The Direct Anterior Approach (DAA) as a Standard Approach for Total Hip Arthroplasty (THA) in Coxa Profunda and Protrusio Acetabuli? A Radiographic Analysis of 188 Cases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Surgical Procedure
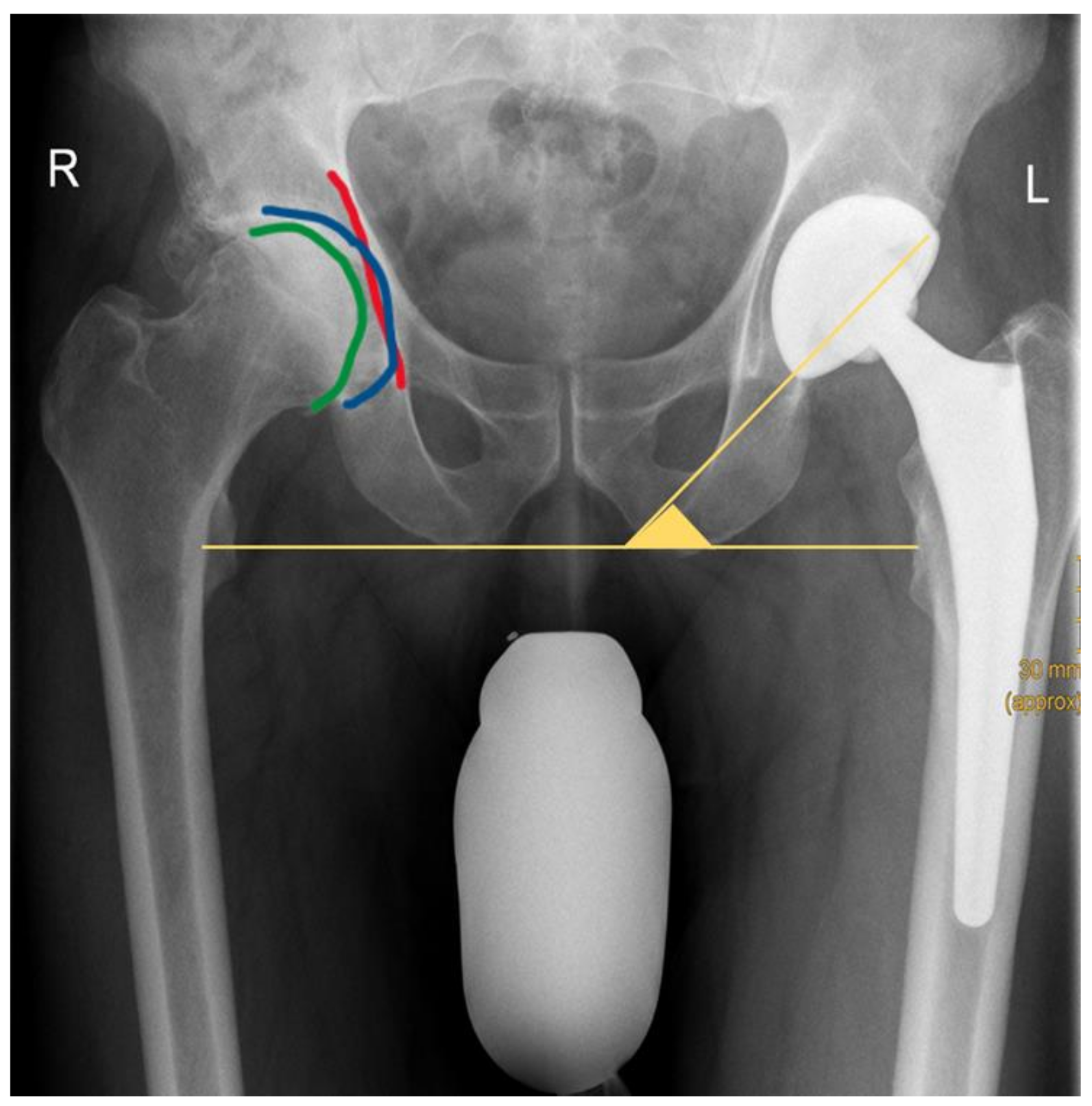
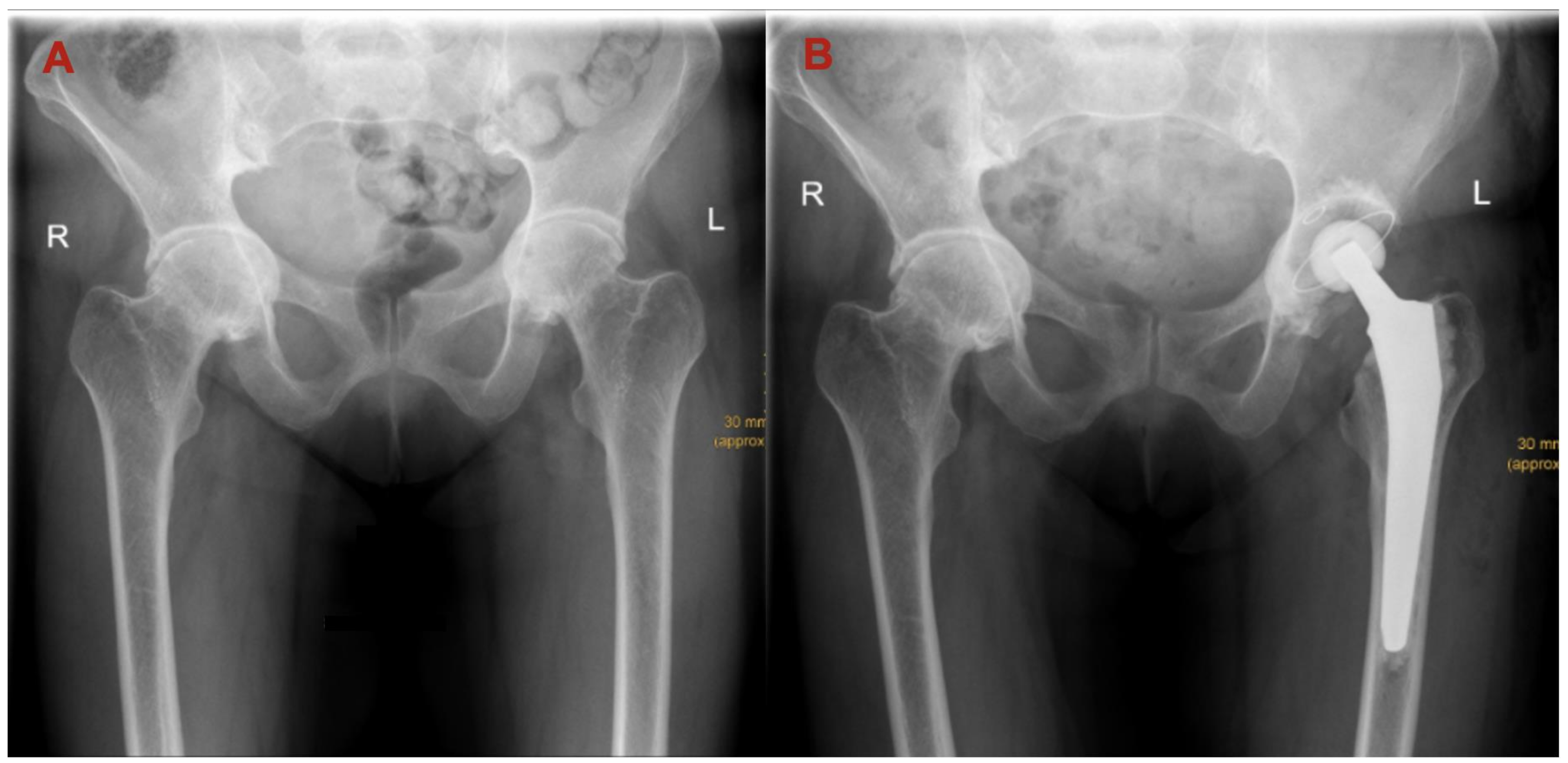
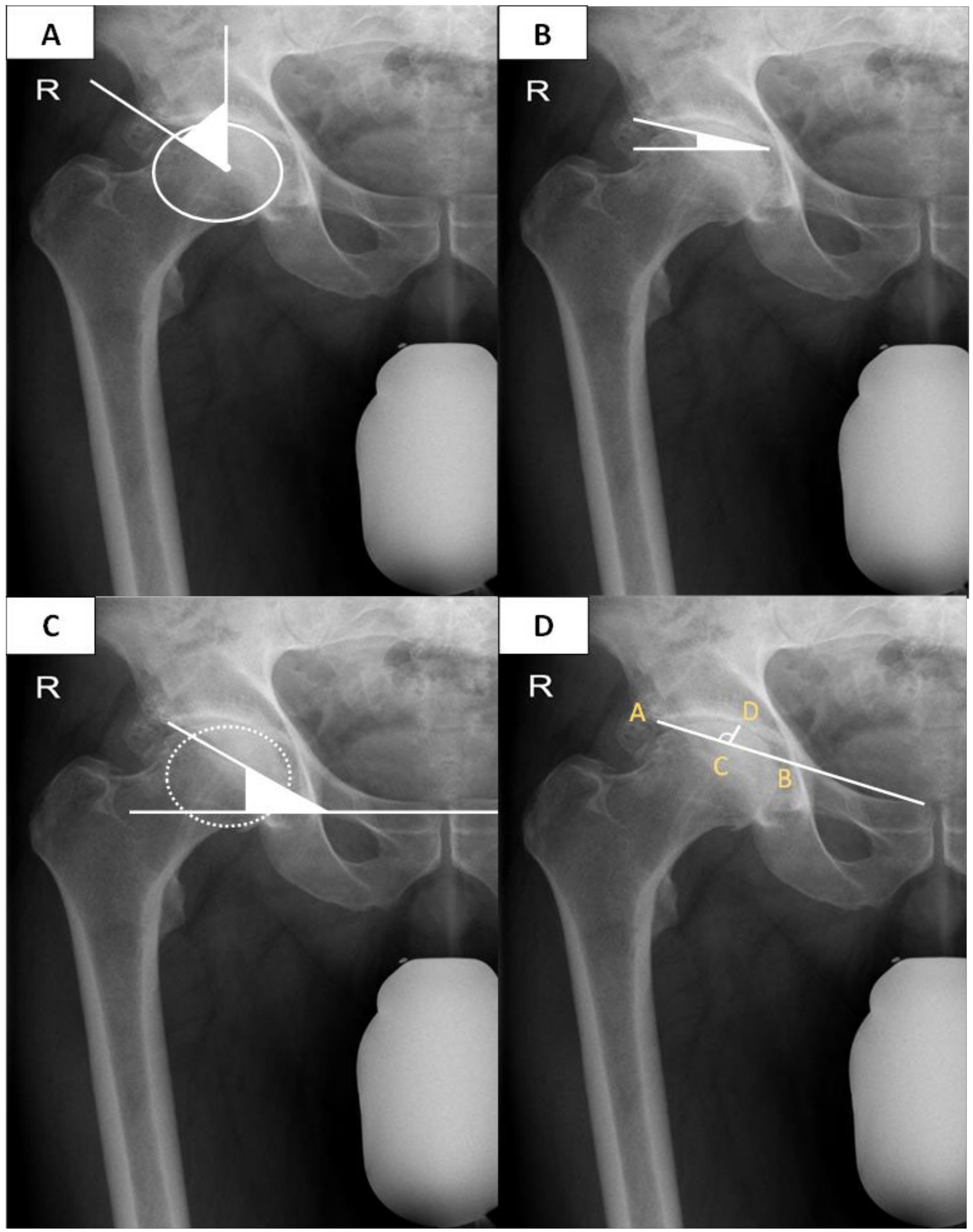
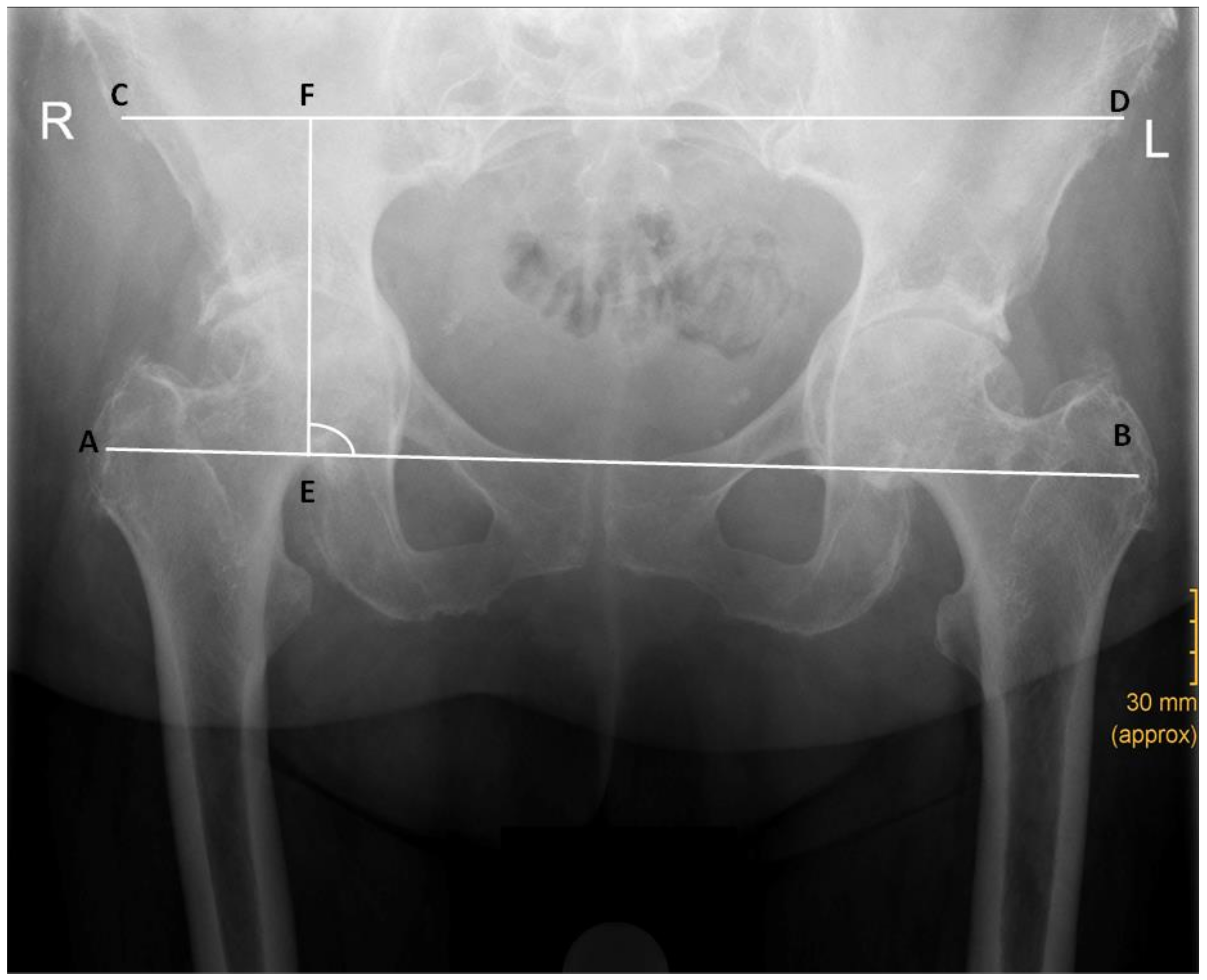
2.3. Measurements
2.4. Statistics
3. Results
3.1. Patient Demographics
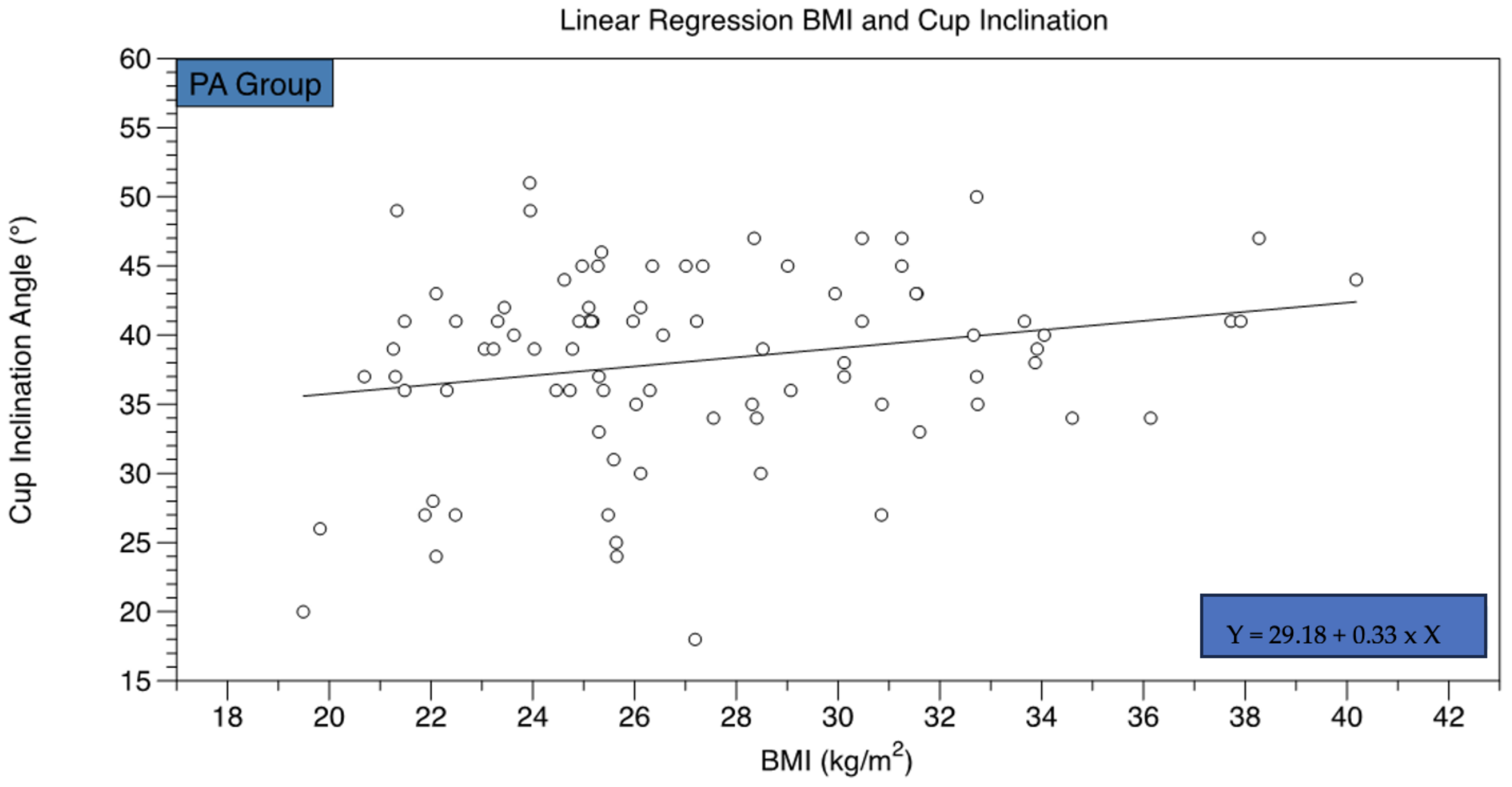
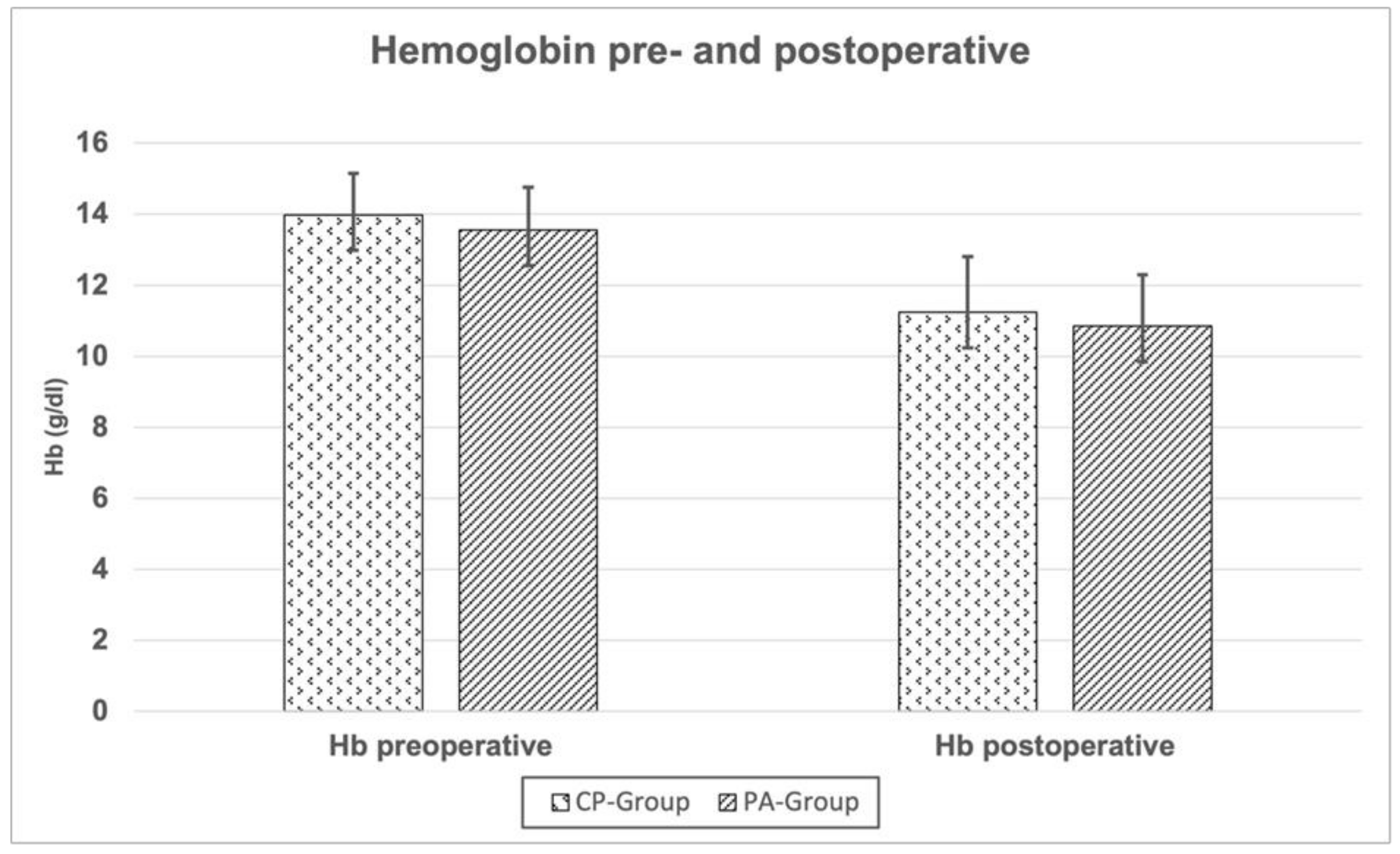
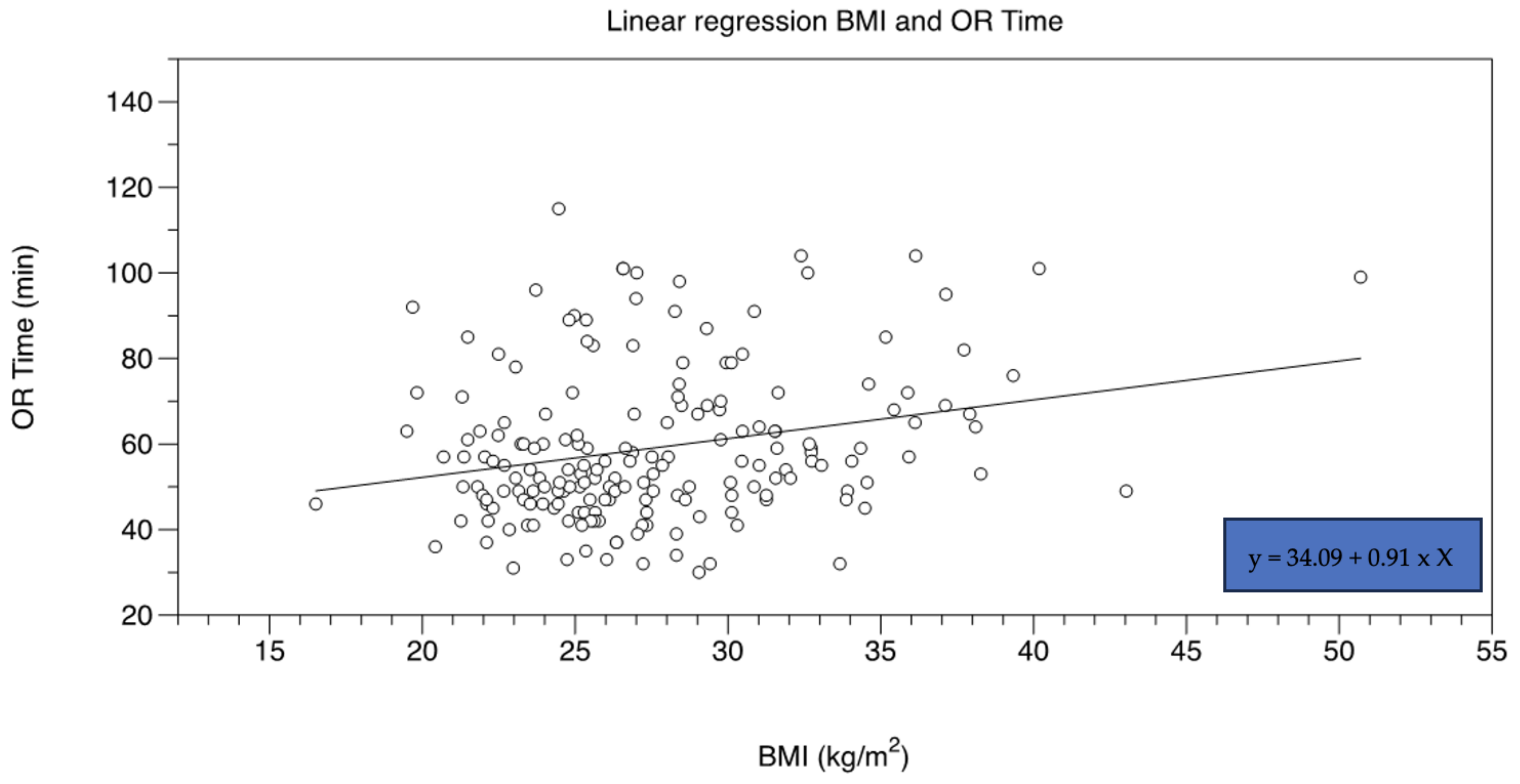
3.2. Radiographic Outcomes
3.3. Clinical Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Callaghan, J.J.; Albright, J.C.; Goetz, D.D.; Olejniczak, J.P.; Johnston, R.C. Charnley total hip arthroplasty with cement: Minimum twenty-five-year follow-up. Jbjs 2000, 82, 487. [Google Scholar] [CrossRef] [PubMed]
- Okafor, L.; Chen, A.F. Patient satisfaction and total hip arthroplasty: A review. Arthroplasty 2019, 1, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Charnley, J. Arthroplasty of the hip: A new operation. Lancet 1961, 277, 1129–1132. [Google Scholar] [CrossRef]
- Unger, A.S.; Stronach, B.M.; Bergin, P.F.; Nogler, M. Direct anterior total hip arthroplasty. Instr. Course Lect. 2014, 63, 227–239. [Google Scholar] [PubMed]
- Rachbauer, F.; Kain, M.S.; Leunig, M. The history of the anterior approach to the hip. Orthop. Clin. N. Am. 2009, 40, 311–320. [Google Scholar] [CrossRef]
- Smith-Petersen, M.N. A New Supra-Articular Subperiosteal Approach to the Hip Joint. JBJS 1917, s2–s15, 592–595. [Google Scholar]
- Judet, J.; Judet, R. The use of an artificial femoral head for arthroplasty of the hip joint. J. Bone Jt. Surg Br. 1950, 32-b, 166–173. [Google Scholar] [CrossRef]
- Meermans, G.; Konan, S.; Das, R.; Volpin, A.; Haddad, F.S. The direct anterior approach in total hip arthroplasty. Bone Jt. J. 2017, 99-B, 732–740. [Google Scholar] [CrossRef]
- Abdel, M.P.; Berry, D.J. Current Practice Trends in Primary Hip and Knee Arthroplasties among Members of the American Association of Hip and Knee Surgeons: A Long-Term Update. J. Arthroplast. 2019, 34 (Suppl. S7), S24–S27. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.; Kim, P.R. Complications of the Direct Anterior Approach for Total Hip Arthroplasty. Orthop. Clin. N. Am. 2009, 40, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Mast, N.H.; Laude, F. Revision Total Hip Arthroplasty Performed through the Hueter Interval. JBJS 2011, 93 (Suppl. S2), 143–148. [Google Scholar] [CrossRef] [PubMed]
- Kennon, R.; Keggi, J.; Zatorski, L.E.; Keggi, K.J. Anterior approach for total hip arthroplasty: Beyond the minimally invasive technique. JBJS 2004, 86, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Nogler, M.M.; Thaler, M.R. The Direct Anterior Approach for Hip Revision: Accessing the Entire Femoral Diaphysis without Endangering the Nerve Supply. J. Arthroplast. 2017, 32, 510–514. [Google Scholar] [CrossRef]
- Randelli, F.; Viganò, M.; Holzapfel, B.M.; Corten, K.; Thaler, M. Conversion hip arthroplasty via the direct anterior approach: Pearls, pitfalls and personal experience. Oper. Orthop. Traumatol. 2022, 34, 177–188. [Google Scholar] [CrossRef]
- Rudert, M.; Thaler, M.; Holzapfel, B.M. Primary hip arthroplasty via the direct anterior approach—German version. Oper. Orthop. Traumatol. 2021, 33, 285–286. [Google Scholar] [CrossRef]
- Molenaers, B.; Driesen, R.; Molenaers, G.; Corten, K. The Direct Anterior Approach for Complex Primary Total Hip Arthroplasty: The Extensile Acetabular Approach on a Regular Operating Room Table. J. Arthroplast. 2017, 32, 1553–1559. [Google Scholar] [CrossRef]
- Realyvasquez, J.; Singh, V.; Shah, A.K.; Ortiz, D.; Robin, J.X.; Brash, A.; Kurapatti, M.; Davidovitch, R.I.; Schwarzkopf, R. The direct anterior approach to the hip: A useful tool in experienced hands or just another approach? Arthroplasty 2022, 4, 1. [Google Scholar] [CrossRef]
- Galakatos, G.R. Direct Anterior Total Hip Arthroplasty. Mo. Med. 2018, 115, 537–541. [Google Scholar]
- Clohisy, J.C.; Carlisle, J.C.; Beaulé, P.E.; Kim, Y.J.; Trousdale, R.T.; Sierra, R.J.; Leunig, M.; Schoenecker, P.L.; Millis, M.B. A systematic approach to the plain radiographic evaluation of the young adult hip. J. Bone Jt. Surg Am. 2008, 90 (Suppl. S4), 47–66. [Google Scholar] [CrossRef] [Green Version]
- Yun, A.; Qutami, M.; Carles, E. Managing Protrusio Acetabuli with a Direct Anterior Approach Total Hip Replacement. Cureus 2021, 13, e14048. [Google Scholar] [CrossRef] [PubMed]
- Mannava, S.; Geeslin, A.G.; Frangiamore, S.J.; Cinque, M.E.; Geeslin, M.G.; Chahla, J.; Philippon, M.J. Comprehensive Clinical Evaluation of Femoroacetabular Impingement: Part 2, Plain Radiography. Arthrosc. Tech. 2017, 6, e2003–e2009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanson, J.A.; Kapron, A.L.; Swenson, K.M.; Maak, T.G.; Peters, C.L.; Aoki, S.K. Discrepancies in measuring acetabular coverage: Revisiting the anterior and lateral center edge angles. J. Hip Preserv. Surg. 2015, 2, 280–286. [Google Scholar] [CrossRef] [Green Version]
- Stone, J.; Kennedy, J. The Foot and Ankle: AANA Advanced Arthroscopic Surgical Techniques; Slack Incorporated: West Deptford, NJ, USA, 2016. [Google Scholar]
- Popat, R.; Lee, S.; George, D.A.; Amiras, D.; Sarraf, K.M. Assessment of the young adult hip joint using plain radiographs. Musculoskelet Surg. 2020, 104, 245–255. [Google Scholar] [CrossRef] [Green Version]
- Jesse, M.K.; Petersen, B.; Strickland, C.; Mei-Dan, O. Normal anatomy and imaging of the hip: Emphasis on impingement assessment. In Seminars in Musculoskeletal Radiology; Thieme Medical Publishers: New York, NY, USA, 2013. [Google Scholar]
- Sang, W.; Zhu, L.; Ma, J.; Lu, H.; Wang, C. The Influence of Body Mass Index and Hip Anatomy on Direct Anterior Approach Total Hip Replacement. Med. Princ. Pract. 2016, 25, 555–560. [Google Scholar] [CrossRef]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Ani, L.; Radford, Z.; Rubin, L.E. Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations. Osteology 2023, 3, 33–46. [Google Scholar] [CrossRef]
- McBride, M.T.; Muldoon, M.P.; Santore, R.F.; Trousdale, R.T.; Wenger, D.R. Protrusio acetabuli: Diagnosis and treatment. JAAOS J. Am. Acad. Orthop. Surg. 2001, 9, 79–88. [Google Scholar] [CrossRef]
- Baghdadi, Y.M.; Larson, A.N.; Sierra, R.J. Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin. Orthop. Relat. Res. 2013, 471, 3251–3259. [Google Scholar] [CrossRef] [Green Version]
- Mullaji, A.B.; Marawar, S.V. Primary Total Hip Arthroplasty in Protrusio Acetabuli Using Impacted Morsellized Bone Grafting and Cementless Cups: A Medium-Term Radiographic Review. J. Arthroplast. 2007, 22, 1143–1149. [Google Scholar] [CrossRef]
- Manrique, J.; Chen, A.F.; Heller, S.; Hozack, W.J. Direct anterior approach for revision total hip arthroplasty. Ann. Transl. Med. 2014, 2, 100. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.; Tarr, R.; Compere, C.; Zimmerman, J. Dislocations after total hip-replacement arthroplasties. Jbjs 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Edeen, J.; Sharkey, P.; Alexander, A. Clinical significance of leg-length inequality after total hip arthroplasty. Am. J. Orthop. 1995, 24, 347–351. [Google Scholar] [PubMed]
- Austin, M.S.; Hozack, W.J.; Sharkey, P.F.; Rothman, R.H. Stability and leg length equality in total hip arthroplasty. J. Arthroplast. 2003, 18, 88–90. [Google Scholar] [CrossRef] [PubMed]
- Love, B. Leg length discrepancy after total hip replacement. J. Bone Jt. Surg. B 1983, 65, 103. [Google Scholar]
- Vanrusselt, J.; Vansevenant, M.; Vanderschueren, G.; Vanhoenacker, F. Postoperative radiograph of the hip arthroplasty: What the radiologist should know. Insights Imaging 2015, 6, 591–600. [Google Scholar] [CrossRef] [Green Version]
- Hochreiter, J.; Hejkrlik, W.; Emmanuel, K.; Hitzl, W.; Ortmaier, R. Blood loss and transfusion rate in short stem hip arthroplasty. A comparative study. Int. Orthop. 2017, 41, 1347–1353. [Google Scholar] [CrossRef] [Green Version]
- Zha, G.-C.; Zhu, X.-R.; Wang, L.; Li, H.-W. Tranexamic acid reduces blood loss in primary total hip arthroplasty performed using the direct anterior approach: A one-center retrospective observational study. J. Orthop. Traumatol. 2022, 23, 12. [Google Scholar] [CrossRef]
- Duchman, K.R.; Pugely, A.J.; Martin, C.T.; Gao, Y.; Bedard, N.A.; Callaghan, J.J. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J. Arthroplast. 2017, 32, 1285–1291. [Google Scholar] [CrossRef]
- Cantrell, W.A.; Samuel, L.T.; Sultan, A.A.; Acuña, A.J.; Kamath, A.F. Operative Times Have Remained Stable for Total Hip Arthroplasty for >15 Years: Systematic Review of 630,675 Procedures. JBJS Open Access 2019, 4, e0047. [Google Scholar] [CrossRef] [Green Version]

| Mean (±SD) or Relative Frequency (%) | p-Value (CP Group vs. PA Group) | ||
|---|---|---|---|
| PA Group | Sex (m/f) | 14.80%/85.20% | 0.55 |
| Age, years (a) | 71.52 + 12.46 | 0.01 | |
| BMI (kg/m2) | 27.24 ± 4.61 | 0.36 | |
| VAS, preoperative | 5.93 ± 2.14 | 0.95 | |
| Hip flexion, preoperative (degrees) | 83.61° ± 18.88° | 0.00 | |
| Hip abduction, preoperative (degrees) | 13.03° ± 8.33° | 0.00 | |
| Hip adduction, preoperative (degrees) | 10.43° ± 7.35° | 0.53 | |
| Hip flexion, postoperative (degrees) | 84.70° ± 8.20° | 0.06 | |
| Cemented cups | 5 (5.68%) | 0.02 | |
| Sex (m/f) | 18.0%/82.0% | 0.55 | |
| CP Group | Age, years (a) | 66.96 ± 10.15 | 0.01 |
| BMI (kg/m2) | 27.91 ± 5.25 | 0.36 | |
| VAS, preoperative | 5.90 ± 2.29 | 0.95 | |
| Hip flexion, preoperative (degrees) | 92.22 ± 15.00 | 0.00 | |
| Hip abduction, preoperative (degrees) | 18.72° ± 10.95° | 0.00 | |
| Hip adduction, preoperative (degrees) | 11.38° ± 8.21° | 0.53 | |
| Hip flexion, postoperative (degrees) | 86.76° ± 5.76° | 0.06 | |
| Cemented cups | 0 (0.00%) | 0.02 |
| Radiographic Parameter | CP Group | PA Group | p-Value (CP vs. PA) |
|---|---|---|---|
| LCEA (mean ± SD) | 40.41° ± 9.82° | 55.09° ± 9.64° | <0.00 |
| Sharp (mean ± SD) | 36.44° ± 5.15° | 34.04° ± 4.81° | <0.00 |
| Tönnis (mean ± SD) | 6.16° ± 5.70° | 3.12° ± 5.89° | <0.00 |
| Acetabular depth (mean ± SD) | 24.73 mm ± 4.01 mm | 27.92 mm ± 4.67 mm | <0.00 |
| ADWR (mean ± SD) | 334.60 ± 43.33 | 388.50 ± 61.22 | <0.00 |
| Change of FO (preoperative vs. postoperative) (mean ± SD) | 4.11 mm ± 7.66 mm | 0.71 mm ± 8.21 mm | <0.00 |
| FO, preoperative (mean ± SD) | 42.94 mm ± 7.20 mm | 46.22 mm ± 7.57 mm | <0.00 |
| FO, postoperative | 47.05 mm ± 5.38 mm | 45.52 mm ± 4.46 mm | 0.03 |
| LLD, preoperative (mean ± SD) | 4.49 mm ± 4.24 mm | 7.65 mm ± 6.76 mm | <0.00 |
| LLD, postoperative (mean ± SD) | 4.87 mm ± 4.12 mm | 5.41 mm ± 5.00 mm | 0.41 |
| AGVD (mean ± SD) | 108.59 mm ± 13.75 mm | 101.91 mm ± 14.36 mm | <0.00 |
| GT/ASIS (mean ± SD) | 1.19 ± 0.07 | 1.13 ± 0.07 | <0.00 |
| Cup inclination | 36.57° ± 6.57° | 38.13° ± 6.82° | 0.04 |
| Preoperative Value | Postoperative Value | p-Value | ||
|---|---|---|---|---|
| CP Group | FO (mean ± SD) | 42.94 mm ± 7.20 mm | 47.05 mm ± 5.38 mm | <0.00 |
| LLD (mean ± SD) | 4.49 mm ± 4.24 mm | 4.87 mm + 4.12 mm | 0.48 | |
| PA Group | FO (mean ± SD) | 46.22 mm ± 7.57 mm | 45.52 mm ± 4.46 mm | 0.42 |
| LLD (mean ± SD) | 7.65 mm ± 6.76 mm | 5.41 mm ± 5.00 mm | 0.02 |
| CP Group | PA Group | p-Value | |
|---|---|---|---|
| Change of Hb (preoperative vs. postoperative) (mean ± SD) | 2.73 g/dL ± 1.22 g/dL | 2.66 g/dL ± 1.18 g/dL | 0.71 |
| Operative time (mean ± SD) | 59.62 min ± 17.78 min | 58.50 min ± 17.81 min | 0.67 |
| LOS (days) (mean ± SD) | 8.44 ± 2.09 | 9.11 ± 3.58 | 0.11 |
| Complication rates (total number n, percent) | |||
| Postoperative anemia | 3 (3.00%) | 2 (2.27%) | 0.54 |
| Prolonged wound healing | 4 (4.00%) | 4 (4.54%) | |
| Postoperative regional paresthesia | 2 (2.00%) | 1 (1.14%) | |
| Respiratory infection Intraoperative fracture (femur or acetabulum) | 2 (2.00%) 1 (0.53%) | 2 (2.27%) 2 (1.06%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinz, T.; Vasilev, H.; Anderson, P.M.; Stratos, I.; Jakuscheit, A.; Horas, K.; Holzapfel, B.M.; Rudert, M.; Weißenberger, M. The Direct Anterior Approach (DAA) as a Standard Approach for Total Hip Arthroplasty (THA) in Coxa Profunda and Protrusio Acetabuli? A Radiographic Analysis of 188 Cases. J. Clin. Med. 2023, 12, 3941. https://doi.org/10.3390/jcm12123941
Heinz T, Vasilev H, Anderson PM, Stratos I, Jakuscheit A, Horas K, Holzapfel BM, Rudert M, Weißenberger M. The Direct Anterior Approach (DAA) as a Standard Approach for Total Hip Arthroplasty (THA) in Coxa Profunda and Protrusio Acetabuli? A Radiographic Analysis of 188 Cases. Journal of Clinical Medicine. 2023; 12(12):3941. https://doi.org/10.3390/jcm12123941
Chicago/Turabian StyleHeinz, Tizian, Hristo Vasilev, Philip Mark Anderson, Ioannis Stratos, Axel Jakuscheit, Konstantin Horas, Boris Michael Holzapfel, Maximilian Rudert, and Manuel Weißenberger. 2023. "The Direct Anterior Approach (DAA) as a Standard Approach for Total Hip Arthroplasty (THA) in Coxa Profunda and Protrusio Acetabuli? A Radiographic Analysis of 188 Cases" Journal of Clinical Medicine 12, no. 12: 3941. https://doi.org/10.3390/jcm12123941






