Plasma-Metanephrines in Patients with Autoimmune Addison’s Disease with and without Residual Adrenocortical Function
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Cosyntropin Testing and Metanephrine Assay
2.3. Statistics
2.4. Ethics
3. Results
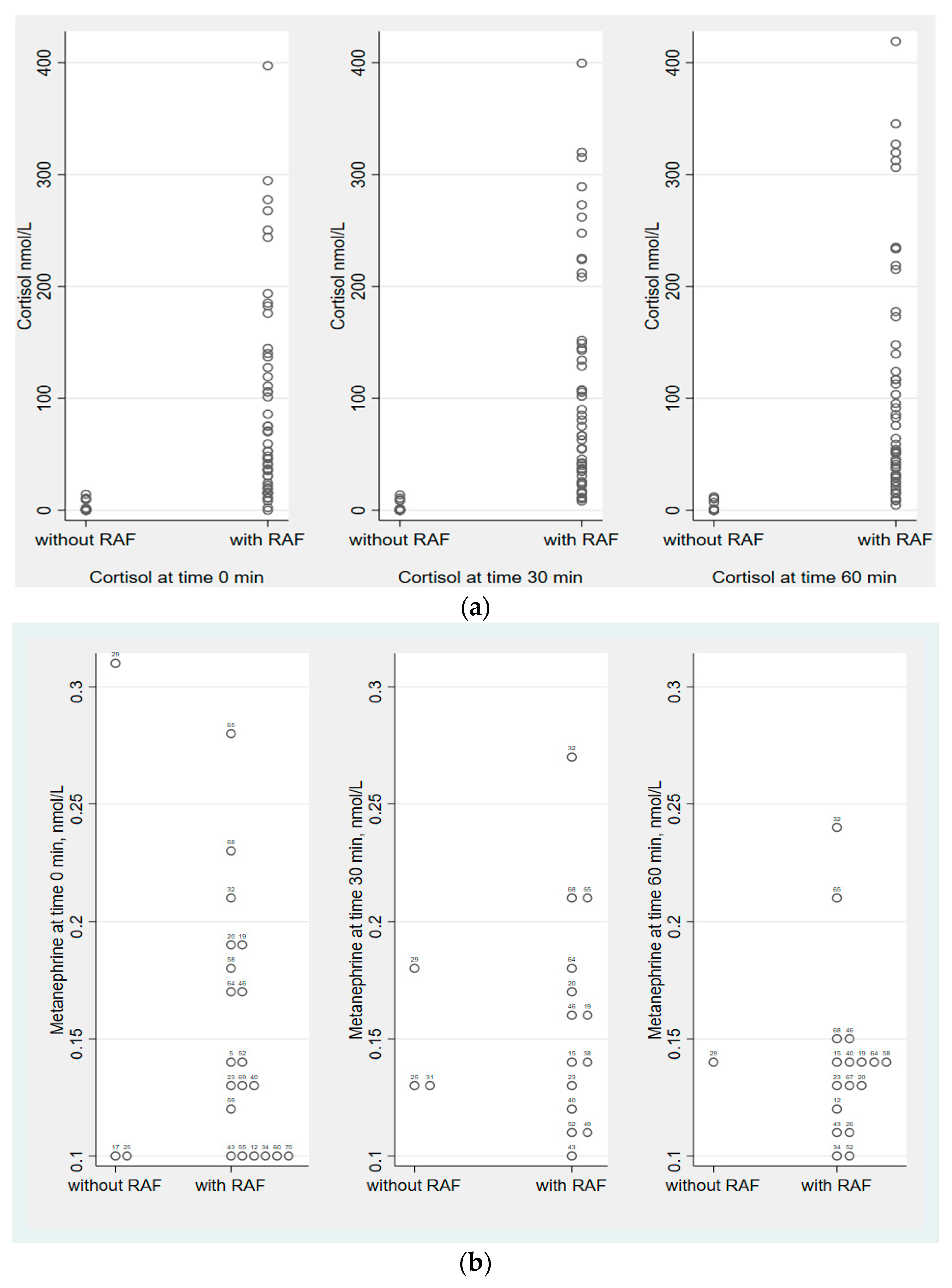
3.1. Comparison of Patients with and without RAF
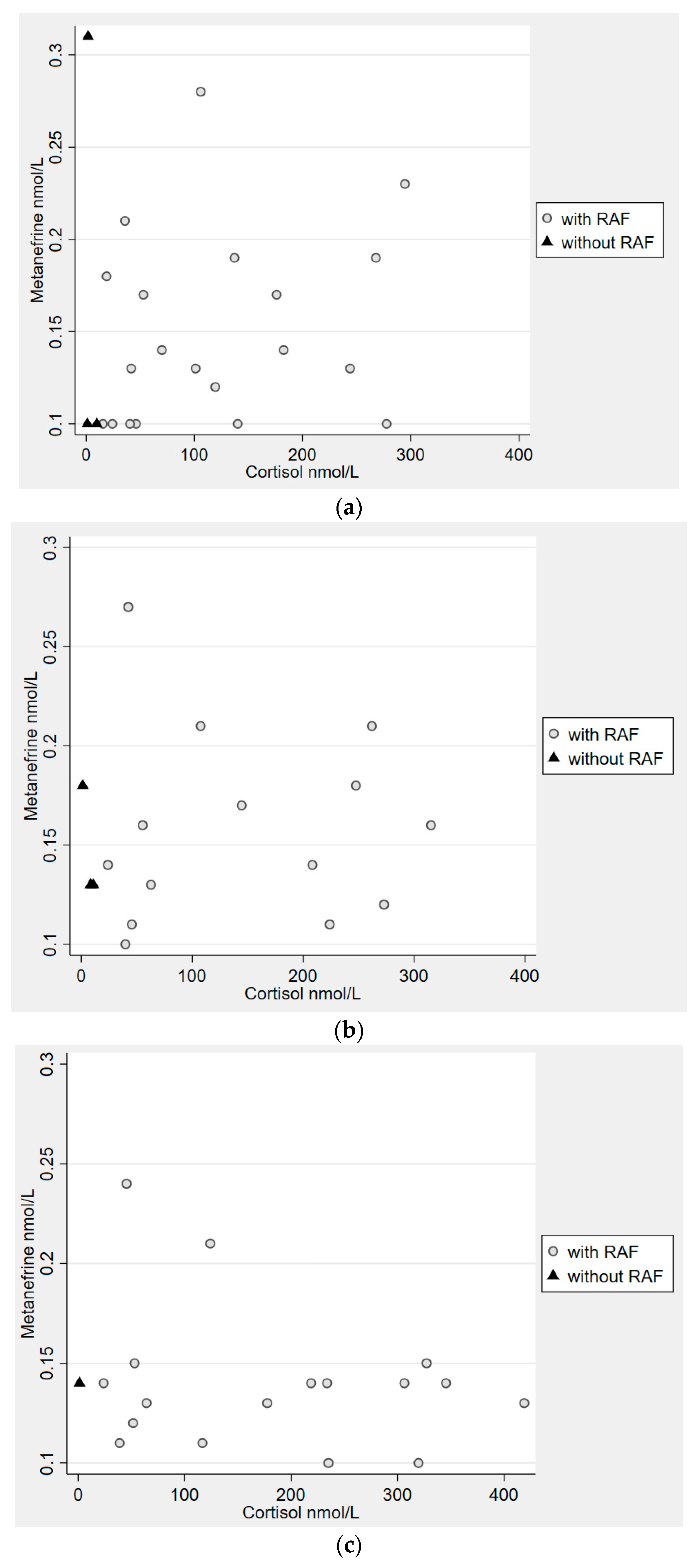
3.2. Metanephrine and Cortisol
3.3. Normetanephrine
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Trial Registration
Abbreviations
| AAD | Autoimmune Addison’s disease |
| ACTH | Adrenocorticotropic hormone |
| AD | Aldehyde dehydrogenase |
| BP | Blood pressure |
| CAH | Congenital adrenal hyperplasia |
| COMT | Catechol O-methyltransferase |
| DBH | DOPA β-hydroxylase |
| DDC | DOPA decarboxylase |
| GC | Glucocorticoid |
| LC-MS/MS | Liquid chromatography–tandem-mass spectrometry |
| MAO | Monoaminoxidase |
| MN | Metanephrine |
| NMN | Normetanephrine |
| PAH | Phenylalanine hydroxylase |
| PNMT | Phenylethanolamine-N-methyltransferase |
| RAF | Residual adrenocorticoid function |
| TH | Tyrosine hydroxylase |
References
- Willenberg, H.S.; Bornstein, S.R. Adrenal Cortex; Development, Anatomy, Physiology. In Endotext; Feingold, K.R., Ed.; MDText.com, Inc.: South Dartmouth, MA, USA, 2017. [Google Scholar]
- Pignatti, E.; Flück, C.E. Adrenal cortex development and related disorders leading to adrenal insufficiency. Mol. Cell. Endocrinol. 2021, 527, 111206. [Google Scholar] [CrossRef] [PubMed]
- Bechmann, N.; Berger, I.; Bornstein, S.R.; Steenblock, C. Adrenal medulla development and medullary-cortical interactions. Mol. Cell. Endocrinol. 2021, 528, 111258. [Google Scholar] [CrossRef] [PubMed]
- Ventura Spagnolo, E.; Mondello, C.; Cardia, L.; Minutoli, L.; Puzzolo, D.; Asmundo, A.; Macaione, V.; Alibrandi, A.; Malta, C.; Baldino, G.; et al. Post-Mortem Immunohistochemical Evidence of β2-Adrenergic Receptor Expression in the Adrenal Gland. Int. J. Mol. Sci 2019, 20, 3065. [Google Scholar] [CrossRef] [PubMed]
- Haase, M.; Willenberg, H.S.; Bornstein, S.R. Update on the corticomedullary interaction in the adrenal gland. Endocr. Dev. 2011, 20, 28–37. [Google Scholar] [CrossRef]
- Kastriti, M.E.; Kameneva, P.; Adameyko, I. Stem cells, evolutionary aspects and pathology of the adrenal medulla: A new developmental paradigm. Mol. Cell. Endocrinol. 2020, 518, 110998. [Google Scholar] [CrossRef]
- Ehrhart-Bornstein, M.; Bornstein, S.R. Cross-talk between adrenal medulla and adrenal cortex in stress. Ann. N. Y. Acad. Sci. 2008, 1148, 112–117. [Google Scholar] [CrossRef]
- Ehrhart-Bornstein, M.; Hinson, J.P.; Bornstein, S.R.; Scherbaum, W.A.; Vinson, G.P. Intraadrenal interactions in the regulation of adrenocortical steroidogenesis. Endocr. Rev. 1998, 19, 101–143. [Google Scholar] [CrossRef]
- Wurtman, R.J.; Axelrod, J. Adrenaline synthesis: Control by the pituitary gland and adrenal glucocorticoids. Science 1965, 150, 1464–1465. [Google Scholar] [CrossRef]
- Wurtman, R.J.; Pohorecky, L.A. Adrenocortical control of epinephrine synthesis in health and disease. Adv. Metab. Disord. 1971, 5, 53–76. [Google Scholar] [CrossRef]
- Finotto, S.; Krieglstein, K.; Schober, A.; Deimling, F.; Lindner, K.; Brühl, B.; Beier, K.; Metz, J.; Garcia-Arraras, J.E.; Roig-Lopez, J.L.; et al. Analysis of mice carrying targeted mutations of the glucocorticoid receptor gene argues against an essential role of glucocorticoid signalling for generating adrenal chromaffin cells. Development 1999, 126, 2935–2944. [Google Scholar] [CrossRef]
- Eisenhofer, G.; Rundquist, B.; Aneman, A.; Friberg, P.; Dakak, N.; Kopin, I.J.; Jacobs, M.C.; Lenders, J.W. Regional release and removal of catecholamines and extraneuronal metabolism to metanephrines. J. Clin. Endocrinol. Metab. 1995, 80, 3009–3017. [Google Scholar] [CrossRef] [PubMed]
- Merke, D.P.; Bornstein, S.R. Congenital adrenal hyperplasia. Lancet 2005, 365, 2125–2136. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.; Tanawattanacharoen, V.K.; Seagroves, A.; Liang, M.C.; Koppin, C.M.; Ross, H.M.; Bachega, T.; Geffner, M.E.; Serrano-Gonzalez, M.; Bhullar, G.; et al. Low Adrenomedullary Function Predicts Acute Illness in Infants With Classical Congenital Adrenal Hyperplasia. J. Clin. Endocrinol. Metab. 2022, 107, e264–e271. [Google Scholar] [CrossRef] [PubMed]
- Green-Golan, L.; Yates, C.; Drinkard, B.; VanRyzin, C.; Eisenhofer, G.; Weise, M.; Merke, D.P. Patients with classic congenital adrenal hyperplasia have decreased epinephrine reserve and defective glycemic control during prolonged moderate-intensity exercise. J. Clin. Endocrinol. Metab. 2007, 92, 3019–3024. [Google Scholar] [CrossRef]
- Morita, S.; Otsuki, M.; Izumi, M.; Asanuma, N.; Izumoto, S.; Saitoh, Y.; Yoshimine, T.; Kasayama, S. Reduced epinephrine reserve in response to insulin-induced hypoglycemia in patients with pituitary adenoma. Eur. J. Endocrinol. 2007, 157, 265–270. [Google Scholar] [CrossRef]
- Guaraldi, F.; Karamouzis, I.; Berardelli, R.; D’Angelo, V.; Rampino, A.; Zichi, C.; Ghigo, E.; Giordano, R. Secondary Adrenal Insufficiency: Where Is It Hidden and What Does It Look Like? Front. Horm. Res. 2016, 46, 159–170. [Google Scholar] [CrossRef]
- Hahner, S.; Ross, R.J.; Arlt, W.; Bancos, I.; Burger-Stritt, S.; Torpy, D.J.; Husebye, E.S.; Quinkler, M. Adrenal insufficiency. Nat. Rev. Dis. Prim. 2021, 7, 2152–2167. [Google Scholar] [CrossRef]
- Zuckerman-Levin, N.; Tiosano, D.; Eisenhofer, G.; Bornstein, S.; Hochberg, Z. The importance of adrenocortical glucocorticoids for adrenomedullary and physiological response to stress: A study in isolated glucocorticoid deficiency. J. Clin. Endocrinol. Metab. 2001, 86, 5920–5924. [Google Scholar] [CrossRef]
- Erichsen, M.M.; Løvås, K.; Skinningsrud, B.; Wolff, A.B.; Undlien, D.E.; Svartberg, J.; Fougner, K.J.; Berg, T.J.; Bollerslev, J.; Mella, B.; et al. Clinical, immunological, and genetic features of autoimmune primary adrenal insufficiency: Observations from a Norwegian registry. J. Clin. Endocrinol. Metab. 2009, 94, 4882–4890. [Google Scholar] [CrossRef]
- Winqvist, O.; Söderbergh, A.; Kämpe, O. The autoimmune basis of adrenocortical destruction in Addison’s disease. Mol. Med. Today 1996, 2, 282–289. [Google Scholar] [CrossRef]
- Bensing, S.; Hulting, A.L.; Husebye, E.S.; Kampe, O.; Lovas, K. Management of endocrine disease: Epidemiology, quality of life and complications of primary adrenal insufficiency: A review. Eur. J. Endocrinol. 2016, 175, R107–R116. [Google Scholar] [CrossRef]
- Bornstein, S.R.; Breidert, M.; Ehrhart-Bornstein, M.; Kloos, B.; Scherbaum, W.A. Plasma catecholamines in patients with Addison’s disease. Clin. Endocrinol. 1995, 42, 215–218. [Google Scholar] [CrossRef]
- Simunkova, K.; Jovanovic, N.; Rostrup, E.; Methlie, P.; Oksnes, M.; Nilsen, R.M.; Henno, H.; Tilseth, M.; Godang, K.; Kovac, A.; et al. Effect of a pre-exercise hydrocortisone dose on short-term physical performance in female patients with primary adrenal failure. Eur. J. Endocrinol. 2016, 174, 97–105. [Google Scholar] [CrossRef]
- Sævik, Å.B.; Åkerman, A.K.; Methlie, P.; Quinkler, M.; Jørgensen, A.P.; Höybye, C.; Debowska, A.J.; Nedrebø, B.G.; Dahle, A.L.; Carlsen, S.; et al. Residual Corticosteroid Production in Autoimmune Addison Disease. J. Clin. Endocrinol. Metab. 2020, 105, 2430–2441. [Google Scholar] [CrossRef]
- Vulto, A.; Bergthorsdottir, R.; van Faassen, M.; Kema, I.P.; Johannsson, G.; van Beek, A.P. Residual endogenous corticosteroid production in patients with adrenal insufficiency. Clin. Endocrinol. 2019, 91, 383–390. [Google Scholar] [CrossRef]
- Napier, C.; Allinson, K.; Gan, E.H.; Mitchell, A.L.; Gilligan, L.C.; Taylor, A.E.; Arlt, W.; Pearce, S.H.S. Natural History of Adrenal Steroidogenesis in Autoimmune Addison’s Disease Following Diagnosis and Treatment. J. Clin. Endocrinol. Metab. 2020, 105, 2322–2330. [Google Scholar] [CrossRef]
- Simonyi, A.; Fekete, M.I.; Kenessey, A.; Páldi-Haris, P.; Gráf, L. Prolonged ACTH treatment increases trypsin-like and phenylethanolamine-N-methyltransferase (PNMT) activity in the adrenals. Eur. J. Pharmacol. 1984, 106, 465–466. [Google Scholar] [CrossRef]
- Eisenhofer, G.; Peitzsch, M.; Kaden, D.; Langton, K.; Mangelis, A.; Pamporaki, C.; Masjkur, J.; Geroula, A.; Kurlbaum, M.; Deutschbein, T.; et al. Reference intervals for LC-MS/MS measurements of plasma free, urinary free and urinary acid-hydrolyzed deconjugated normetanephrine, metanephrine and methoxytyramine. Clin. Chim. Acta. 2019, 490, 46–54. [Google Scholar] [CrossRef]
- Yu, S.; Yin, Y.; Li, Q.; Yu, J.; Liu, W.; Wang, D.; Cheng, Q.; Xie, S.; Cheng, X.; Qiu, L. Validation of an improved liquid chromatography tandem mass spectrometry method for rapid and simultaneous analysis of plasma catecholamine and their metabolites. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2019, 1129, 121805. [Google Scholar] [CrossRef]
- Wurtman, R.J. Stress and the adrenocortical control of epinephrine synthesis. Metabolism 2002, 51 (Suppl. S1), 11–14. [Google Scholar] [CrossRef]
- Merke, D.P.; Chrousos, G.P.; Eisenhofer, G.; Weise, M.; Keil, M.F.; Rogol, A.D.; Van Wyk, J.J.; Bornstein, S.R. Adrenomedullary dysplasia and hypofunction in patients with classic 21-hydroxylase deficiency. N. Engl. J. Med. 2000, 343, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Charmandari, E.; Eisenhofer, G.; Mehlinger, S.L.; Carlson, A.; Wesley, R.; Keil, M.F.; Chrousos, G.P.; New, M.I.; Merke, D.P. Adrenomedullary function may predict phenotype and genotype in classic 21-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 2002, 87, 3031–3037. [Google Scholar] [CrossRef] [PubMed]
- Riepe, F.G.; Krone, N.; Krüger, S.N.; Sweep, F.C.; Lenders, J.W.; Dötsch, J.; Mönig, H.; Sippell, W.G.; Partsch, C.J. Absence of exercise-induced leptin suppression associated with insufficient epinephrine reserve in patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Exp. Clin. Endocrinol. Diabetes. 2006, 114, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Osinga, T.E.; van den Eijnden, M.H.; Kema, I.P.; Kerstens, M.N.; Dullaart, R.P.; de Jong, W.H.; Sluiter, W.J.; Links, T.P.; van der Horst-Schrivers, A.N. Unilateral and bilateral adrenalectomy for pheochromocytoma requires adjustment of urinary and plasma metanephrine reference ranges. J. Clin. Endocrinol. Metab. 2013, 98, 1076–1083. [Google Scholar] [CrossRef]
| Characteristic | without RAF | with RAF | p-Value | |
|---|---|---|---|---|
| N | 20 | 50 | ||
| Age (year), median (IQR) | 49 (32, 55) | 50 (36, 59) | 0.62 | |
| Female | 13 (65%) | 23 (46%) | 0.15 | |
| BMI (kg/m2), mean (SD) | 24 (4.2) | 26 (4.3) | 0.20 | |
| Adrenal crisis ever | no | 5 (25%) | 18 (36%) | 0.38 |
| yes | 15 (75%) | 32 (64%) | ||
| Systolic BP (mmHg), median (IQR) | 110 (101,120) | 121 (116,132) | 0.01 | |
| Diastolic BP (mmHg), median (IQR) | 71 (69, 80) | 78 (70, 85) | 0.14 | |
| PRC. (mIE/L) median (IQR) | 71 (17, 192) | 91 (27, 206) | 0.25 | |
| S-DHEAS (nmol/L) median (IQR) | <0.62 * (0, 192) | 428 (160, 628) | <0.001 | |
| All Patients | Cortisol | Without RAF *** | Cortisol | With RAF | Cortisol | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | Median | Min-Max | N | Median | Min-Max | N | Median | Min-Max | |
| Time 0 min | |||||||||
| MN < 0.1 | 47 | 16 | <0.91–397 | 17 | <0.91 | <0.91–14 | 30 | 47 | <0.91–397 |
| MN ≥ 0.1 | 23 | 70 | 1–294 | 3 | 1.8 | 1–10 | 20 | 104 | 16–294 |
| Time 30 min | |||||||||
| MN < 0.1 | 52 | 25 | <0.91–399 | 17 | <0.91 | <0.91–14 | 35 | 67 | 8–399 |
| MN ≥ 0.1 | 17 | 63 | 1–315 | 3 | 8.5 | 1–11 | 14 | 126 | 24–315 |
| Time 60 min | |||||||||
| MN < 0.1 | 51 | 18 | <0.91–312 | 19 | <0.91 | <0.91–2 | 32 | 47 | 5–312 |
| MN ≥ 0.1 | 18 | 151 | 1–418 | 1 | 1 | 1 | 17 | 178 | 24–418 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Åkerman, A.-K.; Sævik, Å.B.; Thorsby, P.M.; Methlie, P.; Quinkler, M.; Jørgensen, A.P.; Höybye, C.; Debowska, A.J.; Nedrebø, B.G.; Dahle, A.L.; et al. Plasma-Metanephrines in Patients with Autoimmune Addison’s Disease with and without Residual Adrenocortical Function. J. Clin. Med. 2023, 12, 3602. https://doi.org/10.3390/jcm12103602
Åkerman A-K, Sævik ÅB, Thorsby PM, Methlie P, Quinkler M, Jørgensen AP, Höybye C, Debowska AJ, Nedrebø BG, Dahle AL, et al. Plasma-Metanephrines in Patients with Autoimmune Addison’s Disease with and without Residual Adrenocortical Function. Journal of Clinical Medicine. 2023; 12(10):3602. https://doi.org/10.3390/jcm12103602
Chicago/Turabian StyleÅkerman, Anna-Karin, Åse Bjorvatn Sævik, Per Medbøe Thorsby, Paal Methlie, Marcus Quinkler, Anders Palmstrøm Jørgensen, Charlotte Höybye, Aleksandra J. Debowska, Bjørn Gunnar Nedrebø, Anne Lise Dahle, and et al. 2023. "Plasma-Metanephrines in Patients with Autoimmune Addison’s Disease with and without Residual Adrenocortical Function" Journal of Clinical Medicine 12, no. 10: 3602. https://doi.org/10.3390/jcm12103602
APA StyleÅkerman, A.-K., Sævik, Å. B., Thorsby, P. M., Methlie, P., Quinkler, M., Jørgensen, A. P., Höybye, C., Debowska, A. J., Nedrebø, B. G., Dahle, A. L., Carlsen, S., Tomkowicz, A., Sollid, S. T., Nermoen, I., Grønning, K., Dahlqvist, P., Grimnes, G., Skov, J., Finnes, T., ... Bensing, S. (2023). Plasma-Metanephrines in Patients with Autoimmune Addison’s Disease with and without Residual Adrenocortical Function. Journal of Clinical Medicine, 12(10), 3602. https://doi.org/10.3390/jcm12103602





