Extent of Resection in Newly Diagnosed Glioblastoma: Impact of a Specialized Neuro-Oncology Care Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Imaging Protocol and EOR Volumetry
2.3. Statistical Analysis
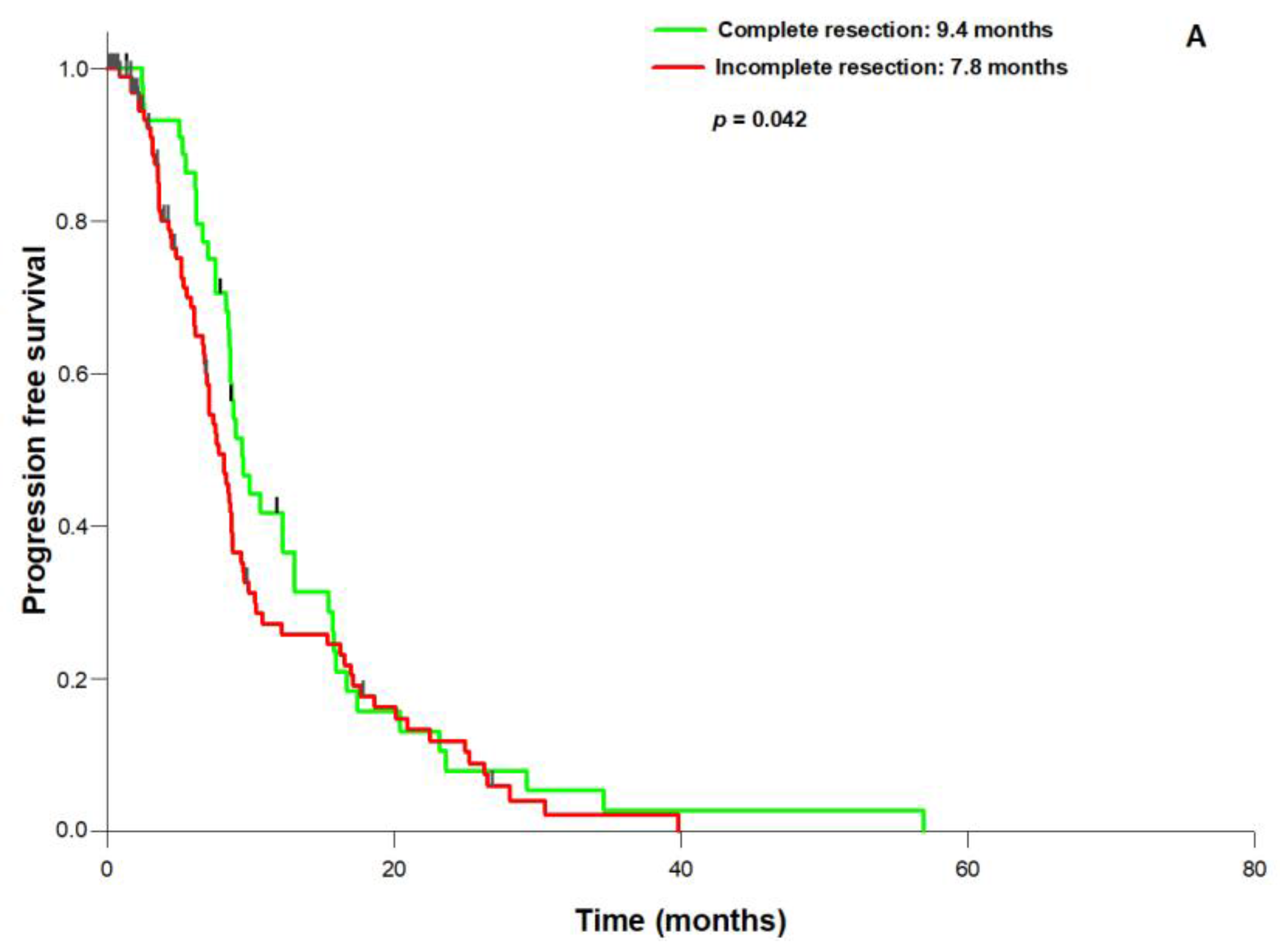
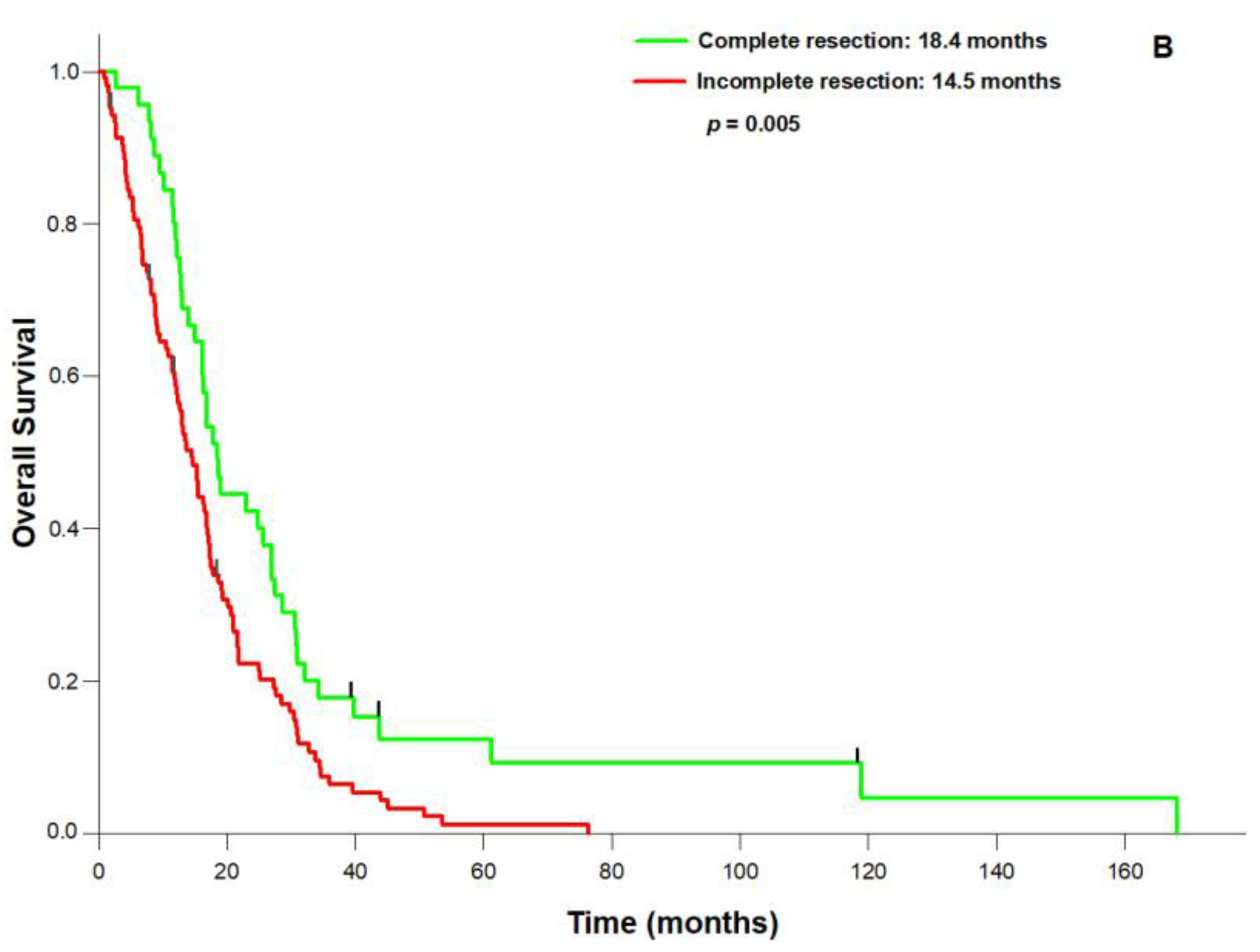
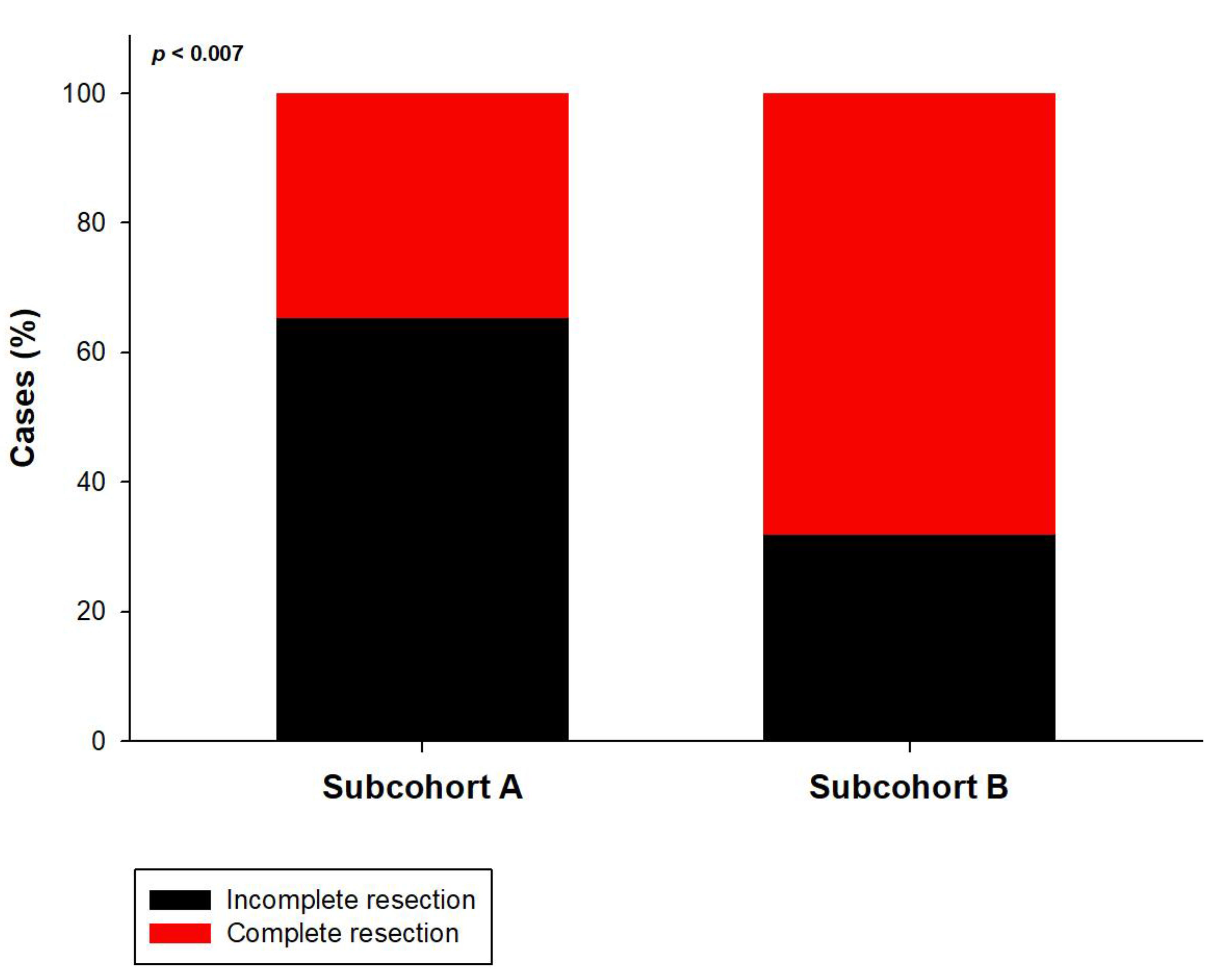
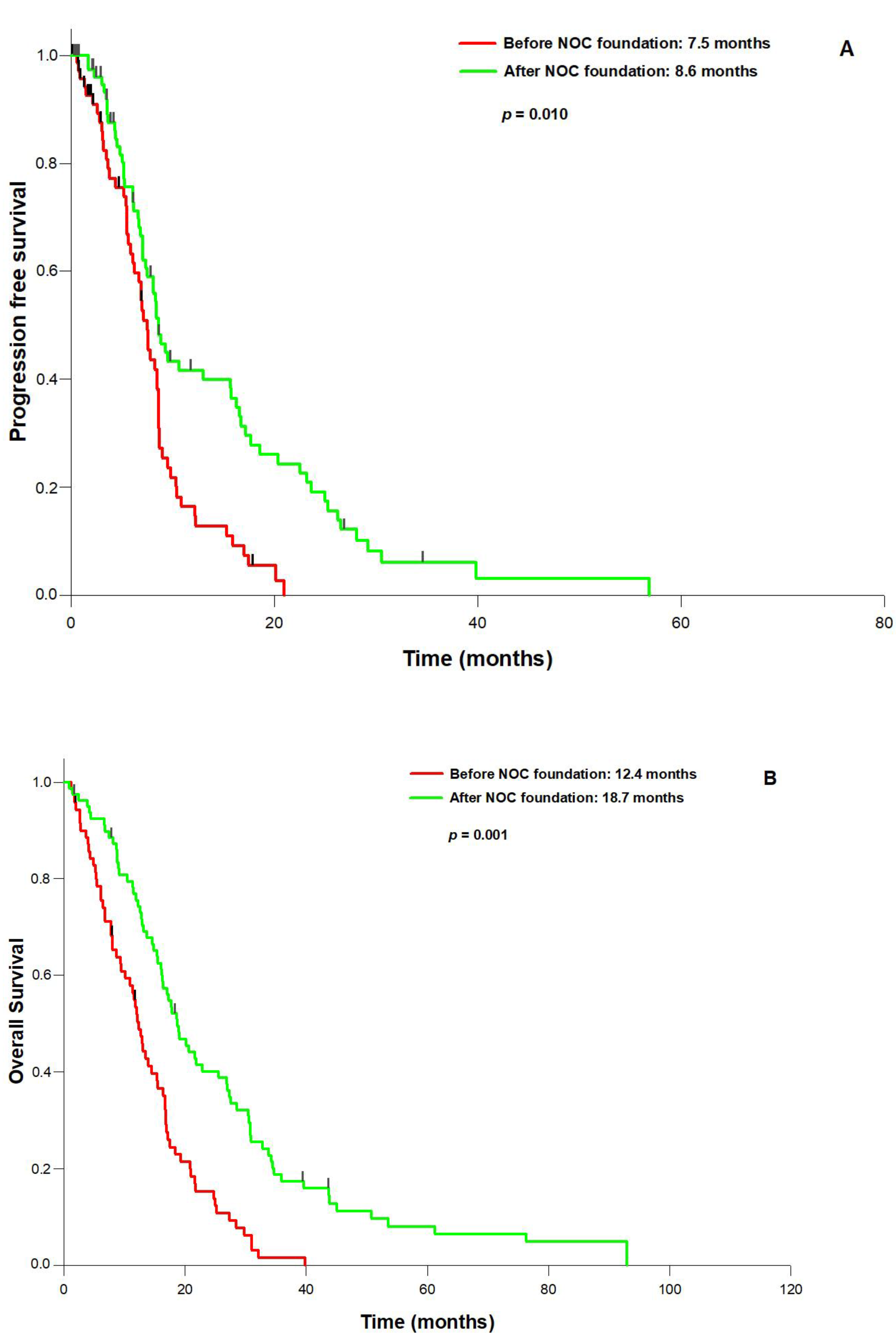
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ohgaki, H.; Kleihues, P. Epidemiology and etiology of gliomas. Acta Neuropathol. 2005, 109, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Wen, P.Y.; Kesari, S. Malignant gliomas in adults. N. Engl. J. Med. 2008, 359, 492–507. [Google Scholar] [CrossRef] [PubMed]
- Omuro, A.; DeAngelis, L.M. Glioblastoma and other malignant gliomas: A clinical review. JAMA 2013, 310, 1842–1850. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.J.; Brennan, M.C.; Li, M.; Church, E.W.; Brandmeir, N.J.; Rakszawski, K.L.; Patel, A.S.; Rizk, E.B.; Suki, D.; Sawaya, R.; et al. Association of the extent of resection with survival in glioblastoma: A systematic review and meta-analysis. JAMA Oncol. 2016, 2, 1460–1469. [Google Scholar] [CrossRef] [PubMed]
- Chaichana, K.L.; Jusue-Torres, I.; Navarro-Ramirez, R.; Raza, S.M.; Pascual-Gallego, M.; Ibrahim, A.; Hernandez-Hermann, M.; Gomez, L.; Ye, X.; Weingart, J.D.; et al. Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 2014, 16, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Sanai, N.; Polley, M.Y.; McDermott, M.W.; Parsa, A.T.; Berger, M.S. An extent of resection threshold for newly diagnosed glioblastomas. J. Neurosurg. 2011, 115, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Kreth, F.W.; Thon, N.; Simon, M.; Westphal, M.; Schackert, G.; Nikkhah, G.; Hentschel, B.; Reifenberger, G.; Pietsch, T.; Weller, M.; et al. Gross total but not incomplete resection of glioblastoma prolongs survival in the era of radiochemotherapy. Ann. Oncol. 2013, 24, 3117–3123. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.L.; van der Hoorn, A.; Larkin, T.J.; Boonzaier, N.R.; Matys, T.; Price, S.J. Extent of resection of peritumoral diffusion tensor imaging-detected abnormality as a predictor of survival in adult glioblastoma patients. J. Neurosurg. 2017, 126, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Eyupoglu, I.Y.; Hore, N.; Merkel, A.; Buslei, R.; Buchfelder, M.; Savaskan, N. Supra-complete surgery via dual intraoperative visualization approach (diva) prolongs patient survival in glioblastoma. Oncotarget 2016, 7, 25755–25768. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.M.; Suki, D.; Hess, K.; Sawaya, R. The influence of maximum safe resection of glioblastoma on survival in 1229 patients: Can we do better than gross-total resection? J. Neurosurg. 2015. [Google Scholar] [CrossRef] [PubMed]
- Gulati, S.; Jakola, A.S.; Nerland, U.S.; Weber, C.; Solheim, O. The risk of getting worse: Surgically acquired deficits, perioperative complications, and functional outcomes after primary resection of glioblastoma. World Neurosurg. 2011, 76, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Jakola, A.S.; Gulati, S.; Weber, C.; Unsgard, G.; Solheim, O. Postoperative deterioration in health related quality of life as predictor for survival in patients with glioblastoma: A prospective study. PLoS ONE 2011, 6, e28592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, U.A.; Bhavsar, A.; Asif, H.; Karabatsou, K.; Leggate, J.R.; Sofat, A.; Kamaly-Asl, I.D. Treatment by specialist surgical neurooncologists improves survival times for patients with malignant glioma. J. Neurosurg. 2015, 122, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Bunnell, C.A.; Weingart, S.N.; Swanson, S.; Mamon, H.J.; Shulman, L.N. Models of Multidisciplinary Cancer Care: Physician and Patient Perceptions in a Comprehensive Cancer Center. J. Oncol. Pract. Am. Soc. Clin. Oncol. 2010, 6, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Lamborn, K.R.; Chang, S.M.; Prados, M.D. Prognostic Factors for Survival of Patients with Glioblastoma: Recursive Partitioning Analysis. Neuro Oncol. 2004, 6, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Bianco, J.; Bastiancich, C.; Jankovski, A.; des Rieux, A.; Preat, V.; Danhier, F. On glioblastoma and the search for a cure: Where do we stand? Cell. Mol. Life Sci. 2017, 74, 2451–2466. [Google Scholar] [CrossRef] [PubMed]
- Diaz, R.J.; Ali, S.; Qadir, M.G.; De La Fuente, M.I.; Ivan, M.E.; Komotar, R.J. The role of bevacizumab in the treatment of glioblastoma. J. Neurooncol. 2017, 133, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Liu, F.; Liu, Z.; Tang, H.; Wu, H.; Gong, Q.; Chen, J. Immune checkpoint in glioblastoma: Promising and challenging. Front. Pharmacol. 2017, 8, 242. [Google Scholar] [CrossRef] [PubMed]
- Eyupoglu, I.Y.; Buchfelder, M.; Savaskan, N.E. Surgical resection of malignant gliomas-role in optimizing patient outcome. Nat. Rev. Neurol. 2013, 9, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Gramatzki, D.; Dehler, S.; Rushing, E.J.; Zaugg, K.; Hofer, S.; Yonekawa, Y.; Bertalanffy, H.; Valavanis, A.; Korol, D.; Rohrmann, S.; et al. Glioblastoma in the canton of zurich, switzerland revisited: 2005 to 2009. Cancer 2016, 122, 2206–2215. [Google Scholar] [CrossRef] [PubMed]
- Woehrer, A.; Bauchet, L.; Barnholtz-Sloan, J.S. Glioblastoma survival: Has it improved? Evidence from population-based studies. Curr. Opin. Neurol. 2014, 27, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Nava, F.; Tramacere, I.; Fittipaldo, A.; Bruzzone, M.G.; Dimeco, F.; Fariselli, L.; Finocchiaro, G.; Pollo, B.; Salmaggi, A.; Silvani, A.; et al. Survival effect of first- and second-line treatments for patients with primary glioblastoma: A cohort study from a prospective registry, 1997–2010. Neuro Oncol. 2014, 16, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Koshy, M.; Villano, J.L.; Dolecek, T.A.; Howard, A.; Mahmood, U.; Chmura, S.J.; Weichselbaum, R.R.; McCarthy, B.J. Improved survival time trends for glioblastoma using the seer 17 population-based registries. J. Neurooncol. 2012, 107, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Leroy, H.A.; Vermandel, M.; Lejeune, J.P.; Mordon, S.; Reyns, N. Fluorescence guided resection and glioblastoma in 2015: A review. Lasers Surg. Med. 2015, 47, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Schucht, P.; Seidel, K.; Beck, J.; Murek, M.; Jilch, A.; Wiest, R.; Fung, C.; Raabe, A. Intraoperative Monopolar Mapping During 5-Ala-Guided Resections of Glioblastomas Adjacent to Motor Eloquent Areas: Evaluation of Resection Rates and Neurological Outcome. Neurosurg. Focus 2014, 37, E16. [Google Scholar] [CrossRef] [PubMed]
- Solheim, O.; Gulati, S.; Jakola, A.S. Glioblastoma resection: In search of a threshold between worthwhile and futile. Neuro Oncol. 2014, 16, 610–611. [Google Scholar] [CrossRef] [PubMed]
| Parameter | (Number (%)) |
|---|---|
| n | 149 |
| Sex (f/m) | 67/82 (44.9/55.1) |
| Age (years, mean) | 61.8 (range: 26.7–87.8) |
| Preoperative KPS (%, median) | 80 (range: 20–100) |
| Preoperative MRC-NPS (points, median) | 2 (range: 1–5) |
| MGMT promoter status | Methylated: 50 (33.6) |
| Unmethylated: 68 (45.6) | |
| Unknown: 31 (20.8) | |
| IDH1 status | Wild type: 144 (96.6) |
| Mutated: 5 (3.4) | |
| Postsurgical treatment | |
| Stupp | 106 (71.1) |
| Radiation only | 15 (10.1) |
| Chemotherapy only | 16 (10.7) |
| No treatment | 12 (8.1) |
| Parameter | Complete Resection (Number (%)) | Incomplete Resection (Number (%)) | p |
|---|---|---|---|
| n | 74 (49.7) | 75 (50.3) | |
| Sex (f/m) | 34/40 (46.0/54.0) | 33/42 (44.0/56.0) | 0.941 |
| Age (years, mean) | 61.7 (range: 32.9–80.1) | 61.8 (range: 26.7–87.8) | 0.939 |
| Preoperative KPS (%, median) | 90 (range: 60–100) | 80 (range: 20–100) | 0.073 |
| Preoperative MRC-NPS (points, median) | 2 (range: 1–3) | 2 (range: 1–5) | 0.219 |
| MGMT: | 0.746 | ||
| Methylated | 24 (32.4) | 26 (34.7) | |
| Unmethylated | 34 (45.9) | 34 (45.3) | |
| Unknown | 16 (21.6) | 15 (20.0) | |
| IDH1 status: | 0.988 | ||
| Wildtype | 71 (97.3) | 73(97.3) | |
| Mutated | 3 (2.7) | 2 (2.7) | |
| Postsurgical treatment: | 0.782 | ||
| Stupp | 55 (74.3) | 51 (68.0) | |
| Radiation only | 6 (8.1) | 9 (12.0) | |
| Chemotherapy only | 8 (10.8) | 8 (10.7) | |
| No treatment | 5 (6.8) | 7(9.3) |
| Parameter | Hazard Ratio | 95% CI | p | |
|---|---|---|---|---|
| Age | 1.032 | 1.014 | 1.050 | 0.001 |
| NOC foundation | 0.697 | 0.482 | 1.008 | 0.015 |
| Preoperative KPS (>/<70%) | 0.971 | 0.957 | 0.988 | 0.001 |
| MGMT | 1.47 | 1.150 | 1.891 | 0.002 |
| Resection status: (complete vs. incomplete) | 0.981 | 0.964 | 0.998 | 0.032 |
| Parameter | Group A (Number (%)) | Group B (Number (%)) | p |
|---|---|---|---|
| n | 49 (32.9) | 100 (67.1) | |
| Sex (f/m) | 21/28 (42.9/57.1) | 46/54 (46.0/54.0) | 0.717 |
| Age (years, mean) | 62.4 (range: 32.1–81.0) | 61.5 (range: 26.7–87.8) | 0.647 |
| Preoperative KPS (%, median) | 80 (range: 40–100) | 80 (range: 20–100) | 0.658 |
| Preoperative MRC-NPS (points, median) | 2 (range: 1–5) | 2 (range: 1–4) | 0.68 |
| MGMT: | 0.431 | ||
| Methylated | 18 (36.7) | 32 (32.0) | |
| Unmethylated | 20 (40.9) | 48 (48.0) | |
| Unknown | 11 (22.4) | 20 (20.0) | |
| IDH1 status: | 0.889 | ||
| Wildtype | 47 (95.9) | 97 (97.0) | |
| Mutated | 2 (4.1) | 3 (3.0) | |
| Postsurgical treatment: | 0.195 | ||
| Stupp | 30 (61.2) | 76 (76.0) | |
| Radiation only | 8 (16.3) | 7 (7.0) | |
| Chemotherapy only | 4 (8.2) | 12 (12.0) | |
| No treatment | 5 (10.2) | 7 (7.0) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haj, A.; Doenitz, C.; Schebesch, K.-M.; Ehrensberger, D.; Hau, P.; Putnik, K.; Riemenschneider, M.J.; Wendl, C.; Gerken, M.; Pukrop, T.; et al. Extent of Resection in Newly Diagnosed Glioblastoma: Impact of a Specialized Neuro-Oncology Care Center. Brain Sci. 2018, 8, 5. https://doi.org/10.3390/brainsci8010005
Haj A, Doenitz C, Schebesch K-M, Ehrensberger D, Hau P, Putnik K, Riemenschneider MJ, Wendl C, Gerken M, Pukrop T, et al. Extent of Resection in Newly Diagnosed Glioblastoma: Impact of a Specialized Neuro-Oncology Care Center. Brain Sciences. 2018; 8(1):5. https://doi.org/10.3390/brainsci8010005
Chicago/Turabian StyleHaj, Amer, Christian Doenitz, Karl-Michael Schebesch, Denise Ehrensberger, Peter Hau, Kurt Putnik, Markus J. Riemenschneider, Christina Wendl, Michael Gerken, Tobias Pukrop, and et al. 2018. "Extent of Resection in Newly Diagnosed Glioblastoma: Impact of a Specialized Neuro-Oncology Care Center" Brain Sciences 8, no. 1: 5. https://doi.org/10.3390/brainsci8010005





