Current Knowledge in Ultrasound-Based Liver Elastography of Pediatric Patients
Abstract
:Featured Application
Abstract
1. Introduction
2. Possible Indications for Shear Wave Elastography (SWE) Measurement
3. Elastographic Methods
3.1. Transient Elastography (TE)
3.1.1. TE in Healthy Children
3.1.2. TE in Non-Alcoholic Fatty Liver Disease (NAFLD)
3.1.3. Correlation with Fibrosis Stage and Different Etiologies
3.2. Point SWE (pSWE)
3.2.1. Liver Fibrosis
3.2.2. Values in Obesity
3.2.3. Liver Disease Associated with Cystic Fibrosis (CFLD)
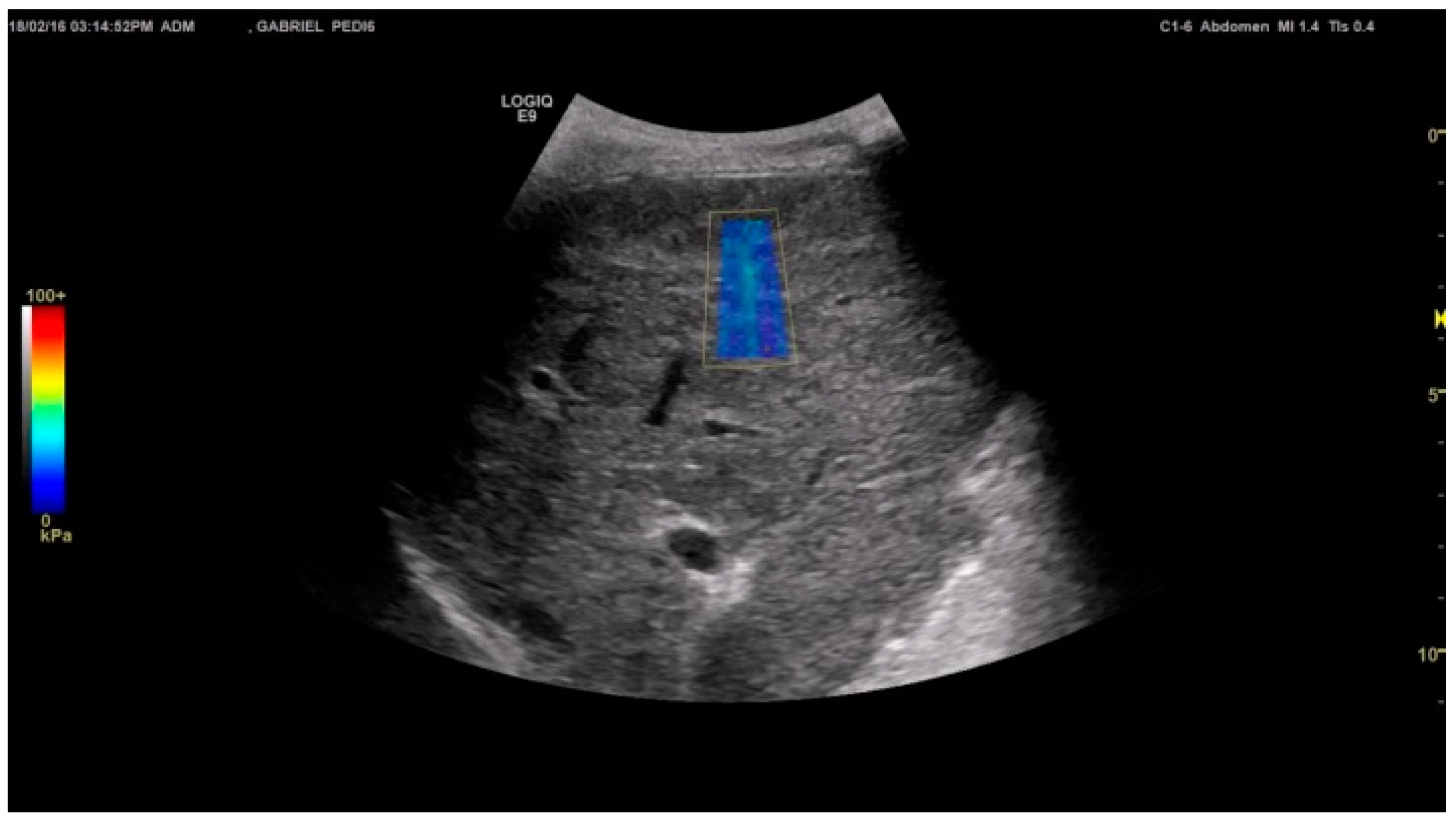
3.3. Two-Dimensional Shear Wave Elastography (2D-SWE)
3.3.1. Technical Success Rates of Liver Stiffness Estimates
3.3.2. Reproducibility and Variability of Liver Stiffness Estimates
3.3.3. Liver Stiffness Estimates in Healthy Controls
3.3.4. Number of Measurements Needed
3.3.5. Pediatric Patients with NAFLD
3.3.6. Liver Fibrosis in Biliary Atresia (BA) Patients
3.3.7. Intrahepatic Portal Hypertension
3.3.8. Focal Liver Lesions
3.4. Strain Imaging (Real-Time Elastography (RTE))
4. Comparison of TE, pSWE and 2D-SWE
5. What Is the Benefit of SWE in Children?
5.1. What Is Best in Children: TE, pSWE or 2D-SWE and Why?
5.2. Scores in Fatty Liver Disease and Fibrosis: Are They Better than SWE?
6. Limits of Liver Elastography
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (long version). Ultraschall Med. 2017, 38, e16–e47. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (short version). Ultraschall Med. 2017, 38, 377–394. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Sirli, R.; Ferraioli, G.; Sporea, I.; Chiorean, L.; Cui, X.; Fan, M.; Wang, W.P.; Gilja, O.H.; Sidhu, P.S.; et al. Shear wave elastography of the liver—Review on normal values. Z. Gastroenterol. 2017, 55, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Bamber, J.; Cosgrove, D.; Dietrich, C.F.; Fromageau, J.; Bojunga, J.; Calliada, F.; Cantisani, V.; Correas, J.M.; D’Onofrio, M.; Drakonaki, E.E.; et al. Efsumb guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med. 2013, 34, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, D.; Piscaglia, F.; Bamber, J.; Bojunga, J.; Correas, J.M.; Gilja, O.H.; Klauser, A.S.; Sporea, I.; Calliada, F.; Cantisani, V.; et al. Efsumb guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013, 34, 238–253. [Google Scholar] [PubMed]
- Shiina, T.; Nightingale, K.R.; Palmeri, M.L.; Hall, T.J.; Bamber, J.C.; Barr, R.G.; Castera, L.; Choi, B.I.; Chou, Y.H.; Cosgrove, D.; et al. Wfumb guidelines and recommendations for clinical use of ultrasound elastography: Part 1: Basic principles and terminology. Ultrasound Med. Biol. 2015, 41, 1126–1147. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, G.; Filice, C.; Castera, L.; Choi, B.I.; Sporea, I.; Wilson, S.R.; Cosgrove, D.; Dietrich, C.F.; Amy, D.; Bamber, J.C.; et al. Wfumb guidelines and recommendations for clinical use of ultrasound elastography: Part 3: Liver. Ultrasound Med. Biol. 2015, 41, 1161–1179. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, G.; Calcaterra, V.; Lissandrin, R.; Guazzotti, M.; Maiocchi, L.; Tinelli, C.; De Silvestri, A.; Regalbuto, C.; Pelizzo, G.; Larizza, D.; et al. Noninvasive assessment of liver steatosis in children: The clinical value of controlled attenuation parameter. BMC Gastroenterol. 2017, 17, 61. [Google Scholar] [CrossRef] [PubMed]
- Kamble, R.; Sodhi, K.S.; Thapa, B.R.; Saxena, A.K.; Bhatia, A.; Dayal, D.; Khandelwal, N. Liver acoustic radiation force impulse (ARFI) in childhood obesity: Comparison and correlation with biochemical markers. J. Ultrasound 2017, 20, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Lodwick, D.; Dienhart, M.; Cooper, J.N.; Fung, B.; Lopez, J.; Smith, S.; Warren, P.; Balint, J.; Minneci, P.C. A pilot study of ultrasound elastography as a non-invasive method to monitor liver disease in children with short bowel syndrome. J. Pediatr. Surg. 2017, 52, 962–965. [Google Scholar] [CrossRef] [PubMed]
- Raizner, A.; Shillingford, N.; Mitchell, P.D.; Harney, S.; Raza, R.; Serino, J.; Jonas, M.M.; Lee, C.K. Hepatic inflammation may influence liver stiffness measurements by transient elastography in children and young adults. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Garcovich, M.; Veraldi, S.; Di Stasio, E.; Zocco, M.A.; Monti, L.; Toma, P.; Pompili, M.; Gasbarrini, A.; Nobili, V. Liver stiffness in pediatric patients with fatty liver disease: Diagnostic accuracy and reproducibility of shear-wave elastography. Radiology 2017, 283, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.; Groth, M.; Petersen, K.U.; Hammel, A.; Brinkert, F.; Grabhorn, E.; Weidemann, S.A.; Busch, J.; Adam, G.; Herrmann, J. Hepatic shear wave elastography in children under free-breathing and breath-hold conditions. Eur. Radiol. 2017, 27, 5337–5343. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, M.B.; Bilgici, M.C.; Eren, E.; Caltepe, G.; Yilmaz, G.; Kara, C.; Gun, S. Role of point shear wave elastography in the determination of the severity of fibrosis in pediatric liver diseases with pathologic correlations. J. Ultrasound Med. 2017, 36, 2337–2344. [Google Scholar] [CrossRef] [PubMed]
- Phelps, A.; Ramachandran, R.; Courtier, J.; Perito, E.; Rosenthal, P.; MacKenzie, J.D. Ultrasound elastography: Is there a shear wave speed cutoff for pediatric liver fibrosis and inflammation? Clin. Imaging 2017, 41, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.M.; Kim, S.Y.; Kim, K.M.; Oh, S.H.; Ko, G.Y.; Park, Y.; Lee, J.S.; Jung, A.Y.; Cho, Y.A. Liver stiffness measured by shear-wave elastography for evaluating intrahepatic portal hypertension in children. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 892–897. [Google Scholar] [CrossRef] [PubMed]
- Behairy, B.S.; Sira, M.M.; Zalata, K.R.; Salama, E.S.E.; Abd-Allah, M.A. Transient elastography compared to liver biopsy and morphometry for predicting fibrosis in pediatric chronic liver disease: Does etiology matter? World J. Gastroenterol. 2016, 22, 4238–4249. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Schreiber, R.A.; Human, D.G.; Potts, J.E.; Guttman, O.R. Assessment of liver stiffness in pediatric fontan patients using transient elastography. Can. J. Gastroenterol. Hepatol. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Liao, B.; Zhong, Z.; Zheng, Y.; Liu, B.; Shan, Q.; Xie, X.; Zhou, L. Supersonic shearwave elastography in the assessment of liver fibrosis for postoperative patients with biliary atresia. Sci. Rep. 2016, 6, 31057. [Google Scholar] [CrossRef] [PubMed]
- Desai, N.K.; Harney, S.; Raza, R.; Al-Ibraheemi, A.; Shillingford, N.; Mitchell, P.D.; Jonas, M.M. Comparison of controlled attenuation parameter and liver biopsy to assess hepatic steatosis in pediatric patients. J. Pediatr. 2016, 173, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Ghaffar, T.A.; Youssef, A.; Zalata, K.; ElSharkawy, A.; Mowafy, M.; Wanis, A.A.A.; Esmat, G. Noninvasive assessment of liver fibrosis in egyptian children with chronic liver diseases. Curr. Pediatr. Res. 2016, 20, 57–63. [Google Scholar]
- Hattapoglu, S.; Goya, C.; Arslan, S.; Alan, B.; Ekici, F.; Tekbas, G.; Yildiz, I.; Hamidi, C. Evaluation of postoperative undescended testicles using point shear wave elastography in children. Ultrasonics 2016, 72, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Tokuhara, D.; Cho, Y.; Shintaku, H. Transient elastography-based liver stiffness age-dependently increases in children. PLoS ONE 2016, 11, e0166683. [Google Scholar] [CrossRef] [PubMed]
- Belei, O.; Sporea, I.; Gradinaru-Tascau, O.; Olariu, L.; Popescu, A.; Simedrea, I.; Marginean, O. Comparison of three ultrasound based elastographic techniques in children and adolescents with chronic diffuse liver diseases. Med. Ultrason. 2016, 18, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Franchi-Abella, S.; Corno, L.; Gonzales, E.; Antoni, G.; Fabre, M.; Ducot, B.; Pariente, D.; Gennisson, J.L.; Tanter, M.; Correas, J.M. Feasibility and diagnostic accuracy of supersonic shear-wave elastography for the assessment of liver stiffness and liver fibrosis in children: A pilot study of 96 patients. Radiology 2016, 278, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Gersak, M.M.; Sorantin, E.; Windhaber, J.; Dudea, S.M.; Riccabona, M. The influence of acute physical effort on liver stiffness estimation using virtual touch quantification (VTQ). Preliminary results. Med. Ultrason. 2016, 18, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Trout, A.T.; Dillman, J.R.; Xanthakos, S.; Kohli, R.; Sprague, G.; Serai, S.; Mahley, A.D.; Podberesky, D.J. Prospective assessment of correlation between US acoustic radiation force impulse and MR elastography in a pediatric population: Dispersion of US shear-wave speed measurement matters. Radiology 2016, 281, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.P.; De Vito, R.; Mosca, A.; Alisi, A.; Armstrong, M.J.; Raponi, M.; Baumann, U.; Nobili, V. Portal inflammation is independently associated with fibrosis and metabolic syndrome in pediatric nonalcoholic fatty liver disease. Hepatology 2016, 63, 745–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanquinet, S.; Courvoisier, D.S.; Rougemont, A.L.; Wildhaber, B.E.; Merlini, L.; McLin, V.A.; Anooshiravani, M. Acoustic radiation force impulse sonography in assessing children with biliary atresia for liver transplantation. Pediatr. Radiol. 2016, 46, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
- Canas, T.; Macia, A.; Munoz-Codoceo, R.A.; Fontanilla, T.; Gonzalez-Rios, P.; Miralles, M.; Gomez-Mardones, G. Hepatic and splenic acoustic radiation force impulse shear wave velocity elastography in children with liver disease associated with cystic fibrosis. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Chichakli, M.; Hirche, T.O.; Bargon, J.; Leitzmann, P.; Wagner, T.O.; Lembcke, B. Sonographic findings of the hepatobiliary-pancreatic system in adult patients with cystic fibrosis. J. Ultrasound Med. 2002, 21, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Hanquinet, S.; Courvoisier, D.S.; Rougemont, A.L.; Dhouib, A.; Rubbia-Brandt, L.; Wildhaber, B.E.; Merlini, L.; McLin, V.A.; Anooshiravani, M. Contribution of acoustic radiation force impulse (ARFI) elastography to the ultrasound diagnosis of biliary atresia. Pediatr. Radiol. 2015, 45, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Lorentzen, T.; Sidhu, P.S.; Jenssen, C.; Gilja, O.H.; Piscaglia, F. An introduction to the EFSUMB guidelines on interventional ultrasound (INVUS). Ultraschall Med. 2015, 36, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Lorentzen, T.; Nolsoe, C.P.; Ewertsen, C.; Nielsen, M.B.; Leen, E.; Havre, R.F.; Gritzmann, N.; Brkljacic, B.; Nurnberg, D.; Kabaalioglu, A.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part I. General aspects (long version). Ultraschall Med. 2015, 36, E1–E14. [Google Scholar] [PubMed]
- Lorentzen, T.; Nolsoe, C.P.; Ewertsen, C.; Nielsen, M.B.; Leen, E.; Havre, R.F.; Gritzmann, N.; Brkljacic, B.; Nurnberg, D.; Kabaalioglu, A.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part I. General aspects (short version). Ultraschall Med. 2015, 36, 464–472. [Google Scholar] [PubMed]
- Sidhu, P.S.; Brabrand, K.; Cantisani, V.; Correas, J.M.; Cui, X.W.; D’Onofrio, M.; Essig, M.; Freeman, S.; Gilja, O.H.; Gritzmann, N.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part II. Diagnostic ultrasound-guided interventional procedures (long version). Ultraschall Med. 2015, 36, E15–E35. [Google Scholar] [PubMed]
- Sidhu, P.S.; Brabrand, K.; Cantisani, V.; Correas, J.M.; Cui, X.W.; D’Onofrio, M.; Essig, M.; Freeman, S.; Gilja, O.H.; Gritzmann, N.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part II. Diagnostic ultrasound-guided interventional procedures (short version). Ultraschall Med. 2015, 36, 566–580. [Google Scholar] [PubMed]
- Dietrich, C.F.; Lorentzen, T.; Appelbaum, L.; Buscarini, E.; Cantisani, V.; Correas, J.M.; Cui, X.W.; D’Onofrio, M.; Gilja, O.H.; Hocke, M.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part III—abdominal treatment procedures (short version). Ultraschall Med. 2016, 37, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Lorentzen, T.; Appelbaum, L.; Buscarini, E.; Cantisani, V.; Correas, J.M.; Cui, X.W.; D’Onofrio, M.; Gilja, O.H.; Hocke, M.; et al. EFSUMB guidelines on interventional ultrasound (INVUS), part III—abdominal treatment procedures (long version). Ultraschall Med. 2016, 37, E1–E32. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Nuernberg, D. Interventional Ultrasound; Thieme: Stuttgart, Germany, 2014. [Google Scholar]
- Dietrich, C.F.; Nuernberg, D. Interventioneller Ultraschall. Lehrbuch und Atlas für die Interventionelle Sonographie; Thieme Verlag: Stuttgart, Germany, 2011. [Google Scholar]
- Nobili, V.; Vizzutti, F.; Arena, U.; Abraldes, J.G.; Marra, F.; Pietrobattista, A.; Fruhwirth, R.; Marcellini, M.; Pinzani, M. Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 2008, 48, 442–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kutty, S.S.; Zhang, M.; Danford, D.A.; Hasan, R.; Duncan, K.F.; Kugler, J.D.; Quiros-Tejeira, R.E.; Kutty, S. Hepatic stiffness in the bidirectional cavopulmonary circulation: The liver adult-pediatric-congenital-heart-disease dysfunction study group. J. Thorac. Cardiovasc. Surg. 2016, 151, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Berzigotti, A.; Ferraioli, G.; Bota, S.; Gilja, O.H.; Dietrich, C.F. Novel ultrasound-based methods to assess liver disease: The game has just begun. Dig. Liver Dis. 2018, 50, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Sandrin, L.; Fourquet, B.; Hasquenoph, J.M.; Yon, S.; Fournier, C.; Mal, F.; Christidis, C.; Ziol, M.; Poulet, B.; Kazemi, F.; et al. Transient elastography: A new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med. Biol. 2003, 29, 1705–1713. [Google Scholar] [CrossRef] [PubMed]
- Sigrist, R.M.S.; Liau, J.; Kaffas, A.E.; Chammas, M.C.; Willmann, J.K. Ultrasound elastography: Review of techniques and clinical applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef] [PubMed]
- Tsochatzis, E.A.; Gurusamy, K.S.; Ntaoula, S.; Cholongitas, E.; Davidson, B.R.; Burroughs, A.K. Elastography for the diagnosis of severity of fibrosis in chronic liver disease: A meta-analysis of diagnostic accuracy. J. Hepatol. 2011, 54, 650–659. [Google Scholar] [CrossRef] [PubMed]
- Engelmann, G.; Gebhardt, C.; Wenning, D.; Wuhl, E.; Hoffmann, G.F.; Selmi, B.; Grulich-Henn, J.; Schenk, J.P.; Teufel, U. Feasibility study and control values of transient elastography in healthy children. Eur. J. Pediatr. 2012, 171, 353–360. [Google Scholar] [CrossRef] [PubMed]
- De Ledinghen, V.; Le Bail, B.; Rebouissoux, L.; Fournier, C.; Foucher, J.; Miette, V.; Castera, L.; Sandrin, L.; Merrouche, W.; Lavrand, F.; et al. Liver stiffness measurement in children using fibroscan: Feasibility study and comparison with fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J. Pediatr. Gastroenterol. Nutr. 2007, 45, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, I.; Streckenbach, C.; Dingemann, C.; Pfister, E.D.; di Nanni, A.; Zapf, A.; Baumann, U. Application and limitations of transient liver elastography in children. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Lewindon, P.J.; Balouch, F.; Pereira, T.N.; Puertolas-Lopez, M.V.; Noble, C.; Wixey, J.A.; Ramm, G.A. Transient liver elastography in unsedated control children: Impact of age and intercurrent illness. J. Paediatr. Child Health 2016, 52, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kang, Y.; Lee, M.J.; Kim, M.J.; Han, S.J.; Koh, H. Points to be considered when applying fibroscan s probe in children with biliary atresia. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Alkhouri, N.; Sedki, E.; Alisi, A.; Lopez, R.; Pinzani, M.; Feldstein, A.E.; Nobili, V. Combined paediatric nafld fibrosis index and transient elastography to predict clinically significant fibrosis in children with fatty liver disease. Liver Int. 2013, 33, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Behrens, A.; Labenz, J.; Schuler, A.; Schroder, W.; Runzi, M.; Steinmann, R.U.; de Mas, C.R.; Kreuzmayr, A.; Barth, K.; Bahr, M.J.; et al. [how safe is sedation in gastrointestinal endoscopy? A multicentre analysis of 388,404 endoscopies and analysis of data from prospective registries of complications managed by members of the working group of leading hospital gastroenterologists (ALGK)]. Z. Gastroenterol. 2013, 51, 432–436. [Google Scholar] [PubMed]
- Bernatik, T.; Schuler, A.; Kunze, G.; Mauch, M.; Dietrich, C.F.; Dirks, K.; Pachmann, C.; Borner, N.; Fellermann, K.; Menzel, J.; et al. Benefit of contrast-enhanced ultrasound (CEUS) in the follow-up care of patients with colon cancer: A prospective multicenter study. Ultraschall Med. 2015, 36, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; Perez-Atayde, A.R.; Mitchell, P.D.; Raza, R.; Afdhal, N.H.; Jonas, M.M. Serum biomarkers and transient elastography as predictors of advanced liver fibrosis in a united states cohort: The Boston children’s hospital experience. J. Pediatr. 2013, 163, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Chongsrisawat, V.; Vejapipat, P.; Siripon, N.; Poovorawan, Y. Transient elastography for predicting esophageal/gastric varices in children with biliary atresia. BMC Gastroenterol. 2011, 11, 41. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.S.; Youssfi, M.; Patel, M.; Hu, H.H.; Shaibi, G.Q.; Towbin, R.B. Shear-wave ultrasound elastography of the liver in normal-weight and obese children. Acta Radiol. 2017, 58, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Eiler, J.; Kleinholdermann, U.; Albers, D.; Dahms, J.; Hermann, F.; Behrens, C.; Luedemann, M.; Klingmueller, V.; Alzen, G.F. Standard value of ultrasound elastography using acoustic radiation force impulse imaging (ARFI) in healthy liver tissue of children and adolescents. Ultraschall Med. 2012, 33, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Hanquinet, S.; Courvoisier, D.; Kanavaki, A.; Dhouib, A.; Anooshiravani, M. Acoustic radiation force impulse imaging-normal values of liver stiffness in healthy children. Pediatr. Radiol. 2013, 43, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Matos, H.; Trindade, A.; Noruegas, M.J. Acoustic radiation force impulse imaging in paediatric patients: Normal liver values. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Fontanilla, T.; Canas, T.; Macia, A.; Alfageme, M.; Gutierrez Junquera, C.; Malalana, A.; Luz Cilleruelo, M.; Roman, E.; Miralles, M. Normal values of liver shear wave velocity in healthy children assessed by acoustic radiation force impulse imaging using a convex probe and a linear probe. Ultrasound Med. Biol. 2014, 40, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Marginean, C.O.; Marginean, C. Elastographic assessment of liver fibrosis in children: A prospective single center experience. Eur. J. Radiol. 2012, 81, e870–e874. [Google Scholar] [CrossRef] [PubMed]
- Pinto, J.; Matos, H.; Nobre, S.; Cipriano, M.A.; Marques, M.; Pereira, J.M.; Goncalves, I.; Noruegas, M.J. Comparison of acoustic radiation force impulse/serum noninvasive markers for fibrosis prediction in liver transplant. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Tomita, H.; Hoshino, K.; Fuchimoto, Y.; Ebinuma, H.; Ohkuma, K.; Tanami, Y.; Du, W.; Masugi, Y.; Shimojima, N.; Fujino, A.; et al. Acoustic radiation force impulse imaging for assessing graft fibrosis after pediatric living donor liver transplantation: A pilot study. Liver Transplant. 2013, 19, 1202–1213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhyani, M.; Gee, M.S.; Misdraji, J.; Israel, E.J.; Shah, U.; Samir, A.E. Feasibility study for assessing liver fibrosis in paediatric and adolescent patients using real-time shear wave elastography. J. Med. Imaging Radiat. Oncol. 2015, 59, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Roensch, M. Lebergewebecharakterisierung Mittels Acoustic Radiation Force Impulse-Elastographie und Zone Speed Index im Kindes- und Jugendalter. Ph.D. Thesis, Martin-Luther-Universität Halle-Wittenberg, Halle, Germany, 2017. [Google Scholar]
- Weinitschke, K. Vergleichswerterstellung für die Acoustic-Radiation-Force-Impulse-Elastographie der Leber im Kindes- und Jugendalter. Ph.D. Thesis, Martin-Luther-Universität Halle-Wittenberg, Halle, Germany, 2015. [Google Scholar]
- Dietrich, C.F.; Nuernberg, D. Interventional Ultrasound. A Practical Guide and Atlas; Thieme: Stuttgart, Germany, 2014. [Google Scholar]
- Bargon, J.; Stein, J.; Dietrich, C.F.; Muller, U.; Caspary, W.F.; Wagner, T.O. [Gastrointestinal complications of adult patients with cystic fibrosis]. Z. Gastroenterol. 1999, 37, 739–749. [Google Scholar] [PubMed]
- Kim, J.R.; Suh, C.H.; Yoon, H.M.; Lee, J.S.; Cho, Y.A.; Jung, A.Y. The diagnostic performance of shear-wave elastography for liver fibrosis in children and adolescents: A systematic review and diagnostic meta-analysis. Eur. Radiol. 2018, 28, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.J.; Kim, M.J.; Kim, H.Y.; Roh, Y.H.; Lee, M.J. Optimal acquisition number for hepatic shear wave velocity measurements in children. PLoS ONE 2016, 11, e0168758. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.Y.; Jiang, H.; Shan, Q.Y.; Chen, D.; Lin, X.N.; Liu, B.X.; Xie, X.Y. Liver stiffness measurements with supersonic shear wave elastography in the diagnosis of biliary atresia: A comparative study with grey-scale us. Eur. Radiol. 2017, 27, 3474–3484. [Google Scholar] [CrossRef] [PubMed]
- Hong, E.K.; Choi, Y.H.; Cheon, J.E.; Kim, W.S.; Kim, I.O.; Kang, S.Y. Accurate measurements of liver stiffness using shear wave elastography in children and young adults and the role of the stability index. Ultrasonography 2017. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.P.; Xu, Y.; Cao, J.; Mao, F.; Dietrich, C.F. Point shear wave speed measurement in differentiating benign and malignant focal liver lesions. Med. Ultrason. 2017, 19, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Averkiou, M.; Nielsen, M.B.; Barr, R.G.; Burns, P.N.; Calliada, F.; Cantisani, V.; Choi, B.; Chammas, M.C.; Clevert, D.A.; et al. How to perform contrast-enhanced ultrasound (CEUS). Ultrasound Int. Open 2018, 4, E2–E15. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, P.S.; Cantisani, V.; Deganello, A.; Dietrich, C.F.; Duran, C.; Franke, D.; Harkanyi, Z.; Kosiak, W.; Miele, V.; Ntoulia, A.; et al. Role of contrast-enhanced ultrasound (CEUS) in paediatric practice: An EFSUMB position statement. Ultraschall Med. 2017, 38, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.P.; Mao, F.; Fan, M.; Ignee, A.; Serra, C.; Sparchez, Z.; Sporea, I.; Braden, B.; Dietrich, C.F. Contrast enhanced ultrasound features of hepatic cystadenoma and hepatic cystadenocarcinoma. Scand. J. Gastroenterol. 2017, 52, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Dong, Y.; Froehlich, E.; Hocke, M. Dynamic contrast-enhanced endoscopic ultrasound: A quantification method. Endosc. Ultrasound 2017, 6, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.P.; Cantisani, V.; D’Onofrio, M.; Ignee, A.; Mulazzani, L.; Saftoiu, A.; Sparchez, Z.; Sporea, I.; Dietrich, C.F. Contrast-enhanced ultrasound of histologically proven hepatic epithelioid hemangioendothelioma. World J. Gastroenterol. 2016, 22, 4741–4749. [Google Scholar] [CrossRef] [PubMed]
- Chiorean, L.; Cui, X.W.; Tannapfel, A.; Franke, D.; Stenzel, M.; Kosiak, W.; Schreiber-Dietrich, D.; Jungert, J.; Chang, J.M.; Dietrich, C.F. Benign liver tumors in pediatric patients—Review with emphasis on imaging features. World J. Gastroenterol. 2015, 21, 8541–8561. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.W.; Pirri, C.; Ignee, A.; De Molo, C.; Hirche, T.O.; Schreiber-Dietrich, D.G.; Dietrich, C.F. Measurement of shear wave velocity using acoustic radiation force impulse imaging is not hampered by previous use of ultrasound contrast agents. Z. Gastroenterol. 2014, 52, 649–653. [Google Scholar] [CrossRef] [PubMed]
- Piscaglia, F.; Nolsoe, C.; Dietrich, C.F.; Cosgrove, D.O.; Gilja, O.H.; Bachmann, N.M.; Albrecht, T.; Barozzi, L.; Bertolotto, M.; Catalano, O.; et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): Update 2011 on non-hepatic applications. Ultraschall Med. 2012, 33, 33–59. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Dong, Y.; Jenssen, C.; Ciaravino, V.; Hocke, M.; Wang, W.P.; Burmester, E.; Moeller, K.; Atkinson, N.S.; Capelli, P.; et al. Serous pancreatic neoplasia, data and review. World J. Gastroenterol. 2017, 23, 5567–5578. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Sahai, A.V.; D’Onofrio, M.; Will, U.; Arcidiacono, P.G.; Petrone, M.C.; Hocke, M.; Braden, B.; Burmester, E.; Moller, K.; et al. Differential diagnosis of small solid pancreatic lesions. Gastrointest. Endosc. 2016, 84, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.W.; Chang, J.M.; Kan, Q.C.; Chiorean, L.; Ignee, A.; Dietrich, C.F. Endoscopic ultrasound elastography: Current status and future perspectives. World J. Gastroenterol. 2015, 21, 13212–13224. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, D.; Barr, R.; Bojunga, J.; Cantisani, V.; Chammas, M.C.; Dighe, M.; Vinayak, S.; Xu, J.M.; Dietrich, C.F. WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: Part 4. Thyroid. Ultrasound Med. Biol. 2017, 43, 4–26. [Google Scholar] [CrossRef] [PubMed]
- Dighe, M.; Barr, R.; Bojunga, J.; Cantisani, V.; Chammas, M.C.; Cosgrove, D.; Cui, X.W.; Dong, Y.; Fenner, F.; Radzina, M.; et al. Thyroid ultrasound: State of the art. Part 2—Focal thyroid lesions. Med. Ultrason. 2017, 19, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Dighe, M.; Barr, R.; Bojunga, J.; Cantisani, V.; Chammas, M.C.; Cosgrove, D.; Cui, X.W.; Dong, Y.; Fenner, F.; Radzina, M.; et al. Thyroid ultrasound: State of the art part 1—Thyroid ultrasound reporting and diffuse thyroid diseases. Med. Ultrason. 2017, 19, 79–93. [Google Scholar] [CrossRef] [PubMed]
- Ceyhan Bilgici, M.; Saglam, D.; Delibalta, S.; Yucel, S.; Tomak, L.; Elmali, M. Shear wave velocity of the healthy thyroid gland in children with acoustic radiation force impulse elastography. J. Med. Ultrason. 2018, 45, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, M.; Yildirim, R. The usefulness of strain wave elastography in the diagnosis and grading of hashimoto’s thyroiditis in children. Radiol. Med. 2017, 122, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Saglam, D.; Ceyhan Bilgici, M.; Kara, C.; Can Yilmaz, G.; Tanrivermis Sayit, A. Does type 1 diabetes mellitus affect the shear wave velocity of the thyroid gland of children without autoimmune thyroiditis? Ultrasound Q. 2017, 33, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Bojunga, J. [Ultrasound of the thyroid]. Laryngorhinootologie 2016, 95, 87–104. [Google Scholar] [PubMed]
- Friedrich-Rust, M.; Vorlaender, C.; Dietrich, C.F.; Kratzer, W.; Blank, W.; Schuler, A.; Broja, N.; Cui, X.W.; Herrmann, E.; Bojunga, J. Evaluation of strain elastography for differentiation of thyroid nodules: Results of a prospective degum multicenter study. Ultraschall Med. 2016, 37, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Barr, R.G.; Cosgrove, D.; Brock, M.; Cantisani, V.; Correas, J.M.; Postema, A.W.; Salomon, G.; Tsutsumi, M.; Xu, H.X.; Dietrich, C.F. WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: Part 5. Prostate. Ultrasound Med. Biol. 2017, 43, 27–48. [Google Scholar] [CrossRef] [PubMed]
- Barr, R.G.; Nakashima, K.; Amy, D.; Cosgrove, D.; Farrokh, A.; Schafer, F.; Bamber, J.C.; Castera, L.; Choi, B.I.; Chou, Y.H.; et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: Breast. Ultrasound Med. Biol. 2015, 41, 1148–1160. [Google Scholar] [CrossRef] [PubMed]
- Friedrich-Rust, M.; Schwarz, A.; Ong, M.; Dries, V.; Schirmacher, P.; Herrmann, E.; Samaras, P.; Bojunga, J.; Bohle, R.M.; Zeuzem, S.; et al. Real-time tissue elastography versus fibroscan for noninvasive assessment of liver fibrosis in chronic liver disease. Ultraschall Med. 2009, 30, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Schenk, J.P.; Alzen, G.; Klingmuller, V.; Teufel, U.; El Sakka, S.; Engelmann, G.; Selmi, B. Measurement of real-time tissue elastography in a phantom model and comparison with transient elastography in pediatric patients with liver diseases. Diagn. Interv. Radiol. 2014, 20, 90–99. [Google Scholar] [PubMed]
- Schenk, J.P.; Selmi, B.; Flechtenmacher, C.; Sakka, S.E.; Teufel, U.; Engelmann, G. Real-time tissue elastography (RTE) for noninvasive evaluation of fibrosis in liver diseases in children in comparison to liver biopsy. J. Med. Ultrason. 2014, 41, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Selmi, B.; Engelmann, G.; Teufel, U.; El Sakka, S.; Dadrich, M.; Schenk, J.P. Normal values of liver elasticity measured by real-time tissue elastography (RTE) in healthy infants and children. J. Med. Ultrason. 2014, 41, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Hermeziu, B.; Messous, D.; Fabre, M.; Munteanu, M.; Baussan, C.; Bernard, O.; Poynard, T.; Jacquemin, E. Evaluation of fibrotest-actitest in children with chronic hepatitis c virus infection. Gastroenterol. Clin. Biol. 2010, 34, 16–22. [Google Scholar] [CrossRef] [PubMed]
- El-Shabrawi, M.H.; Mohsen, N.A.; Sherif, M.M.; El-Karaksy, H.M.; Abou-Yosef, H.; El-Sayed, H.M.; Riad, H.; Bahaa, N.; Isa, M.; El-Hennawy, A. Noninvasive assessment of hepatic fibrosis and necroinflammatory activity in egyptian children with chronic hepatitis c virus infection using fibrotest and actitest. Eur. J. Gastroenterol. Hepatol. 2010, 22, 946–951. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Dong, Y. Shear wave elastography with a new reliability indicator. J. Ultrason. 2016, 16, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Kleiner, D.E.; Dam-Larsen, S.; Adams, L.A.; Bjornsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Keach, J.C.; Lafferty, H.D.; Stahler, A.; et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015, 149, 389–397. [Google Scholar] [CrossRef] [PubMed]

| Factor | LSM, kPa | p Value | No. of Children | Study | ||
|---|---|---|---|---|---|---|
| Transient elastography | Factor | 5.5 vs. 4.8 | <0.01 | 527 | Goldschmidt et al., 2013 [1] | |
| Sedation (with vs. without general anesthesia) | 5.4 vs. 4.2 | <0.01 | 527 | Goldschmidt et al., 2013 [1] | ||
| Food intake (no vs. yes) | 5.4 vs. 5.9 | 0.01 | 527 | Goldschmidt et al., 2013 [1] | ||
| Age (years) | 0–5 vs. 6–11 vs. 12–18 | 4.40 vs. 4.73 vs. 5.1 | 0.001 | 240 | Engelmann et al., 2012 [2] | |
| 0–2 vs. 3–5 vs. 6–11 vs. 12–18 | 3.5 vs. 3.8 vs. 4.1 vs. 4.5 | 0.0006 | 173 | Lewindon et al., 2016 [3] | ||
| 1–5 vs. 6–11 vs. 12–18 | 3.4 vs. 3.8 vs. 4.1 | 0.001 | 139 | Tokuhara et al., 2016 [4] | ||
| Gender: boys vs. girls | 5.6 vs. 4.7 | <0.005 | 240 | Engelmann et al., 2012 [2] | ||
| 4.8 vs. 4.1 | N.S | 173 | Lewindon et al., 2016 [3] | |||
| Point shear wave elastography | Probe (linear vs. convex) | SWV, m/s | ||||
| 1.11 vs. 1.13 | 0.52 | 109 | Hanquinet et al., 2013 | |||
| 1.15 vs. 1.19 | N.S | 60 | Fontanilla et al., 2014 | |||
| Age (years) | 0–1 vs. 2–5 vs. 6–10 vs. 11–18 | 1.05 vs. 1.00 vs. 1.12 vs. 1.12 | <0.05 | 176 | Bailey et al., 2017 | |
| 0–1 vs. 1–5 vs. 1–10 vs. 10–17 | 1.11 vs. 1.15 vs. 1.08 vs. 1.14 | N.S | 109 | Hanquinet et al., 2013 | ||
| 0–5 vs. 6–11 vs. 12–17 | 1.11 vs. 1.05 vs. 1.06 | 0.01 | 150 | Matos et al., 2014 | ||
| Gender: boys vs. girls | 1.08 vs. 1.08 | N.S | 176 | Bailey et al., 2017 | ||
| 1.19 vs. 1.13 | 0.02 | 132 | Eiler et al., 2012 | |||
| 1.11 vs. 1.14 | 0.3 | 109 | Hanquinet et al., 2013 | |||
| 1.07 vs. 1.08 | 0.47 | 150 | Matos et al., 2014 | |||
| 1.21 vs. 1.18 | 0.36 | 60 | Fontanilla et al., 2014 | |||
| Left liver lobe vs. right liver lobe | 1.19 vs. 1.14 | 0.03 | 132 | Eiler et al., 2012 | ||
| 1.21 vs. 1.07 | 0.000 | 150 | Matos et al., 2014 | |||
| 1.27 vs. 1.19 | N.S | 60 | Fontanilla et al., 2014 | |||
| Two-dimensional shear wave elastography | Probe (linear vs. convex) | LSM, kPa | ||||
| 5.96 vs. 6.94 | 0.006 | 51 | Franchi-Abella et al., 2016 | |||
| Age | vs. 1–5 vs. 1–10 vs. 10–17 years | 6.00 vs. 6.85 vs. 7.14 vs. 6.97 | 0.11 | 51 | Franchi-Abella et al., 2016 | |
| 0–60 vs. ≥ 60 days | 6.61 vs. 5.3 | 0.02 | 40 | Zhou et al., 2017 | ||
| Gender: boys vs. girls | 6.61 vs. 6.54 | 0.41 | 51 | Franchi-Abella et al., 2016 | ||
| 5.4 vs. 5.6 | 0.63 | 40 | Zhou et al., 2017 | |||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dietrich, C.F.; Sirli, R.; Ferraioli, G.; Popescu, A.; Sporea, I.; Pienar, C.; Kunze, C.; Taut, H.; Schrading, S.; Bota, S.; et al. Current Knowledge in Ultrasound-Based Liver Elastography of Pediatric Patients. Appl. Sci. 2018, 8, 944. https://doi.org/10.3390/app8060944
Dietrich CF, Sirli R, Ferraioli G, Popescu A, Sporea I, Pienar C, Kunze C, Taut H, Schrading S, Bota S, et al. Current Knowledge in Ultrasound-Based Liver Elastography of Pediatric Patients. Applied Sciences. 2018; 8(6):944. https://doi.org/10.3390/app8060944
Chicago/Turabian StyleDietrich, Christoph F., Roxana Sirli, Giovanna Ferraioli, Alina Popescu, Ioan Sporea, Corina Pienar, Christian Kunze, Heike Taut, Simone Schrading, Simona Bota, and et al. 2018. "Current Knowledge in Ultrasound-Based Liver Elastography of Pediatric Patients" Applied Sciences 8, no. 6: 944. https://doi.org/10.3390/app8060944






