The Interplay between Perioperative Oxidative Stress and Hepatic Dysfunction after Human Liver Resection: A Prospective Observational Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surgical and Anesthesiologic Details
2.2. Sample Collection and Analysis
2.3. Markers of Oxidative Stress
2.4. Immunohistochemical Staining of Liver Biopsies
2.5. Statistical Analysis
3. Results
3.1. Study Cohort
3.2. Clinical Factors Associated with PHLF (Bivariate Analysis)
3.3. Perioperative Oxidative Stress Blood Marker Dynamics after Hepatectomy
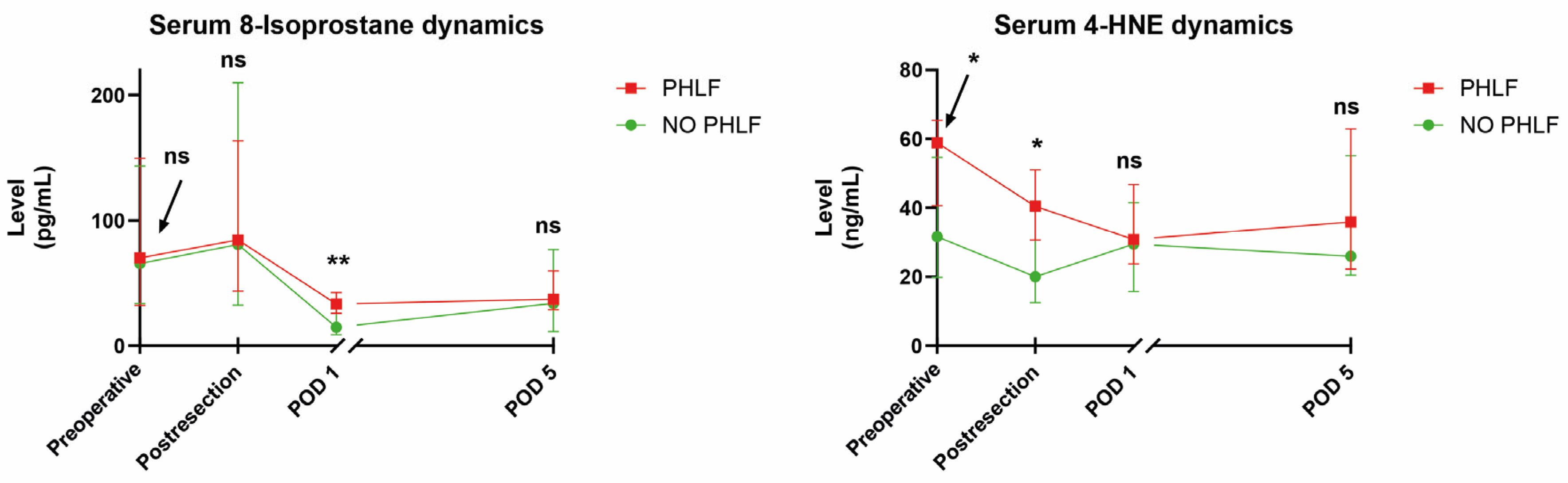
3.4. Associations of Oxidative Stress Blood Markers with PHLF and PHLF-Related Risk Factors
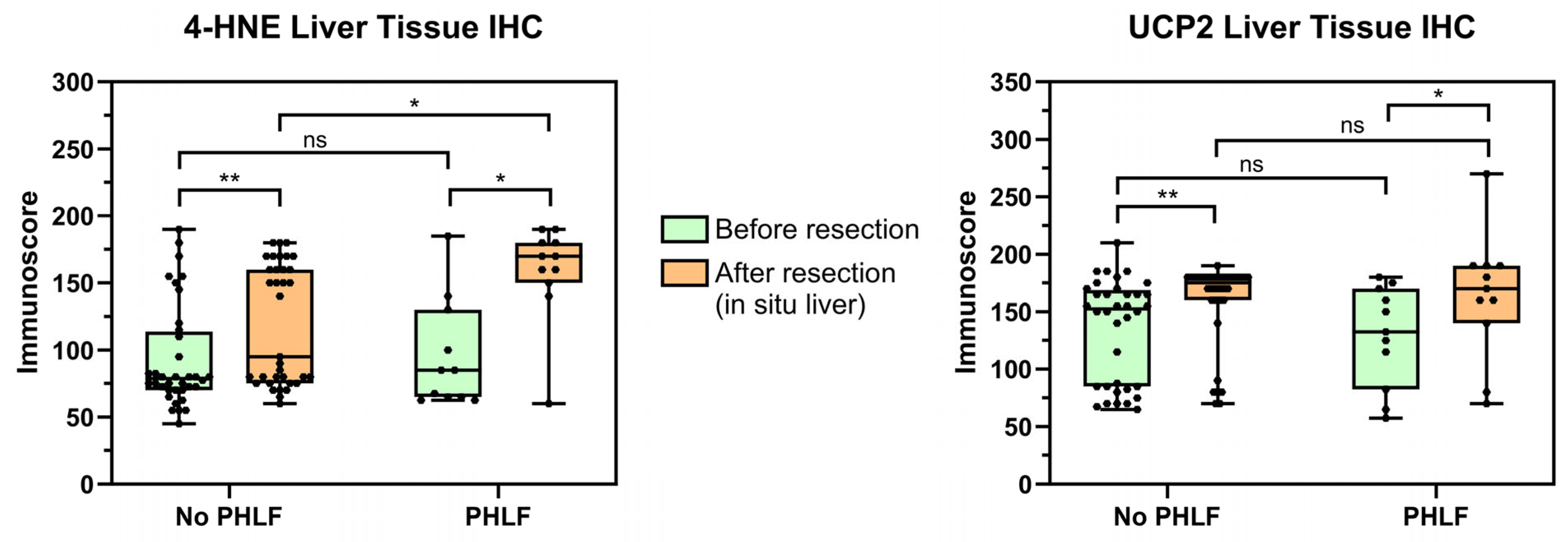
3.5. Immunohistochemical Analysis of Oxidative Stress
3.6. Associations of Liver Tissue Oxidative Stress with PHLF and PHLF-Related Risk Factors
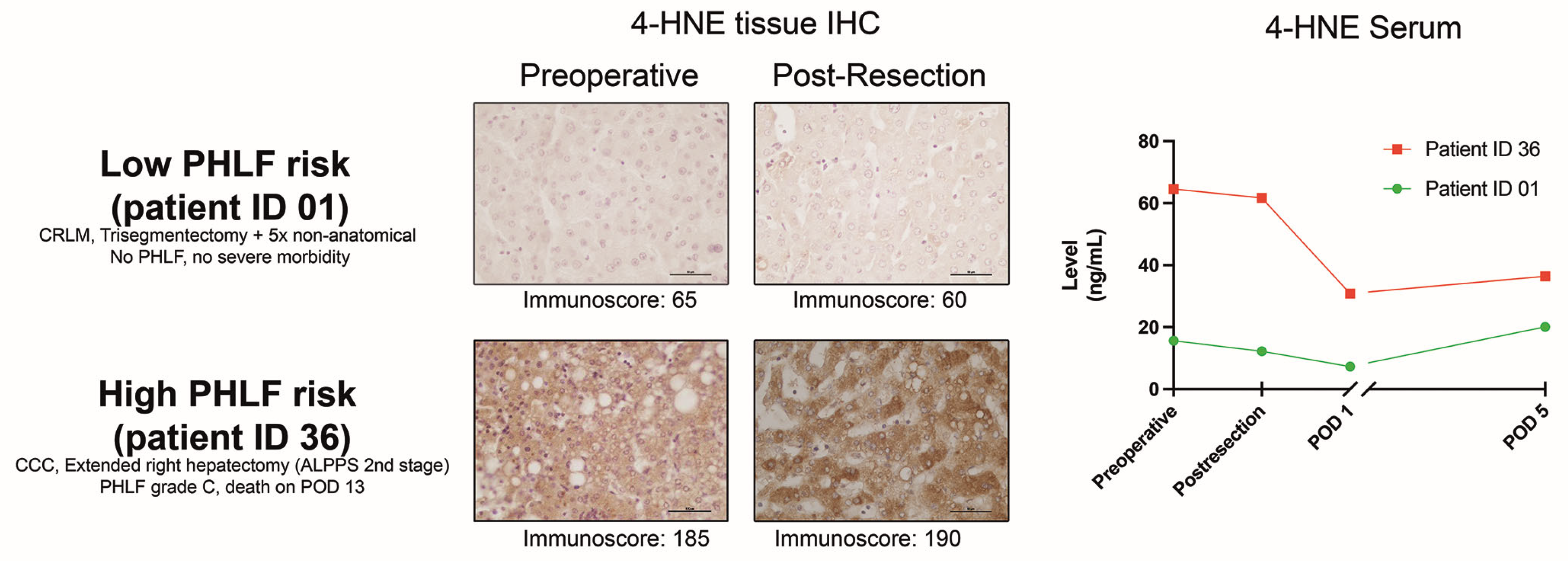
3.7. Intraoperative PHLF Prediction Combining Post-Resection Tissue and Serum Markers
3.8. Potential Influence of Malignant Entities and Tumor Burden on Oxidative Stress Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ambade, A.; Mandrekar, P. Oxidative stress and inflammation: Essential partners in alcoholic liver disease. Int. J. Hepatol. 2012, 2012, 853175. [Google Scholar] [CrossRef] [PubMed]
- Ucar, F.; Sezer, S.; Erdogan, S.; Akyol, S.; Armutcu, F.; Akyol, O. The relationship between oxidative stress and nonalcoholic fatty liver disease: Its effects on the development of nonalcoholic steatohepatitis. Redox Rep. 2013, 18, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Pourova, J.; Kottova, M.; Voprsalova, M.; Pour, M. Reactive oxygen and nitrogen species in normal physiological processes. Acta Physiol. 2010, 198, 15–35. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.; Galano, J.M.; Durand, T.; Le Guennec, J.Y.; Lee, J.C. Physiological role of reactive oxygen species as promoters of natural defenses. FASEB J. 2017, 31, 3729–3745. [Google Scholar] [CrossRef] [PubMed]
- Senoner, T.; Schindler, S.; Stattner, S.; Ofner, D.; Troppmair, J.; Primavesi, F. Associations of oxidative stress and postoperative outcome in liver surgery with an outlook to future potential therapeutic options. Oxid. Med. Cell Longev. 2019, 2019, 3950818. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeldt, F.; Wilson, M.; Lee, G.; Kure, C.; Ou, R.; Braun, L.; de Haan, J. Oxidative stress in surgery in an ageing population: Pathophysiology and therapy. Exp. Gerontol. 2013, 48, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Reiniers, M.J.; van Golen, R.F.; van Gulik, T.M.; Heger, M. Reactive oxygen and nitrogen species in steatotic hepatocytes: A molecular perspective on the pathophysiology of ischemia-reperfusion injury in the fatty liver. Antioxid. Redox Signal 2014, 21, 1119–1142. [Google Scholar] [CrossRef] [PubMed]
- Cavalca, V.; Tremoli, E.; Porro, B.; Veglia, F.; Myasoedova, V.; Squellerio, I.; Manzone, D.; Zanobini, M.; Trezzi, M.; Di Minno, M.N.; et al. Oxidative stress and nitric oxide pathway in adult patients who are candidates for cardiac surgery: Patterns and differences. Interact. Cardiovasc. Thorac. Surg. 2013, 17, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, M.; Sato, E.F.; Inoue, M.; Asada, A. Open abdominal surgery increases intraoperative oxidative stress: Can it be prevented? Anesth. Analg. 2008, 107, 1946–1952. [Google Scholar] [CrossRef]
- Senoner, T.; Velik-Salchner, C.; Luckner, G.; Tauber, H. Anesthesia-induced oxidative stress: Are there differences between intravenous and inhaled anesthetics? Oxid. Med. Cell Longev. 2021, 2021, 8782387. [Google Scholar] [CrossRef]
- Cichoz-Lach, H.; Michalak, A. Oxidative stress as a crucial factor in liver diseases. World J. Gastroenterol. 2014, 20, 8082–8091. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.T.; Cheng, S.B.; Huang, Y.C.; Huang, Y.T.; Lin, P.T. Coenzyme q10 and oxidative stress: Inflammation status in hepatocellular carcinoma patients after surgery. Nutrients 2017, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.; Fitschek, F.; Bar-Or, D.; Klaus, D.A.; Tudor, B.; Fleischmann, E.; Roth, G.; Tamandl, D.; Wekerle, T.; Gnant, M.; et al. Inflammatory response and oxidative stress during liver resection. PLoS ONE 2017, 12, e0185685. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.L.; McKenna, H.T.; Filipe, H.; Lau, L.; Fernandez, B.O.; Murray, A.J.; Feelisch, M.; Martin, D.S. Perioperative redox changes in patients undergoing hepato-pancreatico-biliary cancer surgery. Perioper. Med. 2023, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, X. An oxidative stress-related signature for predicting the prognosis of liver cancer. Front. Genet. 2022, 13, 975211. [Google Scholar] [CrossRef] [PubMed]
- Uchida, D.; Takaki, A.; Ishikawa, H.; Tomono, Y.; Kato, H.; Tsutsumi, K.; Tamaki, N.; Maruyama, T.; Tomofuji, T.; Tsuzaki, R.; et al. Oxidative stress balance is dysregulated and represents an additional target for treating cholangiocarcinoma. Free Radic. Res. 2016, 50, 732–743. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.X.; Wang, Y.B.; Wu, J.; Ding, G.S.; Wu, Y.; Wei, L.H.; Wang, F.; Zhang, Z.M. Clinical significance of serum oxidative stress and serum uric acid levels before surgery for hepatitis b-related liver cancer. World J. Gastrointest. Surg. 2023, 15, 1995–2002. [Google Scholar] [CrossRef]
- Liu, H.T.; Huang, Y.C.; Cheng, S.B.; Huang, Y.T.; Lin, P.T. Effects of coenzyme q10 supplementation on antioxidant capacity and inflammation in hepatocellular carcinoma patients after surgery: A randomized, placebo-controlled trial. Nutr. J. 2016, 15, 85. [Google Scholar] [CrossRef] [PubMed]
- Burke, A.; FitzGerald, G.A.; Lucey, M.R. A prospective analysis of oxidative stress and liver transplantation. Transplantation 2002, 74, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Jara, M.; Reese, T.; Malinowski, M.; Valle, E.; Seehofer, D.; Puhl, G.; Neuhaus, P.; Pratschke, J.; Stockmann, M. Reductions in post-hepatectomy liver failure and related mortality after implementation of the limax algorithm in preoperative work-up: A single-centre analysis of 1170 hepatectomies of one or more segments. HPB 2015, 17, 651–658. [Google Scholar] [CrossRef]
- Fodor, M.; Primavesi, F.; Braunwarth, E.; Cardini, B.; Resch, T.; Bale, R.; Putzer, D.; Henninger, B.; Oberhuber, R.; Maglione, M.; et al. Indications for liver surgery in benign tumours. Eur. Surg. 2018, 50, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Primavesi, F.; Maglione, M.; Cipriani, F.; Denecke, T.; Oberkofler, C.E.; Starlinger, P.; Dasari, B.V.M.; Heil, J.; Sgarbura, O.; Soreide, K.; et al. E-ahpba-esso-essr innsbruck consensus guidelines for preoperative liver function assessment before hepatectomy. Br. J. Surg. 2023, 110, 1331–1347. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; Dematteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the international study group of liver surgery (isgls). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef] [PubMed]
- Sparrelid, E.; Olthof, P.B.; Dasari, B.V.M.; Erdmann, J.I.; Santol, J.; Starlinger, P.; Gilg, S. Current evidence on posthepatectomy liver failure: Comprehensive review. BJS Open 2022, 6, zrac142. [Google Scholar] [CrossRef] [PubMed]
- Kauffmann, R.; Fong, Y. Post-hepatectomy liver failure. Hepatobiliary Surg. Nutr. 2014, 3, 238–246. [Google Scholar] [PubMed]
- Niederwieser, T.; Braunwarth, E.; Dasari, B.V.M.; Pufal, K.; Szatmary, P.; Hackl, H.; Haselmann, C.; Connolly, C.E.; Cardini, B.; Ofner, D.; et al. Early postoperative arterial lactate concentrations to stratify risk of post-hepatectomy liver failure. Br. J. Surg. 2021, 108, 1360–1370. [Google Scholar] [CrossRef] [PubMed]
- Soreide, J.A.; Deshpande, R. Post hepatectomy liver failure (phlf)-recent advances in prevention and clinical management. Eur. J. Surg. Oncol. 2021, 47, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Gilg, S.; Sandstrom, P.; Rizell, M.; Lindell, G.; Ardnor, B.; Stromberg, C.; Isaksson, B. The impact of post-hepatectomy liver failure on mortality: A population-based study. Scand. J. Gastroenterol. 2018, 53, 1335–1339. [Google Scholar] [CrossRef] [PubMed]
- Kawano, F.; Yoshioka, R.; Ichida, H.; Mise, Y.; Saiura, A. Essential updates 2021/2022: Update in surgical strategy for perihilar cholangiocarcinoma. Ann. Gastroenterol. Surg. 2023, 7, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.; Shrikhande, S.; Goel, M. Post hepatectomy liver failure: Concept of management. J. Gastrointest. Cancer 2014, 45, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Fu, Q.; Wuyun, G.; Wuyun, T. Management of post-hepatectomy complications. World J. Gastroenterol. 2013, 19, 7983–7991. [Google Scholar] [CrossRef] [PubMed]
- de Meijer, V.E.; Kalish, B.T.; Puder, M.; Ijzermans, J.N. Systematic review and meta-analysis of steatosis as a risk factor in major hepatic resection. Br. J. Surg. 2010, 97, 1331–1339. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.K.; Barbas, A.S.; Turley, R.S.; Steel, J.L.; Tsung, A.; Marsh, J.W.; Geller, D.A.; Clary, B.M. A standard definition of major hepatectomy: Resection of four or more liver segments. HPB 2011, 13, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Shoeb, M.; Ansari, N.H.; Srivastava, S.K.; Ramana, K.V. 4-hydroxynonenal in the pathogenesis and progression of human diseases. Curr. Med. Chem. 2014, 21, 230–237. [Google Scholar] [CrossRef]
- Boteon, Y.L.; Laing, R.W.; Schlegel, A.; Wallace, L.; Smith, A.; Attard, J.; Bhogal, R.H.; Neil, D.A.H.; Hubscher, S.; Perera, M.; et al. Combined hypothermic and normothermic machine perfusion improves functional recovery of extended criteria donor livers. Liver Transpl. 2018, 24, 1699–1715. [Google Scholar] [CrossRef]
- Kobayashi, H.; Tanaka, Y.; Asagiri, K.; Asakawa, T.; Tanikawa, K.; Kage, M.; Yagi, M. The antioxidant effect of green tea catechin ameliorates experimental liver injury. Phytomedicine 2010, 17, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Detre, S.; Saclani Jotti, G.; Dowsett, M. A “quickscore” method for immunohistochemical semiquantitation: Validation for oestrogen receptor in breast carcinomas. J. Clin. Pathol. 1995, 48, 876–878. [Google Scholar] [CrossRef]
- Akbulut, S.; Uremis, M.M.; Sarici, K.B.; Uremis, N.; Hargura, A.S.; Karakas, S.; Dogan, U.G.; Turkoz, Y.; Yilmaz, S. Measurement of oxidant and antioxidant levels in liver tissue obtained from patients with liver transplantation: A case-control study. Transpl. Immunol. 2022, 75, 101697. [Google Scholar] [CrossRef]
- Augusto, V.S.; Rodrigues, A.J.; Reis, G.S.; Silveira, A.P.; de Castro e Silva, O., Jr.; Mente, E.D.; Jordao, A.A., Jr.; Evora, P.R. Evaluation of oxidative stress in the late postoperative stage of liver transplantation. Transplant. Proc. 2014, 46, 1453–1457. [Google Scholar] [CrossRef]
- Comporti, M.; Arezzini, B.; Signorini, C.; Vecchio, D.; Gardi, C. Oxidative stress, isoprostanes and hepatic fibrosis. Histol. Histopathol. 2009, 24, 893–900. [Google Scholar] [PubMed]
- Smathers, R.L.; Galligan, J.J.; Stewart, B.J.; Petersen, D.R. Overview of lipid peroxidation products and hepatic protein modification in alcoholic liver disease. Chem. Biol. Interact. 2011, 192, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Haga, S.; Ozawa, T.; Yamada, Y.; Morita, N.; Nagashima, I.; Inoue, H.; Inaba, Y.; Noda, N.; Abe, R.; Umezawa, K.; et al. P62/sqstm1 plays a protective role in oxidative injury of steatotic liver in a mouse hepatectomy model. Antioxid. Redox Signal 2014, 21, 2515–2530. [Google Scholar] [CrossRef] [PubMed]
- Kong, E.; Yuan, C.; Li, Y.; Tian, T.; He, Y.; Feng, X. Protective efficiency comparison of direct and remote ischemic preconditioning on ischemia reperfusion injury of the liver in patients undergoing partial hepatectomy. Biomed. Res. Int. 2023, 2023, 2763320. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.; Engstrand, J.; Rajala, P.; Grip, J.; Ghorbani, P.; Sparrelid, E.; Gilg, S. Comparing the accuracy of prediction models to detect clinically relevant post-hepatectomy liver failure early after major hepatectomy. Br. J. Surg. 2024, 111, znad433. [Google Scholar] [CrossRef] [PubMed]
- Starlinger, P.; Pereyra, D.; Haegele, S.; Braeuer, P.; Oehlberger, L.; Primavesi, F.; Kohler, A.; Offensperger, F.; Reiberger, T.; Ferlitsch, A.; et al. Perioperative von willebrand factor dynamics are associated with liver regeneration and predict outcome after liver resection. Hepatology 2018, 67, 1516–1530. [Google Scholar] [CrossRef] [PubMed]
- Ayad, A.; Hallawa, A.; Peine, A.; Martin, L.; Fazlic, L.B.; Dartmann, G.; Marx, G.; Schmeink, A. Predicting abnormalities in laboratory values of patients in the intensive care unit using different deep learning models: Comparative study. JMIR Med. Inform. 2022, 10, e37658. [Google Scholar] [CrossRef] [PubMed]
- Öfner, D. Quality assurance in surgery—A moral obligation. Eur. Surg. 2024. [CrossRef]
- Loffredo, L.; Del Ben, M.; Perri, L.; Carnevale, R.; Nocella, C.; Catasca, E.; Baratta, F.; Ceci, F.; Polimeni, L.; Gozzo, P.; et al. Effects of dark chocolate on nox-2-generated oxidative stress in patients with non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2016, 44, 279–286. [Google Scholar] [CrossRef] [PubMed]



| Age (years), median (IQR) | 58.5 (51; 68.8) |
| Male sex | 31 (59.6%) |
| BMI, median (IQR) | 25.5 (16.2 to 40.3) |
| Charlson Comorbidity Index (CCI), median (IQR) | 6 (3; 7) |
| ASA Classification | |
| 1 | 5 (9.6%) |
| 2 | 38 (73.1%) |
| 3 | 9 (17.3%) |
| Liver parenchymal disease | |
| Steatosis | 8 (15.4%) |
| Fibrosis | 4 (7.7%) |
| Cirrhosis | 0 (0%) |
| Preoperative chemotherapy | 8 (15.4%) |
| Indication for surgery | |
| CRLM | 15 (28.8%) |
| CCC | 11 (21.2%) |
| HCC | 11 (21.2%) |
| Benign/pre-malignant lesions | 6 (11.5%) |
| Non-CRLM | 5 (9.6%) |
| Other primary liver tumors | 2 (3.8%) |
| Echinococcus | 1 (1.9%) |
| Chronic cholangitis | 1 (1.9%) |
| Surgical procedures and perioperative outcomes | |
| Major resection (>3 segments) | 36 (69.2%) |
| Liver resection type | |
| Right hemihepatectomy | 13 (25%) |
| Left hemihepatectomy | 3 (5.8%) |
| Extended right hepatectomy | 10 (19.2%) |
| Extended left hepatectomy | 6 (11.5%) |
| Bisegmentectomy | 7 (13.5%) |
| Other anatomical and non-anatomical resections | 13 (25%) |
| Inflow occlusion/Pringle maneuver applied | 17 (32.7%) |
| Operative time (minutes), median (IQR) | 334 (275; 433) |
| Intraoperative blood loss (mL), median (IQR) | 700 (413; 1000) |
| Intraoperative transfusion (number of packs) | |
| 1 | 6 (12%) |
| >1 | 11 (21%) |
| Length of hospital stay (days), median (IQR) | 10 (8; 19) |
| 90-day morbidity overall | 28 (53.8%) |
| Severe complications (Clavien–Dindo >3a) | 11 (21.2%) |
| 90-day mortality | 2 (3.8%) |
| PHLF (ISGLS); clinically relevant PHLF (ISGLS Grade B/C) | 13 (25%); 7 (13.5%) |
| Preoperatively | Post-Resection | POD 1 | POD 5 | |
|---|---|---|---|---|
| 8-Isoprostane (pg/mL) | ||||
| No PHLF | 65.5 (34.0–143.2) | 80.8 (32.3–209.8) | 14.7 (8.9–30.7) | 33.9 (11.4–76.8) |
| PHLF | 70.2 (32.1–149.6) | 84.5 (43.6–163.5) | 33.3 (25.9–42.5) | 37.2 (28.6–59.7) |
| p-value * | 0.792 | 0.983 | 0.006 | 0.691 |
| 4-HNE (ng/mL) | ||||
| No PHLF | 31.6 (19.8–54.6) | 20.0 (12.5–41.04) | 29.5 (15.7–41.5) | 26.0 (20.5–55.1) |
| PHLF | 58.9 (40.6–65.4) | 40.4 (30.7–51.1) | 30.8 (23.8–46.8) | 35.9 (22.3–62.9) |
| p-value * | 0.029 | 0.013 | 0.296 | 0.820 |
| Vitamin A (mg/L) | ||||
| No PHLF | 0.37 (0.23–0.47) | n/a | 0.2 (0.14–0.28) | n/a |
| PHLF | 0.34 (0.25–0.44) | n/a | 0.13 (0.1–0.24) | n/a |
| p-value * | 0.848 | 0.097 | ||
| Vitamin E (mg/L) | ||||
| No PHLF | 13.32 (10.89–15.51) | n/a | 9.31 (7.42–11.41) | n/a |
| PHLF | 11.32 (10.31–15.12) | n/a | 7.2 (6.02–9.51) | n/a |
| p-value * | 0.719 | 0.170 | ||
| TAC (nmol/μL) | ||||
| No PHLF | 154.5 (117.9–188.9) | 123.3 (88.5–146.8) | 120.3 (103.1–152.8) | 143.7 (116.5–166.6) |
| PHLF | 166.3 (137.6–214.8) | 156.3 (101.8–163.5) | 148.4 (98.1–162.4) | 145.2 (110.0–161.9) |
| p-value * | 0.139 | 0.148 | 0.410 | 1.000 |
| 8-Isoprostane (pg/mL) | 4-HNE (ng/mL) | |||||
|---|---|---|---|---|---|---|
| Preoperative | Post-Resection | POD 1 | Preoperative | Post-Resection | POD 1 | |
| Age > 60 years | ||||||
| No | 59.9 (19.4–105.7) | 68.7 (30.7–172.8) | 17.5 (11.0–31.6) | 45.5 (28.0–61.3) | 30.6 (17.1–46.1) | 30.3 (17.0–45.0) |
| Yes | 73.9 (45.4–146.6) | 82.7 (49.6–190.5) | 23.6 (12.3–39.0) | 31.0 (18.8–52.2) | 24.5 (13.7–41.4) | 29.9 (18.3–42.1) |
| p-value * | 0.212 | 0.497 | 0.388 | 0.069 | 0.582 | 0.890 |
| Steatosis/Fibrosis | ||||||
| No | 64.1 (33.9–147.6) | 84.8 (37.7–172.8) | 21.7 (11.0–35.1) | 39.4 (19.7–58.0) | 25.1 (12.8–41.2) | 28.4 (15.2–39.0) |
| Yes | 69.1 (22.6–117.7) | 69.7 (30.6–176.2) | 27.6 (15.3–38.0) | 42.5 (25.4–62.5) | 39.9 (20.1–54.8) | 42.2 (29.7–56.7) |
| p-value * | 0.680 | 0.704 | 0.799 | 0.441 | 0.039 | 0.008 |
| Cholangiocarcinoma | ||||||
| No | 54.3 (30.6–103.3) | 58.6 (31.4–163.2) | 14.7 (8.9–33.5) | 38.8 (21.7–55.3) | 23.8 (14.5–40.9) | 30.2 (16.5–44.6) |
| Yes | 166.6 (46.7–229.2) | 163.6 (80.7–233.0) | 31.7 (24.3–39.7) | 54.6 (19.8–64.6) | 41.3 (14.2–49.8) | 30.3 (20.8–31.0) |
| p-value * | 0.014 | 0.043 | 0.007 | 0.330 | 0.161 | 0.823 |
| Neoadjuvant CTX | ||||||
| No | 66.8 (34.4–140.5) | 84.8 (42.4–195.9) | 23.5 (12.1–38.8) | 42.5 (23.6–60.6) | 32.9 (18.0–46.1) | 30.4 (21.9–43.4) |
| Yes | 64.0 (19.4–140.0) | 38.25 (24.2–143.5) | 13.4 (9.2–27.1) | 23.8 (16.4–48.9) | 11.5 (6.2–25.7) | 18.5 (8.1–33.9) |
| p-value * | 0.718 | 0.127 | 0.140 | 0.108 | 0.024 | 0.065 |
| Pringle maneuver | ||||||
| No | 77.6 (48.1–157.0) | 50.6 (27.5–167.2) | 28.8 (20.2–39.4) | 42.9 (25.5–58.2) | 41.3 (20.6–51.1) | 30.3 (19.0–46.8) |
| Yes | 54.3 (31.3–117.9) | 84.5 (38.0–174.3) | 13.7 (8.4–35.5) | 38.8 (19.6–58.9) | 19.9 (13.5–38.4) | 29.1 (15.7–39.5) |
| p-value * | 0.230 | 0.592 | 0.015 | 0.501 | 0.031 | 0.532 |
| Intraop. Transfusion | ||||||
| No | 77.6 (33.7–143.2) | 84.5 (30.5–174.3) | 22.2 (11.5–36.2) | 41.2 (19.8–55.4) | 20.5 (14.2–42.3) | 29.5 (17.2–40.7) |
| Yes | 49.4 (34.8–122.7) | 80.7 (43.6–185.8) | 27.5 (10.2–37.1) | 39.1 (28.4–61.8) | 35.6 (16.5–45.5) | 30.5 (19.1–46.5) |
| p-value * | 0.552 | 0.891 | 0.992 | 0.565 | 0.396 | 0.704 |
| Major/Minor | ||||||
| Minor | 59.9 (37.3–128.8) | 66.6 (25.0–151.1) | 24.8 (11.9–39.5) | 33.7 (20.0–55.2) | 29.9 (18.3–50.4) | 24.8 (11.9–39.5) |
| Major | 69.2 (31.9–145.3) | 84.8 (38.2–205.7) | 22.5 (11.1–32.9) | 41.7 (22.4–61.2) | 30.3 (17.0–40.4) | 22.5 (11.1–32.9) |
| p-value * | 0.633 | 0.326 | 0.586 | 0.341 | 0.874 | 0.552 |
| Pre-Resection | Post-Resection | p * | |||
|---|---|---|---|---|---|
| Right Liver Lobe Mean (SD); Median | Left Liver Lobe Mean (SD); Median | In situ FLR Mean (SD); Median | Resected Liver Mean (SD); Median | ||
| UCP2—Intensity | 1.66 (± 0.48); 2 | 1.63 (± 0.53); 2 | 1.84 (±0.42); 2 | 2.13 (± 0.41); 2 | <0.001 |
| UCP2—Extensity | 78.1 (± 8.9); 80 | 81.6 (± 9.6); 80 | 85.2 (± 7.2); 90 | 87.8 (± 8.0); 90 | <0.001 |
| UCP2—Score | 131.7 (± 45.4); 150 | 134.0 (± 48.3); 150 | 158.7 (± 42.3); 170 | 187.8 (± 42.6); 180 | <0.001 |
| 4-HNE—Intensity | 1.23 (± 0.42); 1 | 1.28 (± 0.46); 1 | 1.59 (± 0.50); 2 | 1.91 (± 0.56); 2 | <0.001 |
| 4-HNE—Extensity | 71.5 (± 12.6); 72.5 | 74.8 (± 12.0); 77.5 | 79.9 (± 8.5); 80 | 84.1 (± 8.2); 85 | <0.001 |
| 4-HNE—Score | 89.3 (± 39.9); 75 | 97.3 (± 42.1); 80 | 128.4 (± 46.0); 150 | 161.3 (± 52.9); 170 | <0.001 |
| Pre-Res. UCP2 | Post-Res. UCP2 | Pre-Res. 4-HNE | Post-Res. 4-HNE | |
|---|---|---|---|---|
| Age > 60 years | ||||
| No | 134.2 (42.5) | 157.8 (39.7) | 85.9 (30.8) | 131.5 (47.3) |
| Yes | 132.4 (46.5) | 160.0 (45.8) | 101.6 (45.0) | 125 (45.4) |
| p-value * | 0.957 | 0.648 | 0.579 | 0.808 |
| Steatosis/fibrosis | ||||
| No | 131.8 (46.6) | 154.9 (41.9) | 88.6 (34.6) | 123.8 (47.3) |
| Yes | 137.7 (36.8) | 169.2 (43.4) | 108.1 (47.7) | 141.3 (40.7) |
| p-value * | 0.705 | 0.884 | 0.566 | 0.352 |
| Cholangiocarcinoma | ||||
| No | 131.0 (44.1) | 151.9 (41.2) | 90.5 (35.4) | 119.9 (45.3) |
| Yes | 143.1 (44.9) | 190.0 (33.8) | 106.7 (51.3) | 163.3 (30.8) |
| p-value * | 0.357 | 0.021 | 0.409 | 0.005 |
| Neoadjuvant CTX | ||||
| No | 135.0 (43.0) | 161.1 (40.6) | 97.9 (40.2) | 134.5 (44.1) |
| Yes | 123.6 (52.0) | 145.7 (52.2) | 68.9 (14.4) | 98.6 (43.2) |
| p-value * | 0.549 | 0.616 | 0.120 | 0.012 |
| Pringle maneuver | ||||
| No | 134.8 (41.1) | 159.2 (51.3) | 110.4 (49.2) | 146.9 (33.7) |
| Yes | 132.7 (45.8) | 158.5 (39.5) | 86.5 (31.7) | 121.1 (48.5) |
| p-value * | 0.843 | 0.354 | 0.305 | 0.297 |
| Intraop. transfusion | ||||
| No | 129.8 (44.2) | 162.3 (41.6) | 93.4 (39.7) | 131.0 (45.3) |
| Yes | 140.0 (44.3) | 151.3 (44.2) | 94.1 (38.3) | 123.4 (48.4) |
| p-value * | 0.444 | 0.351 | 0.973 | 0.437 |
| Major/minor | ||||
| Minor | 132.7 (46.2) | 160.7 (37.3) | 108.3 (33.5) | 123.2 (44.3) |
| Major | 133.6 (43.7) | 157.7 (44.9) | 86.7 (46.0) | 130.6 (47.2) |
| p-value * | 0.991 | 0.859 | 0.140 | 0.457 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Primavesi, F.; Senoner, T.; Schindler, S.; Nikolajevic, A.; Di Fazio, P.; Csukovich, G.; Eller, S.; Neumayer, B.; Anliker, M.; Braunwarth, E.; et al. The Interplay between Perioperative Oxidative Stress and Hepatic Dysfunction after Human Liver Resection: A Prospective Observational Pilot Study. Antioxidants 2024, 13, 590. https://doi.org/10.3390/antiox13050590
Primavesi F, Senoner T, Schindler S, Nikolajevic A, Di Fazio P, Csukovich G, Eller S, Neumayer B, Anliker M, Braunwarth E, et al. The Interplay between Perioperative Oxidative Stress and Hepatic Dysfunction after Human Liver Resection: A Prospective Observational Pilot Study. Antioxidants. 2024; 13(5):590. https://doi.org/10.3390/antiox13050590
Chicago/Turabian StylePrimavesi, Florian, Thomas Senoner, Sophie Schindler, Aleksandar Nikolajevic, Pietro Di Fazio, Georg Csukovich, Silvia Eller, Bettina Neumayer, Markus Anliker, Eva Braunwarth, and et al. 2024. "The Interplay between Perioperative Oxidative Stress and Hepatic Dysfunction after Human Liver Resection: A Prospective Observational Pilot Study" Antioxidants 13, no. 5: 590. https://doi.org/10.3390/antiox13050590








