Prematurity and Long-Term Respiratory Morbidity—What Is the Critical Gestational Age Threshold?
Abstract
:1. Introduction
2. Methods
Statistical Analysis
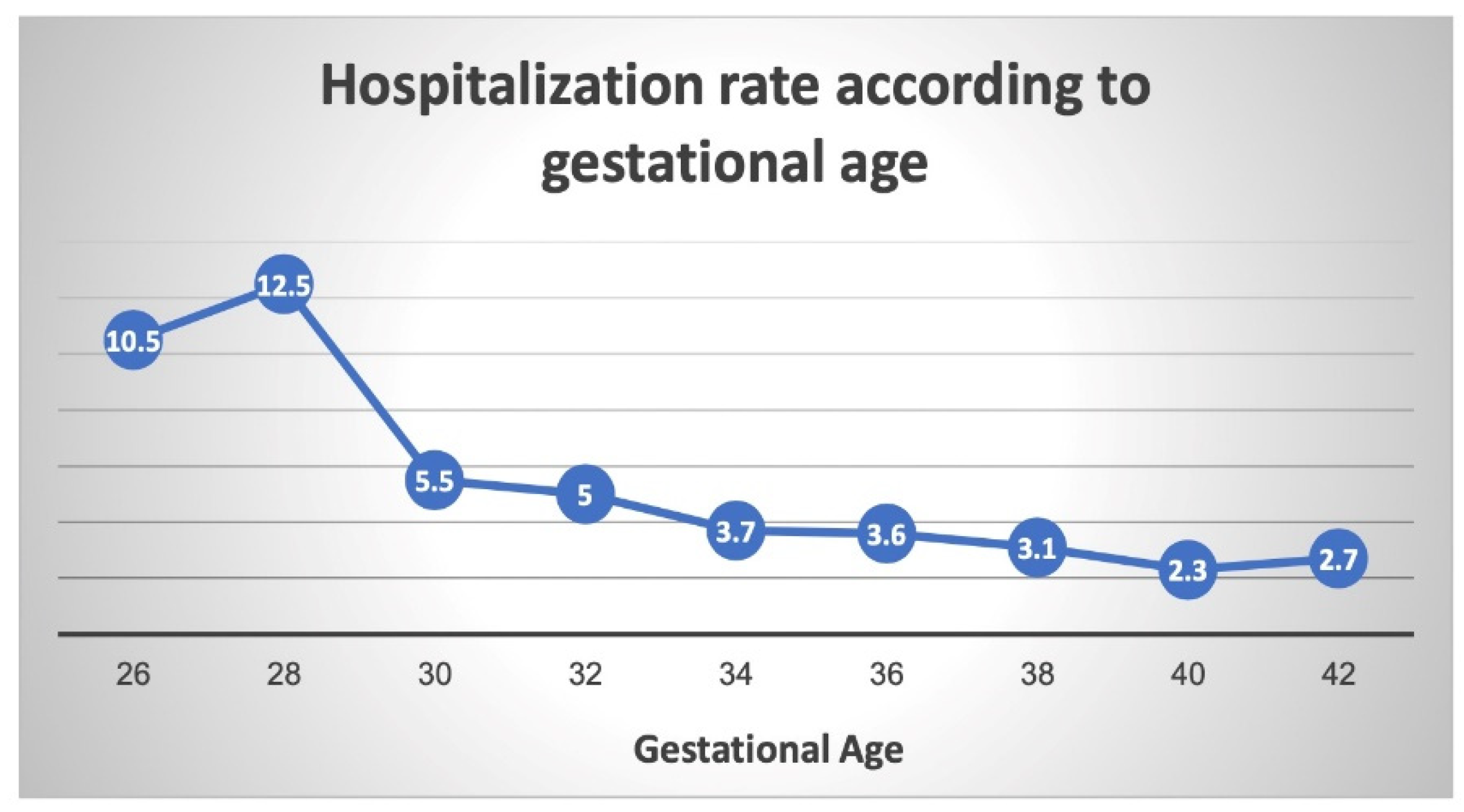
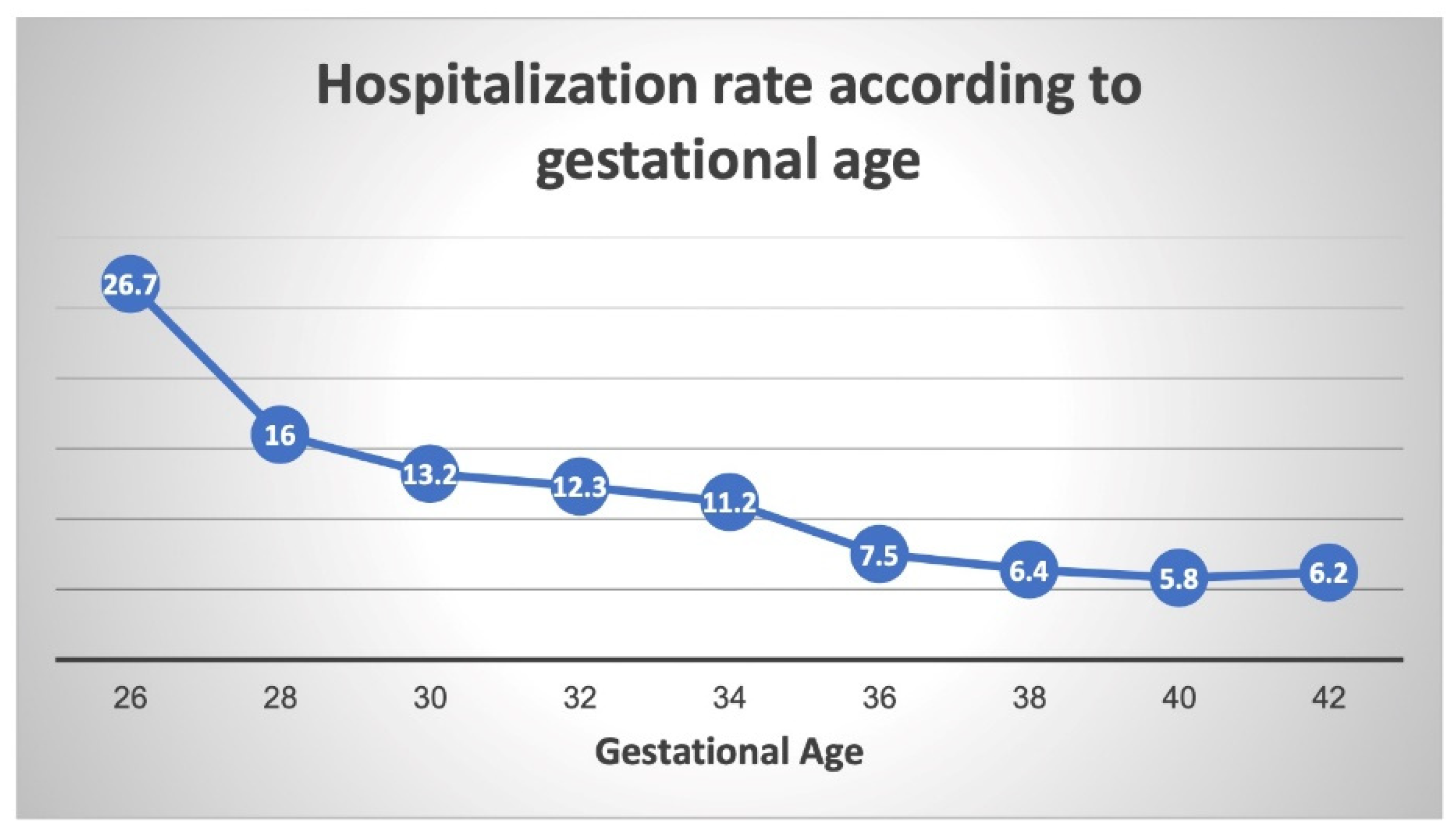
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Blencowe, H.; Cousens, S.; Chou, D.; Oestergaard, M.; Say, L.; Moller, A.-B.; Kinney, M.; Lawn, J.; The Born Too Soon Preterm Birth Action Group. Born Too Soon: The global epidemiology of 15 million preterm births. Reprod. Health 2013, 10 (Suppl. 1), S2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohana, O.; Wainstock, T.; Sheiner, E.; Leibson, T.; Pariente, G. Long-term digestive hospitalizations of premature infants (besides necrotizing enterocolitis): Is there a critical threshold? Arch. Gynecol. Obstet. 2021, 304, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chawanpaiboon, S.; Vogel, J.P.; Moller, A.-B.; Lumbiganon, P.; Petzold, M.; Hogan, D.; Landoulsi, S.; Jampathong, N.; Kongwattanakul, K.; Laopaiboon, M.; et al. Global, regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. Lancet Glob. Health 2019, 7, e37–e46. [Google Scholar] [CrossRef] [Green Version]
- Blencowe, H.; Cousens, S.; Oestergaard, M.Z.; Chou, D.; Moller, A.-B.; Narwal, R.; Adler, A.; Garcia, C.V.; Rohde, S.; Say, L.; et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet 2012, 379, 2162–2172. [Google Scholar] [CrossRef] [Green Version]
- Ely, D.M.; Driscoll, A.K. Infant Mortality in the United States, 2017: Data from the Period Linked Birth/Infant Death File. Natl. Vital. Stat. Rep. 2019, 68, 1–20. [Google Scholar] [PubMed]
- Tyson, J.E.; Parikh, N.; Langer, J.; Green, C.; Higgins, R.D. Intensive Care for Extreme Prematurity—Moving beyond Gestational Age. N. Engl. J. Med. 2008, 358, 1672–1681. [Google Scholar] [CrossRef] [Green Version]
- Helenius, K.; Sjörs, G.; Shah, P.S.; Modi, N.; Reichman, B.; Morisaki, N.; Kusuda, S.; Lui, K.; Darlow, B.A.; Bassler, D.; et al. Survival in Very Preterm Infants: An International Comparison of 10 National Neonatal Networks. Pediatrics 2017, 140, e20171264. [Google Scholar] [CrossRef] [Green Version]
- Alleman, B.W.; Bell, E.F.; Li, L.; Dagle, J.M.; Smith, P.B.; Ambalavanan, N.; Laughon, M.M.; Stoll, B.J.; Goldberg, R.N.; Carlo, W.A.; et al. Individual and Center-Level Factors Affecting Mortality Among Extremely Low Birth Weight Infants. Pediatrics 2013, 132, e175–e184. [Google Scholar] [CrossRef] [Green Version]
- Corchia, C.; Ferrante, P.; Da Frè, M.; Di Lallo, D.; Gagliardi, L.; Carnielli, V.; Miniaci, S.; Piga, S.; Macagno, F.; Cuttini, M. Cause-Specific Mortality of Very Preterm Infants and Antenatal Events. J. Pediatr. 2013, 162, 1125–1132.e4. [Google Scholar] [CrossRef]
- Chandrasekharan, P.; Lakshminrusimha, S.; Chowdhury, D.; Van Meurs, K.; Keszler, M.; Kirpalani, H.; Das, A.; Walsh, M.C.; McGowan, E.C.; Higgins, R.D.; et al. Early Hypoxic Respiratory Failure in Extreme Prematurity: Mortality and Neurodevelopmental Outcomes. Pediatrics 2020, 146, e20193318. [Google Scholar] [CrossRef]
- Kajekar, R. Environmental factors and developmental outcomes in the lung. Pharmacol. Ther. 2007, 114, 129–145. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Shankaran, S.; Laptook, A.R.; Walsh, M.C.; Hale, E.C.; Newman, N.S.; Schibler, K.; Carlo, W.A.; et al. Neonatal Outcomes of Extremely Preterm Infants from the NICHD Neonatal Research Network. Pediatrics 2010, 126, 443–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coathup, V.; Boyle, E.; Carson, C.; Johnson, S.; Kurinzcuk, J.J.; Macfarlane, A.; Petrou, S.; Rivero-Arias, O.; Quigley, M.A. Gestational age and hospital admissions during childhood: Population based, record linkage study in England (TIGAR study). BMJ 2020, 371, m4075. [Google Scholar] [CrossRef] [PubMed]
- Kuint, J.; Lerner-Geva, L.; Chodick, G.; Boyko, V.; Shalev, V.; Reichman, B.; Heymann, E.; Zangen, S.; Smolkin, T.; Mimouni, F.; et al. Rehospitalization Through Childhood and Adolescence: Association with Neonatal Morbidities in Infants of Very Low Birth Weight. J. Pediatr. 2017, 188, 135–141.e2. [Google Scholar] [CrossRef]
- Bolton, C.E.; Stocks, J.; Hennessy, E.; Cockcroft, J.R.; Fawke, J.; Lum, S.; McEniery, C.M.; Wilkinson, I.B.; Marlow, N. The EPICure Study: Association between Hemodynamics and Lung Function at 11 Years after Extremely Preterm Birth. J. Pediatr. 2012, 161, 595–601.e2. [Google Scholar] [CrossRef] [Green Version]
- Choukroun, M.-L.; Feghali, H.; Vautrat, S.; Marquant, F.; Nacka, F.; Leroy, V.; Demarquez, J.-L.; Fayon, M.J. Pulmonary outcome and its correlates in school-aged children born with a gestational age ≤ 32 weeks. Respir. Med. 2013, 107, 1966–1976. [Google Scholar] [CrossRef] [Green Version]
- Thunqvist, P.; Tufvesson, E.; Bjermer, L.; Winberg, A.; Fellman, V.; Domellöf, M.; Melén, E.; Norman, M.; Hallberg, J. Lung function after extremely preterm birth-A population-based cohort study (EXPRESS). Pediatr. Pulmonol. 2018, 53, 64–72. [Google Scholar] [CrossRef] [Green Version]
- Hafström, M.; Källén, K.; Serenius, F.; Maršál, K.; Rehn, E.; Drake, H.; Ådén, U.; Farooqi, A.; Thorngren-Jerneck, K.; Strömberg, B. Cerebral Palsy in Extremely Preterm Infants. Pediatrics 2018, 141, e20171433. [Google Scholar] [CrossRef] [Green Version]
- Hirvonen, M.; Ojala, R.; Korhonen, P.; Haataja, P.; Eriksson, K.; Gissler, M.; Luukkaala, T.; Tammela, O. Cerebral Palsy Among Children Born Moderately and Late Preterm. Pediatrics 2014, 134, e1584–e1593. [Google Scholar] [CrossRef] [Green Version]
- Stocks, J.; Hislop, A.; Sonnappa, S. Early lung development: Lifelong effect on respiratory health and disease. Lancet Respir. Med. 2013, 1, 728–742. [Google Scholar] [CrossRef]
- Harding, R.; Maritz, G. Maternal and fetal origins of lung disease in adulthood. Semin. Fetal Neonatal Med. 2012, 17, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Fawke, J.; Lum, S.; Kirkby, J.; Hennessy, E.; Marlow, N.; Rowell, V.; Thomas, S.; Stocks, J. Lung function and respiratory symptoms at 11 years in children born extremely preterm: The EPICure study. Am. J. Respir. Crit. Care Med. 2010, 182, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Kotecha, S.J.; Watkins, W.J.; Paranjothy, S.; Dunstan, F.D.; Henderson, A.J.; Kotecha, S. Effect of late preterm birth on longitudinal lung spirometry in school age children and adolescents. Thorax 2011, 67, 54–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotecha, S.J.; Dunstan, F.D.; Kotecha, S. Long term respiratory outcomes of late preterm-born infants. Semin. Fetal Neonatal Med. 2012, 17, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Copper, R.L.; Goldenberg, R.L.; Creasy, R.K.; DuBard, M.B.; Davis, R.O.; Entman, S.S.; Iams, J.D.; Cliver, S.P. A multicenter study of preterm birth weight and gestational age—Specific neonatal mortality. Am. J. Obstet. Gynecol. 1993, 168, 78–84. [Google Scholar] [CrossRef]
- Schittny, J.C. Development of the lung. Cell Tissue Res. 2017, 367, 427–444. [Google Scholar] [CrossRef] [Green Version]
- Laughon, M.; Allred, E.N.; Bose, C.; O’Shea, T.M.; Van Marter, L.J.; Ehrenkranz, R.A.; Leviton, A.; ELGAN study investigators. Patterns of Respiratory Disease During the First 2 Postnatal Weeks in Extremely Premature Infants. Pediatrics 2009, 123, 1124–1131. [Google Scholar] [CrossRef] [Green Version]
- Frank, L.; Sosenko, I.R. Development of lung antioxidant enzyme system in late gestation: Possible implications for the prematurely born infant. J. Pediatr. 1987, 110, 9–14. [Google Scholar] [CrossRef]
- Fraser, J.; Walls, M.; McGuire, W. Respiratory complications of preterm birth. BMJ 2004, 329, 962–965. [Google Scholar] [CrossRef] [Green Version]
- Finer, N.; Leone, T. Oxygen saturation monitoring for the preterm infant: The evidence basis for current practice. Pediatr. Res. 2009, 65, 375–380. [Google Scholar] [CrossRef] [Green Version]
- Altman, M.; Vanpee, M.; Cnattingius, S.; Norman, M. Neonatal Morbidity in Moderately Preterm Infants: A Swedish National Population-Based Study. J. Pediatr. 2011, 158, 239–244.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yee, M.; White, R.J.; Awad, H.A.; Bates, W.A.; McGrath-Morrow, S.A.; O’Reilly, M.A. Neonatal Hyperoxia Causes Pulmonary Vascular Disease and Shortens Life Span in Aging Mice. Am. J. Pathol. 2011, 178, 2601–2610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunig, A.M.; Balasubramaniam, V.; Markham, N.E.; Morgan, D.; Montgomery, G.; Grover, T.R.; Abman, S.H. Recombinant human VEGF treatment enhances alveolarization after hyperoxic lung injury in neonatal rats. Am. J. Physiol. Cell. Mol. Physiol. 2005, 289, L529–L535. [Google Scholar] [CrossRef] [PubMed]
- Georgeson, G.D.; Szőny, B.J.; Streitman, K.; Varga, I.S.; Kovács, A.; Kovács, L.; László, A. Antioxidant enzyme activities are decreased in preterm infants and in neonates born via caesarean section. Eur. J. Obstet. Gynecol. Reprod. Biol. 2002, 103, 136–139. [Google Scholar] [CrossRef]
- Hernandez, L.A.; Peevy, K.J.; Moise, A.A.; Parker, J.C. Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. J. Appl. Physiol. 1989, 66, 2364–2368. [Google Scholar] [CrossRef] [PubMed]
- Carlton, D.P.; Cummings, J.J.; Scheerer, R.G.; Poulain, F.R.; Bland, R.D. Lung overexpansion increases pulmonary microvascular protein permeability in young lambs. J. Appl. Physiol. 1990, 69, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Björklund, L.J.; Ingimarsson, J.; Curstedt, T.; John, J.; Robertson, B.; Werner, O.; Vilstrup, C.T.; Bj, L.J. Manual Ventilation with a Few Large Breaths at Birth Compromises the Therapeutic Effect of Subsequent Surfactant Replacement in Immature Lambs. Pediatr. Res. 1997, 42, 348–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laughon, M.M.; Langer, J.C.; Bose, C.L.; Smith, P.B.; Ambalavanan, N.; Kennedy, K.A.; Stoll, B.J.; Buchter, S.; Laptook, A.R.; Ehrenkranz, R.A.; et al. Prediction of Bronchopulmonary Dysplasia by Postnatal Age in Extremely Premature Infants. Am. J. Respir. Crit. Care Med. 2011, 183, 1715–1722. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, C.; Wheeler, K.I.; McCallion, N.; Morley, C.J.; Davis, P.G. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst. Rev. 2017, 10, CD003666. [Google Scholar] [CrossRef]
- Speer, C.P.; Silverman, M. Issues relating to children born prematurely. Eur. Respir. J. Suppl. 1998, 27, 13s–16s. [Google Scholar]
- Been, J.V.; Lugtenberg, M.J.; Smets, E.; Van Schayck, C.P.; Kramer, B.W.; Mommers, M.; Sheikh, A. Preterm Birth and Childhood Wheezing Disorders: A Systematic Review and Meta-Analysis. PLoS Med. 2014, 11, e1001596. [Google Scholar] [CrossRef] [PubMed]
- Leps, C.; Carson, C.; QLeps, C.; Carson, C.; Quigley, M.A. Gestational age at birth and wheezing trajectories at 3–11 years. Arch. Dis. Child. 2018, 103, 1138–1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaakkola, M.S.; Ahmed, P.; Ieromnimon, A.; Goepfert, P.; Laiou, E.; Quansah, R. Preterm delivery and asthma: A systematic review and meta-analysis. J. Allergy Clin. Immunol. 2006, 118, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Källén, B.; Finnström, O.; Nygren, K.G.; Otterblad Olausson, P. Association between preterm birth and intrauterine growth retardation and child asthma. Eur. Respir. J. 2013, 41, 671–676. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.J.; van Asperen, P.P.; McKay, K.O.; Selvadurai, H.; Fitzgerald, D.A. Reduced Exercise Capacity in Children Born Very Preterm. Pediatrics 2008, 122, e287–e293. [Google Scholar] [CrossRef]
- Davidesko, S.; Wainstock, T.; Sheiner, E.; Pariente, G. Long-Term Infectious Morbidity of Premature Infants: Is There a Critical Threshold? J. Clin. Med. 2020, 9, 3008. [Google Scholar] [CrossRef]
- Kallapur, S.G.; Ikegami, M. Physiological consequences of intrauterine insults. Paediatr. Respir. Rev. 2006, 7, 110–116. [Google Scholar] [CrossRef]
- Baumfeld, Y.; Walfisch, A.; Wainstock, T.; Segal, I.; Sergienko, R.; Landau, D.; Sheiner, E. Elective cesarean delivery at term and the long-term risk for respiratory morbidity of the offspring. Eur. J. Nucl. Med. Mol. Imaging 2018, 177, 1653–1659. [Google Scholar] [CrossRef]
- McGoldrick, E.; Stewart, F.; Parker, R.; Dalziel, S.R. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst. Rev. 2020, 2021, CD004454. [Google Scholar] [CrossRef]
- Maritz, G.S.; Morley, C.; Harding, R. Early developmental origins of impaired lung structure and function. Early Hum. Dev. 2005, 81, 763–771. [Google Scholar] [CrossRef]


| Maternal Characteristics | Extremely Preterm (24.0–27.6) N = 118 | Very Preterm (28.0–31.6) N = 776 | Moderate to Late Preterm (32.0–36.6) N = 13,308 | Term Delivery (≥37.0) N = 206,361 | p Value a |
|---|---|---|---|---|---|
| Maternal age (mean ± SD, years) | 28.4 ± 6.3 | 28.3 ± 6.3 | 28.3 ± 6.2 | 28.2 ± 5.7 | <0.001 |
| Diabetes mellitus b (%) | 0.0 | 6.2 | 8.2 | 5.3 | <0.001 |
| Hypertensive disorders c (%) | 8.5 | 19.1 | 12.9 | 4.7 | <0.001 |
| Induction of labor (%) | 10.2 | 9.3 | 23.1 | 27.6 | <0.001 |
| Intra-amniotic infection (%) | 33.1 | 14.3 | 2.6 | 0.3 | <0.001 |
| Cesarean Delivery (%) | 51.7 | 52.8 | 31.0 | 12.7 | <0.001 |
| Low Apgar at 5 min (<7) (%) | 14.4 | 6.2 | 2.5 | 1.4 | <0.001 |
| Gestational age at delivery (mean ± SD, weeks) | 26.4 ± 0.7 | 30.0 ± 1.0 | 35.2 ± 1.1 | 39.4 ± 1.2 | <0.001 |
| Birthweight (mean ± SD, grams) | 1096 ± 601 | 1644 ± 633 | 2540 ± 495 | 3270 ± 445 | <0.001 |
| SGA d (%) | 3.4 | 1.8 | 3.6 | 4.4 | <0.001 |
| Respiratory Morbidity | Extremely Preterm (24.0–27.6) N = 118 | Very Preterm (28.0–31.6) N = 776 | Moderate to Late Preterm (32.0–36.6) N = 13,308 | Term Delivery (≥37.0) N = 206,361 | p Value a |
|---|---|---|---|---|---|
| Asthma (%) | 3.4 | 5.2 | 3.4 | 2.5 | <0.001 |
| Pleural disease (%) | 0.0 | 0.4 | 0.1 | 0.1 | 0.022 |
| Obstructive sleep apnea (OSA) (%) | 1.7 | 1.3 | 0.9 | 0.7 | 0.002 |
| Other * (%) | 8.5 | 6.6 | 3.0 | 1.9 | <0.001 |
| Total respiratory hospitalizations (%) | 12.7 | 11.7 | 7.0 | 4.7 | <0.001 |
| Gestational Age | Adjusted Hazard Ratio (aHR) * | Confidence Interval (95%) | p Value |
|---|---|---|---|
| Term delivery (reference) (37–42 weeks) | 1 | - | - |
| Moderate to late preterm (32–37 weeks) | 1.29 | 1.20–1.39 | <0.01 |
| Very preterm (28–32 weeks) | 2.02 | 1.62–2.52 | <0.01 |
| Extremely preterm (24–28 weeks) | 2.04 | 1.21–3.44 | <0.01 |
| Gestational Age | Adjusted Hazard Ratio (aHR) * | Confidence Interval (95%) | p Value |
|---|---|---|---|
| Term delivery (reference) (37–42 weeks) | 1 | - | - |
| Moderate to late preterm (32–37 weeks) | 1.32 | 1.12–1.56 | <0.01 |
| Very preterm (28–32 weeks) | 2.61 | 1.70–4.02 | <0.01 |
| Extremely preterm (24–28 weeks) | 3.33 | 1.50–7.39 | <0.01 |
| Gestational Age | Adjusted Hazard Ratio (aHR) * | Confidence Interval (95%) | p Value |
|---|---|---|---|
| Term delivery (reference) (37–42 weeks) | 1 | - | - |
| Moderate to late preterm (32–37 weeks) | 1.32 | 1.21–1.44 | <0.01 |
| Very preterm (28–32 weeks) | 1.97 | 1.52–2.55 | <0.01 |
| Extremely preterm (24–28 weeks) | 2.04 | 1.01–4.12 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutvirtz, G.; Wainstock, T.; Sheiner, E.; Pariente, G. Prematurity and Long-Term Respiratory Morbidity—What Is the Critical Gestational Age Threshold? J. Clin. Med. 2022, 11, 751. https://doi.org/10.3390/jcm11030751
Gutvirtz G, Wainstock T, Sheiner E, Pariente G. Prematurity and Long-Term Respiratory Morbidity—What Is the Critical Gestational Age Threshold? Journal of Clinical Medicine. 2022; 11(3):751. https://doi.org/10.3390/jcm11030751
Chicago/Turabian StyleGutvirtz, Gil, Tamar Wainstock, Eyal Sheiner, and Gali Pariente. 2022. "Prematurity and Long-Term Respiratory Morbidity—What Is the Critical Gestational Age Threshold?" Journal of Clinical Medicine 11, no. 3: 751. https://doi.org/10.3390/jcm11030751







