Improvement of Post-Operative Quality of Life in Patients 2 Years after Minimally Invasive Surgery for Pain and Deep Infiltrating Endometriosis
Abstract
:1. Introduction
2. Materials and Methods
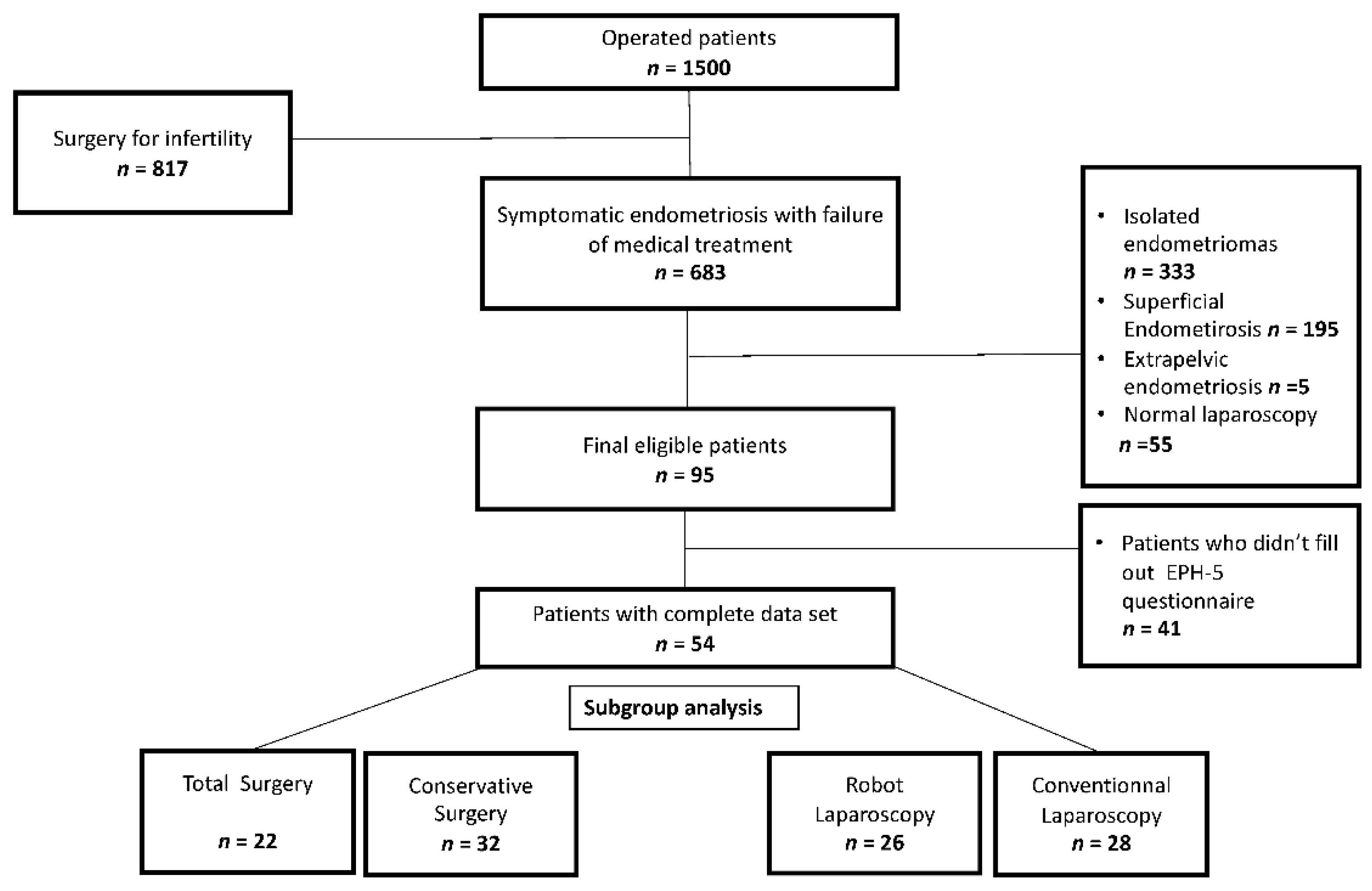
2.1. Patients and Data Collection
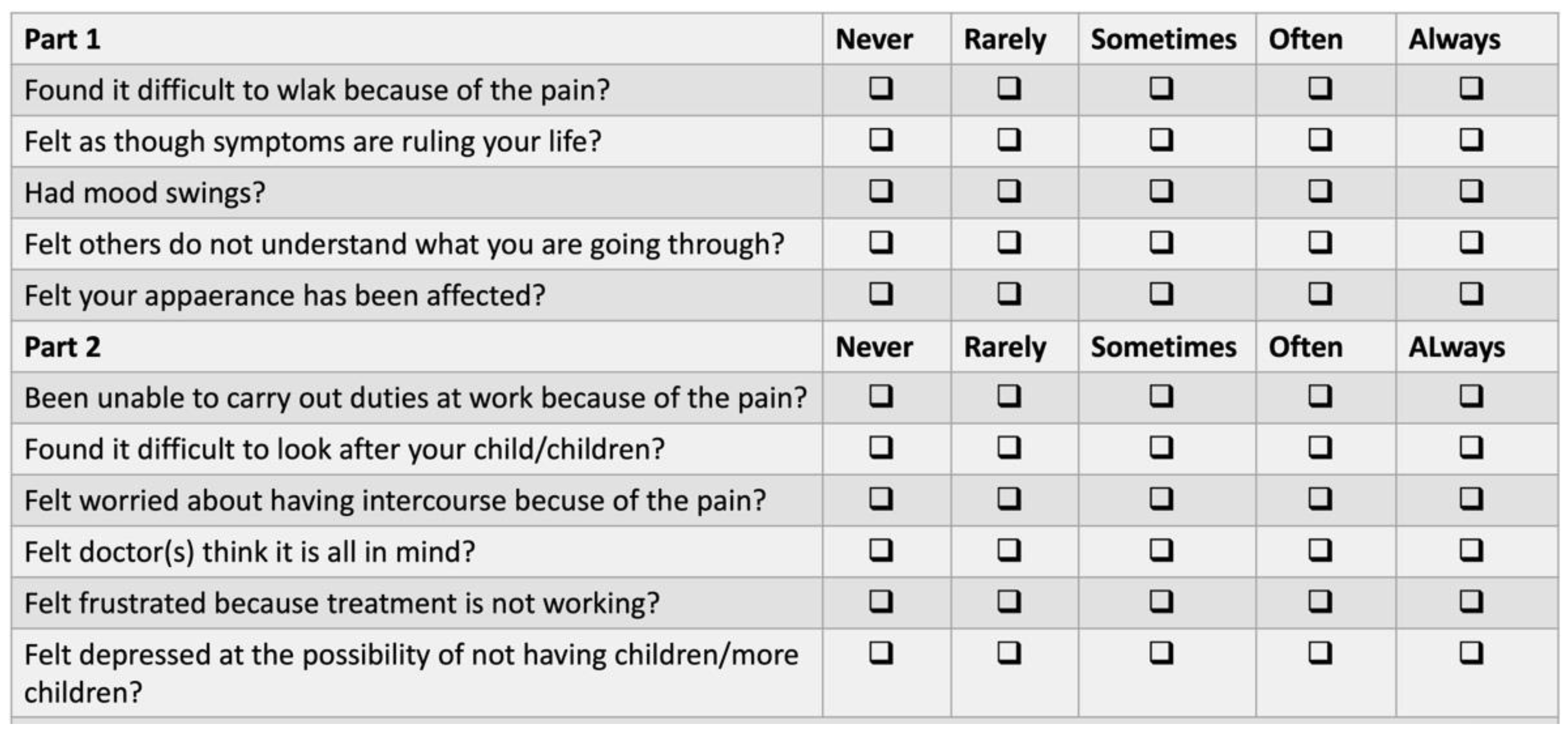
2.2. Quality of Life Evaluation
2.3. Statistics
2.4. Ethics
3. Results
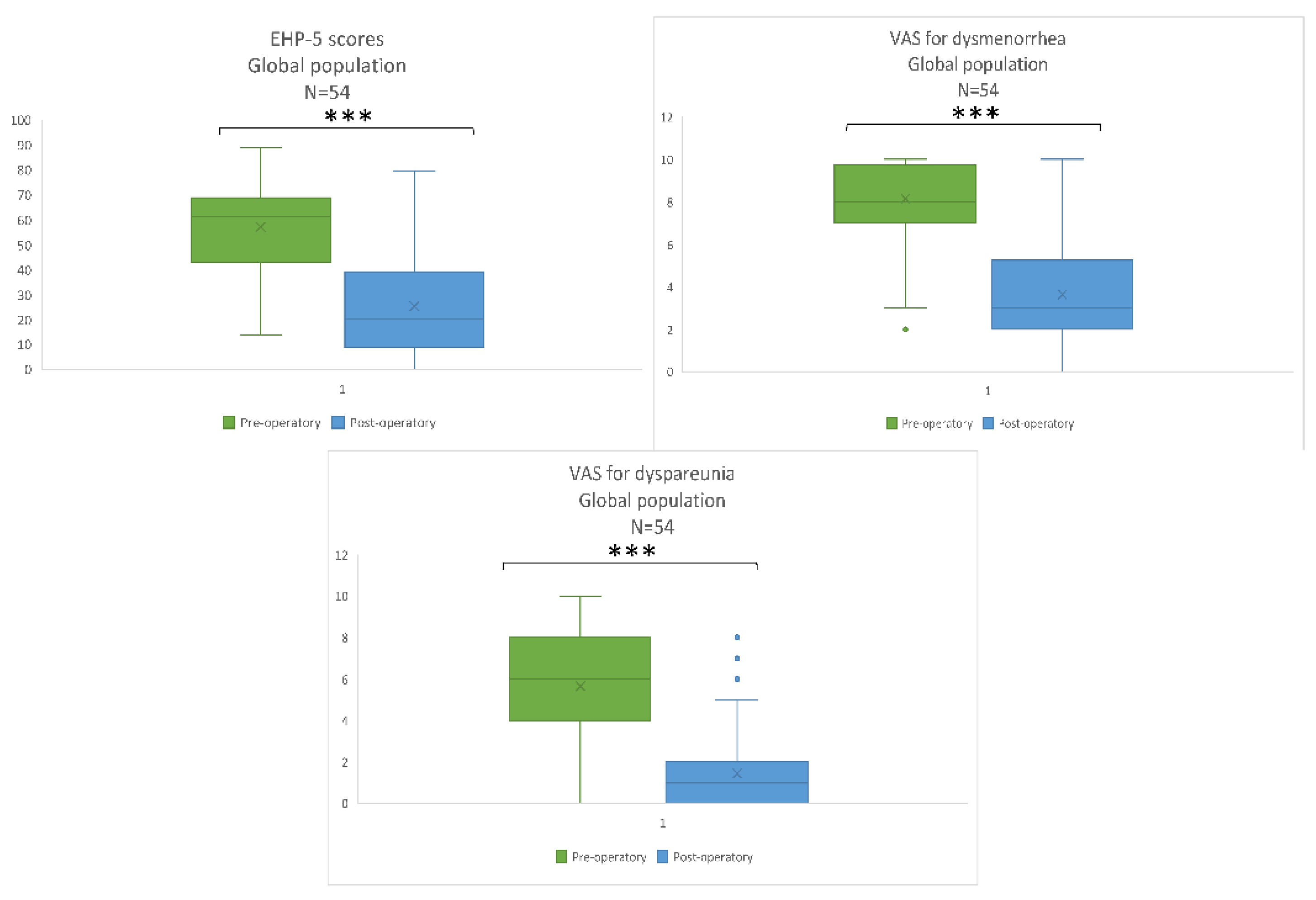
3.1. Global Population Results
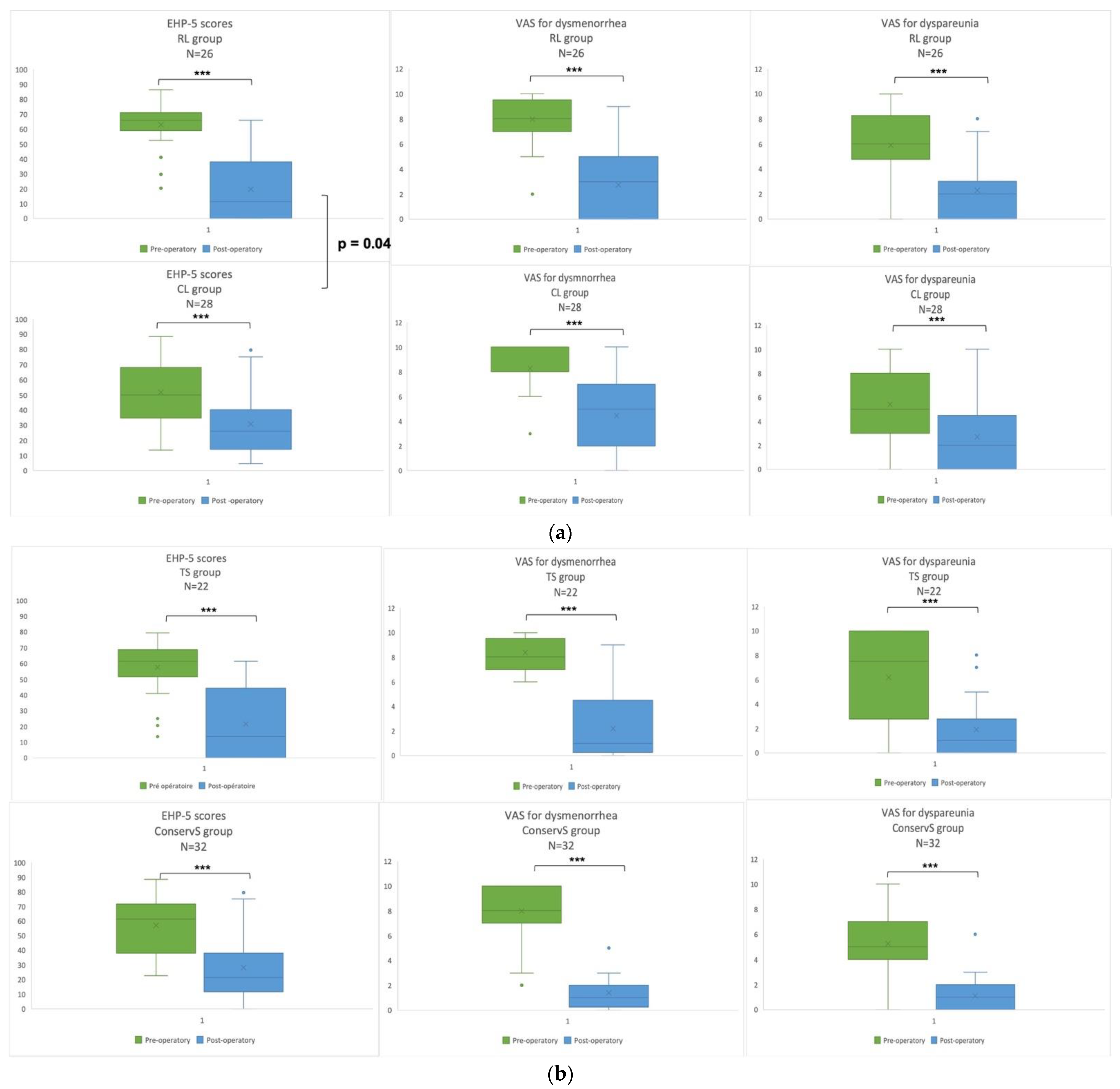
3.2. Subgroup Analysis
4. Discussion
5. Prospects
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- The Members of the Endometriosis Guideline Core Group; Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; et al. ESHRE guideline: Endometriosis. Hum. Reprod. Open 2022, 2022, hoac009. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Donnez, J. Deep endometriosis: Definition, diagnosis, and treatment. Fertil. Steril. 2012, 98, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Della Corte, L.; Di Filippo, C.; Gabrielli, O.; Reppuccia, S.; La Rosa, V.L.; Ragusa, R.; Fichera, M.; Commodari, E.; Bifulco, G.; Giampaolino, P. The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int. J. Environ. Res. Public Health 2020, 17, 4683. [Google Scholar] [CrossRef] [PubMed]
- Dunselman, G.A.J.; Vermeulen, N.; Becker, C.; Calhaz-Jorge, C.; D’Hooghe, T.; De Bie, B.; Heikinheimo, O.; Horne, A.W.; Kiesel, L.; Nap, A.; et al. ESHRE guideline: Management of women with endometriosis. Hum. Reprod. 2014, 29, 400–412. [Google Scholar] [CrossRef] [PubMed]
- Bendifallah, S.; Ballester, M.; Darai, E. Prise en charge chirurgicale des lésions d’endométriose profondes avec atteinte digestive et urinaire. Presse Méd. 2017, 46, 1212–1217. [Google Scholar] [CrossRef]
- Bozdag, G. Recurrence of Endometriosis: Risk Factors, Mechanisms and Biomarkers. Women’s Health 2015, 11, 693–699. [Google Scholar] [CrossRef]
- Yela, D.A.; Vitale, S.G.; Vizotto, M.P.; Benetti-Pinto, C.L. Risk factors for recurrence of deep infiltrating endometriosis after surgical treatment. J. Obstet. Gynaecol. Res. 2021, 47, 2713–2719. [Google Scholar] [CrossRef]
- Bendifallah, S.; Puchar, A.; Vesale, E.; Moawad, G.; Daraï, E.; Roman, H. Surgical Outcomes after Colorectal Surgery for Endometriosis: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2020, 28, 453–466. [Google Scholar] [CrossRef]
- Philip, C.-A.; Froc, E.; Chapron, C.; Hebert, T.; Douvier, S.; Filipuzzi, L.; Descamps, P.; Agostini, A.; Collinet, P.; von Theobald, P.; et al. Surgical Management of Urinary Tract Endometriosis: A 1-year Longitudinal Multicenter Pilot Study at 31 French Hospitals (by the FRIENDS Group). J. Minim. Invasive Gynecol. 2021, 28, 1889–1897.e1. [Google Scholar] [CrossRef]
- Sima, R.-M.; Pleş, L.; Socea, B.; Sklavounos, P.; Negoi, I.; Stănescu, A.-D.; Iordache, I.-I.; Hamoud, B.H.; Radosa, M.P.; Juhasz-Boess, I.; et al. Evaluation of the SF-36 questionnaire for assessment of the quality of life of endometriosis patients undergoing treatment: A systematic review and meta-analysis. Exp. Ther. Med. 2021, 22, 1283. [Google Scholar] [CrossRef]
- Torng, P.-L.; Pan, S.-P.; Hwang, J.-S.; Shih, H.-J.; Chen, C.-L. Learning curve in concurrent application of laparoscopic and robotic-assisted hysterectomy with lymphadenectomy in endometrial cancer. Taiwan. J. Obstet. Gynecol. 2017, 56, 781–787. [Google Scholar] [CrossRef]
- Abo, C.; Roman, H.; Bridoux, V.; Huet, E.; Tuech, J.-J.; Resch, B.; Stochino, E.; Marpeau, L.; Darwish, B. Management of deep infiltrating endometriosis by laparoscopic route with robotic assistance: 3-year experience. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Gala, R.B.; Margulies, R.; Steinberg, A.; Murphy, M.; Lukban, J.; Jeppson, P.; Aschkenazi, S.; Olivera, C.; South, M.; Lowenstein, L.; et al. Systematic Review of Robotic Surgery in Gynecology: Robotic Techniques Compared with Laparoscopy and Laparotomy. J. Minim. Invasive Gynecol. 2014, 21, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Jenkinson, C.; Kennedy, S. Development of the Short Form Endometriosis Health Profile Questionnaire: The EHP-5. Qual. Life Res. 2004, 13, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo Classification of Surgical Complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aubry, G.; Panel, P.; Thiollier, G.; Huchon, C.; Fauconnier, A. Measuring health-related quality of life in women with endometriosis: Comparing the clinimetric properties of the Endometriosis Health Profile-5 (EHP-5) and the EuroQol-5D (EQ-5D). Hum. Reprod. 2017, 32, 1258–1269. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, S.K.; Chapron, C.; Giudice, L.C.; Laufer, M.R.; Leyland, N.; Missmer, S.A.; Singh, S.S.; Taylor, H.S. Clinical diagnosis of endometriosis: A call to action. Am. J. Obstet. Gynecol. 2019, 220, 354.e1–354.e12. [Google Scholar] [CrossRef] [Green Version]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of endometriosis on quality of life and mental health: Pelvic pain makes the difference. J. Psychosom. Obstet. Gynecol. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- Bot-Robin, V.; Rubod, C.; Zini, L.; Collinet, P. Étude de faisabilité du traitement laparoscopique robot-assisté de lésions d’endométriose pelvienne profonde. Gynécologie Obs. Fertil. 2011, 39, 407–411. [Google Scholar] [CrossRef]
- Iavazzo, C.; Gkegkes, I.D. Cost–benefit analysis of robotic surgery in gynaecological oncology. Best Pr. Res. Clin. Obstet. Gynaecol. 2017, 45, 7–18. [Google Scholar] [CrossRef]
- Carbonnel, M.; Moawad, G.N.; Tarazi, M.M.; Revaux, A.; Kennel, T.; Favre-Inhofer, A.; Ayoubi, J.M. Robotic Hysterectomy for Benign Indications: What Have We Learned from a Decade? JSLS J. Soc. Laparoendosc. Surg. 2021, 25, e2020.00091. [Google Scholar] [CrossRef] [PubMed]
- Favre, A.; Huberlant, S.; Carbonnel, M.; Goetgheluck, J.; Revaux, A.; Ayoubi, J.M. Pedagogic Approach in the Surgical Learning: The First Period of “Assistant Surgeon” May Improve the Learning Curve for Laparoscopic Robotic-Assisted Hysterectomy. Front. Surg. 2016, 3, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman, H.; Bubenheim, M.; Huet, E.; Bridoux, V.; Zacharopoulou, C.; Daraï, E.; Collinet, P.; Tuech, J.-J. Conservative surgery versus colorectal resection in deep endometriosis infiltrating the rectum: A randomized trial. Hum. Reprod. 2017, 33, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Ballester, M.; Roman, H. Prise en charge chirurgicale de l’endométriose profonde avec atteinte digestive, RPC Endométriose CNGOF-HAS. Gynécologie Obs. Fertil. Sénologie 2018, 46, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Bolze, P.-A.; Paparel, P.; Golfier, F. Localisations urinaires de l’endométriose. Résultats et modalités techniques de la prise en charge chirurgicale. RPC Endométriose CNGOF-HAS. Gynécol. Obs. Fertil. Sénol. 2018, 46, 301–308. [Google Scholar] [CrossRef]
- Bendifallah, S.; Vesale, E.; Daraï, E.; Thomassin-Naggara, I.; Bazot, M.; Tuech, J.-J.; Abo, C.; Roman, H. Recurrence after Surgery for Colorectal Endometriosis: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2020, 27, 441–451.e2. [Google Scholar] [CrossRef]
| Studied Variables | Global Population n = 54 | CL n = 28 | RL n = 26 | p | ConservS n = 32 | TS n = 22 | p |
|---|---|---|---|---|---|---|---|
| Age (years) Median (min–max) | 35.5 (27.8–43.2) | 34 (27.5–37.5) | 36.5 (29.75–43.5) | 0.04 | 37 (29–39) | 34 (27.75–39) | 0.83 |
| BMI (kg/m2) Median (min–max) | 23 (18.7–27.3) | 23 (21–29) | 23 (20.5–27.5) | 0.27 | 24.5 (21–28.25) | 21.5 (20–26.5) | 0.21 |
| Pre-operative hormonal treatment (%) | 80 (43/54) | 78 (22/28) | 81 (21/26) | 1 | 72 (23/32) | 91% (20/22) | 0.16 |
| Level 3 painkiller (%) | 20.4 (11/54) | 17.9 (5/28) | 26.9 (7/26) | 0.72 | 25 (8/32) | 18.18 (4/22) | 0.20 |
| Prior surgery for endometriosis (%) | 11.1 (6/54) | 14.3 (4/28) | 7.7 (2/26) | 0.25 | 12.5 (4/32) | 9.1 (2/22) | 0.31 |
| Hysterectomy (%) | 18.5 (10/54) | 0 (0/28) | 38.5 (10/26) | <0.001 | 9,4 (3/32) | 31.82 (7/21) | 0.04 |
| Salpingectomy (%) | 11.1 (6/54) | 10.7 (3/28) | 11.5 (3/26) | 0.99 | 15.6 (5/32) | 4.55 (1/22) | 0.38 |
| Ureterolysis (%) | 31.5 (17/54) | 28.6 (8/28) | 34.6 (9/26) | 0.83 | 25 (8/32) | 40.91 (9/22) | 0.36 |
| Adhesiolysis (%) | 50 (27/54) | 64.3 (18/28) | 53.8 (9/26) | 0.43 | 71.9 (23/32) | 40.91 (9/22) | 0.02 |
| USL resection (%) | 51.9 (28/54) | 39.3 (11/28) | 65.4 (17/26) | 0.03 | 21.9 (7/32) | 95.45 (21/22) | <0.001 |
| Bladder node resection (%) | 16.7 (9/54) | 7.1 (5/28) | 7.7 (4/26) | 0.94 | 6.2 (2/32) | 9.09 (2/22) | 0.69 |
| Superficial digestive node resection (%) | 18.5 (10/54) | 25 (7/28) | 26.9 (3/26) | 0.87 | 31.2 (10/32) | 18.18 (0/22) | 0.28 |
| Studied Variables | Global Population n = 54 | CL n = 28 | RL n = 26 | ConservS n = 32 | TS n = 22 | p | |
|---|---|---|---|---|---|---|---|
| Post-operative hormonal treatment (%) | 31.5 | 25 (7/28) | 38 (10/26) | 0.38 | 34.3 (11/32) | 27.2 (6/22) | 0.77 |
| Post-operative use of level 3 pain killer (%) | 30.7 (16/52) | 50 (7/28) | 32.14 (9/28) | 0.55 | 43.75 (14/32) | 22.72 (5/22) | 0.15 |
| Pre-operative complications (%) | 2 (1/53) | 3.7 (1/27) | 0 (0/26) | 0.32 | 3.45 (1/28) | 0 (0/22) | 0.38 |
| Post-operative complications (%) | 5.7 (3/52) | 7.69 (2/26) | 3.85 (1/26) | 0.55 | 6.45 (2/31) | 4.76 (1/21) | 0.8 |
| Blood loss 400 (mL) | 0.02 (1/52) | 0 | 4.17 (1/24) | 0.33 | 3.85 (1/26) | 0 (0/22) | 0.41 |
| Post-operative recurrence rate (%) | 11.1% (6/54) | 17.8 (5/28) | 3.8 (1/26) | 0.19 | 15.6 (5/32) | 4.5 (1/22) | 0.38 |
| Complete surgery (%) | 40.7 | 17.8 (7/28) | 65.38 (15/26) | 0.04 | NA | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Legendri, S.; Carbonnel, M.; Feki, A.; Moawad, G.; Aubry, G.; Vallée, A.; Ayoubi, J.-M. Improvement of Post-Operative Quality of Life in Patients 2 Years after Minimally Invasive Surgery for Pain and Deep Infiltrating Endometriosis. J. Clin. Med. 2022, 11, 6132. https://doi.org/10.3390/jcm11206132
Legendri S, Carbonnel M, Feki A, Moawad G, Aubry G, Vallée A, Ayoubi J-M. Improvement of Post-Operative Quality of Life in Patients 2 Years after Minimally Invasive Surgery for Pain and Deep Infiltrating Endometriosis. Journal of Clinical Medicine. 2022; 11(20):6132. https://doi.org/10.3390/jcm11206132
Chicago/Turabian StyleLegendri, Sophie, Marie Carbonnel, Anis Feki, Gaby Moawad, Gabrielle Aubry, Alexandre Vallée, and Jean-Marc Ayoubi. 2022. "Improvement of Post-Operative Quality of Life in Patients 2 Years after Minimally Invasive Surgery for Pain and Deep Infiltrating Endometriosis" Journal of Clinical Medicine 11, no. 20: 6132. https://doi.org/10.3390/jcm11206132






