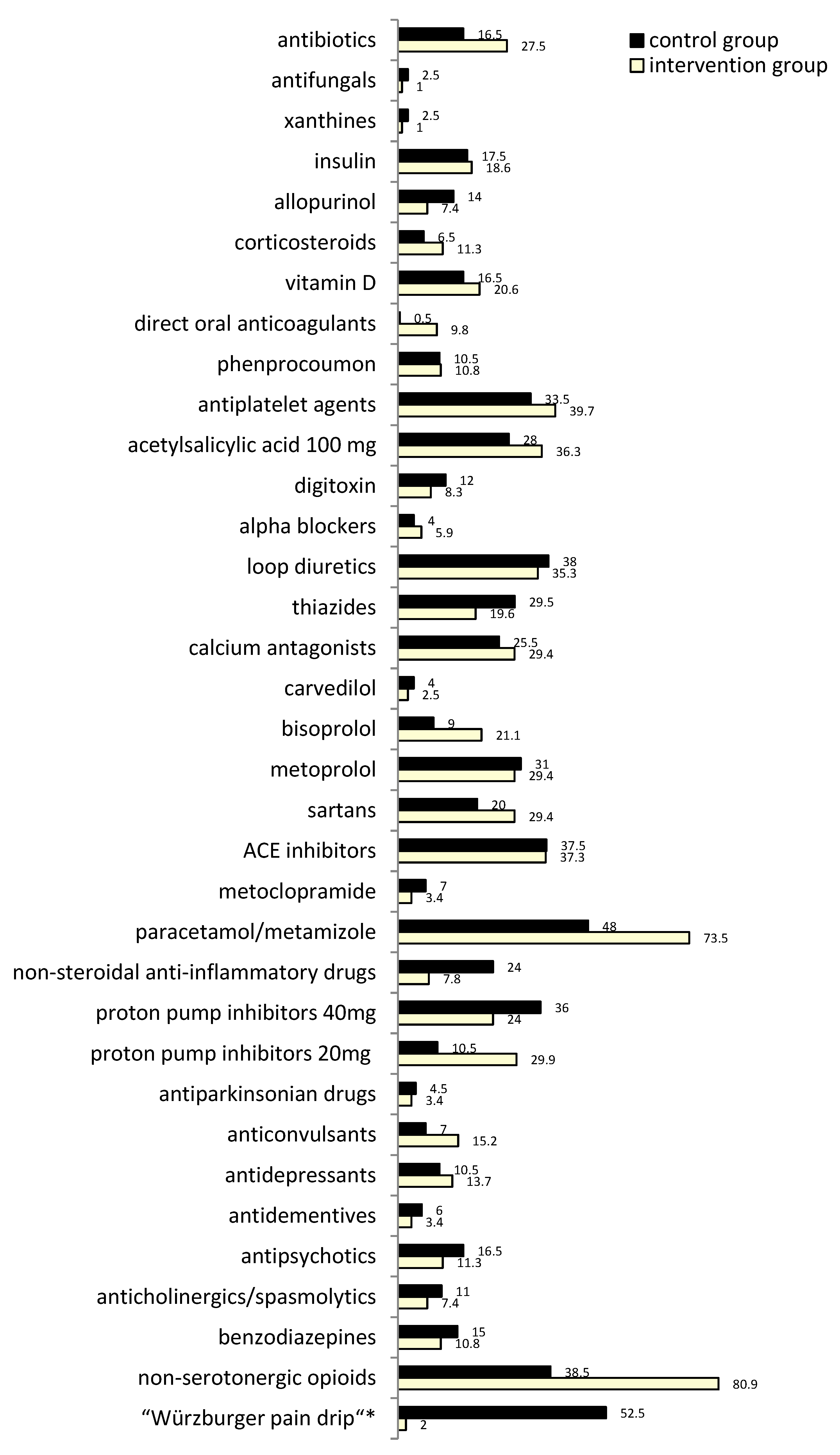
3.2. Polypharmacy and IPM
- Dose fine-tuning of all drugs from the patient’s overall perioperative medication list adapted to current renal function and pharmacokinetic DDIs, not least with antibiotics.
- Blood pressure optimization,
- Targeted treatment of bradycardia, tachycardia, and arrhythmias,
- Exclusion of hypo- and dehydration,
- Avoidance of single and cumulative nephrotoxic risks from direct drug actions as, e.g., from NSAIDs mono or even coadministered with ACE-inhibitors or sartans,
- Avoidance of single and cumulative indirect nephrotoxic risks from ADRs, e.g., from statins, and pharmacodynamic DDIs,
- Early treatment of bacterial urinary tract infections,
- Compensating for electrolyte and acid-base imbalances by timely targeted discontinuation of intensifying medications and, when compatible with respiratory capacity, bicarbonate use,
- Following standard operating procedures for preventive measures in contrast to media administration.
3.3. Analytic Statistics on Associations of IPM and redGFR
4. Discussion
4.1. IPM Effectiveness and Evaluated Outcome
4.2. CKD and eGFR Estimation Aspects
4.3. CKD Unawareness and Associated Risks
4.4. Patients, IPM Focuses in Polypharmacy, Renal Risks and Prevention
5. Strengths and Weaknesses
6. Conclusions, Challenges, and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Quality Assurance and Safety of Medicines Team. The Safety of Medicines in Public Health Programmes: Pharmacovigilance, an Essential Tool. 2006. Available online: https://apps.who.int/iris/handle/10665/43384 (accessed on 8 October 2022).
- World Health Organization. Medication Without Harm—Global Patient Safety Challenge on Medication Safety. Geneva: World Health Organization. 2017. Licence: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/bitstream/handle/10665/255263/WHO-HIS-SDS-2017.6-eng.pdf (accessed on 10 February 2023).
- World Health Assembly, 73 (2020). Decade of Healthy Ageing: The Global Strategy and Action Plan on Ageing and Health 2016–2020: Towards a World in Which Everyone Can Live a Long and Healthy Life: Report by the Director-General. World Health Organization. 2020. Available online: https://apps.who.int/iris/handle/10665/355618 (accessed on 10 February 2023).
- The UN Decade of Healthy Ageing (2021–2030). Available online: https://www.un.org/en/UN-system/ageing (accessed on 10 February 2023).
- United Nations. General Assembly Seventy-Fifth Session Agenda Item 131. Global Health and Foreign Policy. Resolution Adopted by the General Assembly on 14 December 2020. 75/131. United Nations Decade of Healthy Ageing (2021–2030). Available online: https://documents-dds-ny.un.org/doc/UNDOC/GEN/N20/363/87/PDF/N2036387.pdf?OpenElement (accessed on 10 February 2023).
- The Health Care Quality Indicators Team Final Report. Data and Analysis of Data on Patient Safety within the OECD Health Care Quality Indicators Project (OECD-PS). 2018, 1–294. Available online: https://ec.europa.eu/chafea/health/documents/OECD-Patient-Safety-VS-2015-5402-D00035-FINAL.pdf (accessed on 10 February 2023).
- United Nations, Department of Economic and Social Affairs, Population Devision. World Population Ageing 2019. In Highlights; (ST/ESA/SER.A/430); United Nations, Department of Economic and Social Affairs: New York, NY, USA, 2019; Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 11 February 2023).
- Drewas, L.; Ghadir, H.; Neef, R.; Delank, K.S.; Wolf, U. Individual Pharmacotherapy Management (IPM)—I: A group-matched retrospective controlled clinical study on prevention of complicating delirium in the elderly trauma patients and identification of associated factors. BMC Geriatr. 2022, 22, 29. [Google Scholar] [CrossRef] [PubMed]
- Wolf, U.; Eckert, S.; Walter, G.; Wienke, A.; Bartel, S.; Plontke, S.K.; Naumann, C. Prevalence of oropharyngeal dysphagia in geriatric patients and real-life associations with diseases and drugs. Sci. Rep. 2021, 11, 21955. [Google Scholar] [CrossRef] [PubMed]
- Clifford, K.M.; Selby, A.R.; Reveles, K.R.; Teng, C.; Hall, R.G., 2nd; McCarrell, J.; Alvarez, C.A. The Risk and Clinical Implications of Antibiotic-Associated Acute Kidney Injury: A Review of the Clinical Data for Agents with Signals from the Food and Drug Administration’s Adverse Event Reporting System (FAERS) Database. Antibiotics 2022, 11, 1367. [Google Scholar] [CrossRef] [PubMed]
- US Centers for Disease Control and Prevention (CDC). Chronic Kidney Disease Initiative. Chronic Kidney Disease Basics. Page Last Reviewed: 28 February 2022. Available online: https://www.cdc.gov/kidneydisease/basics.html (accessed on 18 February 2023).
- Sundström, J.; Bodegard, J.; Bollmann, A.; Vervloet, M.G.; Mark, P.B.; Karasik, A.; Taveira-Gomes, T.; Botana, M.; Birkeland, K.I.; Thuresson, M.; et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2·4 million patients from 11 countries: The CaReMe CKD study. Lancet Reg. Health Eur. 2022, 20, 100438. [Google Scholar] [CrossRef]
- Girndt, M.; Trocchi, P.; Scheidt-Nave, C.; Markau, S.; Stang, A. The Prevalence of Renal Failure. Results from the German Health Interview and Examination Survey for Adults, 2008–2011 (DEGS1). Dtsch. Ärzteblatt Int. 2016, 113, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Schaeffner, E.S.; Ebert, N.; Delanaye, P.; Frei, U.; Gaedeke, J.; Jakob, O.; Kuhlmann, M.K.; Schuchardt, M.; Tölle, M.; Ziebig, R.; et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann. Intern. Med. 2012, 157, 471–481. [Google Scholar] [CrossRef] [Green Version]
- Statistisches Bundesamt Deutschland. Koordinierte Bevölkerungsvorausberechnung. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/_inhalt.html (accessed on 15 October 2022).
- Bundeszentrale für Politische Bildung. Bevölkerung Nach Altersgruppen und Geschlecht. Available online: https://www.bpb.de/kurz-knapp/zahlen-und-fakten/soziale-situation-in-deutschland/61538/bevoelkerung-nach-altersgruppen-und-geschlecht/ (accessed on 17 February 2023).
- Wolf, U.; Baust, H.; Neef, R.; Steinke, T. Individual Pharmacotherapy Management (IPM)—IV: Optimized Usage of Approved Antimicrobials Addressing Under-Recognized Adverse Drug Reactions and Drug-Drug Interactions in Polypharmacy. Antibiotics 2022, 11, 1381. [Google Scholar] [CrossRef]
- Ghadir, H. Klinisch-pharmakologische Visiten in der Alterstraumatologie—Möglichkeit der Prävention Einer Nierenfunktionsverschlechterung und Definition Prädisponierender Faktoren. Doctoral Thesis, Medizinische Fakultät der Martin-Luther-Universität Halle-Wittenberg, Halle (Saale), Germany, 2023. [Google Scholar]
- Coca, S.G. Acute kidney injury in elderly persons. Am. J. Kidney Dis. 2010, 56, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Teruel, J.L.; Sabater, J.; Galeano, C.; Rivera, M.; Merino, J.L.; Fernández Lucas, M.; Marcén, R.; Ortuño, J. La ecuación de Cockcroft-Gault es preferible a la ecuación MDRD para medir el filtrado glomerular en la insuficiencia renal crónica avanzada [The Cockcroft-Gault equation is better than MDRD equation to estimate the glomerular filtration rate in patients with advanced chronic renal failure]. Nefrol. Publ. Of. Soc. Esp. Nefrol. 2007, 27, 313–319. [Google Scholar]
- Helou, R. Should We Continue to Use the Cockcroft-Gault Formula? Nephron Clin. Pract. 2010, 116, c172–c186. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, K.; Mahmoodi, B.K.; Woodward, M.; Emberson, J.R.; Jafar, T.H.; Jee, S.H.; Polkinghorne, K.R.; Shankar, A.; Smith, D.H.; Tonelli, M.; et al. Comparison of risk prediction using the CKD-EPI equation and the MDRD study equation for estimated glomerular filtration rate. JAMA 2012, 307, 1941–1951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drugs.com. Drug Interaction Checker. Check for Multi-Drug Interactions Including Alcohol, Food, Supplements & Diseases. Available online: https://www.drugs.com/drug_interactions.html (accessed on 10 March 2023).
- Dosing. Arzneimitteldosierung bei Niereninsuffizienz. 1998—2023 Abt. Klinische Pharmakologie & Pharmakoepidemiologie, Universitätsklinikum Heidelberg. Available online: https://dosing.de/ (accessed on 10 March 2023).
- Single Care. Piperacillin Sod-Tazobactam So Side Effects, Interactions, and Warnings. Available online: https://www.singlecare.com/prescription/piperacillin-sod-tazobactam-so/side-effects (accessed on 10 March 2023).
- Kadomura, S.; Takekuma, Y.; Sato, Y.; Sumi, M.; Kawamoto, K.; Itoh, T.; Sugawara, M. Higher incidence of acute kidney injury in patients treated with piperacillin/tazobactam than in patients treated with cefepime: A single-center retrospective cohort study. J. Pharm. Health Care Sci. 2019, 5, 13. [Google Scholar] [CrossRef]
- Karino, F.; Nishimura, N.; Ishihara, N.; Moriyama, H.; Miura, K.; Hamaguchi, S.; Sutani, A.; Kuraki, T.; Ikawa, K.; Morikawa, N. Nephrotoxicity induced by piperacillin–tazobactam in late elderly Japanese patients with nursing and healthcare associated pneumonia. Biol. Pharm. Bull. 2014, 37, 1971–1976. [Google Scholar] [CrossRef] [Green Version]
- Pravastatin-CT 20 mg/40 mg Tabletten. Fachinformation September 2018. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/88578.pdf (accessed on 20 February 2023).
- Moxonidin AL 0.2 mg/- 0.3 mg/- 0.4 mg Filmtabletten. Fachinformation January 2015. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/58210.pdf (accessed on 22 February 2023).
- Martin, U.; Hill, C.; O’ Mahony, D. Use of moxonidine in elderly patients with resistant hypertension. J. Clin. Pharm. Ther. 2005, 30, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Allopurinol-Ratiopharm Tabletten. Fachinformation November 2017. Available online: https://www.ratiopharm.de/assets/products/de/label/Allopurinol-ratiopharm%20100%20mg%20300%20mg%20Tabletten%20-%20Version%202.pdf?pzn=1686206 (accessed on 22 February 2023).
- Carvedilol AL 3.125 mg/- 6.25 mg/- 12.5 mg/- 25 mg Tabletten. Fachinformation February 2017. Available online: https://fachinformation.srz.de/pdf/aliudpharma/carvedilolaltabletten.pdf (accessed on 22 February 2023).
- Protopapas, A.; Lambrinou, E. Metoprolol and sertraline combined treatment may increase the risk of bradycardia. Arch. Hell. Med./Arheia Ellenikes Iatr. 2020, 37, 692–695. [Google Scholar]
- Ramipril—1 A Pharma® Tabletten. Fachinformation January 2019. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/91537.pdf (accessed on 22 February 2023).
- Enalapril-CT 5 mg/10 mg/20 mg Tabletten. Fachinformation April 2017. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/77352.pdf (accessed on 22 February 2023).
- Fouassier, D.; Blanchard, A.; Fayol, A.; Bobrie, G.; Boutouyrie, P.; Azizi, M.; Hulot, J.S. Sequential nephron blockade with combined diuretics improves diastolic function in patients with resistant hypertension. ESC Heart Fail. 2020, 7, 2561–2571. [Google Scholar] [CrossRef]
- Alendronat acis® 70 mg Tabletten. Fachinformation Juni 2017. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/79077.pdf (accessed on 22 February 2023).
- Metformin Aristo N 500 mg/- 850 mg/- 1000 mg Filmtabletten. Fachinformation July 2017. Available online: https://fachinformation.srz.de/pdf/aristo/metforminariston5008501000mgfilmtabletten.pdf (accessed on 22 February 2023).
- Pernicova, I.; Korbonits, M. Metformin—Mode of action and clinical implications for diabetes and cancer. Nat. Rev. Endocrinol. 2014, 10, 143–156. [Google Scholar] [CrossRef]
- Calvert, J.W.; Gundewar, S.; Jha, S.; Greer, J.J.; Bestermann, W.H.; Tian, R.; Lefer, D.J. Acute metformin therapy confers cardioprotection against myocardial infarction via AMPK-eNOS-mediated signaling. Diabetes 2008, 57, 696–705. [Google Scholar] [CrossRef] [Green Version]
- Qi, D.; Young, L.H. AMPK: Energy sensor and survival mechanism in the ischemic heart. Trends Endocrinol. Metab. 2015, 26, 422–429. [Google Scholar] [CrossRef] [Green Version]
- Tang, G.; Yang, H.; Chen, J.; Shi, M.; Ge, L.; Ge, X.; Zhu, G. Metformin ameliorates sepsis-induced brain injury by inhibiting apoptosis, oxidative stress and neuroinflammation via the PI3K/Akt signaling pathway. Oncotarget 2017, 8, 97977–97989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metamizol AbZ 500 mg Tabletten. Fachinformation 2017. Available online: https://www.abz.de/assets/products/de/label/Metamizol%20AbZ%20500%20mg%20Tabletten%20-%20Version%202.pdf?pzn=943603 (accessed on 22 February 2023).
- Hassan, K.; Khazim, K.; Hassan, F.; Hassan, S. Acute kidney injury associated with metamizole sodium ingestion. Ren. Fail. 2011, 33, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Spasmex 45 mg Filmtabletten—Trospiumchlorid. Fachinformation July 2017. Available online: https://s3.eu-central-1.amazonaws.com/prod-cerebro-ifap/media_all/78731.pdf (accessed on 22 February 2023).
- Chancellor, M.; Boone, T. Anticholinergics for overactive bladder therapy: Central nervous system effects. CNS Neurosci. Ther. 2012, 18, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef]
- Stevens, L.A.; Viswanathan, G.; Weiner, D.E. Chronic kidney disease and end-stage renal disease in the elderly population: Current prevalence, future projections, and clinical significance. Adv. Chronic Kidney Dis. 2010, 17, 293–301. [Google Scholar] [CrossRef] [Green Version]
- Manski-Nankervis, J.A.; McMorrow, R.; Nelson, C.; Jesudason, S.; Sluggett, J.K. Prescribing and deprescribing in chronic kidney disease. Aust. J. Gen. Pract. 2021, 50, 183–187. [Google Scholar] [CrossRef]
- Kitai, Y.; Nangaku, M.; Yanagita, M. Aging-Related Kidney Diseases. Contrib. Nephrol. 2021, 199, 266–273. [Google Scholar] [CrossRef]
- Sturmlechner, I.; Durik, M.; Sieben, C.J.; Baker, D.J.; van Deursen, J.M. Cellular senescence in renal ageing and disease. Nat. Rev. Nephrol. 2017, 13, 77–89. [Google Scholar] [CrossRef]
- O’Sullivan, E.D.; Hughes, J.; Ferenbach, D.A. Renal Aging: Causes and Consequences. JASN 2017, 28, 407–420. [Google Scholar] [CrossRef] [Green Version]
- Martin, J.E.; Sheaff, M.T. Renal ageing. J. Pathol. 2007, 211, 198–205. [Google Scholar] [CrossRef]
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef]
- O’Mahony, D.; O’Sullivan, D.; Byrne, S.; O’Connor, M.N.; Ryan, C.; Gallagher, P. STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age Ageing 2015, 44, 213–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Mahony, D. STOPP/START criteria for potentially inappropriate medications/potential prescribing omissions in older people: Origin and progress. Expert Rev. Clin. Pharmacol. 2020, 13, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, J.T.; Schmader, K.E. The medication appropriateness index at 20: Where it started, where it has been, and where it may be going. Drugs Aging 2013, 30, 893–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanlon, J.T.; Schmader, K.E. The Medication Appropriateness Index: A Clinimetric Measure. Psychother. Psychosom. 2022, 91, 78–83. [Google Scholar] [CrossRef]
- Kuhn-Thiel, A.M.; Weiß, C.; Wehling, M.; FORTA authors/expert panel members. Consensus validation of the FORTA (Fit fOR The Aged) List: A clinical tool for increasing the appropriateness of pharmacotherapy in the elderly. Drugs Aging 2014, 31, 131–140. [Google Scholar] [CrossRef] [Green Version]
- Huiskes, V.J.B.; Burger, D.M.; van den Ende, C.H.M.; van den Bemt, B.J.F. Effectiveness of medication review: A systematic review and meta-analysis of randomized controlled trials. BMC Fam. Pract. 2017, 18, 5. [Google Scholar] [CrossRef] [Green Version]
- Bosch-Lenders, D.; Jansen, J.; Stoffers, H.E.J.H.; Winkens, B.; Aretz, K.; Twellaar, M.; Schols, J.M.G.A.; van der Kuy, P.-H.M.; Knottnerus, J.A.; van den Akker, M. The Effect of a Comprehensive Interdisciplinary Medication Review on Quality of Life and Medication Use in Community Dwelling Older People with Polypharmacy. J. Clin. Med. 2021, 10, 600. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Workgroup. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. Suppl. 2012, 2, c179–c184. [Google Scholar] [CrossRef] [Green Version]
- Delanaye, P.; Glassock, R.J.; Pottel, H.; Rule, A.D. An Age-Calibrated Definition of Chronic Kidney Disease: Rationale and Benefits. Clin. Biochem. Rev. 2016, 37, 17–26. [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Chapter 1: Definition and classification of CKD. Kidney Int. Suppl. 2013, 3, 19–62. [Google Scholar] [CrossRef] [Green Version]
- Levin, A.; Stevens, P.E. Summary of KDIGO 2012 CKD Guideline: Behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014, 85, 49–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galle, J. Glomeruläre Filtrationsrate: Fallstricke der Berechnung. Dtsch. Ärztebl. 2016, 113, 33–34. [Google Scholar] [CrossRef]
- Thomas, C.; Thomas, L. Renal failure—measuring the glomerular filtration rate. Dtsch. Arztebl. Int. 2009, 106, 849–854. [Google Scholar] [CrossRef]
- van den Brand, J.A.; van Boekel, G.A.; Willems, H.L.; Kiemeney, L.A.; den Heijer, M.; Wetzels, J.F. Introduction of the CKD-EPI equation to estimate glomerular filtration rate in a Caucasian population. Nephrol. Dial. Transplant. 2011, 26, 3176–3181. [Google Scholar] [CrossRef] [Green Version]
- Ebert, N.; Pottel, H.; van der Giet, M.; Kuhlmann, M.K.; Delanaye, P.; Schaeffner, E. The impact of the new CKD-EPI equation on GFR estimation in the elderly. Dtsch. Arztebl. Int. 2022, 119, 694–695. [Google Scholar] [CrossRef]
- Inker, L.A.; Eneanya, N.D.; Coresh, J.; Tighiouart, H.; Wang, D.; Sang, Y.; Crews, D.C.; Doria, A.; Estrella, M.M.; Froissart, M.; et al. Chronic Kidney Disease Epidemiology Collaboration. New Creatinine- and Cystatin C-Based Equations to Estimate GFR without Race. N. Engl. J. Med. 2021, 385, 1737–1749. [Google Scholar] [CrossRef]
- Pottel, H.; Björk, J.; Rule, A.D.; Delanaye, P. Cystatin C-based equation to estimate GFR without the inclusion of race and sex. N. Engl. J. Med. 2023, 388, 333–343. [Google Scholar] [CrossRef]
- Stolpe, S.; Kowall, B.; Scholz, C.; Stang, A.; Blume, C. High Unawareness of Chronic Kidney Disease in Germany. Int. J. Environ. Res. Public Health 2021, 18, 11752. [Google Scholar] [CrossRef]
- Wagner, M.; Wanne, C.; Schich, M.; Kotseva, K.; Wood, D.; Hartmann, K.; Fette, G.; Rücker, V.; Oezkur, M.; Störk, S.; et al. Patient’s and physician’s awareness of kidney disease in coronary heart disease patients—A cross-sectional analysis of the German subset of the EUROASPIRE IV survey. BMC Nephrol. 2017, 18, 321. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, L.-L. Raising awareness, screening and prevention of chronic kidney disease: It takes more than a village. Nephrology 2018, 23, 107–111. [Google Scholar] [CrossRef] [Green Version]
- Welch, J.L.; Bartlett Ellis, R.J.; Perkins, S.M.; Johnson, C.S.; Zimmerman, L.M.; Russell, C.L.; Richards, C.; Guise, D.M.; Decker, B.S. Knowledge and Awareness Among Patients with Chronic Kidney Disease Stage 3. Nephrol. Nurs. J. 2016, 43, 513–519. [Google Scholar] [PubMed]
- Delanaye, P.; Jager, K.J.; Bökenkamp, A.; Christensson, A.; Dubourg, L.; Eriksen, B.O.; Gaillard, F.; Gambaro, G.; van der Giet, M.; Glassock, R.J.; et al. CKD: A Call for an Age-Adapted Definition. J. Am. Soc. Nephrol. 2019, 30, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, S.E.; Böger, C.A.; Krämer, B.K.; Döring, A.; Eheberg, D.; Fischer, B.; John, J.; Koenig, W.; Meisinger, C. Effect of chronic kidney disease and comorbid conditions on health care costs: A 10-year observational study in a general population. Am. J. Nephrol. 2010, 31, 222–229. [Google Scholar] [CrossRef]
- Morales-Alvarez, M.C. Nephrotoxicity of Antimicrobials and Antibiotics. Adv. Chronic Kidney Dis. 2020, 27, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Bairami, S.; Kargar, M. Antibiotics induced acute kidney injury: Incidence, risk factors, onset time and outcome. Acta Med. Iran. 2013, 51, 871–878. [Google Scholar]
- Cattaneo, D.; Gervasoni, C.; Corona, A. The Issue of Pharmacokinetic-Driven Drug-Drug Interactions of Antibiotics: A Narrative Review. Antibiotics 2022, 11, 1410. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Genesis Online Datenbank, Eigene Berechnung: Bevölkerung nach Altersgruppen und Geschlecht 2021—In Mio. und Anteil an der Jeweiligen Altersgruppe in %; am Jahresende. Available online: https://www.sozialpolitik-aktuell.de/files/sozialpolitik-aktuell/_Politikfelder/Bevoelkerung/Datensammlung/PDF-Dateien/abbVIII3.pdf (accessed on 26 January 2023).
- Li, G.; Thabane, L.; Papaioannou, A.; Ioannidis, G.; Levine, M.A.; Adachi, J.D. An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet. Disord. 2017, 18, 46. [Google Scholar] [CrossRef] [Green Version]
- Greco, E.A.; Pietschmann, P.; Migliaccio, S. Osteoporosis and Sarcopenia Increase Frailty Syndrome in the Elderly. Front. Endocrinol. 2019, 10, 255. [Google Scholar] [CrossRef]
- U.S. Preventive Services Task Force. Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann. Intern. Med. 2011, 154, 356–364. [Google Scholar] [CrossRef] [Green Version]
- Drenth-van Maanen, A.C.; Wilting, I.; Jansen, P.A.F. Prescribing medicines to older people-How to consider the impact of ageing on human organ and body functions. Br. J. Clin. Pharmacol. 2020, 86, 1921–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.; Zhang, W.; Ren, H.; Chen, X.; Xie, J.; Chen, N. Diuretics associated acute kidney injury: Clinical and pathological analysis. Fail 2014, 36, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Goicoechea, M.; de Vinuesa, S.G.; Verdalles, U.; Ruiz-Caro, C.; Ampuero, J.; Rincón, A.; Arroyo, D.; Luño, J. Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. CJASN 2010, 5, 1388–1393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mackenzie, I.S.; Hawkey, C.J.; Ford, I.; Greenlaw, N.; Pigazzani, F.; Rogers, A.; Struthers, A.D.; Begg, A.G.; Wei, L.; Avery, A.J.; et al. Allopurinol versus usual care in patients with ischaemic heart disease (ALL-HEART): A multicentre, prospective, randomised, open-label, blinded-endpoint trial. Lancet 2022, 400, 1195–1205. [Google Scholar] [CrossRef]
- Tanaka, A.; Node, K. Xanthine oxidase inhibition for cardiovascular disease prevention. Comment. Lancet 2022, 400, 1172–1173. [Google Scholar] [CrossRef]
- Febuxostat-Ratiopharm 80 mg Filmtabletten. Fachinformation 2019. Available online: https://www.ratiopharm.de/assets/products/de/label/Febuxostat-ratiopharm%2080%20mg%20Filmtabletten%20-%202.pdf?pzn=14168559 (accessed on 21 February 2023).
- Eleftheriadis, T.; Golphinopoulos, S.; Pissas, G.; Stefanidis, I. Asymptomatic hyperuricemia and chronic kidney disease: Narrative review of a treatment controversial. J. Adv. Res. 2017, 8, 555–560. [Google Scholar] [CrossRef]
- Leape, L.L.; Brennan, T.A.; Laird, N.; Lawthers, A.G.; Localio, A.R.; Barnes, B.A.; Hebert, L.; Newhouse, J.P.; Weiler, P.C.; Hiatt, H. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N. Engl. J. Med. 1991, 324, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Sánchez Muñoz-Torrero, J.F.; Barquilla, P.; Velasco, R.; del Fernández Capitan, M.C.; Pacheco, N.; Vicente, L.; Chicón, J.L.; Trejo, S.; Zamorano, J.; Lorenzo Hernandez, A. Adverse drug reactions in internal medicine units and associated risk factors. Eur. J. Clin. Pharmacol. 2010, 66, 1257–1264. [Google Scholar] [CrossRef] [Green Version]
- Dicu-Andreescu, I.; Penescu, M.N.; Căpușă, C.; Verzan, C. Chronic Kidney Disease, Urinary Tract Infections and Antibiotic Nephrotoxicity: Are There Any Relationships? Medicina 2022, 59, 49. [Google Scholar] [CrossRef]
- Su, H.; Lei, C.T.; Zhang, C. Interleukin-6 Signaling Pathway and Its Role in Kidney Disease: An Update. Front. Immunol. 2017, 8, 405. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, C.Y.; Yang, H.Y.; Hsiao, M.C.; Hung, P.H.; Wang, M.C. Risk Factors for Development of Acute Kidney Injury in Patients with Urinary Tract Infection. PLoS ONE 2015, 10, e0133835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fliser, D.; Schröter, M.; Neubeck, M.; Ritz, E. Coadministration of thiazides increases the efficacy of loop diuretics even in patients with advanced renal failure. Kidney Int. 1994, 46, 482–488. [Google Scholar] [CrossRef] [Green Version]
- Al-Aly, Z.; Maddukuri, G.; Xie, Y. Proton Pump Inhibitors and the Kidney: Implications of Current Evidence for Clinical Practice and When and How to Deprescribe. Am. J. Kidney Dis. 2020, 75, 497–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blank, M.L.; Parkin, L.; Paul, C.; Herbison, P. A nationwide nested case-control study indicates an increased risk of acute interstitial nephritis with proton pump inhibitor use. Kidney Int. 2014, 86, 837–844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, Y.; Bowe, B.; Li, T.; Xian, H.; Yan, Y.; Al-Aly, Z. Long-term kidney outcomes among users of proton pump inhibitors without intervening acute kidney injury. Kidney Int. 2017, 91, 1482–1494. [Google Scholar] [CrossRef] [Green Version]
- Lapi, F.; Azoulay, L.; Yin, H.; Nessim, S.J.; Suissa, S. Concurrent use of diuretics, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers with non-steroidal anti-inflammatory drugs and risk of acute kidney injury: Nested case-control study. BMJ 2013, 346, e8525. [Google Scholar] [CrossRef] [Green Version]
- MEDSAFE. NSAIDs and acute kidney injury. MEDSAFE 2013, 34, 14–15. Available online: http://medsafe.govt.nz/profs/PUArticles/June2013NSAIDS.htm (accessed on 21 February 2023).
- Saran, R.; Robinson, B.; Abbott, K.C.; Agodoa, L.Y.C.; Bragg-Gresham, J.; Balkrishnan, R.; Bhave, N.; Dietrich, X.; Ding, Z.; Eggers, P.W.; et al. US Renal Data System 2018 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J. Kidney Dis. 2019, 73, A7–A8. [Google Scholar] [CrossRef] [Green Version]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Chapter 3: Management of progression and complications of CKD. Kidney Int. Suppl. 2013, 3, 73–90. [Google Scholar] [CrossRef] [Green Version]
- Jeong, J.; Kwon, S.K.; Kim, H.Y. Effect of bicarbonate supplementation on renal function and nutritional indices in predialysis advanced chronic kidney disease. Electrolytes Blood Press. 2014, 12, 80–87. [Google Scholar] [CrossRef] [Green Version]
- Susantitaphong, P.; Sewaralthahab, K.; Balk, E.M.; Jaber, B.L.; Madias, N.E. Short- and long-term effects of alkali therapy in chronic kidney disease: A systematic review. Am. J. Nephrol. 2012, 35, 540–547. [Google Scholar] [CrossRef]
- Ying, T.; Chan, S.; Lane, S.; Somerville, C. Acute kidney injury post-major orthopaedic surgery: A single-Centre case-control study. Nephrology 2018, 23, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Naughton, C.A. Drug-induced nephrotoxicity. Am. Fam. Physician 2008, 78, 743–750. [Google Scholar] [PubMed]
- Aucella, F.; Corsonello, A.; Soraci, L.; Fabbietti, P.; Prencipe, M.A.; Gatta, G.; Lattanzio, F.; Cortese, L.; Pagnotta, M.R.; Antonelli Incalzi, R. A focus on CKD reporting and inappropriate prescribing among older patients discharged from geriatric and nephrology units throughout Italy: A nationwide multicenter retrospective cross-sectional study. Front. Pharmacol. 2022, 13, 996042. [Google Scholar] [CrossRef] [PubMed]
- Mangin, D.; Bahat, G.; Golomb, B.A.; Mallery, L.H.; Moorhouse, P.; Onder, G.; Petrovic, M.; Garfinkel, D. International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): Position Statement and 10 Recommendations for Action. Drugs Aging 2018, 35, 575–587. [Google Scholar] [CrossRef] [Green Version]
- Hsu, R.K.; Hsu, C.Y. The Role of Acute Kidney Injury in Chronic Kidney Disease. Semin. Nephrol. 2016, 36, 283–292. [Google Scholar] [CrossRef] [Green Version]
- Hobson, C.; Ruchi, R.; Bohorac, A. Perioperative acute kidney injury. Crit. Care Clin. 2017, 33, 379–396. [Google Scholar] [CrossRef] [Green Version]
- Romagnoli, S.; Ricci, Z.; Ronco, C. Perioperative Acute Kidney Injury: Prevention, Early Recognition, and Supportive Measures. Nephron 2018, 140, 105–110. [Google Scholar] [CrossRef]
- Pathak, S.; Olivieri, G.; Mohamed, W.; Abbasciano, R.; Roman, M.; Tomassini, S.; Lai, F.; Wozniak, M.; Murphy, G.J. Pharmacological interventions for the prevention of renal injury in surgical patients: A systematic literature review and meta-analysis. Br. J. Anaesth. 2021, 126, 131–138. [Google Scholar] [CrossRef]
- Gameiro, J.; Fonseca, J.A.; Outerelo, C.; Lopes, J.A. Acute Kidney Injury: From Diagnosis to Prevention and Treatment Strategies. J. Clin. Med. 2020, 9, 1704. [Google Scholar] [CrossRef]
- Chawla, L.S.; Eggers, P.W.; Star, R.A.; Kimmel, P.L. Acute Kidney Injury and Chronic Kidney Disease as Interconnected Syndromes. N. Engl. J. Med. 2014, 371, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Calvert, S.; Shaw, A. Perioperative acute kidney injury. Perioper Med. 2012, 1, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liangos, O.; Wald, R.; O’Bell, J.W.; Price, L.; Pereira, B.J.; Jaber, B.L. Epidemiology and outcomes of acute renal failure in hospitalized patients: A national survey. Clin. J. Am. Soc. Nephrol. 2006, 1, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Brennan, T.A.; Leape, L.L.; Laird, N.M.; Hebert, L.; Localio, A.R.; Lawthers, A.G.; Newhouse, J.P.; Weiler, P.C.; Hiatt, H.H. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N. Engl. J. Med. 1991, 324, 370–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Douros, A.; Bronder, E.; Klimpel, A.; Erley, C.; Garbe, E.; Kreutz, R. Drug-induced kidney injury: A large case series from the Berlin Case-Control Surveillance Study. Clin. Nephrol. 2018, 89, 18–26. [Google Scholar] [CrossRef]
- Dormuth, C.R.; Hemmelgarn, B.R.; Paterson, J.M.; James, M.T.; Teare, G.F.; Raymond, C.B.; Lafrance, J.P.; Levy, A.; Garg, A.X.; Ernst, P.; et al. Use of high potency statins and rates of admission for acute kidney injury: Multicenter, retrospective observational analysis of administrative databases. BMJ (Clin. Res. Ed.) 2013, 346, f880. [Google Scholar] [CrossRef] [Green Version]
- Keys, D.O.; Edelstein, C.L. High-potency statins are associated with increased hospitalisations with acute kidney injury. Evid.-Based Med. 2014, 19, 28. [Google Scholar] [CrossRef] [Green Version]
- Yau, K.; Dharia, A.; Alrowiyti, I.; Cherney, D.Z.I. Prescribing SGLT2 Inhibitors in Patients With CKD: Expanding Indications and Practical Considerations. Kidney Int. Rep. 2022, 7, 1463–1476. [Google Scholar] [CrossRef]
- Wheeler, D.C.; Stefansson, B.V.; Batiushin, M.; Bilchenko, O.; Cherney, D.Z.I.; Chertow, G.M.; Douthat, W.; Dwyer, J.P.; Escudero, E.; Pecoits-Filho, R.; et al. The dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial: Baseline characteristics. Nephrol. Dial. Transplant. 2020, 35, 1700–1711. [Google Scholar] [CrossRef]
- Shi, S.; Mörike, K.; Klotz, U. The clinical implications of ageing for rational drug therapy. Eur. J. Clin. Pharmacol. 2008, 64, 183–199. [Google Scholar] [CrossRef]



|
|
|
|
|
|
|
|
| Renal Impairment at Admission * | CG n = 199 | IG n = 204 |
|---|---|---|
| eGFR <60 mL/min/1.73 m2 | 83 (41.7%) | 101 (49.5%) |
| CKD 3a | 38 (19.1%) | 47 (23.0%) |
| CKD 3b | 24 (12.1%) | 33 (16.2%) |
| CKD 4 | 17 (8.5%) | 13 (6.4%) |
| CKD 5 | 4 (2.0%) | 8 (3.9%) |
| Patient Number | Mean | Standard Error | Standard Deviation | |
|---|---|---|---|---|
| BIS-1-formula | 42 | 21.89 | 1.08 | 7.01 |
| eGFR (0–29.99 mL/min) | 42 | 20.01 | 1.10 | 7.16 |
| BIS-1-formula | 142 | 42.21 | 0.70 | 8.38 |
| * eGFR (30–59.99 mL/min) | 142 | 46.75 | 0.71 | 8.49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolf, U.; Ghadir, H.; Drewas, L.; Neef, R. Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III). J. Clin. Med. 2023, 12, 4545. https://doi.org/10.3390/jcm12134545
Wolf U, Ghadir H, Drewas L, Neef R. Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III). Journal of Clinical Medicine. 2023; 12(13):4545. https://doi.org/10.3390/jcm12134545
Chicago/Turabian StyleWolf, Ursula, Hassan Ghadir, Luise Drewas, and Rüdiger Neef. 2023. "Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III)" Journal of Clinical Medicine 12, no. 13: 4545. https://doi.org/10.3390/jcm12134545




