Potential of Stroke Imaging Using a New Prototype of Low-Field MRI: A Prospective Direct 0.55 T/1.5 T Scanner Comparison
Abstract
:1. Introduction
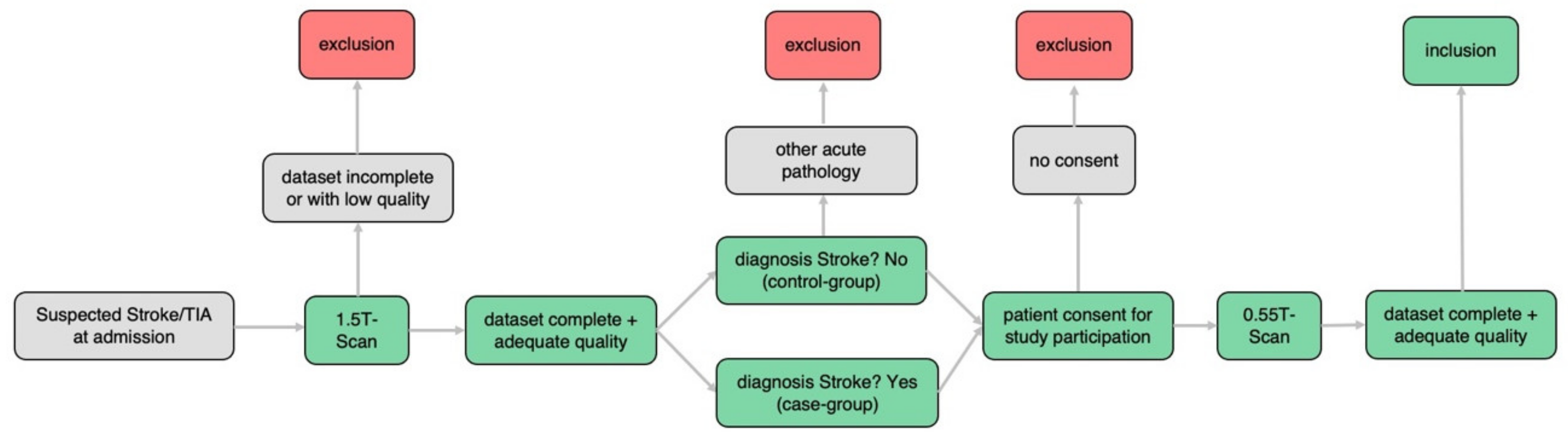
2. Materials and Methods
2.1. Patient Selection and Data Acquisition
- (a)
- Incomplete dataset 0.55T or 1.5T examination
- (b)
- Insufficient image quality 0.55T or 1.5T examination
- (c)
- No stroke but other acute pathology within initial 1.5T scan
- (d)
- No informed consent for additional 0.55T examination
- (e)
- Too large time difference between 1.5T and 0.55T examination (cut off 2 h)
- (f)
- Foreign materials not authorized for 0.55T scanners (i.e., cardiac pacemakers)
2.2. Data Analysis
2.2.1. Likert Rating
- (a)
- Overall image quality;
- (b)
- Resolution;
- (c)
- Noise;
- (d)
- Contrast;
- (e)
- Diagnostic quality.
2.2.2. Reading Study
- (a)
- Evaluation stroke yes/no;
- (b)
- Number of DWI lesions: 0, 1, 2–10, >10;
- (c)
- DWI lesion main localization (especially in the case of multiple DWI lesions);
- (d)
- Number of FLAIR lesions: 0, 1, 2–10, >10;
- (e)
- FLAIR lesion main localization (especially in the case of multiple FLAIR lesions).
2.2.3. Segmentation of DWI/ADC and FLAIR Lesions
2.3. Statistical Analysis
3. Results
3.1. Likert Rating
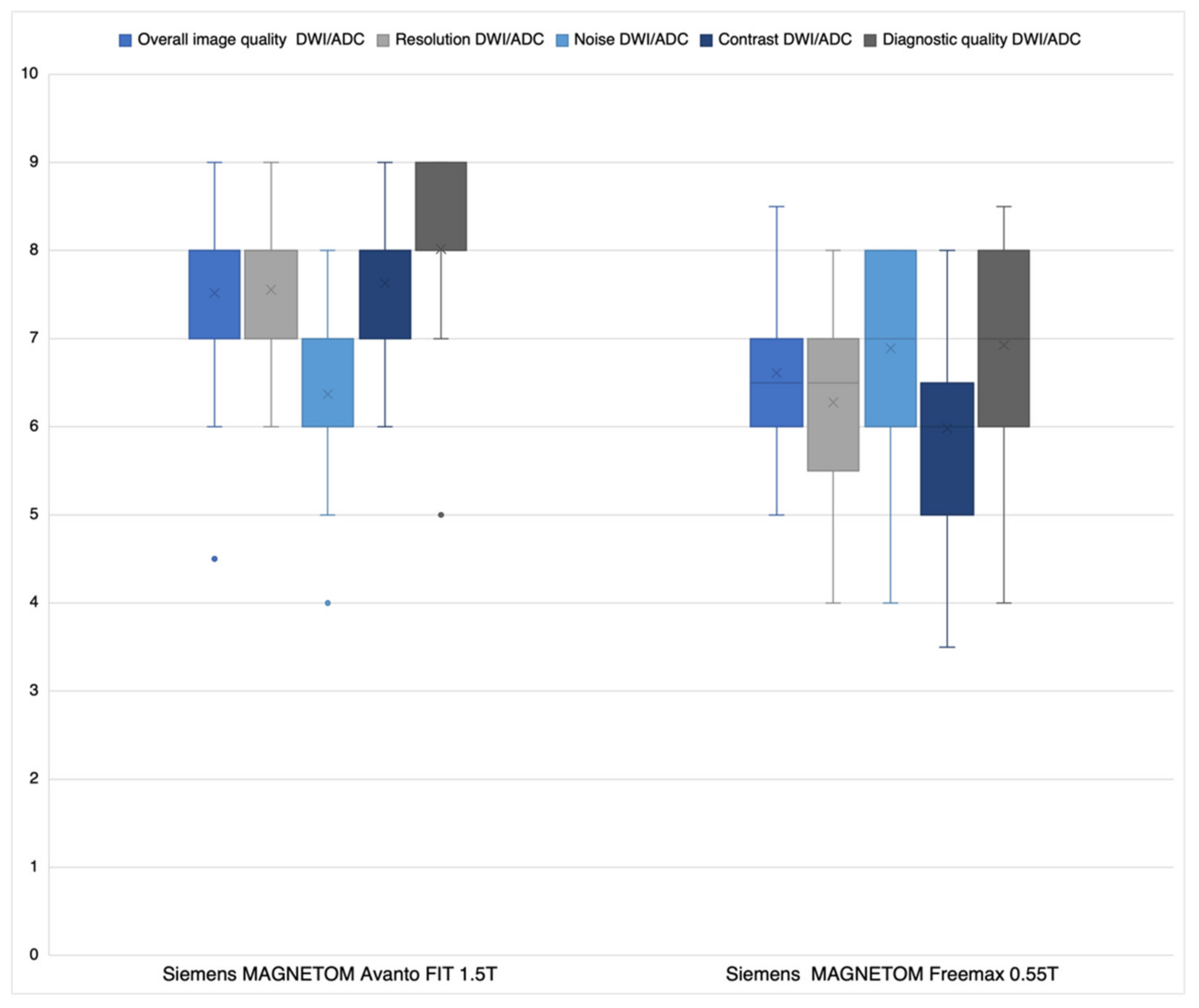
3.1.1. DWI/ADC Datasets
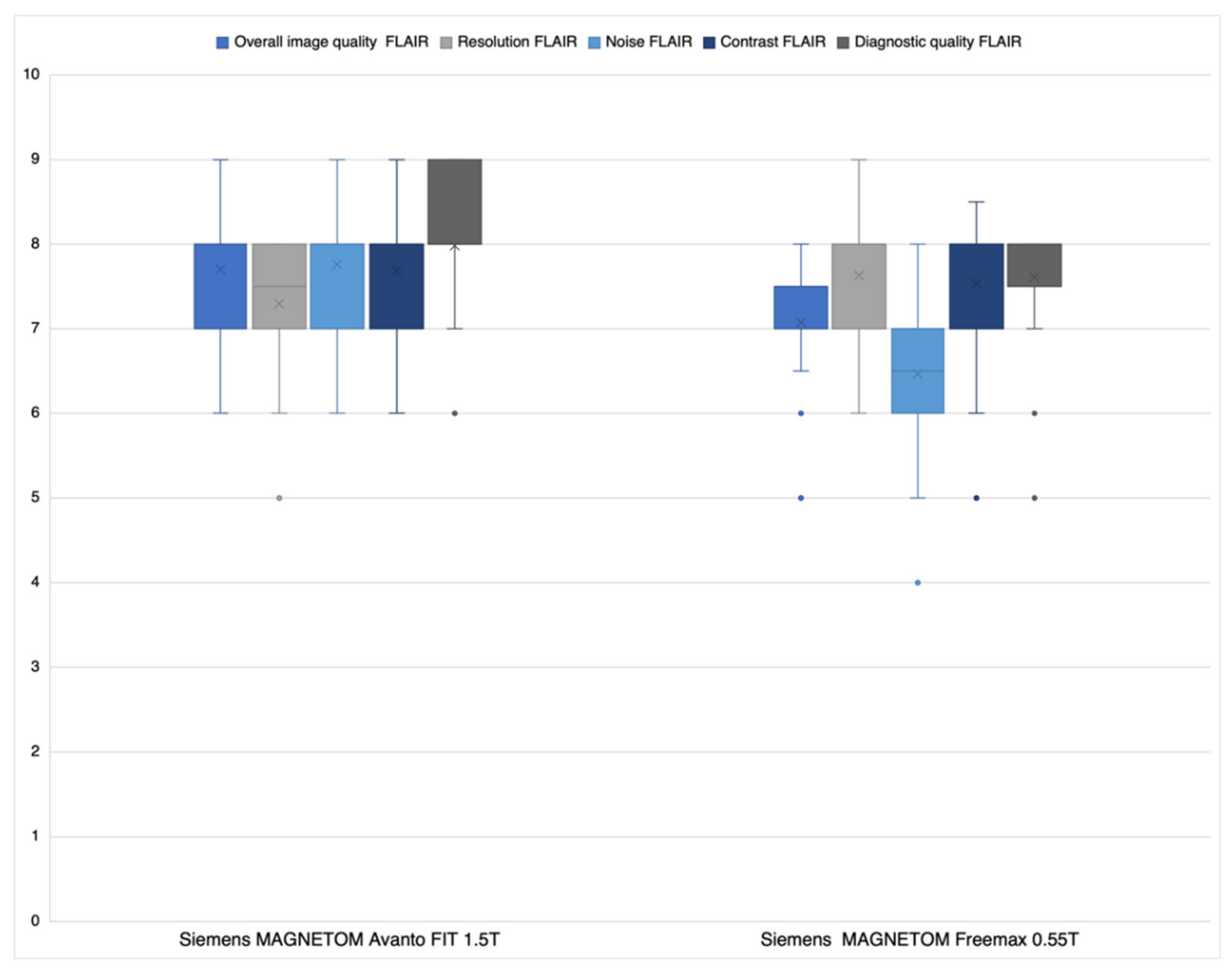
3.1.2. FLAIR Datasets
3.2. Reading Study
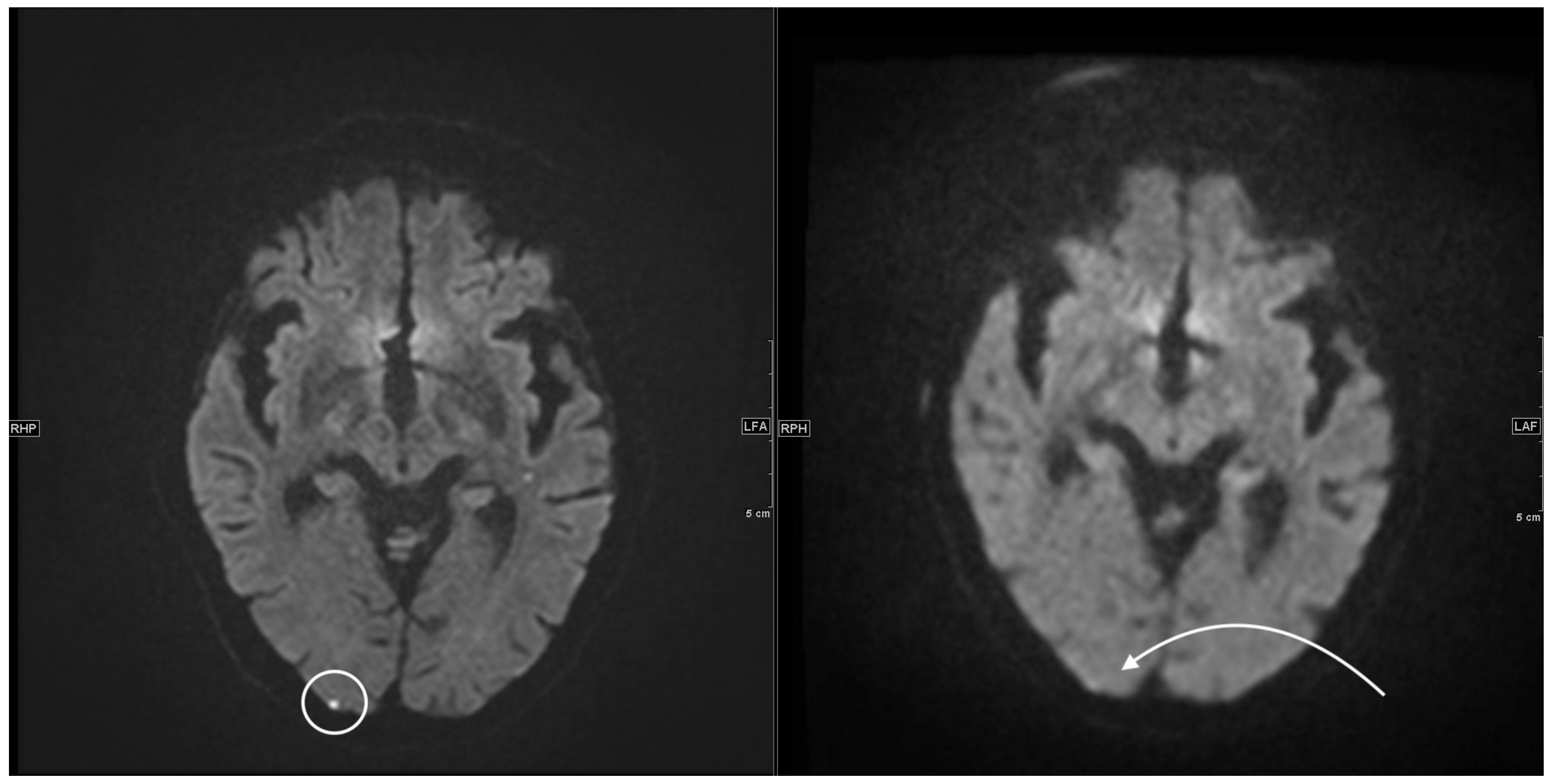
3.2.1. DWI/ADC Datasets
3.2.2. FLAIR Datasets
3.3. Segmentation of DWI/ADC and FLAIR Lesions
4. Discussion
4.1. Likert Rating
Reading Study
4.2. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADC | apparent diffusion coefficient |
| bSSFP | balanced steady-state free precession |
| BW | bandwidth |
| CNR | contrast-to-noise ratio |
| CT | computed tomography |
| DWI | diffusion-weighted imaging |
| Epi | echo-planar imaging |
| FLAIR | fluid attenuated inversion recovery |
| ICC | intraclass correlation coefficient |
| MRI | magnetic resonance imaging |
| NIHSS | National Institutes of Health Stroke Scale |
| PACS | Picture Archiving and Communication System |
| QALY | quality-adjusted life years |
| SNR | signal-to-noise ratio |
| SP | slice spacing |
| ST | slice thickness |
| SWI | susceptibility-weighted imaging |
| TIA | transient ischemic attack |
References
- Gorelick, P.B. The global burden of stroke: Persistent and disabling. Lancet Neurol. 2019, 18, 417–418. [Google Scholar] [CrossRef] [Green Version]
- Katan, M.; Luft, A. Global Burden of Stroke. Semin. Neurol. 2018, 38, 208–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnamurthi, R.V.; Moran, A.E.; Feigin, V.L.; Barker-Collo, S.; Norrving, B.; Mensah, G.A.; Taylor, S.; Naghavi, M.; Forouzanfar, M.H.; Nguyen, G.; et al. Stroke Prevalence, Mortality and Disability-Adjusted Life Years in Adults Aged 20–64 Years in 1990–2013: Data from the Global Burden of Disease 2013 Study. Neuroepidemiology 2015, 45, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Kalkonde, Y.V.; Alladi, S.; Kaul, S.; Hachinski, V. Stroke Prevention Strategies in the Developing World. Stroke 2018, 49, 3092–3097. [Google Scholar] [CrossRef] [PubMed]
- Bhat, S.S.; Fernandes, T.T.; Poojar, P.; da Silva Ferreira, M.; Rao, P.C.; Hanumantharaju, M.C.; Ogbole, G.; Nunes, R.G.; Geethanath, S. Low-Field MRI of Stroke: Challenges and Opportunities. J. Magn. Reson. Imaging 2021, 54, 372–390. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.; Parsons, M.W. Imaging selection for acute stroke intervention. Int. J. Stroke 2018, 13, 554–567. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.; Katz, J.M.; Pandya, A.; Wang, J.J.; Boltyenkov, A.; Malhotra, A.; Mushlin, A.I.; Sanelli, P.C. Cost-Effectiveness Study of Initial Imaging Selection in Acute Ischemic Stroke Care. J. Am. Coll. Radiol. 2021, 18, 820–833. [Google Scholar] [CrossRef] [PubMed]
- Mehdizade, A.; Somon, T.; Wetzel, S.; Kelekis, A.; Martin, J.B.; Scheidegger, J.R.; Sztajzel, R.; Lovblad, K.O.; Ruefenacht, D.A.; Delavelle, J. Diffusion weighted MR imaging on a low-field open magnet. Comparison with findings at 1.5 T in 18 patients with cerebral ischemia. J. Neuroradiol. 2003, 30, 25–30. [Google Scholar] [PubMed]
- Terada, H.; Gomi, T.; Harada, H.; Chiba, T.; Nakamura, T.; Iwabuchi, S.; Nemoto, H.; Kawasaki, S.; Watanabe, S.; Nagamoto, M.; et al. Development of diffusion-weighted image using a 0.3T open MRI. J. Neuroradiol. 2006, 33, 57–61. [Google Scholar] [CrossRef]
- Heiss, R.; Nagel, A.M.; Laun, F.B.; Uder, M.; Bickelhaupt, S. Low-Field Magnetic Resonance Imaging: A New Generation of Breakthrough Technology in Clinical Imaging. Investig. Radiol. 2021, 56, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Runge, V.M.; Heverhagen, J.T. The Clinical Utility of Magnetic Resonance Imaging According to Field Strength, Specifically Addressing the Breadth of Current State-of-the-Art Systems, Which Include 0.55 T, 1.5 T, 3 T, and 7 T. Investig. Radiol. 2022, 57, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Edlow, B.L.; Hurwitz, S.; Edlow, J.A. Diagnosis of DWI-negative acute ischemic stroke: A meta-analysis. Neurology 2017, 89, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Nagaraja, N. Diffusion weighted imaging in acute ischemic stroke: A review of its interpretation pitfalls and advanced diffusion imaging application. J. Neurol. Sci. 2021, 425, 117435. [Google Scholar] [CrossRef] [PubMed]
- Makin, S.D.; Doubal, F.N.; Dennis, M.S.; Wardlaw, J.M. Clinically Confirmed Stroke with Negative Diffusion-Weighted Imaging Magnetic Resonance Imaging: Longitudinal Study of Clinical Outcomes, Stroke Recurrence, and Systematic Review. Stroke 2015, 46, 3142–3148. [Google Scholar] [CrossRef] [PubMed]

| Siemens MAGNETOM FreeMax 0.55 T | Siemens MAGNETOM Avanto Fit 1.5 T | |
|---|---|---|
| FLAIR (fluid attenuated inversion recovery) transversal | ||
| Field strength in T | 0.55 | 1.5 |
| FOV (field of view) in mm2 | 209 × 230 | 187 × 230 |
| ST (slice thickness) in mm | 3 | 3 |
| SS (slice spacing) | 3.6 | 3.6 |
| Number of slices | 40 | 40 |
| PS (pixel spacing) in mm2 | 1.28 × 1.03 | 0.9 × 0.9 |
| TR (repetition time) in msec | 7780 | 8510 |
| TE (echo time) in msec | 96 | 112 |
| TI (inversion delay) in msec | 2368.8 | 2460 |
| Turbo Factor | 15 | 19 |
| TA (time of acquisition) in min | 5:28 | 3:26 |
| BW (Bandwidth) | 150 | 130 |
| 3D SWI (susceptibility weighted imaging) transversal | ||
| Field strength in T | 0.55 | 1.5 |
| Sequence type | Multi shot 3D EPI | 3D FLASH |
| FOV (field of view) in mm2 | 201 × 230 | 194 × 230 |
| ST (slice thickness) in mm | 3 | 3 |
| Number of slices | 40 | 48 |
| PS (pixel spacing) in mm2 | 0.94 × 0.8 | 1.12 × 0.9 |
| TR (repetition time) in msec | 172 | 48 |
| TE (echo time) in msec | 100 | 40 |
| Parallel imaging | - | GRAPPA factor 2 |
| TA (time of acquisition) in min | 2:23 | 2:17 |
| BW (Bandwidth) | 276 | 80 |
| Single shot diffusion EPI (echo-planar imaging) transversal | ||
| Field strength in T | 0.55 | 1.5 |
| FOV (field of view) in mm2 | 220 × 220 | 230 × 230 |
| ST (slice thickness) in mm | 3 | 3 |
| SS (slice spacing) | 3.6 | 3.6 |
| Number of slices | 40 | 40 |
| PS (pixel spacing) in mm2 | 1.67 × 1.67 | 1.44 × 1.44 |
| b values in s/mm2 | 0, 1000 | 0, 1000 |
| TR (repetition time) in msec | 7400 | 6200 |
| TE (echo time) in msec | 102 | 103 |
| Parallel imaging | GRAPPA factor 2 | GRAPPA factor 2 |
| TA (time of acquisition) in min | 4:35 | 2:04 |
| BW (Bandwidth) | 842 | 1490 |
| Patient | Patient Age | Neurological Symptoms at Admission | NIHSS | Control-Group (C), Stroke-Cohort (S) | Final Radiological Report | Time Gap between Scans in min | Time Gap between Onset and Scan 1 in min |
|---|---|---|---|---|---|---|---|
| Patient 1 | 87 | facial droop, dysarthria, hemiparesis right side | 3 | S | acute to subacute infarct corpus nuclei caudati and cranial parts of the nucleus lentiformis left side | 46 | 1166 |
| Patient 2 | 88 | ataxic gait and standing | no data | S | acute to subacute infarct lateral pontin left side | 37 | unknown |
| Patient 3 | 82 | visual deficit | no data | S | acute to subacute punctiform infarcts parietal left and cerebellar right | 93 | unknown |
| Patient 4 | 84 | intermittent dysarthria | 1 | S | acute to subacute infarct thalamus left side | 33 | unknown |
| Patient 5 | 58 | facial droop, hemiparesis right side | 10 | S | multiple subacute infarcts posterior circulation on both sides | 40 | 1050 |
| Patient 6 | 65 | low-grade facial paresis left side | 1 | S | acute to subacute infarcts of the thalamus and occipital/occipitotemporal right side | 20 | 1175 |
| Patient 7 | 65 | dysdiadochokinesis right side | no data | S | subacute punctiform infarcts frontal and parietal left side | 24 | 1704 |
| Patient 8 | 75 | facial droop right side | 0 | S | punctiform infarct gyrus postcentralis left side | 22 | 1135 |
| Patient 9 | 82 | confusion | no data | S | acute to subacute infarcts frontal and parietal left side | 32 | unknown |
| Patient 10 | 79 | hemiataxia left side | 2 | S | acute to subacute infarct thalamus right side | 42 | 1492 |
| Patient 11 | 86 | dysarthria, ataxia right leg | 3 | S | acute infarct posterolateral pons left side | 25 | unknown |
| Patient 12 | 83 | leg-emphasized hemiparesis left side | 5 | S | subacute infarct gyrus precentralis right side | 31 | unknown |
| Patient 13 | 89 | visual deficit | 2 | S | acute cortical infarcts parietooccipital and frontal right side | 38 | 2198 |
| Patient 14 | 69 | no data | no data | S | subacute infarct central left side | 42 | unknown |
| Patient 15 | 73 | amaurosis fugax | 0 | C | no stroke | 25 | 1197 |
| Patient 16 | 29 | strong nystagmus to left side, headache right frontal, vertigo | no data | C | no stroke | 48 | unknown |
| Patient 17 | 70 | atypical transient global amnesia | no data | C | no stroke | 44 | unknown |
| Patient 18 | 87 | aphasia | no data | C | no stroke | 32 | unknown |
| Patient 19 | 74 | vertigo | 0 | C | no stroke | 25 | 826 |
| Patient 20 | 60 | aphasia | 0 | C | no stroke | 21 | unknown |
| Patient 21 | 44 | vertigo | 0 | C | no stroke | 49 | unknown |
| Patient 22 | 80 | short-term loss of vision left side | no data | C | no stroke | 35 | 2092 |
| Patient 23 | 84 | vertigo, gait instability | no data | C | no stroke | 48 | 425 |
| Patient 24 | 84 | vertigo, gait instability | no data | C | no stroke | 32 | unknown |
| Patient 25 | 53 | aphasia | 1 | excluded | subacute punctiform infarcts frontal and parietal left side | 916 | 1197 |
| Patient 26 | 59 | transient global amnesia | 0 | excluded | bilateral punctiform diffusion-restrictions of the hippocampus head | 2936 | 1394 |
| Patient 27 | 46 | facial droop, descending arm left side | 2 | excluded | acute to subacute infarct lenticostriatal right side | 2812 | 1406 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rusche, T.; Breit, H.-C.; Bach, M.; Wasserthal, J.; Gehweiler, J.; Manneck, S.; Lieb, J.M.; De Marchis, G.M.; Psychogios, M.N.; Sporns, P.B. Potential of Stroke Imaging Using a New Prototype of Low-Field MRI: A Prospective Direct 0.55 T/1.5 T Scanner Comparison. J. Clin. Med. 2022, 11, 2798. https://doi.org/10.3390/jcm11102798
Rusche T, Breit H-C, Bach M, Wasserthal J, Gehweiler J, Manneck S, Lieb JM, De Marchis GM, Psychogios MN, Sporns PB. Potential of Stroke Imaging Using a New Prototype of Low-Field MRI: A Prospective Direct 0.55 T/1.5 T Scanner Comparison. Journal of Clinical Medicine. 2022; 11(10):2798. https://doi.org/10.3390/jcm11102798
Chicago/Turabian StyleRusche, Thilo, Hanns-Christian Breit, Michael Bach, Jakob Wasserthal, Julian Gehweiler, Sebastian Manneck, Johanna Maria Lieb, Gian Marco De Marchis, Marios Nikos Psychogios, and Peter B. Sporns. 2022. "Potential of Stroke Imaging Using a New Prototype of Low-Field MRI: A Prospective Direct 0.55 T/1.5 T Scanner Comparison" Journal of Clinical Medicine 11, no. 10: 2798. https://doi.org/10.3390/jcm11102798
APA StyleRusche, T., Breit, H.-C., Bach, M., Wasserthal, J., Gehweiler, J., Manneck, S., Lieb, J. M., De Marchis, G. M., Psychogios, M. N., & Sporns, P. B. (2022). Potential of Stroke Imaging Using a New Prototype of Low-Field MRI: A Prospective Direct 0.55 T/1.5 T Scanner Comparison. Journal of Clinical Medicine, 11(10), 2798. https://doi.org/10.3390/jcm11102798







